1. Introduction
As of 2018, 55% of the world’s population—4.2 billion people—live in urban areas [
1]. This trend is expected to continue. By 2050, the urban population is expected to more than double its current size, and around 68% of the world’s population will live in cities [
1]. Many issues in health and environment are likely to arise with rapid urbanization. To deal with these threats, WHO has begun to advocate the construction of healthy cities as a global strategy since the 1980s. The Healthy Cities strategy has been adopted as the national development strategy of many countries around the world. This strategy is also critical to the implementation of the UN’s New Urban Agenda [
2] and the achievement of the UN Sustainable Development Goals (SDGs) [
3]. A common theme in these documents is that a sustainable development depends increasingly on the successful management of urban growth, especially in low-income and lower-middle-income countries where the most rapid urbanization is expected between now and 2050 [
1].
Over the past few decades, healthy cities have been successfully developed worldwide. According to WHO, a healthy city is one that is “continually creating and improving those physical and social environments and expanding those community resources which enable people to mutually support each other in performing all the functions of life and developing to their maximum potential” [
4]. To achieve the goal of a healthy city, it is important to create a health supporting environment via healthy setting approaches. Settings for health or healthy settings, refer to “the place or social context in which people engage in daily activities in which environmental, organizational and personal factors interact to affect health and wellbeing” [
4]. Today, various settings are used to facilitate the improvement of public health throughout the world and examples of settings include schools, work sites, hospitals, villages, and cities [
5]. The importance of health supporting environments is also documented in the literature of the psychology of sustainability and sustainable development. The key idea is to place the psychological well-being of human beings in different environments, from the natural environment, the personal environment, the social environment, the organizational environment, and the inter-organizational environment, to the globalized environment and the virtual environment [
6].
For China, the national healthy setting movement can be traced back to the National Healthy Lifestyle for All (NHLA) campaign in 2007. The NHLA campaign calls on “the Chinese people to develop a healthy diet and engage in physical exercises, advocating healthy lifestyle ideas, creating a supporting environment for a healthy lifestyle, and enhancing the people’s awareness and behavioral abilities to develop a healthy lifestyle” [
7], which coincides with the UN’s SDGs on good health and well-being (i.e., ensure healthy lives and promote well-being for all at all ages). Following the NHLA missions, the Chinese government issued the “Health Supporting Environment Development Guideline for the National Healthy Lifestyle for All” in 2013 (hereinafter referred to as the “Guideline”) [
8]. In this Guideline, governments at regional levels are required to build nine types of health supporting environments, including healthy worksites, healthy communities, health schools, health canteens, healthy restaurants, healthy trails, healthy huts, healthy street and healthy parks [
8]. Up until 2018, over 60,000 health supporting environments were built and accredited nationwide [
9]. From an empirical perspective, the growth may be considered as meeting the national guidelines. However, evaluating the quality of these environments remains an important task to provide guidance for future policies. Therefore, the primary goal of our paper is to study the relationship between health supporting environments and residents’ health and well-being. It is worth noting well-being—often synonymous with quality of life—is widely used in many different fields. In the field of urban spaces and architecture, quality of life generally refers to the condition of the environment in which people live and/or some attribute of people themselves, such as their health or educational achievement [
10]. Here we use self-reported health status to indicate health-related quality of life, which is often viewed as a multidimensional concept that incorporates symptoms, functional ability, and perceptions of health in the field of health care [
11,
12]. Although our measures may not holistically convey many aspects of the notion of health-related quality of life, we believe our study is a starting point to provide a larger platform for multi-disciplinary dialogue between public health and urban spaces.
Health literacy (HL) is another topic with growing importance in the field of public health, which is particularly true in China. The first “National Health Literacy Surveillance” (NHLS) survey was conducted in 2008, in which the Chinese government adopted the widely accepted definition of health literacy, which was developed by the (US) National Library of Medicine—“the degree to which individuals can obtain, process, and understand the basic health information and services they need to make appropriate health-related decisions”. The first NHLS surveyed around 80,000 residents aged 15–69 and included 96 items intended to measure adult health literacy. The national health literacy rate in 2008 is merely 6.48%. This rate measures the percentage of residents who gave correct answers to at least 80% of the survey questions, i.e., classified as having adequate health literacy. A large rural–urban disparity exists with the rate of health literacy being 9.49% among urban residents and only 3.43% among rural residents [
13]. The second NHLS survey was conducted in 2012 and the survey has run annually since then. This rate of health literacy rose steadily from 8.8% in 2012 to 10.25% in 2015. In 2016, the Chinese government issued its “Healthy China 2030 Blueprint”, which proposed major health indicators to be achieved in 2030. In this blueprint, the rate of national health literacy is aimed to increase to 30%, tripling the existing level in 2015.
