Pickleball for Inactive Mid-Life and Older Adults in Rural Utah: A Feasibility Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Eligibility
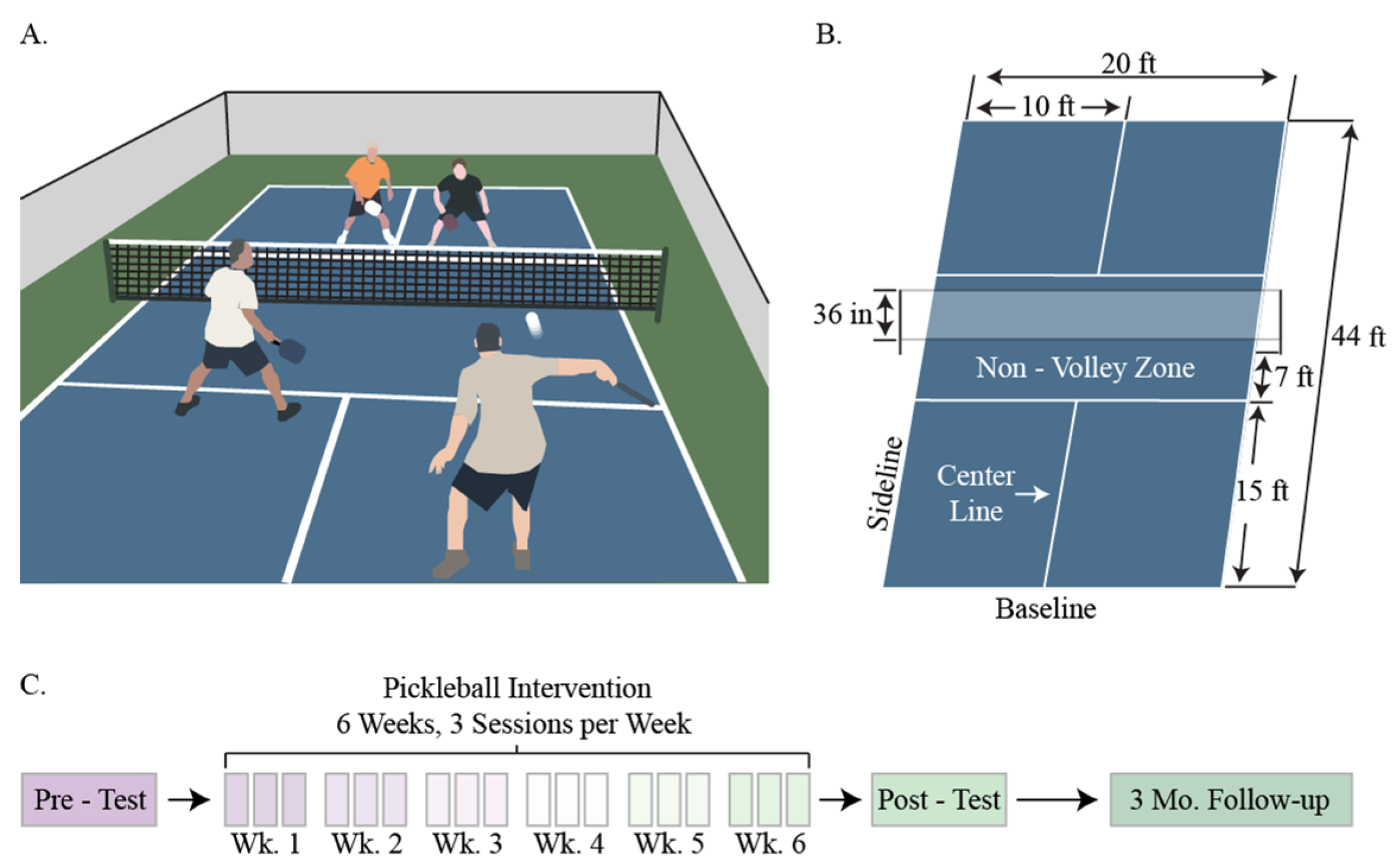
2.2. Pickleball Intervention
2.3. Outcome Measures
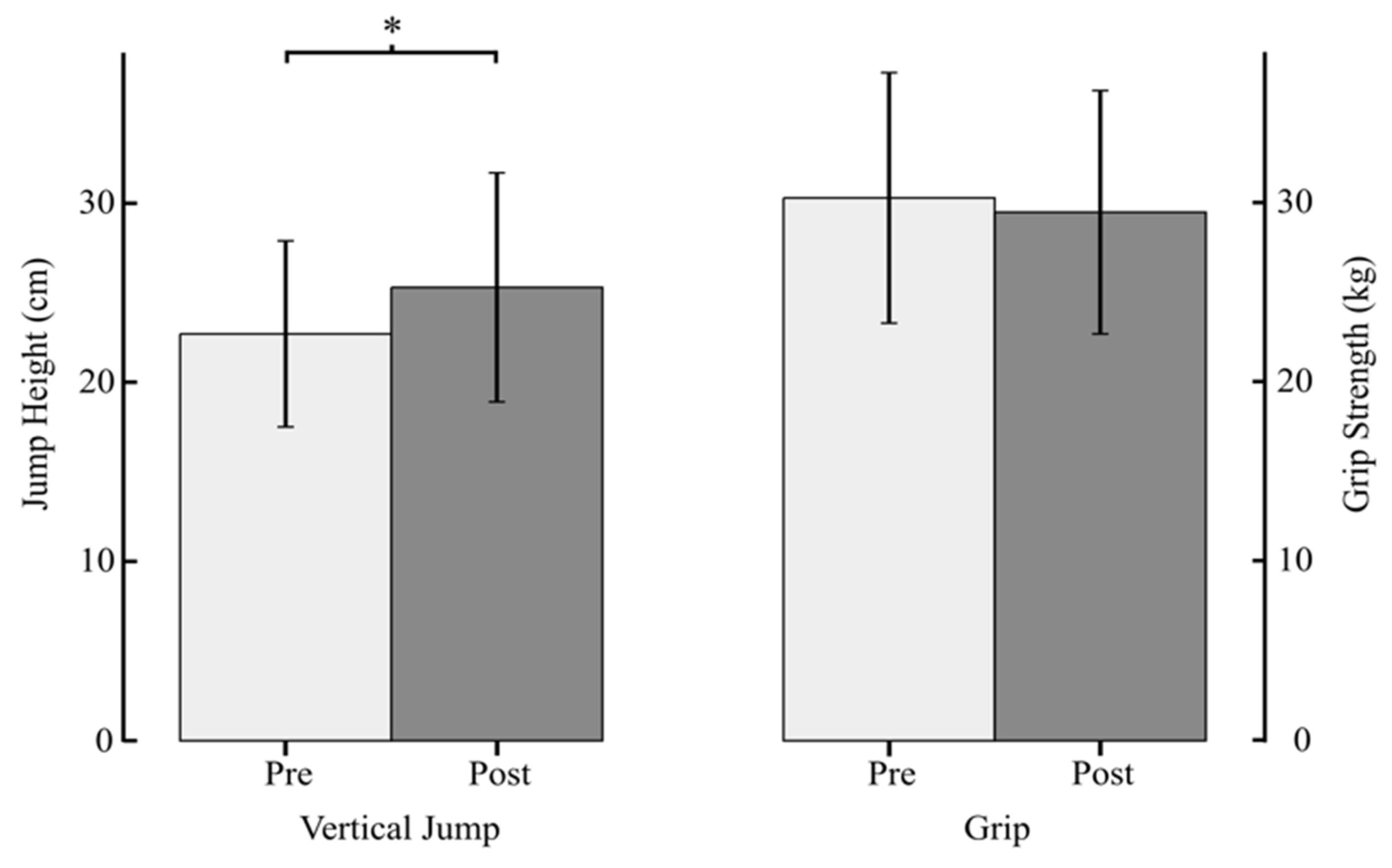
2.3.1. Muscle Function
2.3.2. Cognitive Function
2.3.3. Perceived Pain
2.3.4. Cardio-Metabolic Risk
2.3.5. Psychosocial Factors
2.4. Data Analysis
3. Results
4. Discussion
4.1. Limitations
4.2. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.-M.; Nieman, D.C.; Swain, D.P.; American College of Sports Medicine American College of Sports Medicine Position Stand. Quantity and Quality of Exercise for Developing and Maintaining Cardiorespiratory, Musculoskeletal, and Neuromotor Fitness in Apparently Healthy Adults: Guidance for Prescribing Exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Carter, N.D.; Khan, K.M.; McKay, H.A.; Petit, M.A.; Waterman, C.; Heinonen, A.; Janssen, P.A.; Donaldson, M.G.; Mallinson, A.; Riddell, L.; et al. Community-Based Exercise Program Reduces Risk Factors for Falls in 65- to 75-Year-Old Women with Osteoporosis: Randomized Controlled Trial. CMAJ 2002, 167, 997–1004. [Google Scholar] [PubMed]
