Cancer Healthcare Workers’ Perceptions toward Psychedelic-Assisted Therapy: A Preliminary Investigation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Researcher Declaration
2.2. Participants
2.3. Study Procedure
2.4. Data Analysis
3. Results
“Yeah, I know a lot … in the last palliative care conference there were excellent presentations … they work with LSD in palliative care, it’s fascinating, and has been shoved under the carpet because of the Vietnam war and I don’t really know the whole history … could talk for hours about that”.[Doctor, 12]
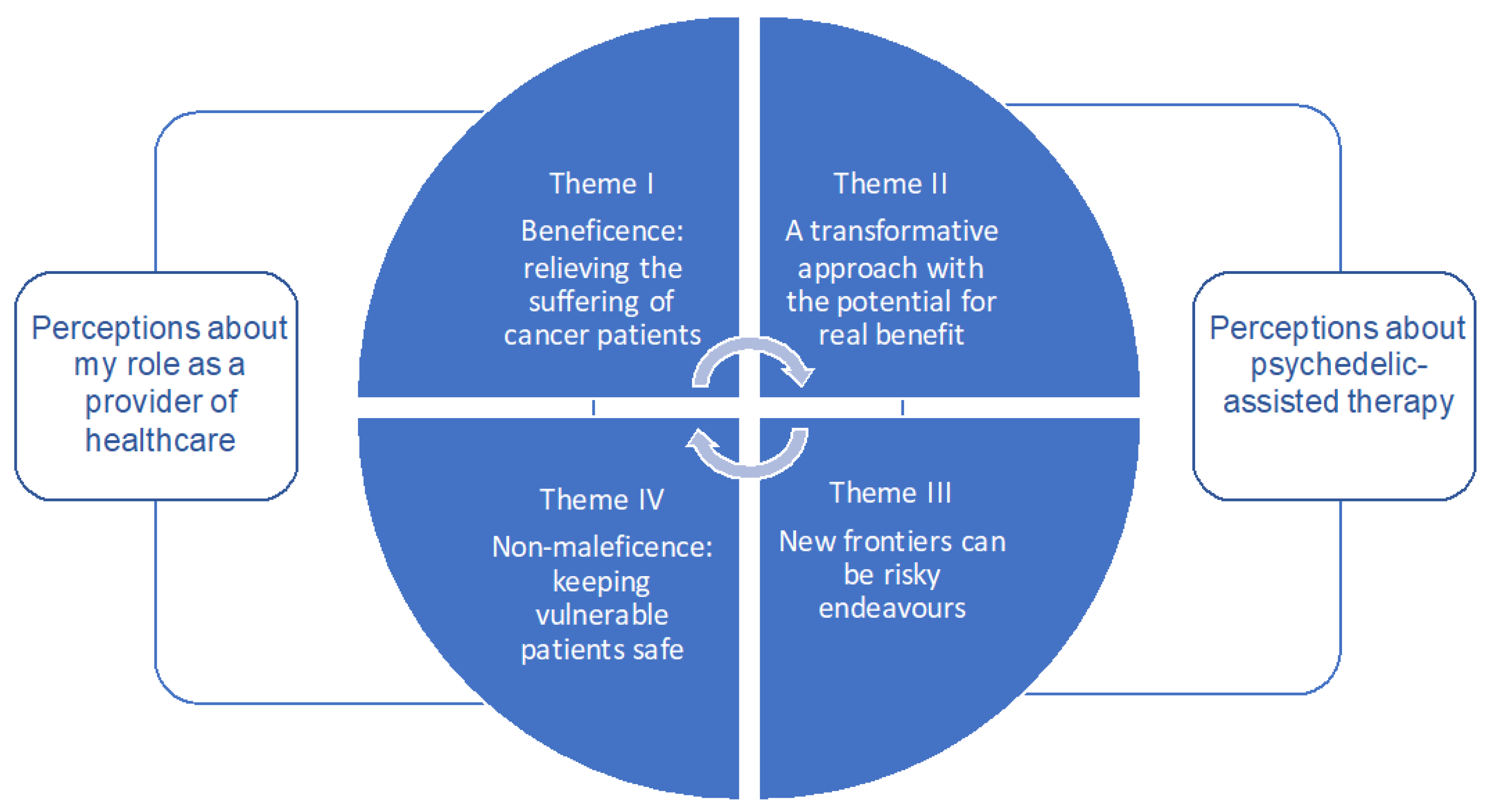
3.1. Key Themes
3.1.1. Theme I: Beneficence—A Need to Alleviate Suffering
“There are people that I see that aren’t coping well” and “I think there is a lot of avoidance and they try to avoid the emotions that they are feeling and I guess live in denial. So I think it definitely probably increases stress, more avoidance, more anxiety among those patients which is really difficult, because I think when it is advanced cancer you want them to be able to live the rest of their days the best that they can … at the end of the day advanced cancer patients are in a really difficult situation”.[Psychologist, 6]
“I think probably, there is a big unmet need … I think that often we, because it is easier, we focus on our job of discussing treatment, and obviously we are aware of how distressed people are, but we aren’t always able to address it appropriately”.[Doctor, #2]
“It can be really difficult. I think, you know, as a health professional you want to be compassionate, you want to alleviate someone’s suffering, and so you feel bad that you can’t get them out of that situation … It can be really difficult knowing that even though someone has got such a short time to live they’re still suffering. It is really difficult”.[Doctor, #2]
“There are people that I see that aren’t coping well and I think that something like that, if it was going to increase their ability to be open and, I think, alleviate some of the anxiety and depression so that they can engage in a life that they want to for the rest of their lifetime that they have, then I think that they would be willing to consider it”.[Psychologist, #6]
“When you have advanced cancer you are willing to do anything to improve your life, and so I think in one way you know it’s not curing the cancer, but it does give some people hope that they will be able to live a better life throughout those months”.[Social Worker, #5]
3.1.2. Theme II: A Transformative Approach with the Potential for Real Benefit
“Something which society, or the powers that be, have deemed as illicit and not good for humans could potentially be slightly altered and given to people in an appropriate dose to make their health or whatever better … that’s part of science, you kind of have to push the boat out a bit … that’s what research is for”.[Doctor, #9]