Although empirical evidence on the relationship between health literacy and health outcomes remains mixed, a growing body of literature has found that lower health literacy is associated with poorer health outcomes [
14,
15,
16,
17]. As a result, promoting health literacy is a public health goal in many countries. In an integrated framework that draws on several models of health literacy, health literacy plays a key role that determines an adult’s health outcomes at different stages of health behavior change [
18]. Our secondary goal thus, is to explore the role that health literacy plays in mediating the impact that access to health supporting environments has on residents’ health and well-being.
4. Discussion
We use a sample of 12,360 adults (aged 15–69) surveyed in 2018 and 2019 NHLS survey in Ningbo, China and examine the effects that access to health supporting environments have on residents’ health and well-being. We study the role of HL in moderating the effect of community health supporting environment. By health supporting environments, we pick up three types of health supporting environments at neighborhood level, namely, healthy parks, healthy trails, and healthy huts, and construct the corresponding measures by aggregating at community level, which we then merge with individual level data characterizing residents’ HL, self-reported health status and chronic disease status.
On average, 66% of residents rated their health as being good or excellent as opposed to fair, poor or very poor. We examine the association of self-reported health with healthy parks, healthy trails, and healthy huts in
Table 2. We find access to healthy parks or healthy trails is positively associated with residents’ self-reported health controlling for community level covariates and residents’ individual level demographic and socioeconomic characteristics. Parks and trails can improve health in several ways including increased physical activity and improved mental health [
36]. For example, walkable access to sites like parks may motive people to participate in physical activity and to do so more frequently. Outdoor activities in parks can also help for stress reduction. In addition, parks can reduce air and water pollution, protect hazard areas from inappropriate development and mitigate urban heat islands [
36]. In contrast, we find access to healthy huts is negatively associated with residents’ likelihood of self-reporting good health. It is not unreasonable that on average the proportion of residents self-reporting good health is lower among communities with healthy huts. The testing services in healthy huts enable residents to test their blood pressure and glucose level and they are likely to be alert to their health problems and be encouraged to see doctors. Residents might be diagnosed with diseases if they had not used the services in healthy huts. As a result, they self-report a lower level of health. In the long run, however, early detection prevents the disease to progress to more serious stage. Alternatively, residents might not be diagnosed with any diseases from using the services in healthy huts, but they are likely to evaluate their own health with a more objective perception. Therefore, when being asked to rate their health in general, their responses come with a smaller self-reporting bias. A prior, we do not know whether this bias is positive or negative, but a positive bias is more likely among some groups than others. For example, some smokers may justify or rationalize their smoking behaviors by believing they are healthy [
37,
38]. For both reasons above, we are likely to observe a lower level of self-reported health among communities with healthy huts.
The above results have some noteworthy implications. Healthy huts might play a role in reducing the likelihood of undiagnosed diseases and changing people’s lifestyle. Disease prevention is a challenge in many countries. Diabetes among adults (18+) in China in 2010 was 12 percent, and pre-diabetes was estimated to be 50 percent with the majority of patients undiagnosed and untreated [
39]. If healthy huts do encourage residents to seek care who may otherwise forgo health care due to their perception on their own health, it implies the cases of undiagnosed diseases would be less prevalent among communities with healthy huts. In [
37], we find that smokers whose self-reported health is higher are less likely to consider quitting. This relationship persists after we control for their objective health status. In other words, one’s perception of health matters. We speculate healthy huts could serve a role in motivating smokers to quit because smokers perceive their health differently. It is like the effect of being advised to quit by health care professionals.
