The Shinyanga Patient: A Patient’s Journey through HIV Treatment Cascade in Rural Tanzania
Abstract
1. Introduction
2. Materials and Methods
2.1. HIV Testing Access
2.2. CD4 and HIV Viral Load (HVL) Testing Access
2.3. Treatment Access and Outcome
2.4. Ethical Considerations
3. Results
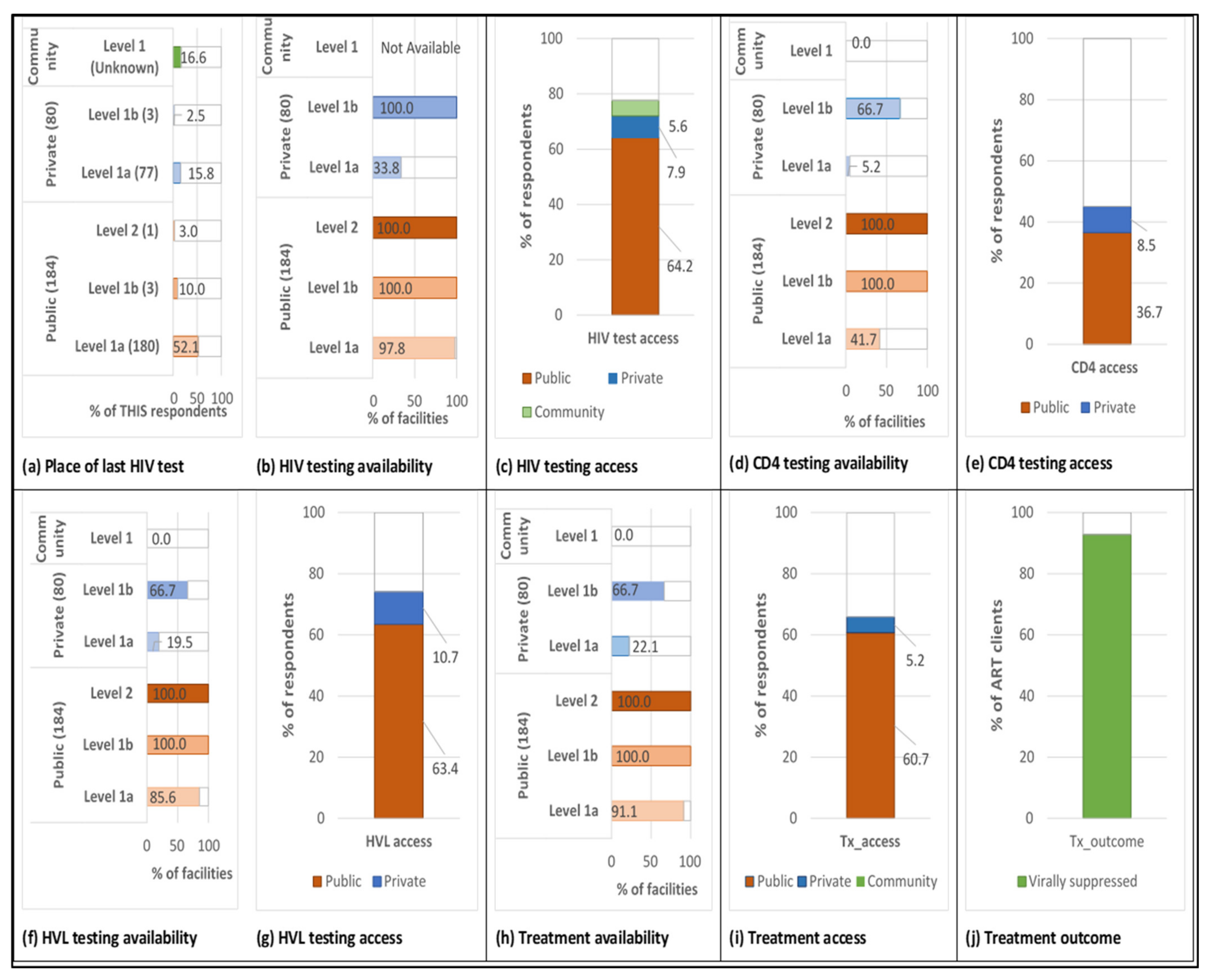
3.1. HIV Testing Access
3.2. CD4 and HIV Viral Load Testing Access
3.3. Treatment Access and Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- UNAIDS (Joint United Nations Programme on HIV/AIDS). Ambitious Treatment Targets: Writing the Final Chapter of the AIDS Epidemic: Writing the Final Chapter of the AIDS Epidemic; UNAIDS: Geneva, Switzerland, 2014; pp. 1–36. [Google Scholar]
- UNAIDS (Joint United Nations Programme on HIV/AIDS). UNAIDS Data 2020; UNAIDS: Geneva, Switzerland, 2020; pp. 1–436. [Google Scholar]
- NACP. Tanzania Hiv Impact Survey (THIS) 2016–2017; NACP: Dodoma, Tanzania, 2018; pp. 2016–2017. [Google Scholar]
- Rice, B.; Boulle, A.; Baral, S.; Egger, M.; Mee, P.; Fearon, E.; Reniers, G.; Todd, J.; Schwarcz, S.; Weir, S.; et al. Strengthening Routine Data Systems to Track the HIV Epidemic and Guide the Response in Sub-Saharan Africa. JMIR Public Health Surveill. 2018, 4, e36. [Google Scholar] [CrossRef] [PubMed]
- Ehrenkranz, P.; Rosen, S.; Boulle, A.; Eaton, J.W.; Ford, N.; Fox, M.P.; Grimsrud, A.; Rice, B.D.; Sikazwe, I.; Holmes, C.B. The revolving door of HIV care: Revising the service delivery cascade to achieve the UNAIDS 95-95-95 goals. PLoS Med. 2021, 18, e1003651. [Google Scholar] [CrossRef]
- Ostermann, J.; Njau, B.; Brown, D.; Mühlbacher, A.; Thielman, N. Heterogeneous HIV Testing Preferences in an Urban Setting in Tanzania: Results from a Discrete Choice Experiment. PLoS ONE 2014, 9, e92100. [Google Scholar] [CrossRef]
- Ostermann, J.; Njau, B.; Mtuy, T.; Brown, D.; Muhlbacher, A.C.; Thielman, N.M. One size does not fit all: HIV testing preferences differ among high-risk groups in Northern Tanzania. AIDS Care 2015, 27, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Njau, B.; Ostermann, J.; Brown, D.; Mühlbacher, A.; Reddy, E.; Thielman, N. HIV testing preferences in Tanzania: A qualitative exploration of the importance of confidentiality, accessibility, and quality of service. BMC Public Health 2014, 14, 838. [Google Scholar] [CrossRef]
