DEEP SCOPE: A Framework for Safe Healthcare Design
Abstract
1. Introduction
1.1. The Challenges of Complexity
Although healthcare providers work together, they are trained in separate disciplines, where the primary emphasis is the mastery of the skills and knowledge to diagnose ailments and render care. In the pursuit of becoming as knowledgeable and skillful as possible in their individual disciplines, a challenge facing nursing, medicine, and the other care specialties is to be aware of the reality that they are but one component of a very intricate and fragmented web of interacting subsystems of care where no single person or entity is in charge.[7] (p. 3)
1.2. An Evolution in Conceptualizing Patient Safety
1.2.1. Work System Design: Human Factors/Ergonomics for Safety in Healthcare
1.2.2. Resilience and Safety-II
2. Theoretical Underpinning
2.1. Designing to Mitigate Risk
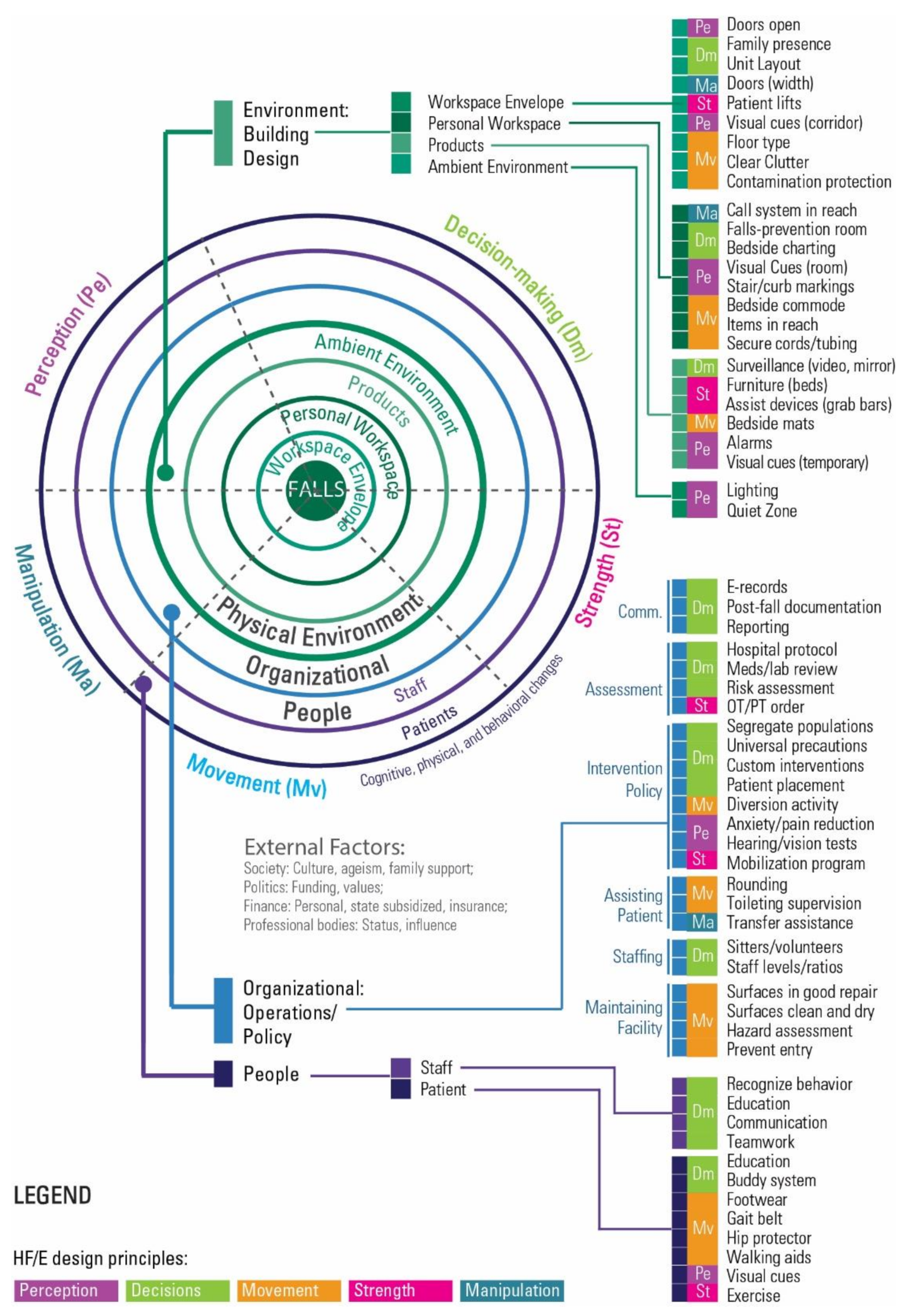
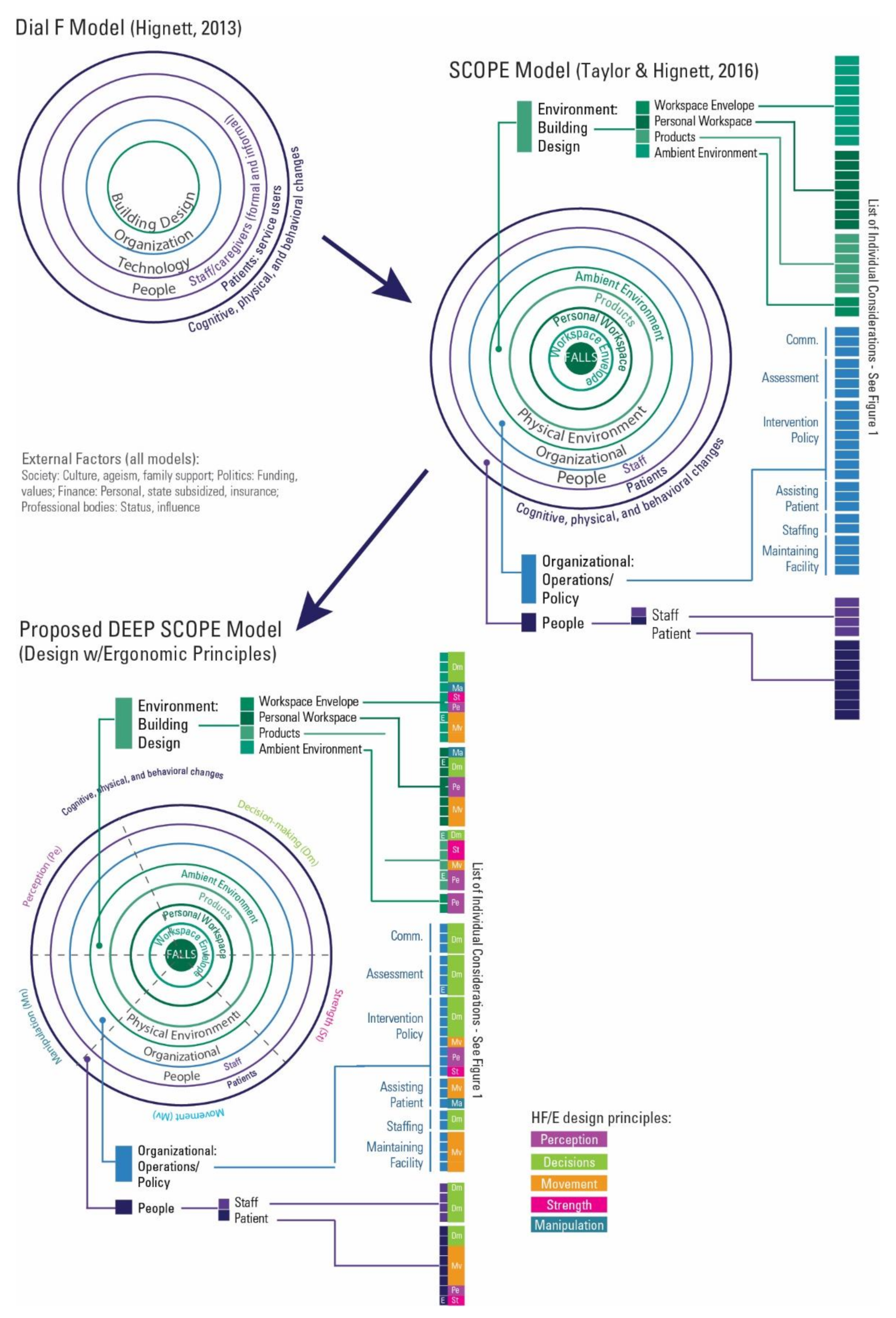
2.2. The SCOPE Model
2.3. HF/E Design Principles
- Optimizing opportunities for movement;
- Minimizing manipulation time;
- Minimizing the need for human strength;
- Minimizing perception time, and
- Minimizing decision-making time.