“I think that there is a whole branch of psycho-pharmacology that’s been latent for 50 years and it’s just scientifically interesting, where could it lead, what could it mean? … that interests me as a scientist. It might not work, it might turn out to be too toxic, but it’s there waiting to be investigated and I think the investigations have been shut down for the wrong reasons”.[Doctor, #12]
“The idea of patients feeling like they need to process … their existential concerns, in terms of what has my life meant … what happens from here … what do I believe in … do I die and that’s it, the end of me. So … I guess in that sense, an experience like this would open their mindset enough to maybe explore some of those existential ideas that typically comfort patients when they have advanced cancer”.[Psychologist, #4]
“Ibogaine, ayahuasca, mescaline have got a fairly long traditional history … so, there’s a large volume of traditional knowledge … I think that the ones that have got the history are also in the bed with the large body of traditional and indigenous knowledge, and so they intersect with quite different worlds or world views of understanding”.[Doctor, #12]
“I worry about such research that it trivialises the spiritual dimensions of stuff like this … one thing that pops out at the start is worries about cultural appropriation … because we don’t really understand the compound … it’s just the leaping off point for a whole cultural understanding, which you can’t really separate from the compounds”.[Doctor, #12]
3.1.3. Theme III: New Frontiers Can Be Risky
“I think with substances that are illegal, they are not evidence-based, and I think that if something’s not evidence-based then it’s not good to consume it …”[Psychologist, #6]
“It’s portrayed as something that is used for fun, rather than for medicinal use and I guess, if I was to think about it in a medical context, rather than in a fun context, that seems to jar—like things that you do for fun aren’t often things that are prescribed”.[Psychologist, #4]
“The feeling that I have is similar to the feelings that I have about high voltage electricity, it’s really important … and potentially very powerful for all the things that we do … and you have to be very careful around it”.[Doctor, #12]
3.1.4. Theme IV: Non-Maleficence—Keeping Vulnerable Patients Safe
“We’re talking about … a vulnerable population or people that are at risk. So, I’m yeah—that is my concern—I mean perhaps there has to be more research with people who don’t have cancer before advancing to people that do have cancer”.[Doctor, #12]
“They are just another drug, so as long as there is rigorous testing like there is with all of the drugs that people are being given now, if there is evidence to support, I personally wouldn’t have a problem with it”.[Social worker, #3]