- Sofi, F.; Valecchi, D.; Bacci, D.; Abbate, R.; Gensini, G.F.; Casini, A.; Macchi, C. Physical Activity and Risk of Cognitive Decline: A Meta-Analysis of Prospective Studies. J. Intern. Med. 2011, 269, 107–117. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.J.; Xavier, D.; Liu, L.; Zhang, H.; Chin, S.L.; Rao-Melacini, P.; Rangarajan, S.; Islam, S.; Pais, P.; McQueen, M.J.; et al. Risk Factors for Ischaemic and Intracerebral Haemorrhagic Stroke in 22 Countries (the INTERSTROKE Study): A Case-Control Study. Lancet 2010, 376, 112–123. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention’s (CDC); National Center for Health Statistics (NCHS). Available online: https://www.cdc.gov/nchs/fastats/exercise.htm (accessed on 17 December 2020).
- Whitfield, G.P.; Carlson, S.A.; Ussery, E.N.; Fulton, J.E.; Galuska, D.A.; Petersen, R. Trends in Meeting Physical Activity Guidelines Among Urban and Rural Dwelling Adults—United States, 2008-2017. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 513–518. [Google Scholar] [CrossRef] [Green Version]
- Blackwell, D.L.; Clarke, T.C. State Variation in Meeting the 2008 Federal Guidelines for Both Aerobic and Muscle-Strengthening Activities Through Leisure-Time Physical Activity Among Adults Aged 18–64: United States, 2010–2015. Natl. Health Stat. Rep. 2018, 6, 1–22. [Google Scholar]
