Association between Ambient Temperature and Severe Diarrhoea in the National Capital Region, Philippines
Abstract
:1. Introduction
2. Materials and Methods
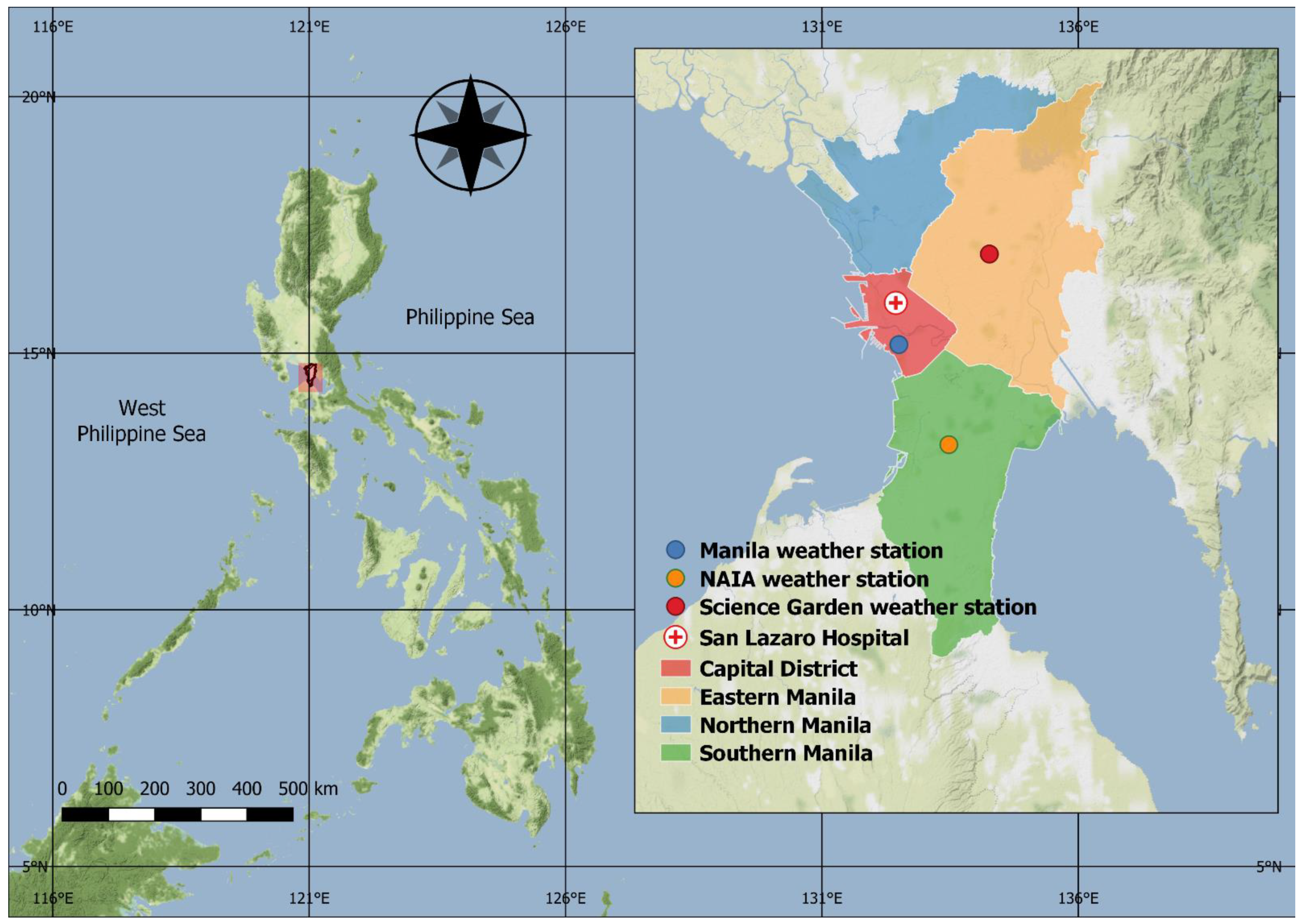
2.1. Study Site
2.2. Data Sources
2.3. Statistical Analysis
2.4. Sensitivity Analysis
2.5. Software
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Troeger, C.; Blacker, B.F.; Khalil, I.A.; Rao, P.C.; Cao, S.; Zimsen, S.R.; Albertson, S.B.; Stanaway, J.D.; Deshpande, A.; Abebe, Z.; et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018, 18, 1211–1228. [Google Scholar] [CrossRef] [Green Version]
- Levy, K.; Woster, A.P.; Goldstein, R.S.; Carlton, E.J. Untangling the Impacts of Climate Change on Waterborne Diseases: A Systematic Review of Relationships between Diarrheal Diseases and Temperature, Rainfall, Flooding, and Drought. Environ. Sci. Technol. 2016, 50, 4905–4922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carlton, E.J.; Woster, A.P.; DeWitt, P.; Goldstein, R.S.; Levy, K. A systematic review and meta-analysis of ambient temperature and diarrhoeal diseases. Int. J. Epidemiol. 2015, 45, 117–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petri, W.A.; Miller, M.; Binder, H.J.; Levine, M.M.; Dillingham, R.; Guerrant, R.L. Enteric infections, diarrhea, and their impact on function and development. J. Clin. Investig. 2008, 118, 1277–1290. [Google Scholar] [CrossRef] [PubMed]
- Akech, S.; Ayieko, P.; Gathara, D.; Agweyu, A.; Irimu, G.; Stepniewska, K.; English, M.; Ngarngar, S.; Aduro, N.; Mutai, L.; et al. Risk factors for mortality and effect of correct fluid prescription in children with diarrhoea and dehydration without severe acute malnutrition admitted to Kenyan hospitals: An observational, association study. Lancet Child Adolesc. Health 2018, 2, 516–524. [Google Scholar] [CrossRef]