2.3.1. Optimizing Opportunity for Movement (Mv)
- locate visual displays within a normal line of sight and cone of easy eye rotation [45].
2.3.2. Minimizing Manipulation Time (Ma)
- designing for the extreme (e.g., clearance for the largest, reach for the smallest);
- designing for adjustability (e.g., seats);
- designing for the average (e.g., a registration counter);
- designing for a percentile (e.g., the 5th or 95th to define upper and lower limits).
2.3.3. Minimizing the Need for Human Strength (St)
2.3.4. Minimizing Perception Time (Pe)
- Understand that hidden or invisible parts are sometimes forgotten (e.g., small fonts on display monitors);
- Use visual discrimination such as size or color coding to form families of parts that belong together and enhance stimulus response for reduced reaction time (e.g., red for alarms);
- Recognize that touch (texture and size) can be a discriminating factor (e.g., sanded door knob finish to indicate no entry).
2.3.5. Minimizing Decision-Making Time (Dm)
- Consider the user’s mental model and recognize that diverse tasks result in different mental models to achieve different things with differing priorities (e.g., visibility, different alarm sounds);
- Minimize the number of (or co-locate) components and related tools (also saving space) to reduce choice reaction time (e.g., code button at the bed);
- Locate work elements in sequential order with task items that belong together in close physical proximity (e.g., crash carts) to improve spatial compatibility and improve stimulus response;
- Incorporate visual, tactile, or auditory feedback to indicate that the task was completed (e.g., electronic sound for touchscreen functions).
3. Results: An Expanded Model for Safety
3.1. The Development of DEEP SCOPE
3.1.1. The DEEP SCOPE Model
3.1.2. The DEEP SCOPE Matrix
4. Discussion
4.1. The Proposed Model in Context
4.2. Designing Safe Facilities—An HF/E Problem
- establishing the stability of the built environment and identifying HF/E environment categories (workplace envelope, personal workspace, products, and ambient environment);
- categorizing design interventions into three interacting categories (organization, people, and environment);
- creating connections across the organization, people, and environment through five HF/E design principles (manipulation, strength, movement, perception, decision-making).
4.3. Strengths, Limitations, and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Henriksen, K.; Kaplan, H. Hindsight Bias, Outcome Knowledge and Adaptive Learning. Qual. Saf. Health Care 2003, 12, ii46–ii50. [Google Scholar] [CrossRef]
- Catchpole, K. Spreading Human Factors Expertise in Healthcare: Untangling the Knots in People and Systems. BMJ Qual. Saf. 2013. [Google Scholar] [CrossRef]
- Carayon, P. (Ed.) Handbook of Human Factors and Ergonomics in Health Care and Patient Safety, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2011; ISBN 978-1-4398-3033-8. [Google Scholar]
- Dekker, S. Patient Safety: A Human Factors Approach; CRC Press: Boca Raton, FL, USA, 2011; ISBN 978-1-4398-5225-5. [Google Scholar]
- Dekker, S. Safety Differently: Human Factors for a New Era, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2014; ISBN 978-1-4822-4200-3. [Google Scholar]
- Simon, H.A. The Architecture of Complexity. Proc. Am. Philos. Soc. 1962, 106, 467–482. [Google Scholar]