- King, A.C.; King, D.K. Physical Activity for an Aging Population. Public Health Rev. 2010, 32, 401–426. [Google Scholar] [CrossRef] [Green Version]
- Schutzer, K.A.; Graves, B.S. Barriers and Motivations to Exercise in Older Adults. Prev. Med. 2004, 39, 1056–1061. [Google Scholar] [CrossRef]
- Chao, D.; Foy, C.G.; Farmer, D. Exercise Adherence among Older Adults: Challenges and Strategies. Control. Clin. Trials 2000, 21, S212–S217. [Google Scholar] [CrossRef]
- Costello, E.; Kafchinski, M.; Vrazel, J.; Sullivan, P. Motivators, Barriers, and Beliefs Regarding Physical Activity in an Older Adult Population. J. Geriatr. Phys. Ther. 2011, 34, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Belza, B.; Walwick, J.; Shiu-Thornton, S.; Schwartz, S.; Taylor, M.; LoGerfo, J. Older Adult Perspectives on Physical Activity and Exercise: Voices from Multiple Cultures. Prev. Chronic Dis. 2004, 1, A09. [Google Scholar] [PubMed]
- Neighborhood Safety and the Prevalence of Physical Inactivity—Selected States. 1996. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/00056582.htm (accessed on 24 November 2020).