- Levine, M.M.; Nasrin, D.; Acácio, S.; Bassat, Q.; Powell, H.; Tennant, S.M.; Sow, S.O.; Sur, D.; Zaidi, A.K.M.; Faruque, A.S.G.; et al. Diarrhoeal disease and subsequent risk of death in infants and children residing in low-income and middle-income countries: Analysis of the GEMS case-control study and 12-month GEMS-1A follow-on study. Lancet Glob. Health 2020, 8, e204–e214. [Google Scholar] [CrossRef] [Green Version]
- Lin, S.; Sun, M.; Fitzgerald, E.; Hwang, S.-A. Did summer weather factors affect gastrointestinal infection hospitalizations in New York State? Sci. Total Environ. 2016, 550, 38–44. [Google Scholar] [CrossRef]
- Morral-Puigmal, C.; Martínez-Solanas, È.; Villanueva, C.M.; Basagaña, X. Weather and gastrointestinal disease in Spain: A retrospective time series regression study. Environ. Int. 2018, 121, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Ekamper, P.; Van Poppel, F.; Van Duin, C.; Garssen, J. 150 Years of temperature-related excess mortality in the Netherlands. Demogr. Res. 2009, 21, 385–426. [Google Scholar] [CrossRef] [Green Version]
- Alonso, W.J.; Acuna-Soto, R.; Giglio, R.; Nuckols, J.; Leyk, S.; Schuck-Paim, C.; Viboud, C.; Miller, M.A.; McCormick, B.J.J. Spatio-temporal patterns of diarrhoeal mortality in Mexico. Epidemiol. Infect. 2011, 140, 91–99. [Google Scholar] [CrossRef] [Green Version]
- PSA Philippine Population Density (Based on the 2015 Census of Population). Available online: https://psa.gov.ph/content/philippine-population-density-based-2015-census-population (accessed on 1 January 2021).
- Philippine Statistics Authority Updated 2015 and 2018 Full Year Official Poverty Statistics. Available online: https://psa.gov.ph/poverty-press-releases/nid/162559 (accessed on 1 January 2021).