“You’ve got to have a good template for understanding the toxicity, that’s the way we develop cancer drugs—with the first step is understanding, it’s understanding the toxicity of the medicine. So, you know that’s why we’ve got Phase One studies to learn what the limits are on dosing, what the dosing toxicities are, and the sort of things that can go wrong. This is all very well parameterized, protocolised, in how you develop medicines”.[Doctor, #12]
“The idea of micro-dosing, so very small doses which I take to mean doesn’t necessarily induce all of those psychedelic effects that a full dose would…but then I guess the question is what’s the point in this micro-dose?”[Psychologist, #4]
4. Discussion
4.1. The Responsibility of Healthcare Workers: Beneficence and Non-Maleficence
4.2. Perceptions about Psychedelic-Assisted Therapy: A Transformative Approach That Is High Risk/High Reward
4.3. Study Limitations and Research Agenda
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- O’Connor, M.; White, K.; Kristjanson, L.L.J.; Cousins, K.; Wilkes, L. The prevalence of anxiety and depression in palliative care patients with cancer in Western Australia and New South Wales. Med. J. Aust. 2010, 193, S44–S47. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.E.M.; Gomm, S.A.; Dickens, C.M.C. Assessing the independent contribution to quality of life from anxiety and depression in patients with advanced cancer. Palliat. Med. 2003, 17, 509–513. [Google Scholar] [CrossRef]
- Boston, P.; Bruce, A.; Schreiber, R. Existential suffering in the palliative care setting: An integrated literature review. J. Pain Symptom Manag. 2011, 41, 604–618. [Google Scholar] [CrossRef]
- Kissane, D. Psychospiritual and existential distress. The challenge for palliative care. Aust. Fam. Physician 2000, 29, 1022–1025. [Google Scholar] [PubMed]
- Donovan, K.A.; Thompson, L.M.A.; Jacobsen, P.B. Pain, depression, and anxiety in cancer. In Handbook of Pain and Palliative Care; Springer: New York, NY, USA, 2013; pp. 615–637. [Google Scholar]
- Arrieta, Ó.; Angulo, L.P.; Núñez-Valencia, C.; Dorantes-Gallareta, Y.; Macedo, E.O.; Martínez-López, D.; Alvarado, S.; Corona-Cruz, J.-F.; Oñate-Ocaña, L.F. Association of depression and anxiety on quality of life, treatment adherence, and prognosis in patients with advanced non-small cell lung cancer. Ann. Surg. Oncol. 2012, 20, 1941–1948. [Google Scholar] [CrossRef]
- Prieto, J.M.; Blanch, J.; Atala, J.; Carreras, E.; Rovira, M.; Cirera, E.; Gastó, C. Psychiatric morbidity and impact on hospital length of stay among hematologic cancer patients receiving stem-cell transplantation. J. Clin. Oncol. 2002, 20, 1907–1917. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M.; Duberstein, R.P. Depression and cancer mortality: A meta-analysis. Psychol. Med. 2010, 40, 1797. [Google Scholar] [CrossRef] [PubMed]
- Ross, S. Therapeutic use of classic psychedelics to treat cancer-related psychiatric distress. Int. Rev. Psychiatry 2018, 30, 317–330. [Google Scholar] [CrossRef]
- Grassi, L.; Caruso, R.; Hammelef, K.; Nanni, M.G.; Riba, M. Efficacy and safety of pharmacotherapy in cancer-related psychiatric disorders across the trajectory of cancer care: A review. Int. Rev. Psychiatry 2014, 26, 44–62. [Google Scholar] [CrossRef]