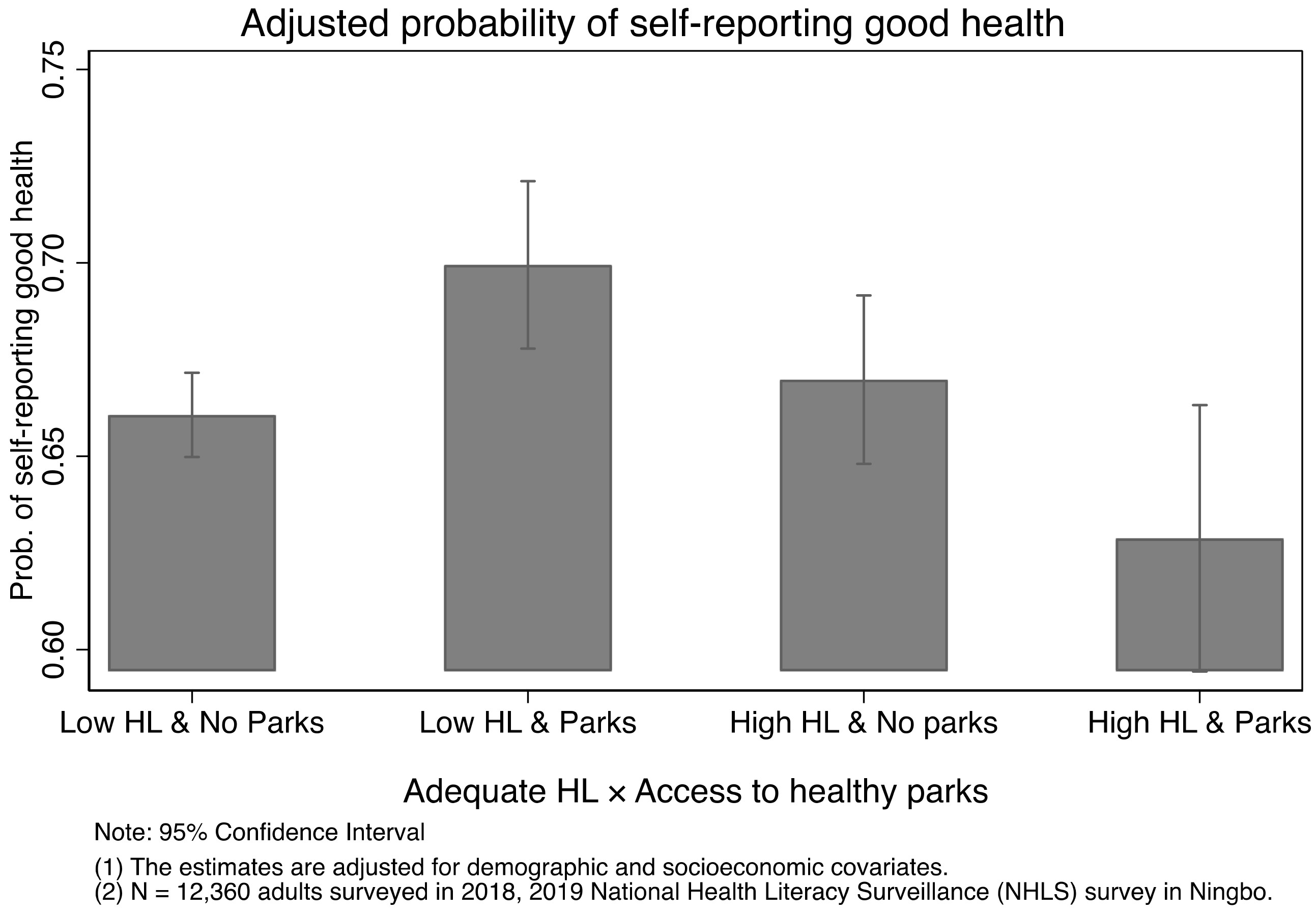
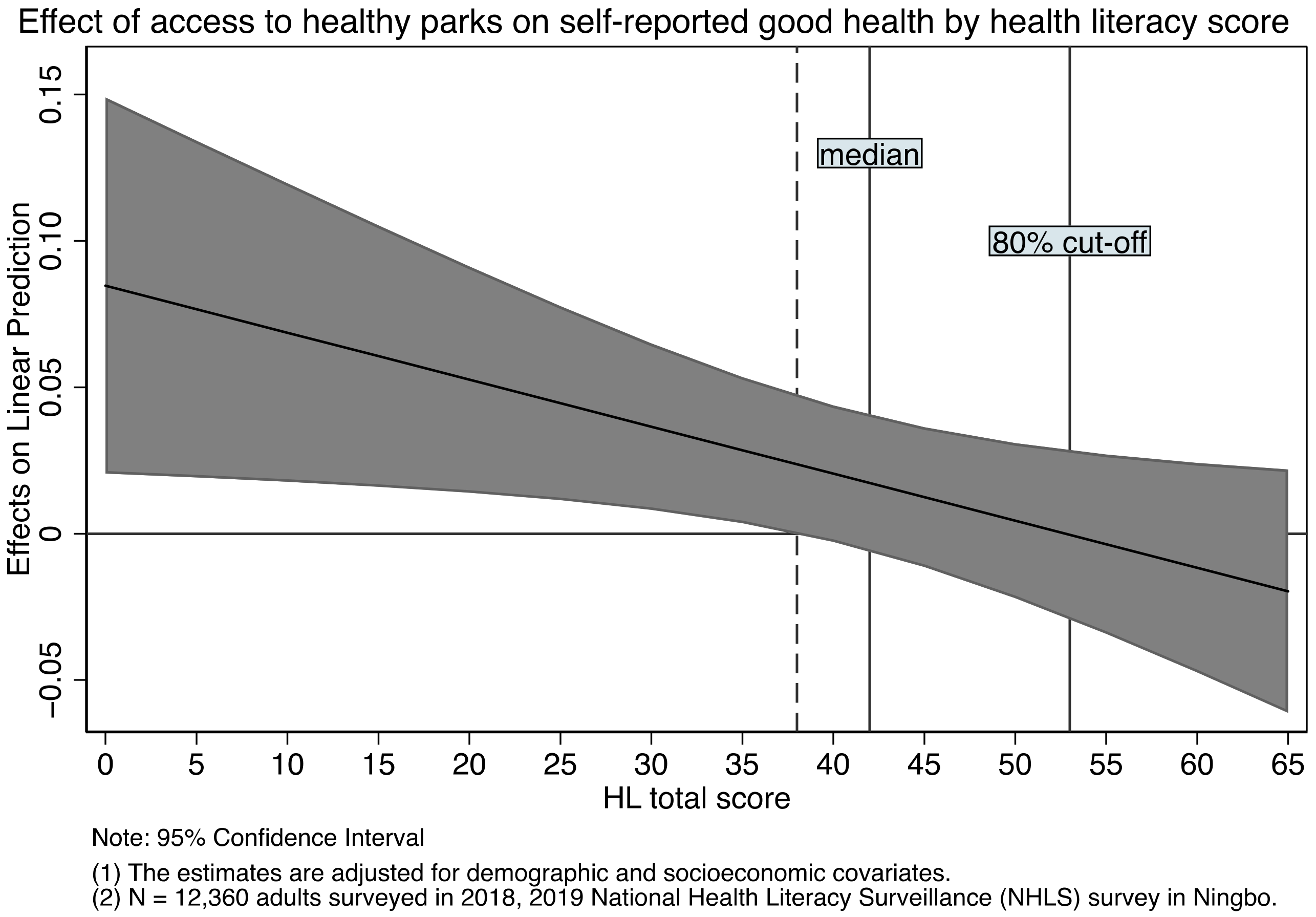
We investigated the role of HL in
Table 3 and
Table 4. We find HL plays a role in moderating the effects of healthy parks. The positive association between access to healthy parks and self-reported health is more likely to be observed among people with a low level of HL, which is shown in
Table 3 (and illustrated in
Figure A1 and
Figure A2 in the
Appendix B). This might arise because residents with adequate HL have different sources of learning health news. Education is one of the key