- Cruz, F.A.; Tibig, L.; Villarin, J.R.; de Guzman, R.; Cinco, T.; Narisma, G.T.; Hilario, F. The Philippine Climate. In 2016 Philippine Climate Change Assessment (PhilCCA): The Physical Science Basis; Villarin, J.R.T., Algo, J.L.C., Cinco, T.A., Cruz, F.A.T., de Guzman, R.G., Hilario, F.D., Narisma, G.T.T., Ortiz, A.M.D., Siringan, F.P., Tibig, L.V., Eds.; The Oscar M. Lopez Center for Climate Change Adaptation and Disaster Risk Management Foundation Inc. and Climate Change Commission: Pasig, Philippines, 2016; pp. 18–28. [Google Scholar]
- Philippine Atmospheric, Geophysical and Astronomical Services Administration. Climate Change in the Philippines; Philippine Atmospheric, Geophysical and Astronomical Services Administration: Quezon City, Philippines, 2011.
- National Oceanic and Atmospheric Administration—National Centers for Environmental Information Global Historical Climatology Network Daily—Data Access. Available online: https://www.ncdc.noaa.gov/ghcnd-data-access (accessed on 1 January 2021).
- Afrifa-Yamoah, E.; Mueller, U.A.; Taylor, S.M.; Fisher, A.J. Missing data imputation of high-resolution temporal climate time series data. Meteorol. Appl. 2019, 27. [Google Scholar] [CrossRef]
- Gasparrini, A. Distributed Lag Linear and Non-Linear Models inR: The Packagedlnm. J. Stat. Softw. 2011, 43, 1–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Z.; Tong, M.X.; Xiang, J.; Dear, K.; Wang, C.; Ma, W.; Lu, L.; Liu, Q.; Jiang, B.; Bi, P. Daily Temperature and Bacillary Dysentery: Estimated Effects, Attributable Risks, and Future Disease Burden in 316 Chinese Cities. Environ. Health Perspect. 2020, 128, 057008. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y.; Liao, W.; Ma, W.; Zhang, J.; Zhang, N.; Zhong, S.; Wang, Z.; Yang, L.; Huang, C. Effects of ambient temperature on bacillary dysentery: A multi-city analysis in Anhui Province, China. Sci. Total Environ. 2019, 671, 1206–1213. [Google Scholar] [CrossRef] [PubMed]
- Onozuka, D.; Gasparrini, A.; Sera, F.; Hashizume, M.; Honda, Y. Modeling Future Projections of Temperature-Related Excess Morbidity due to Infectious Gastroenteritis under Climate Change Conditions in Japan. Environ. Health Perspect. 2019, 127, 077006. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat. Med. 2012, 31, 3821–3839. [Google Scholar] [CrossRef] [Green Version]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobías, A.; Tong, S.; Rocklöv, J.; Forsberg, B.; et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Xiao, X.; Gasparrini, A.; Huang, J.; Liao, Q.; Liu, F.; Yin, F.; Yu, H.; Li, X. The exposure-response relationship between temperature and childhood hand, foot and mouth disease: A multicity study from mainland China. Environ. Int. 2017, 100, 102–109. [Google Scholar] [CrossRef]