- Yamanis, T.J.; Dervisevic, E.; Mulawa, M.I.; Conserve, D.F.; Barrington, C.; Kajula, L.J.; Maman, S. Social Network Influence on HIV Testing Among Urban Men in Tanzania. AIDS Behav. 2017, 21, 1171–1182. [Google Scholar] [CrossRef] [PubMed]
- Meremo, A.; Mboya, B.; Ngilangwa, D.; Dulle, R.; Tarimo, E.; Urassa, D.; Michael, E.; Gibore, N.; Mpondo, B.; Mchonde, G.; et al. Barriers to accessibility and utilization of HIV testing and counseling services in Tanzania: Experience from Angaza Zaidi programme. Pan Afr. Med. J. 2016, 23. [Google Scholar] [CrossRef]
- Sanga, E.S.; Mukumbang, F.C.; Mushi, A.K.; Lerebo, W.; Zarowsky, C. Understanding factors influencing linkage to HIV care in a rural setting, Mbeya, Tanzania: Qualitative findings of a mixed methods study. BMC Public Health 2019, 19, 383. [Google Scholar] [CrossRef]
- Conserve, D.F.; Issango, J.; Kilale, A.M.; Njau, B.; Nhigula, P.; Memiah, P.; Mbita, G.; Choko, A.T.; Hamilton, A.; King, G. Developing national strategies for reaching men with HIV testing services in Tanzania: Results from the male catch-up plan. BMC Health Serv. Res. 2019, 19, 317. [Google Scholar] [CrossRef]
- Mukumbang, F.C.; Mwale, J.C.; van Wyk, B. Conceptualising the Factors Affecting Retention in Care of Patients on Antiretroviral Treatment in Kabwe District, Zambia, Using the Ecological Framework. AIDS Res. Treat. 2017, 2017, 1–11. [Google Scholar] [CrossRef]
- Ayieko, J.; Brown, L.; Anthierens, S.; van Rie, A.; Getahun, M.; Charlebois, E.D.; Petersen, M.L.; Clark, T.D.; Kamya, M.R.; Cohen, C.R.; et al. “Hurdles on the path to 90-90-90 and beyond”: Qualitative analysis of barriers to engagement in HIV care among individuals in rural East Africa in the context of test-and-treat. PLoS ONE 2018, 13, e0202990. [Google Scholar] [CrossRef]
- Ankomah, A.; Ganle, J.K.; Lartey, M.Y.; Kwara, A.; Nortey, P.A.; Okyerefo, M.P.K.; Laar, A.K. ART access-related barriers faced by HIV-positive persons linked to care in southern Ghana: A mixed method study. BMC Infect. Dis. 2016, 16, 738. [Google Scholar] [CrossRef] [PubMed]
- The United Republic of Tanzania. Global Aids Response Country Progress Report; UNAIDS: Geneva, Switzerland, 2014; pp. 1–43. [Google Scholar]
- WorldLifeExpectancy.com. Physicians per 10,000 by Country. 2017. Available online: https://www.worldlifeexpectancy.com/physicians-ratio-by-country (accessed on 11 May 2021).