- Martin, S.L.; Kirkner, G.J.; Mayo, K.; Matthews, C.E.; Durstine, J.L.; Hebert, J.R. Urban, Rural, and Regional Variations in Physical Activity. J. Rural. Health 2005, 21, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.X.; Wen, M.; Kowaleski-Jones, L. Rural-Urban Differences in Objective and Subjective Measures of Physical Activity: Findings from the National Health and Nutrition Examination Survey (NHANES) 2003–2006. Prev. Chronic Dis. 2014, 11, E141. [Google Scholar] [CrossRef] [Green Version]
- Kolt, G.S.; Driver, R.P.; Giles, L.C. Why Older Australians Participate in Exercise and Sport. J. Aging Phys. Act. 2004, 12, 185–198. [Google Scholar] [CrossRef] [PubMed]
- Newson, R.S.; Kemps, E.B. Factors That Promote and Prevent Exercise Engagement in Older Adults. J. Aging Health 2007, 19, 470–481. [Google Scholar] [CrossRef]
- Oja, P.; Kelly, P.; Pedisic, Z.; Titze, S.; Bauman, A.; Foster, C.; Hamer, M.; Hillsdon, M.; Stamatakis, E. Associations of Specific Types of Sports and Exercise with All-Cause and Cardiovascular-Disease Mortality: A Cohort Study of 80 306 British Adults. Br. J. Sports Med. 2017, 51, 812–817. [Google Scholar] [CrossRef] [Green Version]
- Ryu, J.; Yang, H.; Kim, A.C.H.; Kim, K.M.; Heo, J. Understanding Pickleball as a New Leisure Pursuit among Older Adults. Educ. Gerontol. 2018, 44, 128–138. [Google Scholar] [CrossRef]
- Pelletier, C.A.; Pousette, A.; Ward, K.; Keahey, R.; Fox, G.; Allison, S.; Rasali, D.; Faulkner, G. Implementation of Physical Activity Interventions in Rural, Remote, and Northern Communities: A Scoping Review. INQUIRY 2020, 57, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.M.; Eyler, A.A.; Aaron Hipp, J.; King, A.C.; Tabak, R.G.; Yan, Y.; Reis, R.S.; Duncan, D.D.; Gilbert, A.S.; Serrano, N.H.; et al. A Multilevel Approach for Promoting Physical Activity in Rural Communities: A Cluster Randomized Controlled Trial. BMC Public Health 2019, 19, 126. [Google Scholar] [CrossRef] [PubMed]
- USDA ERS. Rural-Urban Continuum Codes. Available online: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx (accessed on 26 July 2021).
- OPCRH. County Classifications Map. Available online: https://ruralhealth.health.utah.gov/portal/county-classifications-map/ (accessed on 30 July 2021).
- OPCRH. HPSA Map. Available online: https://ruralhealth.health.utah.gov/portal/hpsa-map/ (accessed on 26 July 2021).
- Hart, L.G.; Larson, E.H.; Lishner, D.M. Rural Definitions for Health Policy and Research. Am. J. Public Health 2005, 95, 1149–1155. [Google Scholar] [CrossRef]
- Bhuiyan, N.; Singh, P.; Harden, S.M.; Mama, S.K. Rural Physical Activity Interventions in the United States: A Systematic Review and RE-AIM Evaluation. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 140. [Google Scholar] [CrossRef]
- Defining Rural Population. Available online: https://www.hrsa.gov/rural-health/about-us/definition/index.html (accessed on 26 July 2021).
- US Census Bureau American Community Survey (ACS). Available online: https://www.census.gov/programs-surveys/acs (accessed on 5 August 2021).