- Kotloff, K.L.; Nataro, J.P.; Blackwelder, W.C.; Nasrin, D.; Farag, T.H.; Panchalingam, S.; Wu, Y.; Sow, S.O.; Sur, D.; Breiman, R.F.; et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): A prospective, case-control study. Lancet 2013, 382, 209–222. [Google Scholar] [CrossRef]
- Sera, F.; Armstrong, B.; Blangiardo, M.; Gasparrini, A. An extended mixed-effects framework for meta-analysis. Stat. Med. 2019, 38, 5429–5444. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Chua, P.L.C.; Fook, C.; Ng, S.; Tobias, A.; Seposo, X.T.; Hashizume, M. Associations between Ambient Temperature and Enteric Infections by Aetiology: A Systematic Review and Meta-Analysis. SSRN 2020, 1–28. [Google Scholar] [CrossRef]
- Adkins, H.J.; Escamilla, J.; Santiago, L.T.; Rañoa, C.; Echeverria, P.; Cross, J.H. Two-year survey of etiologic agents of diarrheal disease at San Lazaro Hospital, Manila, Republic of the Philippines. J. Clin. Microbiol. 1987, 25, 1143–1147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Operario, D.J.; Platts-Mills, J.A.; Nadan, S.; Page, N.; Seheri, L.M.; Mphahlele, J.; Praharaj, I.; Kang, G.; Araujo, I.T.; Leite, J.P.G.; et al. Etiology of Severe Acute Watery Diarrhea in Children in the Global Rotavirus Surveillance Network Using Quantitative Polymerase Chain Reaction. J. Infect. Dis. 2017, 216, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Kotloff, K.L.; Nasrin, D.; Blackwelder, W.C.; Wu, Y.; Farag, T.; Panchalingham, S.; Sow, S.O.; Sur, D.; Zaidi, A.K.M.; Faruque, A.S.G.; et al. The incidence, aetiology, and adverse clinical consequences of less severe diarrhoeal episodes among infants and children residing in low-income and middle-income countries: A 12-month case-control study as a follow-on to the Global Enteric Multicenter Study (GEMS). Lancet Glob. Health 2019, 7, e568–e584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dewan, A.M.; Corner, R.; Hashizume, M.; Ongee, E.T. Typhoid Fever and Its Association with Environmental Factors in the Dhaka Metropolitan Area of Bangladesh: A Spatial and Time-Series Approach. PLoS Negl. Trop. Dis. 2013, 7, e1998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thindwa, D.; Chipeta, M.G.; Henrion, M.Y.R.; Gordon, M.A. Distinct climate influences on the risk of typhoid compared to invasive non-typhoid Salmonella disease in Blantyre, Malawi. Sci. Rep. 2019, 9, 20310. [Google Scholar] [CrossRef] [Green Version]
- Erdem, H.; Kiliç, S.; Çinar, E.; Pahsa, A. Symptomatic Intestinal Amoebiasis and Climatic Parameters. Scand. J. Infect. Dis. 2003, 35, 186–188. [Google Scholar] [PubMed]
- Zavala, G.A.; Van Dulm, E.; Doak, C.M.; García, O.P.; Polman, K.; Campos-Ponce, M. Ascariasis, Amebiasis and Giardiasis in Mexican children: Distribution and geographical, environmental and socioeconomic risk factors. J. Parasit. Dis. 2020, 44, 829–836. [Google Scholar] [CrossRef]