- Church, K.; Machiyama, K.; Todd, J.; Njamwea, B.; Mwangome, M.; Hosegood, V.; Michel, J.; Oti, S.; Nyamukapa, C.; Crampin, A.; et al. Identifying gaps in HIV service delivery across the diagnosis-to-treatment cascade: Findings from health facility surveys in six sub-Saharan countries. J. Int. AIDS Soc. 2017, 20, 21188. [Google Scholar] [CrossRef] [PubMed]
- Ma, A.; Chambers, B.D.; Hall, W.J.; Tanner, A.E.; Piper, C.N. Individual and structural factors influencing HIV care linkage and engagement: Perceived barriers and solutions among HIV-positive persons. J. HIV/AIDS Soc. Serv 2016, 1–9. [Google Scholar] [CrossRef]
- National Bureau of Statistics Tanzania, (NBS); Office of Chief Government Statistician (OCGS). Shinyanga Region: Basic Demographic and Socio-Economic Profile—2012 Population and Housing Census; NBS: Dar Es Salaam, Tanzania; OCGS: Zanzibar, Tanzania, 2016.
- MoHCDGEC. NACP HIV Data Handbook, 2nd ed; Ministry of Health, Community Development, Gender, Elderly, and Children; MoHCDGEC: Dodoma, Tanzania, 2019. [Google Scholar]
- Hanson, C.L.; Osberg, M.; Brown, J.; Durham, G.; Chin, D.P. Conducting Patient-Pathway Analysis to Inform Programming of Tuberculosis Services: Methods. J. Infect. Dis. 2017, 216, S679–S685. [Google Scholar] [CrossRef] [PubMed]
- Masini, E.; Hanson, C.; Ogoro, J.; Brown, J.; Ngari, F.; Mingkwan, P.; Makayova, J.; Osberg, M. Using Patient-Pathway Analysis to Inform a Differentiated Program Response to Tuberculosis: The Case of Kenya. J. Infect. Dis. 2017, 216, S714–S723. [Google Scholar] [CrossRef]
- Ministry of Health. Community Development, Gender E and C. HFR WEB PORTAL—Site. 2018. Available online: http://hfrportal.ehealth.go.tz/index.php?r=site/index (accessed on 22 February 2019).
- MOHCDGEC; NACP. DHIS2 Summary Report; MOHCDGEC: Dodoma, Tanzania; NACP: Dodoma, Tanzania, 2019. [Google Scholar]
- MoHSW; MoH; NBS; OCGS; ICF International. Tanzania Service Provision Assessment Survey (TSPA) 2014–15; Ministry of Health and Social Welfare: Dar es Salaam, Tanzania; Ministry of Health: Zanzibar, Tanzania; National Bureau of Statistics: Dar es Salaam, Tanzania; Office of Chief Government Statistician: Zanzibar, Tanzania; ICF InternationaL: Rockville, MD, USA, 2016. [Google Scholar]
- PHIA Project. Guiding the Global HIV Response n.d. Available online: https://phia.icap.columbia.edu/ (accessed on 21 July 2021).