- Henriksen, K.; Dayton, E.; Keyes, M.A.; Carayon, P.; Hughes, R.G. Understanding Adverse Events: A Human Factors Framework. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Hughes, R.G., Ed.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2008; pp. 67–85. [Google Scholar]
- Henriksen, K. Opportunities and Challenges in the Pursuit of Patient Safety. In Handbook of Human Factors and Ergonomics in Health Care and Patient Safety; CRC Press: Boca Raton, FL, USA, 2011; pp. 17–26. [Google Scholar]
- Willis, S.R. NLM Technical Bulletin; National Library of Medicine: Bethesda, MD, USA, 2012. [Google Scholar]
- Carayon, P.; Hundt, A.S.; Karsh, B.-T.; Gurses, A.P.; Alvarado, C.J.; Smith, M.; Brennan, P.F. Work System Design for Patient Safety: The SEIPS Model. Qual. Saf. Health Care 2006, 15, i50–i58. [Google Scholar] [CrossRef]
- Reason, J. The Contribution of Latent Human Failures to the Breakdown of Complex Systems. Philos. Trans. R. Soc. B Biol. Sci. 1990, 327, 475–484. [Google Scholar]
- Vincent, C.; Taylor-Adams, S.; Stanhope, N. Framework for Analysing Risk and Safety in Clinical Medicine. BMJ 1998, 316, 1154–1157. [Google Scholar] [CrossRef] [PubMed]
- Brasel, K.J.; Layde, P.M.; Hargarten, S. Evaluation of Error in Medicine Application of a Public Health Model. Acad. Emerg. Med. 2000, 7, 1298–1302. [Google Scholar] [CrossRef]
- Holden, R.J.; Carayon, P.; Gurses, A.P.; Hoonakker, P.; Hundt, A.S.; Ozok, A.A.; Rivera-Rodriguez, A.J. SEIPS 2.0: A Human Factors Framework for Studying and Improving the Work of Healthcare Professionals and Patients. Ergonomics 2013, 56. [Google Scholar] [CrossRef]
- Carayon, P.; Wooldridge, A.; Hoonakker, P.; Hundt, A.S.; Kelly, M.M. SEIPS 3.0: Human-Centered Design of the Patient Journey for Patient Safety. Appl. Erg. 2020, 84, 103033. [Google Scholar] [CrossRef] [PubMed]
- Donabedian, A. Evaluating the Quality of Medical Care. Milbank Mem. Fund Q. 1966, 44, 166–206. [Google Scholar] [CrossRef]
- Donabedian, A. The Quality of Care: How Can It Be Assessed? JAMA 1988, 260, 1743–1748. [Google Scholar] [CrossRef]
- Carayon, P.; Smith, M.J. Work Organization and Ergonomics. Appl. Ergon. 2000, 31, 649–662. [Google Scholar] [CrossRef]
- Smith, M.J.; Sainfort, P.C. A Balance Theory of Job Design for Stress Reduction. Int. J. Ind. Ergon. 1989, 4, 67–79. [Google Scholar] [CrossRef]
- Carthey, J. Understanding Safety in Healthcare: The System Evolution, Erosion and Enhancement Model. J. Public Health Res. 2013, 2, 25. [Google Scholar] [CrossRef]
- Braithwaite, J.; Wears, R.L.; Hollnagel, E. Resilient Health Care: Turning Patient Safety on Its Head. Int. J. Qual. Health Care 2015, 27, 418–420. [Google Scholar] [CrossRef] [PubMed]
- Hollnagel, E.; Woods, D.D. Epilogue: Resilience engineering precepts. In Resilience Engineering–Concepts and Precepts; Ashgate Publishing, Ltd.: Aldershot, UK, 2006; pp. 347–358. ISBN 0-7546-4641-6. [Google Scholar]
- Woods, D.D.; Hollnagel, E. Prologue: Resilience engineering concepts. In Resilience Engineering. Concepts and Precepts; Ashgate Publishing, Ltd.: Aldershot, UK, 2006; pp. 1–16. ISBN 0-7546-4641-6. [Google Scholar]
- Hollnagel, E. Accidents and Barriers. In Proceedings of the Seventh European Conference on Cognitive Science Approaches to Process Control, Lez Valenciennes, France, 21–24 September 1999; Volume 28, pp. 175–182. [Google Scholar]
- Hollnagel, E. Barriers and Accident Prevention; Ashgate: Aldershot, UK, 2004. [Google Scholar]