- US Census Bureau Census—Geography Profile. Available online: https://data.census.gov/cedsci/profile?g=0100000US (accessed on 5 August 2021).
- CDC. All About Adult BMI. Available online: https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html (accessed on 25 November 2020).
- Westcott, W.L. Resistance Training Is Medicine: Effects of Strength Training on Health. Curr. Sports Med. Rep. 2012, 11, 209–216. [Google Scholar] [CrossRef]
- Carson, R.G. Get a Grip: Individual Variations in Grip Strength Are a Marker of Brain Health. Neurobiol. Aging 2018, 71, 189–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thompson, B.J.; Whitson, M.; Sobolewski, E.J.; Stock, M.S. Effects of Age, Joint Angle, and Test Modality on Strength Production and Functional Outcomes. Int. J. Sports Med. 2018, 39, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Orssatto, L.B.R.; Bezerra, E.S.; Schoenfeld, B.J.; Diefenthaeler, F. Lean, Fast and Strong: Determinants of Functional Performance in the Elderly. Clin. Biomech. 2020, 78, 105073. [Google Scholar] [CrossRef]
- Singh, H.; Kim, D.; Kim, E.; Bemben, M.G.; Anderson, M.; Seo, D.-I.; Bemben, D.A. Jump Test Performance and Sarcopenia Status in Men and Women, 55 to 75 Years of Age. J. Geriatr. Phys. Ther. 2014, 37, 76–82. [Google Scholar] [CrossRef]
- Leard, J.S.; Cirillo, M.A.; Katsnelson, E.; Kimiatek, D.A.; Miller, T.W.; Trebincevic, K.; Garbalosa, J.C. Validity of two alternative systems for measuring vertical jump height. J. Strength Cond. Res. 2007, 21, 1296–1299. [Google Scholar]
- Lustig, C.; Shah, P.; Seidler, R.; Reuter-Lorenz, P.A. Aging, Training, and the Brain: A Review and Future Directions. Neuropsychol. Rev. 2009, 19, 504–522. [Google Scholar] [CrossRef] [Green Version]
- Dwolatzky, T.; Whitehead, V.; Doniger, G.M.; Simon, E.S.; Schweiger, A.; Jaffe, D.; Chertkow, H. Validity of a Novel Computerized Cognitive Battery for Mild Cognitive Impairment. BMC Geriatr. 2003, 3, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jensen, M. The Pain Stethoscope: A Clinician’s Guide to Measuring Pain; Springer Healthcare Communications: Houten, The Netherlands, 2011; ISBN 978-1-907673-22-1. [Google Scholar]
- CDC Injury Center. Drug Overdose Deaths | Drug Overdose. Available online: https://www.cdc.gov/drugoverdose/data/statedeaths.html (accessed on 17 December 2020).
- Hsieh, H.-F.; Shannon, S.E. Three Approaches to Qualitative Content Analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- NeuroTrax NeuroTrax—Innovative Science for Brain Health. Available online: https://www.neurotrax.com/ (accessed on 5 August 2021).