- Deribew, A.; Biadgilign, S.; Berhanu, D.; Defar, A.; Deribe, K.; Tekle, E.; Asheber, K.; Dejene, T. Capacity of health facilities for diagnosis and treatment of HIV/AIDS in Ethiopia. BMC Health Serv. Res. 2018, 18, 535. [Google Scholar] [CrossRef]
- Boex, J.; Fuller, L.; Malik, A. Decentralized Local Health Services in Tanzania. Urban Institute: Washington, DC, USA, 2015; p. 20037. [Google Scholar]
- Olakunde, B.; Adeyinka, D.; Ozigbu, C.; Ogundipe, T.; Menson, W.; Olawepo, J.; Olakunde, O.; Ezeanolue, E. Revisiting aid dependency for HIV programs in Sub-Saharan Africa. Public Health 2019, 170, 57–60. [Google Scholar] [CrossRef]
- Ochonye, B.; Folayan, M.O.; Fatusi, A.O.; Emmanuel, G.; Adepoju, O.; Ajidagba, B.; Jaiyebo, T.; Umoh, P.; Yusuf, A. Satisfaction with use of public health and peer-led facilities for HIV prevention services by key populations in Nigeria. BMC Health Serv. Res. 2019, 19, 856. [Google Scholar] [CrossRef]
- Leveraging the Private Health Sector to Expand the HIV/AIDS Workforce; Report; USAID: Washington, DC, USA, 2018.
- Nash, D.; Yotebieng, M.; Sohn, A.H. Treating all people living with HIV in sub-Saharan Africa: A new era calling for new approaches. J. Virus Erad. 2018, 4, 1–4. [Google Scholar] [CrossRef]
- Sileo, K.M.; Fielding-Miller, R.; Dworkin, S.L.; Fleming, P.J. What Role Do Masculine Norms Play in Men’s HIV Testing in Sub-Saharan Africa? A Scoping Review. AIDS Behav. 2018, 22, 2468–2479. [Google Scholar] [CrossRef]
- Mosha, I.H.; Nsanzugwanko, N.W.; Ezekiel, M.J.; Metta, E. Factors Influencing Retention of HIV/AIDS Care and Treatment among Adolescents Living with HIV in Mkuranga District Tanzania; BAOJ HIV; ACADEMIA: San Fracisco, CA, USA.
- Lippman, S.A.; El Ayadi, A.M.; Grignon, J.S.; Puren, A.; Liegler, T.; Venter, W.D.F.; Ratlhagana, M.J.; Morris, J.L.; Naidoo, E.; Agnew, E.; et al. Improvements in the South AfricanHIVcare cascade: Findings on 90-90-90 targets from successive population-representative surveys in North West Province. J. Int. AIDS Soc. 2019, 22, e25295. [Google Scholar] [CrossRef]
- Lopez-Varela, E.; Augusto, O.; Fuente-Soro, L.; Sacoor, C.; Nhacolo, A.; Casavant, I.; Karajeanes, E.; Vaz, P.; Naniche, D. Quantifying the gender gap in the HIV care cascade in southern Mozambique: We are missing the men. PLoS ONE 2021, 16, e0245461. [Google Scholar] [CrossRef]
- Vyas, S.; Songo, J.; Guinness, L.; Dube, A.; Geis, S.; Kalua, T.; Todd, J.; Renju, J.; Crampin, A.; Wringe, A. Assessing the costs and efficiency of HIV testing and treatment services in rural Malawi: Implications for future “test and start” strategies. BMC Health Serv. Res. 2020, 20, 740. [Google Scholar] [CrossRef]
- Govender, K.; Masebo, W.G.; Nyamaruze, P.; Cowden, R.G.; Schunter, B.T.; Bains, A. HIV Prevention in Adolescents and Young People in the Eastern and Southern African Region: A Review of Key Challenges Impeding Actions for an Effective Response. Open AIDS J. 2018, 12, 53–67. [Google Scholar] [CrossRef] [PubMed]