- Smith, K.M.; Valenta, A.L. Safety I to Safety II: A Paradigm Shift or More Work as Imagined? Int. J. Health Policy Manag. 2018, 7, 671–673. [Google Scholar] [CrossRef]
- Provan, D.J.; Woods, D.D.; Dekker, S.W.A.; Rae, A.J. Safety II Professionals: How Resilience Engineering Can Transform Safety Practice. Reliab. Eng. Syst. Saf. 2020, 195, 106740. [Google Scholar] [CrossRef]
- Hollnagel, E. Resilience Engineering and the Built Environment. Build. Res. Inf. 2014, 42, 221–228. [Google Scholar] [CrossRef]
- Hassler, U.; Kohler, N. Resilience in the Built Environment. Build. Res. Inf. 2014, 42, 119–129. [Google Scholar] [CrossRef]
- Wiig, S.; Braithwaite, J.; Clay-Williams, R. It’s Time to Step It up. Why Safety Investigations in Healthcare Should Look More to Safety Science. Int. J. Qual. Health Care 2020, 32, 281–284. [Google Scholar] [CrossRef]
- Taylor, E.; Joseph, A.; Quan, X. Design for Patient Safety—Considering a Patient Safety Risk Assessment. In Advances in Human Aspects of Healthcare; Duffy, V., Ed.; Advances in Human Factors and Ergonomics Series; CRC Press (Taylor & Francis Group): Boca Raton, FL, USA, 2012; Volume 3, pp. 249–258. [Google Scholar]
- The Center for Health Design Online Safety Risk Assessment Toolkit|A Process to Mitigate Risk. Available online: https://www.healthdesign.org/sra (accessed on 21 August 2019).
- Taylor, E.; Quan, X.; Joseph, A. Testing a Tool to Support Safety in Healthcare Facility Design. Procedia Manuf. 2015, 3, 136–143. [Google Scholar] [CrossRef][Green Version]
- Pati, D.; Harvey, T.E., Jr.; Reyers, E.; Evans, J.; Waggener, L.; Serrano, M.; Saucier, R.; Nagle, T. A Multidimensional Framework for Assessing Patient Room Configurations. HERD Health Environ. Res. Des. J. 2009, 2, 88–111. [Google Scholar] [CrossRef]
- Hignett, S.; Carayon, P.; Buckle, P.; Catchpole, K. State of Science: Human Factors and Ergonomics in Healthcare. Ergonomics 2013, 56, 1491–1503. [Google Scholar] [CrossRef] [PubMed]
- Taylor, E.; Hignett, S. The SCOPE of Hospital Falls: A Systematic Mixed Studies Review. HERD Health Environ. Res. Des. J. 2016, 9, 86–109. [Google Scholar] [CrossRef] [PubMed]
- Hignett, S. Why Design Starts with People. Health Found. 2013, 1–5. Available online: https://improve.bmj.com/sites/default/files/resources/why_design_starts_with_people.pdf (accessed on 21 July 2021).
- McNeese, M.D.; Zaff, B.S.; Citera, M.; Brown, C.E.; Whitaker, R. AKADAM: Eliciting User Knowledge to Support Participatory Ergonomics. Int. J. Ind. Ergon. 1995, 15, 345–363. [Google Scholar] [CrossRef]
- Carayon, P.; Alvarado, C.; Hundt, A.S. Reducing Workload and Increasing Patient Safety through Work and Workspace Design; Institute of Medicine Committee on the Work Environment for Nurses and Patient Safety: Washington, DC, USA, 2003. [Google Scholar]
- Helander, M.G.; Willén, B.Å. Design for Human Assembly (DHA). In The Occupational Ergonomics Handbook; Karwowski, W., Marras, W.S., Eds.; CRC Press: Boca Raton, FL, USA, 1999; pp. 1849–1865. ISBN 978-0-203-01045-7. [Google Scholar]
- Kroemer, K.H.E.; Kroemer, A.D. Office Ergonomics; Taylor & Francis, Ltd.: London, UK, 2001; ISBN 978-0-7484-0952-5. [Google Scholar]
- Kroemer, K.H.E.; Kroemer, H.B.; Kroemer-Elbert, K.E. Ergonomics: How to Design for Ease and Efficiency; Prentice Hall: Hoboken, NJ, USA, 2000; ISBN 978-0-13-278359-0. [Google Scholar]