- Iovieno, N.; Tedeschini, E.; Ameral, V.E.; Rigatelli, M.; Papakostas, G.I. Antidepressants for major depressive disorder in patients with a co-morbid axis-III disorder. Int. Clin. Psychopharmacol. 2011, 26, 69–74. [Google Scholar] [CrossRef]
- Laoutidis, Z.G.; Mathiak, K. Antidepressants in the treatment of depression/depressive symptoms in cancer patients: A systematic review and meta-analysis. BMC Psychiatry 2013, 13, 140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ostuzzi, G.; Matcham, F.; Dauchy, S.; Barbui, C.; Hotopf, M. Antidepressants for the treatment of depression in people with cancer. Cochrane Database Syst. Rev. 2018, 4, 1–74. [Google Scholar] [CrossRef] [PubMed]
- Eakin, E.G.; Strycker, L.A. Awareness and barriers to use of cancer support and information resources by HMO patients with breast, prostate, or colon cancer: Patient and provider perspectives. Psychooncology 2001, 10, 103–113. [Google Scholar] [CrossRef]
- Lepore, S.J.; Coyne, J.C. Psychological interventions for distress in cancer patients: A review of reviews. Ann. Behav. Med. 2006, 32, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Kamenov, K.; Twomey, C.; Cabello, M.; Prina, A.M.; Ayuso-Mateos, J.L. The efficacy of psychotherapy, pharmacotherapy and their combination on functioning and quality of life in depression: A meta-analysis. Psychol. Med. 2016, 47, 414–425. [Google Scholar] [CrossRef] [Green Version]
- Greenway, K.T.; Garel, N.; Jerome, L.; Feduccia, A.A. Integrating psychotherapy and psychopharmacology: Psychedelic-assisted psychotherapy and other combined treatments. Expert Rev. Clin. Pharmacol. 2020, 13, 655–670. [Google Scholar] [CrossRef] [PubMed]
- Andersen, K.A.A.; Carhart-Harris, R.; Nutt, D.J.; Erritzoe, D. Therapeutic effects of classic serotonergic psychedelics: A systematic review of modern-era clinical studies. Acta Psychiatr. Scand. 2021, 143, 101–118. [Google Scholar] [CrossRef] [PubMed]
- Ly, C.; Greb, A.C.; Cameron, L.P.; Wong, J.M.; Barragan, E.V.; Wilson, P.C.; Burbach, K.F.; Zarandi, S.S.; Sood, A.; Paddy, M.R.; et al. Psychedelics promote structural and functional neural plasticity. Cell Rep. 2018, 23, 3170–3182. [Google Scholar] [CrossRef]
- Hutten, N.R.P.W.; Mason, N.L.; Dolder, P.C.; Theunissen, E.L.; Holze, F.; Liechti, M.E.; Varghese, N.; Eckert, A.; Feilding, A.; Ramaekers, J.G.; et al. Low Doses of LSD Acutely Increase BDNF Blood Plasma Levels in Healthy Volunteers. ACS Pharmacol. Transl. Sci. 2021, 4, 461–466. [Google Scholar] [CrossRef]
- D’Sa, C.; Duman, R.S. Antidepressants and neuroplasticity. Bipolar Disord. 2002, 4, 183–194. [Google Scholar] [CrossRef]
- Grinspoon, L.; Doblin, R. Psychedelics as catalysts of insight-oriented psychotherapy. Soc. Res. 2001, 68, 677–695. [Google Scholar]