- Asiimwe, S.; Ross, J.; Arinaitwe, A.; Tumusiime, O.; Turyamureeba, B.; Roberts, A.; O’Malley, G.; Barnabas, R.V. Expanding HIV testing and linkage to care in southwestern Uganda with community health extension workers. J. Int. AIDS Soc. 2017, 20, 80–87. [Google Scholar] [CrossRef]
- Mfinanga, G.A.; Mutayoba, B.; Mbogo, G.; Kahwa, A.; Kimaro, G.; Mhame, P.P.; Mwangi, C.; Malecela, M.N.; Kitua, A.Y. Quality of HIV laboratory testing in Tanzania: A situation analysis. Tanzan. J. Health Res. 2007, 9, 44–47. [Google Scholar] [CrossRef] [PubMed]
- Oberth, G.; Whiteside, A. What does sustainability mean in the HIV and AIDS response? Afr. J. AIDS Res. 2016, 15, 35–43. [Google Scholar] [CrossRef]
- Renju, J.; Rice, B.; Songo, J.; Hassan, F.; Chimukuche, R.S.; McLean, E.; Kalua, T.; Kajoka, D.; Geubbels, E.; Moshabela, M.; et al. Influence of evolving HIV treatment guidance on CD4 counts and viral load monitoring: A mixed-methods study in three African countries. Glob. Public Health 2021, 16, 288–304. [Google Scholar] [CrossRef]
- Thimbleby, H. Guidelines for ‘manipulative’ text editing. Behav. Inf. Technol. 1983, 2, 127–161. [Google Scholar] [CrossRef]
- PEPFAR. What’s New in COP20; Guidance for all PEPFAR Countries; PEPFAR: Washington, DC, USA, 2020. [Google Scholar]
- Zaniewski, E.; Ostinelli, C.H.D.; Chammartin, F.; Maxwell, N.; Davies, M.; Euvrard, J.; van Dijk, J.; Bosomprah, S.; Phiri, S.; Tanser, F.; et al. Trends in CD4 and viral load testing 2005 to 2018: Multi-cohort study of people living with HIV in Southern Africa. J. Int. AIDS Soc. 2020, 23. [Google Scholar] [CrossRef]
- Mboera, L.E.; Ishengoma, D.S.; Kilale, A.M.; Massawe, I.S.; Rutta, A.S.; Kagaruki, G.B.; Kamugisha, E.; Baraka, V.; Mandara, C.I.; Materu, G.S.; et al. The readiness of the national health laboratory system in supporting care and treatment of HIV/AIDS in Tanzania. BMC Health Serv. Res. 2015, 15, 248. [Google Scholar] [CrossRef]
- Vogt, F.; Tayler-Smith, K.; Bernasconi, A.; Makondo, E.; Taziwa, F.; Moyo, B.; Havazvidi, L.; Satyanarayana, S.; Manzi, M.; Khogali, M.; et al. Access to CD4 Testing for Rural HIV Patients: Findings from a Cohort Study in Zimbabwe. PLoS ONE 2015, 10, e0129166. [Google Scholar] [CrossRef]
- Alemnji, G.; Peter, T.; Vojnov, L.; Alexander, H.; Zeh, C.; Cohn, J.; Watts, D.H.; de Lussigny, S. Building and Sustaining Optimized Diagnostic Networks to Scale-up HIV Viral Load and Early Infant Diagnosis. JAIDS J. Acquir. Immune Defic. Syndr. 2020, 84, S56–S62. [Google Scholar] [CrossRef] [PubMed]
- Alemnji, G.; Fonjungo, P.; van der Pol, B.; Peter, T.; Kantor, R.; Nkengasong, J. The centrality of laboratory services in the HIV treatment and prevention cascade: The need for effective linkages and referrals in resource-limited settings. AIDS Patient Care STDs 2014, 28, 268–273. [Google Scholar] [CrossRef]
- International Monetary Fund; African Dept. United Republic of Tanzania. IMF Staff Country Report; International Monetary Fund: Washington, DC, USA, 2020; p. 20. [Google Scholar] [CrossRef]