- Gajewski, J.; Michalski, R.; Buśko, K.; Mazur-Różycka, J.; Staniak, Z. Countermovement Depth – a Variable Which Clarifies the Relationship between the Maximum Power Output and Height of a Vertical Jump. Acta Bioeng. Biomech. 2018, 20, 127–134. [Google Scholar] [CrossRef]
- Caserotti, P.; Aagaard, P.; Simonsen, E.B.; Puggaard, L. Contraction-Specific Differences in Maximal Muscle Power during Stretch-Shortening Cycle Movements in Elderly Males and Females. Eur. J. Appl. Physiol. 2001, 84, 206–212. [Google Scholar] [CrossRef]
- Bean, J.F.; Kiely, D.K.; Herman, S.; Leveille, S.G.; Mizer, K.; Frontera, W.R.; Fielding, R.A. The Relationship Between Leg Power and Physical Performance in Mobility-Limited Older People. J. Am. Geriatr. Soc. 2002, 50, 461–467. [Google Scholar] [CrossRef]
- Sundstrup, E.; Jakobsen, M.D.; Andersen, L.L.; Andersen, T.R.; Randers, M.B.; Helge, J.W.; Suetta, C.; Schmidt, J.F.; Bangsbo, J.; Krustrup, P.; et al. Positive Effects of 1-Year Football and Strength Training on Mechanical Muscle Function and Functional Capacity in Elderly Men. Eur. J. Appl. Physiol. 2016, 116, 1127–1138. [Google Scholar] [CrossRef]
- Carey, J.R.; Bhatt, E.; Nagpal, A. Neuroplasticity Promoted by Task Complexity. Exerc. Sport Sci. Rev. 2005, 33, 24–31. [Google Scholar] [PubMed]
- Kroll, H.R. Exercise Therapy for Chronic Pain. Phys. Med. Rehabil. Clin. 2015, 26, 263–281. [Google Scholar] [CrossRef]
- Koltyn, K.F.; Arbogast, R.W. Perception of Pain after Resistance Exercise. Br. J. Sports Med. 1998, 32, 20–24. [Google Scholar] [CrossRef]
- DasGupta, D.; Madden, E.F.; Sulzer, S.; Light, T.; Chapoose, M.; Prevedel, S. The Urban/Rural Divide in Access to Medication-Assisted Treatment for Opioid Use Disorder in Utah. Curr. Publ. 2020, 1, 1–7. [Google Scholar]
- Kang, H.-W.; Park, M.; Wallace (Hernandez), J.P. The Impact of Perceived Social Support, Loneliness, and Physical Activity on Quality of Life in South Korean Older Adults. J. Sport Health Sci. 2018, 7, 237–244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, A.C.H.; Ryu, J.; Lee, C.; Kim, K.M.; Heo, J. Sport Participation and Happiness Among Older Adults: A Mediating Role of Social Capital. J. Happiness Stud. 2020, 22, 1623–1641. [Google Scholar] [CrossRef]
- Rogers, M.W.; Hedman, L.D.; Johnson, M.E.; Cain, T.D.; Hanke, T.A. Lateral Stability During Forward-Induced Stepping for Dynamic Balance Recovery in Young and Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M589–M594. [Google Scholar] [CrossRef]
- Kirk, E.P.; Jacobsen, D.J.; Gibson, C.; Hill, J.O.; Donnelly, J.E. Time Course for Changes in Aerobic Capacity and Body Composition in Overweight Men and Women in Response to Long-Term Exercise: The Midwest Exercise Trial (MET). Int. J. Obes. 2003, 27, 912–919. [Google Scholar] [CrossRef] [Green Version]
- Vitale, K.; Liu, S. Pickleball: Review and Clinical Recommendations for This Fast-Growing Sport. Curr. Sports Med. Rep. 2020, 19, 406–413. [Google Scholar] [CrossRef] [PubMed]
- Madden, E.F. Intervention Stigma: How Medication-Assisted Treatment Marginalizes Patients and Providers. Soc. Sci. Med. 2019, 232, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Bergen, G.; Stevens, M.R.; Burns, E.R. Falls and Fall Injuries Among Adults Aged ≥65 Years—United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 993–998. [Google Scholar] [CrossRef] [PubMed]