- Carhart-Harris, R.L.; Kaelen, M.; Whalley, M.G.; Bolstridge, M.; Feilding, A.; Nutt, D.J. LSD enhances suggestibility in healthy volunteers. Psychopharmacology 2015, 232, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Hartogsohn, I. The meaning-enhancing properties of psychedelics and their mediator role in psychedelic therapy, spirituality, and creativity. Front. Neurosci. 2018, 12, 129. [Google Scholar] [CrossRef]
- Grof, S.; Goodman, L.E.; Richards, W.A.; Kurland, A.A. LSD assisted psychotherapy in patients with terminal cancer. Int. Pharm. 1973, 8, 129–144. [Google Scholar] [CrossRef]
- Richards, W.A.; Rhead, J.C.; Dileo, F.B.; Yensen, R.; Kurland, A.A. The peak experience variable in DPT-assisted psychotherapy with cancer patients. J. Psychoact. Drugs 1977, 9, 1–10. [Google Scholar] [CrossRef]
- Kast, E. Attenuation of anticipation: A therapeutic use of lysergic acid diethylamide. Psychiatr. Q. 1967, 41, 646–657. [Google Scholar] [CrossRef] [PubMed]
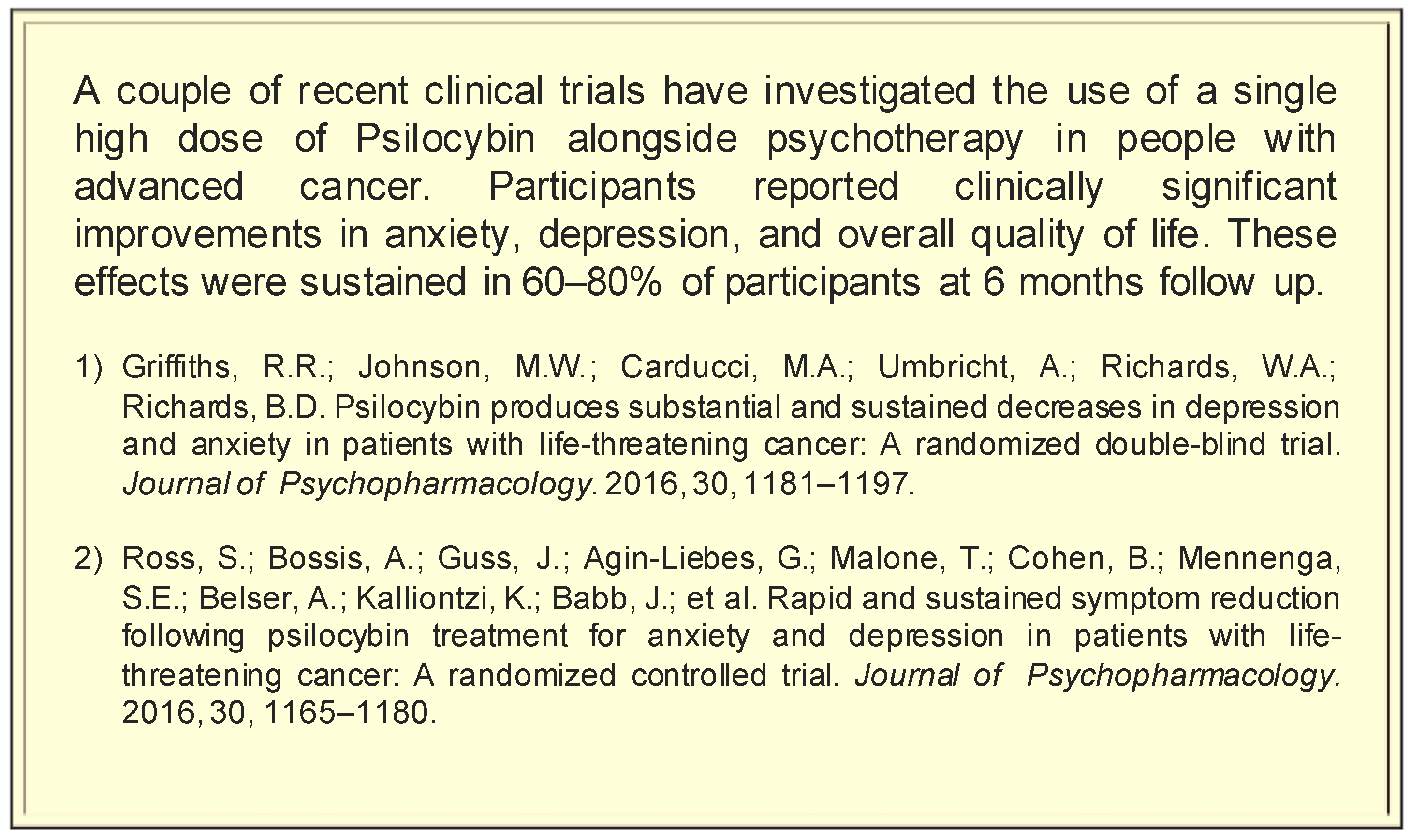
- Griffiths, R.R.; Johnson, M.W.; Carducci, M.A.; Umbricht, A.; Richards, W.A.; Richards, B.D.; Cosimano, M.P.; Klinedinst, M.A. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial. J. Psychopharmacol. 2016, 30, 1181–1197. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.; Bossis, A.; Guss, J.; Agin-Liebes, G.; Malone, T.; Cohen, B.; Mennenga, S.E.; Belser, A.; Kalliontzi, K.; Babb, J.; et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: A randomized controlled trial. J. Psychopharmacol. 2016, 30, 1165–1180. [Google Scholar] [CrossRef] [Green Version]
- Grob, C.S.; Danforth, A.L.; Chopra, G.S.; Hagerty, M.; McKay, C.R.; Halberstadt, A.L.; Greer, G.R. Pilot study of psilocybin treatment for anxiety in patients with advanced-stage cancer. Arch. Gen. Psychiatry 2011, 68, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Swift, T.C.; Belser, A.B.; Agin-Liebes, G.; Devenot, N.; Terrana, S.; Friedman, H.L.; Guss, J.; Bossis, A.P.; Ross, S. Cancer at the dinner table: Experiences of Psilocybin-Assisted Psychotherapy for the treatment of cancer-related distress. J. Humanist. Psychol. 2017, 57, 488–519. [Google Scholar] [CrossRef] [Green Version]
- Johnson, M.W.; Richards, W.A.; Griffiths, R.R. Human hallucinogen research: Guidelines for safety. J. Psychopharmacol. 2008, 22, 603–620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Studerus, E.; Kometer, M.; Hasler, F.; Vollenweider, F.X. Acute, subacute and long-term subjective effects of psilocybin in healthy humans: A pooled analysis of experimental studies. J. Psychopharmacol. 2011, 25, 1434–1452. [Google Scholar] [CrossRef]
- Family, N.; Maillet, E.L.; Williams, L.T.J.; Krediet, E.; Carhart-Harris, R.L.; Williams, T.M.; Nichols, C.D.; Goble, D.J.; Raz, S. Safety, tolerability, pharmacokinetics, and pharmacodynamics of low dose lysergic acid diethylamide (LSD) in healthy older volunteers. Psychopharmacology 2020, 237, 841–853. [Google Scholar] [CrossRef] [Green Version]