- Stanifer, J.W.; Patel, U.D.; Karia, F.; Thielman, N.; Maro, V.; Shimbi, D.; Kilaweh, H.; Lazaro, M.; Matemu, O.; Omolo, J.; et al. The Determinants of Traditional Medicine Use in Northern Tanzania: A Mixed-Methods Study. PLoS ONE 2015, 10, e0122638. [Google Scholar] [CrossRef] [PubMed]
- Wanyama, J.N.; Tsui, S.; Kwok, C.; Wanyenze, R.K.; Denison, J.; Koole, O.; van Praag, E.; Castelnuovo, B.; Wabwire-Mangen, F.; Kwesigabo, G.P.; et al. Persons living with HIV infection on antiretroviral therapy also consulting traditional healers: A study in three African countries. Int. J. STD AIDS 2017, 28, 1018–1027. [Google Scholar] [CrossRef] [PubMed]
- Moshabela, M.; Bukenya, D.; Darong, G.G.; Wamoyi, J.; McLean, E.; Skovdal, M.; Ddaaki, W.; Ondeng’E, K.; Bonnington, O.; Seeley, J.; et al. Traditional healers, faith healers and medical practitioners: The contribution of medical pluralism to bottlenecks along the cascade of care for HIV/AIDS in Eastern and Southern Africa. Sex. Transm. Infect. 2017, 93, e052974. [Google Scholar] [CrossRef]
- Rutta, E.; Liana, J.; Embrey, M.; Johnson, K.J.; Kimatta, S.; Valimba, R.; Lieber, R.; Shekalaghe, E.; Sillo, H. Accrediting retail drug shops to strengthen Tanzania’s public health system: An ADDO case study. J. Pharm. Policy Pr. 2015, 8, 1–15. [Google Scholar] [CrossRef]
- Ntamatungiro, A.J.; Muri, L.; Glass, T.; Erb, S.; Battegay, M.; Furrer, H.; Hatz, C.; Tanner, M.; Felger, I.; Klimkait, T.; et al. Strengthening HIV therapy and care in rural Tanzania affects rates of viral suppression. J. Antimicrob. Chemother. 2017, 72, 2069–2074. [Google Scholar] [CrossRef] [PubMed]
- Petersen, M.; Balzer, L.; Kwarsiima, D.; Sang, N.; Chamie, G.; Ayieko, J.; Kabami, J.; Owaraganise, A.; Liegler, T.; Mwangwa, F.; et al. Association of Implementation of a Universal Testing and Treatment Intervention with HIV Diagnosis, Receipt of Antiretroviral Therapy, and Viral Suppression in East Africa. JAMA 2017, 317, 2196–2206. [Google Scholar] [CrossRef]
- Webber, G.; Chirangi, B.; Magatti, N. Promoting respectful maternity care in rural Tanzania: Nurses’ experiences of the “Health Workers for Change” program. BMC Health Serv. Res. 2018, 18, 658. [Google Scholar] [CrossRef] [PubMed]
- Khamis, K.; Njau, B. Patients’ level of satisfaction on quality of health care at Mwananyamala hospital in Dar es Salaam, Tanzania. BMC Health Serv. Res. 2014, 14, 400. [Google Scholar] [CrossRef]
- QAP Tanzania HIV Stigma Study Team. Evaluation of Knowledge, Attitudes, and Practices of Health Care Providers toward HIV-positive Patients in Tanzania. Operations Research Results. Published for the U.S. Agency for International Development (USAID); University Research Co., LLC: Chevy Chase, MD, USA, 2007. [Google Scholar]
- Primary Healthcare Systems (PRIMASYS) Comprehensive Case Study from the United Republic of Tanzania; World Health Organisation: Geneva, Switzerland, 2017.