- Sanders, M.S.; McCormick, E.J. Human Factors in Engineering and Design, 7th ed.; McGraw-Hill Education: New York, NY, USA, 1993; ISBN 978-0-07-054901-2. [Google Scholar]
- Wickens, C.D.; Lee, J.; Gordon-Becker, S.; Liu, Y. An Introduction to Human Factors Engineering, 2nd ed.; Pearson: London, UK, 2014; ISBN 978-1-292-02231-4. [Google Scholar]
- Kroemer, K.H.E. Assessment of Human Muscle Strength for Engineering Purposes: A Review of the Basics. Ergonomics 1999, 42, 74–93. [Google Scholar] [CrossRef]
- Noyes, J.; Garland, K.; Bruneasu, D. Humans: Skills, Capabilities and Limitations. In Human Factors for Engineers; Sandorn, C., Harvey, R.S., Eds.; The Institution of Engineering and Technology: London, UK, 2004; pp. 35–56. ISBN 978-0-86341-329-2. [Google Scholar]
- Noyes, J. Psychology at Work. In Designing for Humans; Psychology Press: Hove, UK, 2002. [Google Scholar]
- Wilson, J.R.; Sharples, S. Evaluation of Human Work, 4th ed.; CRC Press: Boca Raton, FL, USA, 2015; ISBN 978-1-4665-5962-2. [Google Scholar]
- Lopez, K.D.; Gerling, G.J.; Cary, M.P.; Kanak, M.F. Cognitive Work Analysis to Evaluate the Problem of Patient Falls in an Inpatient Setting. JAMIA 2010, 17, 313–321. [Google Scholar] [CrossRef][Green Version]
- Hollnagel, E.; Braithwaite, J.; Wears, R.L. (Eds.) Resilient Health Care; Ashgate Studies in Resilient Engineering; Ashgate Publishing, Ltd.: Surrey, UK, 2013; ISBN 978-1-4724-6919-9. [Google Scholar]
- Colman, N.; Dalpiaz, A.; Hebbar, K.B. Simulation Enhances Safety Evaluation in the Design of New Healthcare Facilities. Curr. Treat. Options Peds. 2020, 6, 214–225. [Google Scholar] [CrossRef]
- Jurewicz, K.A.; Neyens, D.M.; Catchpole, K.; Joseph, A.; Reeves, S.T.; Abernathy, J.H. Observational Study of Anaesthesia Workflow to Evaluate Physical Workspace Design and Layout. Br. J. Anaesth. 2021, 126, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Bayramzadeh, S.; Aghaei, P. Technology Integration in Complex Healthcare Environments: A Systematic Literature Review. Appl. Ergon. 2021, 92. [Google Scholar] [CrossRef] [PubMed]
- RIPCHD.OR Study Group. Realizing Improved Patient Care through Human-Centered Design in the OR; Clemson Center for Health Facilities Design & Testing: Clemson, SC, USA, 2016. [Google Scholar]
- Taylor, E. The Healthcare Workplace: More Than a New ‘Old’ Hospital. J. Inter. Des. 2017, 42, 9–18. [Google Scholar] [CrossRef]
- Piatkowksi, M.; Taylor, E.; Wong, B.; Taylor, D.; Foreman, K.B.; Merryweather, A. Designing a Patient Room as a Fall Protection Strategy: The Perspectives of Architects. Int. J. Environ. Res. Public Health 2021. under review. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taylor, E.; Hignett, S. DEEP SCOPE: A Framework for Safe Healthcare Design. Int. J. Environ. Res. Public Health 2021, 18, 7780. https://doi.org/10.3390/ijerph18157780
Taylor E, Hignett S. DEEP SCOPE: A Framework for Safe Healthcare Design. International Journal of Environmental Research and Public Health. 2021; 18(15):7780. https://doi.org/10.3390/ijerph18157780
Chicago/Turabian StyleTaylor, Ellen, and Sue Hignett. 2021. "DEEP SCOPE: A Framework for Safe Healthcare Design" International Journal of Environmental Research and Public Health 18, no. 15: 7780. https://doi.org/10.3390/ijerph18157780
APA StyleTaylor, E., & Hignett, S. (2021). DEEP SCOPE: A Framework for Safe Healthcare Design. International Journal of Environmental Research and Public Health, 18(15), 7780. https://doi.org/10.3390/ijerph18157780