- Beaussant, Y.; Sanders, J.; Sager, Z.; Tulsky, J.A.; Braun, I.M.; Blinderman, C.D.; Bossis, A.P.; Byock, I. Defining the roles and research priorities for Psychedelic-Assisted Therapies in patients with serious illness: Expert clinicians’ and investigators’ perspectives. J. Palliat. Med. 2020, 23, 1323–1334. [Google Scholar] [CrossRef]
- Shortall, S. Psychedelic drugs and the problem of experience. Past Present 2014, 222, 187–206. [Google Scholar] [CrossRef]
- US Drug Enforcement Administration. Title 21 United States Code (USC) Controlled Substances Act: Section 812; US Drug Enforcement Administration: Fairfax County, VA, USA, 2016.
- Barnett, B.S.; Siu, W.O.; Pope, H.G. A survey of American psychiatrists’ attitudes toward classic hallucinogens. J. Nerv. Ment. Dis. 2018, 206, 476–480. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, J.A. A critical realist perspective for qualitative research. In Qualitative Enquiry—Past, Present and Future: A Critical Reader; Denzin, N.K., Giardina, M.D., Eds.; Left Coast Press, Inc.: Walnut Creek, CA, USA, 2015; pp. 88–102. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Inserra, A. Current status of psychedelic therapy in Australia and New Zealand: Are we falling behind? Aust. N. Z. J. Psychiatry 2019, 53, 190–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia-Romeu, A.; Richards, W.A. Current perspectives on psychedelic therapy: Use of serotonergic hallucinogens in clinical interventions. Int. Rev. Psychiatry 2018, 30, 291–316. [Google Scholar] [CrossRef] [PubMed]
- Puspanathan, P. Psychedelic research in Australia: Breaking through the stigma. Aust. N. Z. J. Psychiatry 2017, 51, 940–941. [Google Scholar] [CrossRef]
- Koffman, J.; Morgan, M.; Edmonds, P.; Speck, P.; Higginson, I.J. Vulnerability in palliative care research: Findings from a qualitative study of black Caribbean and white British patients with advanced cancer. J. Med. Ethics 2009, 35, 440–444. [Google Scholar] [CrossRef]
- Agin-Liebes, G.I.; Malone, T.; Yalch, M.M.; Mennenga, S.E.; Ponté, K.L.; Guss, J.; Bossis, A.P.; Grigsby, J.; Fischer, S.; Ross, S. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. J. Psychopharmacol. 2020, 34, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Beauchamp, T.L.; Childress, J.F. Principles of Biomedical Ethics, 5th ed.; Oxford University Press: New York, NY, USA, 2001. [Google Scholar]
- Nurgali, K.; Jagoe, R.T.; Abalo, R. Editorial: Adverse effects of cancer chemotherapy: Anything new to improve tolerance and reduce sequelae? Front. Pharmacol. 2018, 9, 245. [Google Scholar] [CrossRef]
- Aronson, J.K. Meyler’s Side Effects of Psychiatric Drugs; Elsevier Science: Amsterdam, The Netherlands, 2009. [Google Scholar]
- Nutt, D.J.; Sharpe, M. Uncritical positive regard? Issues in the efficacy and safety of psychotherapy. J. Psychopharmacol. 2008, 22, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Tunis, S.R.; Stryer, D.B.; Clancy, M.C. Practical Clinical Trials: Increasing the Value of Clinical Research for Decision Making in Clinical and Health Policy. J. Am. Med. Assoc. 2003, 290, 1624–1632. [Google Scholar] [CrossRef] [PubMed]