- Makuka, G.J.; Sango, M.M.; Mashambo, A.E.; Mashambo, A.E.; Msuya, S.E.; Mtweve, S.P. Clients’ Perspectives on Quality of Delivery Services in a Rural Setting in Tanzania: Findings from a Qualitative Action-Oriented Research. Int. J. Mch. Aids 2017, 6, 60–68. [Google Scholar] [CrossRef]
- An, S.J.; George, A.S.; Lefevre, A.E.; Mpembeni, R.; Mosha, I.; Mohan, D.; Yang, A.; Chebet, J.; Lipingu, C.; Baqui, A.H.; et al. Supply-side dimensions and dynamics of integrating HIV testing and counselling into routine antenatal care: A facility assessment from Morogoro Region, Tanzania. BMC Health Serv. Res. 2015, 15, 451. [Google Scholar] [CrossRef]
- Marwa, R.; Anaeli, A. Perceived Barriers Toward Provider-Initiated HIV Testing and Counseling (PITC) in Pediatric Clinics: A Qualitative Study Involving Two Regional Hospitals in Dar-Es-Salaam, Tanzania. HIV/AIDS Res. Palliat. Care 2020, 12, 141–150. [Google Scholar] [CrossRef]
- Nsimba, S.E.; Irunde, H.; Comoro, C. Barriers to ARV Adherence among HIV/AIDS Positive Persons taking Anti-Retroviral Therapy in Two Tanzanian Regions 8-12 Months after Program Initiation. J. AIDS Clin. Res. 2010, 1, 2155–6113. [Google Scholar] [CrossRef] [PubMed]
- Layer, E.H.; Kennedy, C.E.; Beckham, S.W.; Mbwambo, J.K.; Likindikoki, S.; Davis, W.W.; Kerrigan, D.L.; Brahmbhatt, H. The LTC Tanzania Collaborative Study Team Multi-Level Factors Affecting Entry into and Engagement in the HIV Continuum of Care in Iringa, Tanzania. PLoS ONE 2014, 9, e104961. [Google Scholar] [CrossRef]
- Tomori, C.; Kennedy, C.E.; Brahmbhatt, H.; Wagman, J.; Mbwambo, J.K.; Likindikoki, S.; Kerrigan, D.L. Barriers and facilitators of retention in HIV care and treatment services in Iringa, Tanzania: The importance of socioeconomic and sociocultural factors. AIDS Care 2014, 26, 907–913. [Google Scholar] [CrossRef]
- Nyato, D.; Nnko, S.; Komba, A.; Kuringe, E.; Plotkin, M.; Mbita, G.; Shao, A.; Changalucha, J.; Wambura, M. Facilitators and barriers to linkage to HIV care and treatment among female sex workers in a community-based HIV prevention intervention in Tanzania: A qualitative study. PLoS ONE 2019, 14, e0219032. [Google Scholar] [CrossRef] [PubMed]
- Mnzava, T.; Mmari, E.; Berruti, A. Drivers of Patient Costs in Accessing HIV/AIDS Services in Tanzania. J. Int. Assoc. Provid. AIDS Care 2018, 17. [Google Scholar] [CrossRef] [PubMed]
- Chimbindi, N.; Bor, J.; Newell, M.-L.; Tanser, F.; Baltussen, R.; Hontelez, J.; de Vlas, S.J.; Lurie, M.; Pillay, D.; Bärnighausen, T. Time and Money. JAIDS J. Acquir. Immune Defic. Syndr. 2015, 70, e52–e60. [Google Scholar] [CrossRef] [PubMed]
- Sanga, E.S.; Lerebo, W.; Mushi, A.K.; Clowes, P.; Olomi, W.; Maboko, L.; Zarowsky, C. Linkage into care among newly diagnosed HIV-positive individuals tested through outreach and facility-based HIV testing models in Mbeya, Tanzania: A prospective mixed-method cohort study. BMJ Open 2017, 7, e013733. [Google Scholar] [CrossRef] [PubMed]
| Component | Sub-Component | Data Source(s) |
|---|---|---|
| Number of facilities | Formal private and public facilities | Tanzania Health Facility registry (HFR) [24] |
| Place of last HIV test | HIV testing availability | HFR [24] |
| District Health Information Software (DHIS2) summary report [25] | ||
| 2014 – 2015 Tanzanian Service Provision Assessment Survey (TSPA) [26] | ||
| HIV testing access | 2016 – 2017 Tanzanian HIV impact survey (THIS) [3] | |
| HIV diagnostics at the place of last HIV test | *CD4 count and HIV viral load test availability | HFR [24]; |
| DHIS2 summary report | ||
| CD4 count and HIV viral load access | THIS [3] | |
| HIV treatment at the place of last HIV test | HIV treatment availability | THIS [3] |
| DHIS2 summary report | ||
| HIV treatment access | THIS [24] | |
| HFR [24] | ||
| HIV treatment outcome | HIV treatment outcome (viral suppression) | National AIDS Control Program (NACP) HIV data handbook [21] |
| Data Source | Facility Type | Facility Sector | Level |
|---|---|---|---|
| Tanzania Health Facility Registry (HFR) | Clinic | Public and Private | 1a |