- Peeters, G.; van Schoor, N.M.; Cooper, R.; Tooth, L.; Kenny, R.A. Should Prevention of Falls Start Earlier? Co-Ordinated Analyses of Harmonised Data on Falls in Middle-Aged Adults across Four Population-Based Cohort Studies. PLoS ONE 2018, 13. [Google Scholar] [CrossRef] [Green Version]
- Maki, B.E.; McIlroy, W.E. The Role of Limb Movements in Maintaining Upright Stance: The “Change-in-Support” Strategy. Phys.Ther. 1997, 77, 488–507. [Google Scholar] [CrossRef] [PubMed]
| County | County Population | Study Site | Site Population and Demographics | Distance of Site from Urban Area (Miles) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Size | Density (per Square Mile) | Size | Density (per Square Mile) | 50–64 Years (%) | 65 Years and above (%) | 50 Years and above (%) | |||
| Beaver | 6517 | 2.50 | Beaver City | 3074 | 459 | 17.3 | 18.9 | 36.2 | 103.0 |
| Garfield | 4998 | 0.97 | Panguitch City | 1785 | 616 | 16.8 | 17.7 | 34.5 | 108.9 |
| San Juan | 15,302 | 1.96 | Monticello City | 2604 | 723 | 9.8 | 13.6 | 23.4 | 206.0 |
| Test | Global Cognitive Score | Memory | Executive Function | Attention | Information Processing Speed | Visual Spatial | Verbal Function | Motor Skills |
|---|---|---|---|---|---|---|---|---|
| Pre | 109.9 | 106.1 | 111.3 | 108.4 | 112.9 | 116.4 | 102.6 | 111.4 |
| Post | 111.8 | 108.8 | 110.9 | 108.7 | 118.5 | 118.4 | 105.1 | 112.4 |
| Outcome Measure | Pre-Test | Post-Test |
|---|---|---|
| Vertical Jump Height (cm) | 22.7 ± 5.2 | 25.3 ± 6.4 * |
| Grip Strength (kg) | 30.3 ± 7.0 | 29.5 ± 6.8 |
| Diastolic Blood Pressure (mm/Hg) | 87.5 ± 12.2 | 87.4 ± 7.3 |
| Systolic Blood Pressure (mm/Hg) | 134.9 ± 12.7 | 129.8 ± 12.8 |
| Resting Heart Rate (bpm) | 77.0 ± 15.6 | 75.7 ± 9.3 |
| Pain (median score 0–10) | 3 | 2 * |
| Interview Section | Themes |
|---|---|
| Positive aspects of intervention |
|
| Negative aspects of intervention |
|
| Suggestions for improvement of the intervention |
|
| Perceived benefits |
|
| Long-term adherence |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wray, P.; Ward, C.K.; Nelson, C.; Sulzer, S.H.; Dakin, C.J.; Thompson, B.J.; Vierimaa, M.; Das Gupta, D.; Bolton, D.A.E. Pickleball for Inactive Mid-Life and Older Adults in Rural Utah: A Feasibility Study. Int. J. Environ. Res. Public Health 2021, 18, 8374. https://doi.org/10.3390/ijerph18168374
Wray P, Ward CK, Nelson C, Sulzer SH, Dakin CJ, Thompson BJ, Vierimaa M, Das Gupta D, Bolton DAE. Pickleball for Inactive Mid-Life and Older Adults in Rural Utah: A Feasibility Study. International Journal of Environmental Research and Public Health. 2021; 18(16):8374. https://doi.org/10.3390/ijerph18168374
Chicago/Turabian StyleWray, Paige, Callahan K. Ward, Cindy Nelson, Sandra H. Sulzer, Christopher J. Dakin, Brennan J. Thompson, Matthew Vierimaa, Debasree Das Gupta, and David A. E. Bolton. 2021. "Pickleball for Inactive Mid-Life and Older Adults in Rural Utah: A Feasibility Study" International Journal of Environmental Research and Public Health 18, no. 16: 8374. https://doi.org/10.3390/ijerph18168374
APA StyleWray, P., Ward, C. K., Nelson, C., Sulzer, S. H., Dakin, C. J., Thompson, B. J., Vierimaa, M., Das Gupta, D., & Bolton, D. A. E. (2021). Pickleball for Inactive Mid-Life and Older Adults in Rural Utah: A Feasibility Study. International Journal of Environmental Research and Public Health, 18(16), 8374. https://doi.org/10.3390/ijerph18168374