- Saturni, S.; Bellini, F.; Braido, F.; Paggiaro, P.; Sanduzzi, A.; Scichilone, N.; Santus, P.A.; Morandi, L.; Papi, A. Randomized controlled trials and real life studies. Approaches and methodologies: A clinical point of view. Pulm. Pharmacol. Ther. 2014, 27, 129–138. [Google Scholar] [CrossRef] [Green Version]
- Beaussant, Y.; Tulsky, J.; Guérin, B.; Schwarz-Plaschg, C.; Sanders, J.J. Mapping an Agenda for Psychedelic-Assisted Therapy Research in Patients with Serious Illness. J. Palliat. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Hannah, D.R.; Lautsch, B.A. Counting in qualitative research: Why to conduct it, when to avoid it, and when to closet it. J. Manag. Inq. 2011, 20, 14–22. [Google Scholar] [CrossRef]
| Participant Number | Age Range | Gender | Ethnicity | Profession | Years of Experience |
|---|---|---|---|---|---|
| 1 | 40–49 | Male | Asian | Doctor | >15 years |
| 2 | 30–39 | Female | NZ European | Doctor | 5 to 15 years |
| 3 | 30–39 | Female | NZ European | Social worker | <5 years |
| 4 | 20–29 | Female | NZ European | Psychologist | <5 years |
| 5 | 40–49 | Female | NZ European | Social worker | >15 years |
| 6 | 20–29 | Female | Māori | Psychologist | <5 years |
| 7 | 40–49 | Female | NZ European | Psychologist | >15 years |
| 8 | 50–59 | Female | Māori | Psychologist | 5 to 15 years |
| 9 | 20–29 | Female | Asian | Doctor | <5 years |
| 10 | 30–39 | Female | NZ European | Nurse | 5 to 15 years |
| 11 | 60–69 | Male | NZ European | Doctor | >15 years |
| 12 | 50–59 | Male | Māori | Doctor | 5 to 15 years |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reynolds, L.M.; Akroyd, A.; Sundram, F.; Stack, A.; Muthukumaraswamy, S.; Evans, W.J. Cancer Healthcare Workers’ Perceptions toward Psychedelic-Assisted Therapy: A Preliminary Investigation. Int. J. Environ. Res. Public Health 2021, 18, 8160. https://doi.org/10.3390/ijerph18158160
Reynolds LM, Akroyd A, Sundram F, Stack A, Muthukumaraswamy S, Evans WJ. Cancer Healthcare Workers’ Perceptions toward Psychedelic-Assisted Therapy: A Preliminary Investigation. International Journal of Environmental Research and Public Health. 2021; 18(15):8160. https://doi.org/10.3390/ijerph18158160
Chicago/Turabian StyleReynolds, Lisa M., Amelia Akroyd, Frederick Sundram, Aideen Stack, Suresh Muthukumaraswamy, and William J. Evans. 2021. "Cancer Healthcare Workers’ Perceptions toward Psychedelic-Assisted Therapy: A Preliminary Investigation" International Journal of Environmental Research and Public Health 18, no. 15: 8160. https://doi.org/10.3390/ijerph18158160
APA StyleReynolds, L. M., Akroyd, A., Sundram, F., Stack, A., Muthukumaraswamy, S., & Evans, W. J. (2021). Cancer Healthcare Workers’ Perceptions toward Psychedelic-Assisted Therapy: A Preliminary Investigation. International Journal of Environmental Research and Public Health, 18(15), 8160. https://doi.org/10.3390/ijerph18158160