| Clinic – Dental Clinic | Private | 1a | |
| Clinic – Diagnostic Centre | Private | 1a | |
| Clinic – Dialysis Clinic | Private | 1a | |
| Clinic – Eye Clinic | Private | 1a | |
| Clinic – General Clinic | Private | 1a | |
| Clinic – Medical Clinic | Public and Private | 1a | |
| Clinic – Optometry Clinic | Private | 1a | |
| Clinic – Other Clinic | Public and Private | 1a | |
| Clinic – Physiotherapy Clinic | Private | 1a | |
| Clinic – Polyclinic | Private | 1a | |
| Clinic – Specialized clinic/Polyclinic; Super specialized clinic/ Polyclinic | Private | 1a | |
| Dispensary | Public and Private | 1a | |
| Health Center | Public and Private | 1a | |
| Health Labs | Public and Private | 1a | |
| Health Labs – Level IA1 (Health Center Laboratory) | Private | 1a | |
| Health Labs – Level IA2 (Dispensary Laboratory) | Public and Private | 1a | |
| Health Labs – Level III Multipurpose Health Laboratory | Private | 1a | |
| Health Labs – Level III single purpose Health Laboratory | Private | 1a | |
| Health Labs – Specimen collection point | Private | 1a | |
| Hospital | Private | 1a | |
| Hospital – Council Designated Hospital | Public and Private | 1a | |
| Hospital – Other Hospital | Public and Private | 1a | |
| Maternity and Nursing Home | Private | 1a | |
| Maternity Home | Public and Private | 1a | |
| Nursing Home | Public and Private | 1 | |
| Health Labs – Level IIA2 (District Laboratory) | Private | 1b | |
| Hospital – District Hospital | Public | 1b | |
| Hospital – Hospital at District Level | Public and Private | 1b | |
| Hospital – Hospital at Regional Level | Private | 2 | |
| Hospital – Referral Hospital at Regional Level | Private | 2 | |
| Hospital – Regional Referral Hospital | Public | 2 | |
| Hospital – Hospital at Zonal Level | Public and Private | 3 | |
| Hospital – Referral Hospital at Zonal Level | Public and Private | 3 | |
| Hospital – Super Specialized Hospital at National Level | Public and Private | 4 | |
| Hospital – Referral Hospital at National Level | Public | 4 | |
| 2016–2017 Tanzania HIV Impact Survey (THIS) | ANC clinic | Public and Private | 1a |
| At home | Community | 1a | |
| Blood donating center | Public | 1b, 2 | |
| Campaigns | Community | 1a | |
| Health clinic/Facility | Public and Private | 1a | |
| Hospital inpatient wards | Public and Private | 1b, 2 | |
| Hospital outpatient clinic | Public and Private | 1b, 2 | |
| Mobile VCT | Community | 1a | |
| Social events | Community | 1a | |
| STI clinic | Public and Private | 1a | |
| TB clinic | Public and Private | 1a | |
| VCT facility | Public and Private | 1a |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okere, N.E.; Sambu, V.; Ndungile, Y.; van Praag, E.; Hermans, S.; Naniche, D.; de Wit, T.F.R.; Maokola, W.; Gomez, G.B. The Shinyanga Patient: A Patient’s Journey through HIV Treatment Cascade in Rural Tanzania. Int. J. Environ. Res. Public Health 2021, 18, 8418. https://doi.org/10.3390/ijerph18168418
Okere NE, Sambu V, Ndungile Y, van Praag E, Hermans S, Naniche D, de Wit TFR, Maokola W, Gomez GB. The Shinyanga Patient: A Patient’s Journey through HIV Treatment Cascade in Rural Tanzania. International Journal of Environmental Research and Public Health. 2021; 18(16):8418. https://doi.org/10.3390/ijerph18168418
Chicago/Turabian StyleOkere, Nwanneka E, Veryeh Sambu, Yudas Ndungile, Eric van Praag, Sabine Hermans, Denise Naniche, Tobias F Rinke de Wit, Werner Maokola, and Gabriela B Gomez. 2021. "The Shinyanga Patient: A Patient’s Journey through HIV Treatment Cascade in Rural Tanzania" International Journal of Environmental Research and Public Health 18, no. 16: 8418. https://doi.org/10.3390/ijerph18168418
APA StyleOkere, N. E., Sambu, V., Ndungile, Y., van Praag, E., Hermans, S., Naniche, D., de Wit, T. F. R., Maokola, W., & Gomez, G. B. (2021). The Shinyanga Patient: A Patient’s Journey through HIV Treatment Cascade in Rural Tanzania. International Journal of Environmental Research and Public Health, 18(16), 8418. https://doi.org/10.3390/ijerph18168418