- Popkin, B.M.; D’Anci, K.E.; Rosenberg, I.H. Water, Hydration, and Health. Nutr. Rev. 2010, 68, 439–458. [Google Scholar] [CrossRef]
- Kovats, R.S.; Hajat, S. Heat Stress and Public Health: A Critical Review. Annu. Rev. Public Health 2008, 29, 41–55. [Google Scholar] [CrossRef]
- Grenov, B.; Lanyero, B.; Nabukeera-Barungi, N.; Namusoke, H.; Ritz, C.; Friis, H.; Michaelsen, K.F.; Mølgaard, C. Diarrhea, Dehydration, and the Associated Mortality in Children with Complicated Severe Acute Malnutrition: A Prospective Cohort Study in Uganda. J. Pediatr. 2019, 210, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Chisti, M.J.; Duke, T.; Robertson, C.F.; Ahmed, T.; Faruque, A.S.G.; Bardhan, P.K.; La Vincente, S.; Salam, M.A. Co-morbidity: Exploring the clinical overlap between pneumonia and diarrhoea in a hospital in Dhaka, Bangladesh. Ann. Trop. Paediatr. 2011, 31, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Ugboko, H.U.; Nwinyi, O.C.; Oranusi, S.U.; Oyewale, J.O. Childhood diarrhoeal diseases in developing countries. Heliyon 2020, 6, e03690. [Google Scholar] [CrossRef]
- Miller, R.R.; Montoya, V.; Gardy, J.L.; Patrick, D.M.; Tang, P. Metagenomics for pathogen detection in public health. Genome Med. 2013, 5, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carter, K.L.; Williams, G.; Tallo, V.; Sanvictores, D.; Madera, H.; Riley, I. Capture-recapture analysis of all-cause mortality data in Bohol, Philippines. Popul. Health Metr. 2011, 9, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lucero, M.; Riley, I.D.; Hazard, R.H.; Sanvictores, D.; Tallo, V.; Dumaluan, D.G.M.; Ugpo, J.M.; Lopez, A.D. Assessing the quality of medical death certification: A case study of concordance between national statistics and results from a medical record review in a regional hospital in the Philippines. Popul. Health Metr. 2018, 16, 23. [Google Scholar] [CrossRef]
- Fan, X.; Duan, Q.; Shen, C.; Wu, Y.; Xing, C. Global surface air temperatures in CMIP6: Historical performance and future changes. Environ. Res. Lett. 2020, 15, 104056. [Google Scholar] [CrossRef]
- Li, X.-X. Heat wave trends in Southeast Asia during 1979–2018: The impact of humidity. Sci. Total Environ. 2020, 721, 137664. [Google Scholar] [CrossRef]
- Troeger, C.E.; Khalil, I.A.; Blacker, B.F.; Biehl, M.H.; Albertson, S.B.; Zimsen, S.R.M.; Rao, P.C.; Abate, D.; Ahmadi, A.; Ahmed, M.L.C.B.; et al. Quantifying Risks and Interventions That Have Affected the Burden of Diarrhoea among Children Younger than 5 Years: An Analysis of the Global Burden of Disease Study 2017. Lancet Infect. Dis. 2020, 20, 37–59. [Google Scholar] [CrossRef] [Green Version]
| Location | Weekly Mean Values (Range: Minimum, Maximum) | |||
|---|---|---|---|---|
| Diarrhoeal Deaths | Hospitalised Severe Diarrhoea Cases * | Mean Temperature (°C) | Dew Point Temperature (°C) | |
| Capital District | 1.9 (0, 10) | 6.1 (0, 32) | 28.5 (24.5, 31.8) | 23.6 (17.8, 26.4) |
| Eastern Manila District | 3.2 (0, 17) | 1.4 (0, 22) | 27.4 (23.3, 31.3) | 23.1 (18.2, 25.7) |
| Southern Manila District | 3.2 (0, 10) | 0.9 (0, 12) | 28.1 (24.2, 31.8) | 23.9 (17.4, 27.4) |
| National Capital Region ** | 8.3 (0, 37) | 9.1 (0, 50) | 28.0 (24.1, 31.6) | 23.5 (17.8, 26.2) |
| Location | Temperatures (°C) | Mortality | Hospitalised Severe Diarrhoea | |||||
|---|---|---|---|---|---|---|---|---|
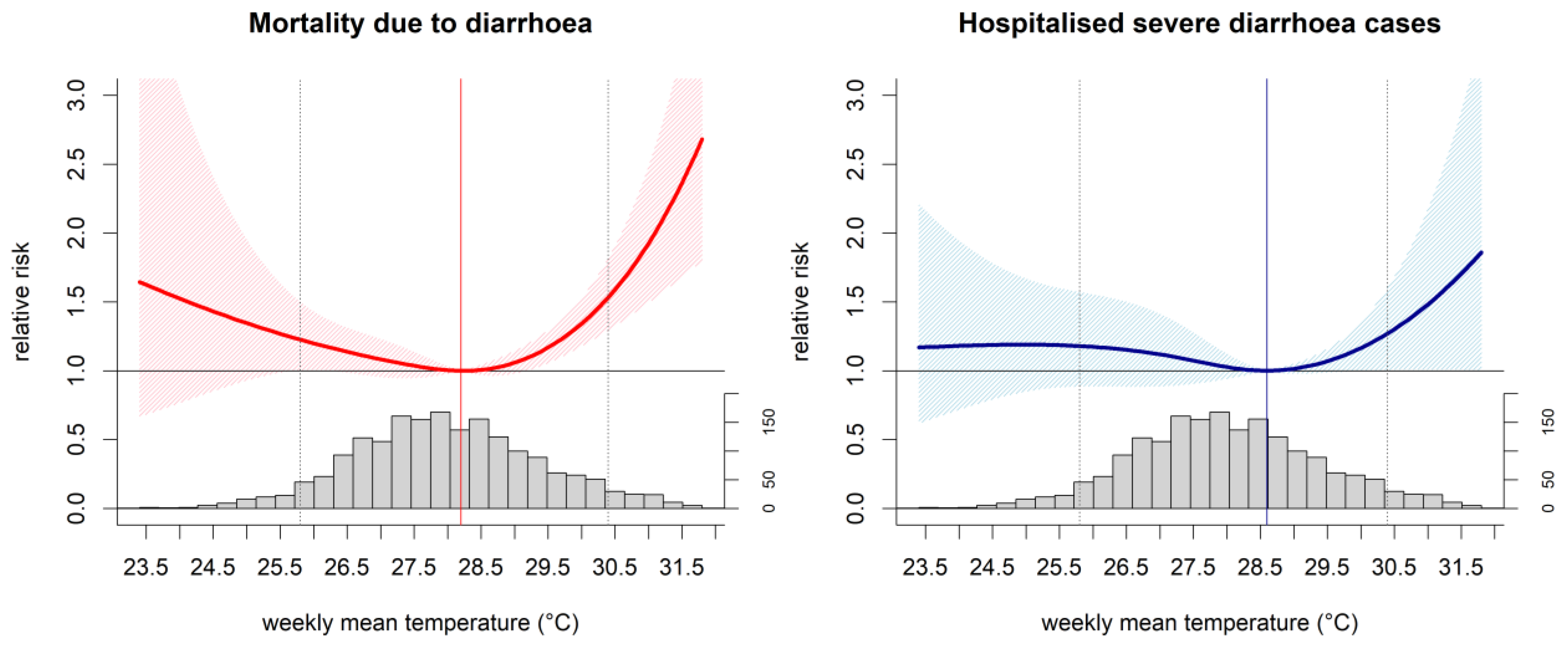
| 95% Pctl | 5% Pctl | MRT (°C) | RRs (95% CI) for HT | RRs (95% CI) for LT | MRT (°C) | RRs (95% CI) for HT | RRs (95% CI) for LT | |
| Capital District | 30.6 | 26.4 | 28.9 | 1.540 (1.303; 1.820) | 1.139 (0.859; 1.511) | 29.0 | 1.267 (0.979; 1.640) | 1.166 (0.831; 1.637) |
| Eastern Manila District | 29.8 | 25.2 | 27.5 | 1.504 (1.261; 1.794) | 1.342 (0.981; 1.836) | 28.2 | 1.284 (1.014; 1.625) | 1.263 (0.870; 1.833) |
| Southern Manila District | 30.6 | 26.1 | 28.2 | 1.646 (1.351; 2.005) | 1.319 (1.004; 1.735) | 28.6 | 1.270 (0.937; 1.722) | 1.113 (0.784; 1.581) |
| National Capital Region | 30.4 | 25.8 | 28.2 | 1.533 (1.294; 1.817) | 1.226 (1.004; 1.496) | 28.6 | 1.271 (1.007; 1.604) | 1.179 (0.886; 1.57) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chua, P.L.C.; Ng, C.F.S.; Rivera, A.S.; Salva, E.P.; Salazar, M.A.; Huber, V.; Hashizume, M. Association between Ambient Temperature and Severe Diarrhoea in the National Capital Region, Philippines. Int. J. Environ. Res. Public Health 2021, 18, 8191. https://doi.org/10.3390/ijerph18158191
Chua PLC, Ng CFS, Rivera AS, Salva EP, Salazar MA, Huber V, Hashizume M. Association between Ambient Temperature and Severe Diarrhoea in the National Capital Region, Philippines. International Journal of Environmental Research and Public Health. 2021; 18(15):8191. https://doi.org/10.3390/ijerph18158191
Chicago/Turabian StyleChua, Paul L. C., Chris Fook Sheng Ng, Adovich S. Rivera, Eumelia P. Salva, Miguel Antonio Salazar, Veronika Huber, and Masahiro Hashizume. 2021. "Association between Ambient Temperature and Severe Diarrhoea in the National Capital Region, Philippines" International Journal of Environmental Research and Public Health 18, no. 15: 8191. https://doi.org/10.3390/ijerph18158191
APA StyleChua, P. L. C., Ng, C. F. S., Rivera, A. S., Salva, E. P., Salazar, M. A., Huber, V., & Hashizume, M. (2021). Association between Ambient Temperature and Severe Diarrhoea in the National Capital Region, Philippines. International Journal of Environmental Research and Public Health, 18(15), 8191. https://doi.org/10.3390/ijerph18158191