factors that determine the level of HL, which also plays a key role in explaining how people learn and internalize health information [
40]. For example, in one study, it is documented that people with a college education are more likely to receive their most useful health information from books, newspapers, or magazines. In contrast, the less educated (i.e., those with a high school degree or less) are most likely to get their information from a doctor [
40]. This difference might imply walkable access to sites, such as parks and trails, may not serve as the primary venue for physical activity (a key ingredient to keep a good health) when people are equipped with better health knowledge. As a result, the effect of healthy parks is less salient among the group with better HL. We find similar results when we replace the health outcome with chronic disease occurrence in
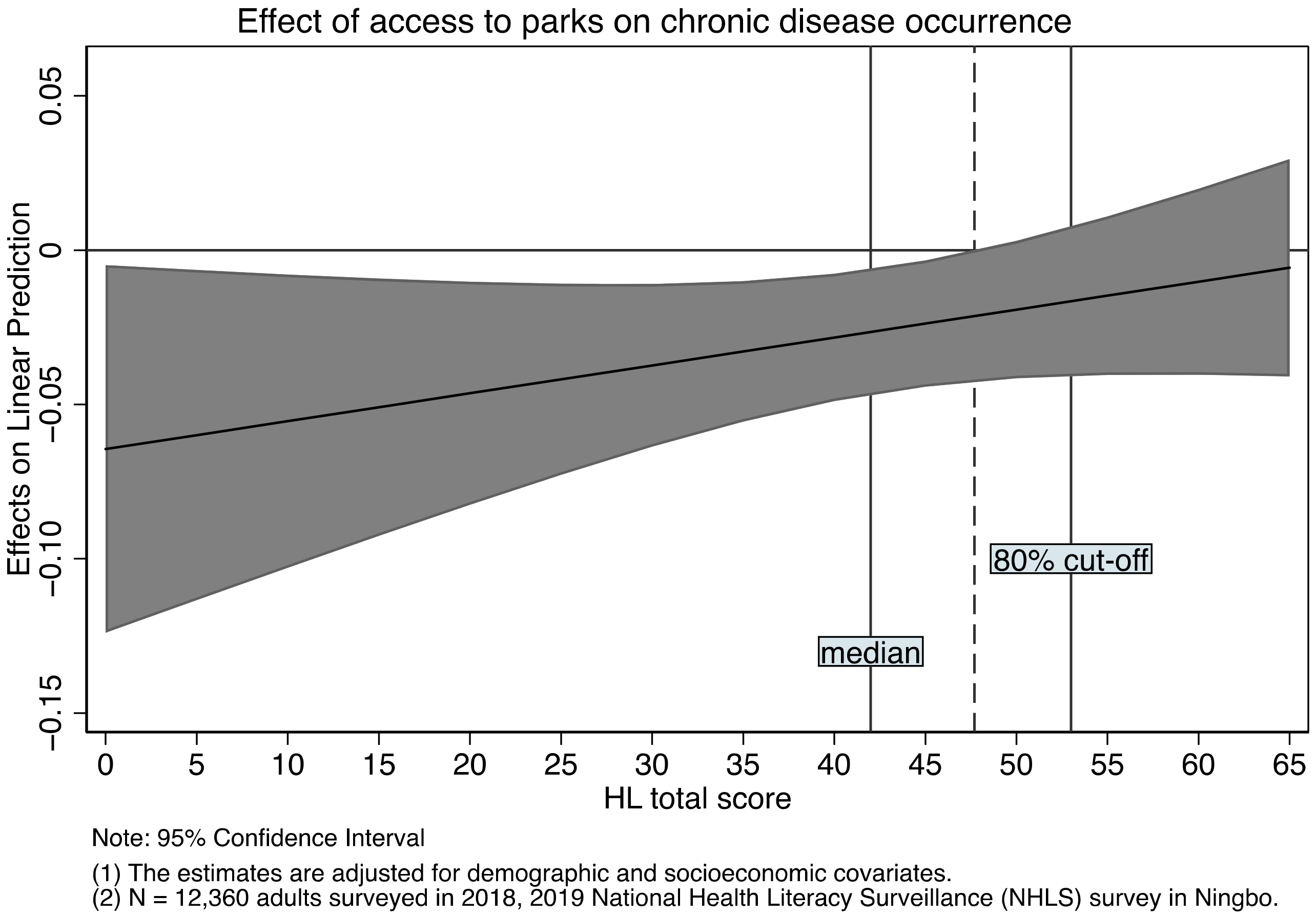
Table 5, and we observe a similar pattern in
Figure A5 in the
Appendix B that access to community healthy parks is associated with a reduced likelihood of having chronic diseases, but only among those with a low level of HL.
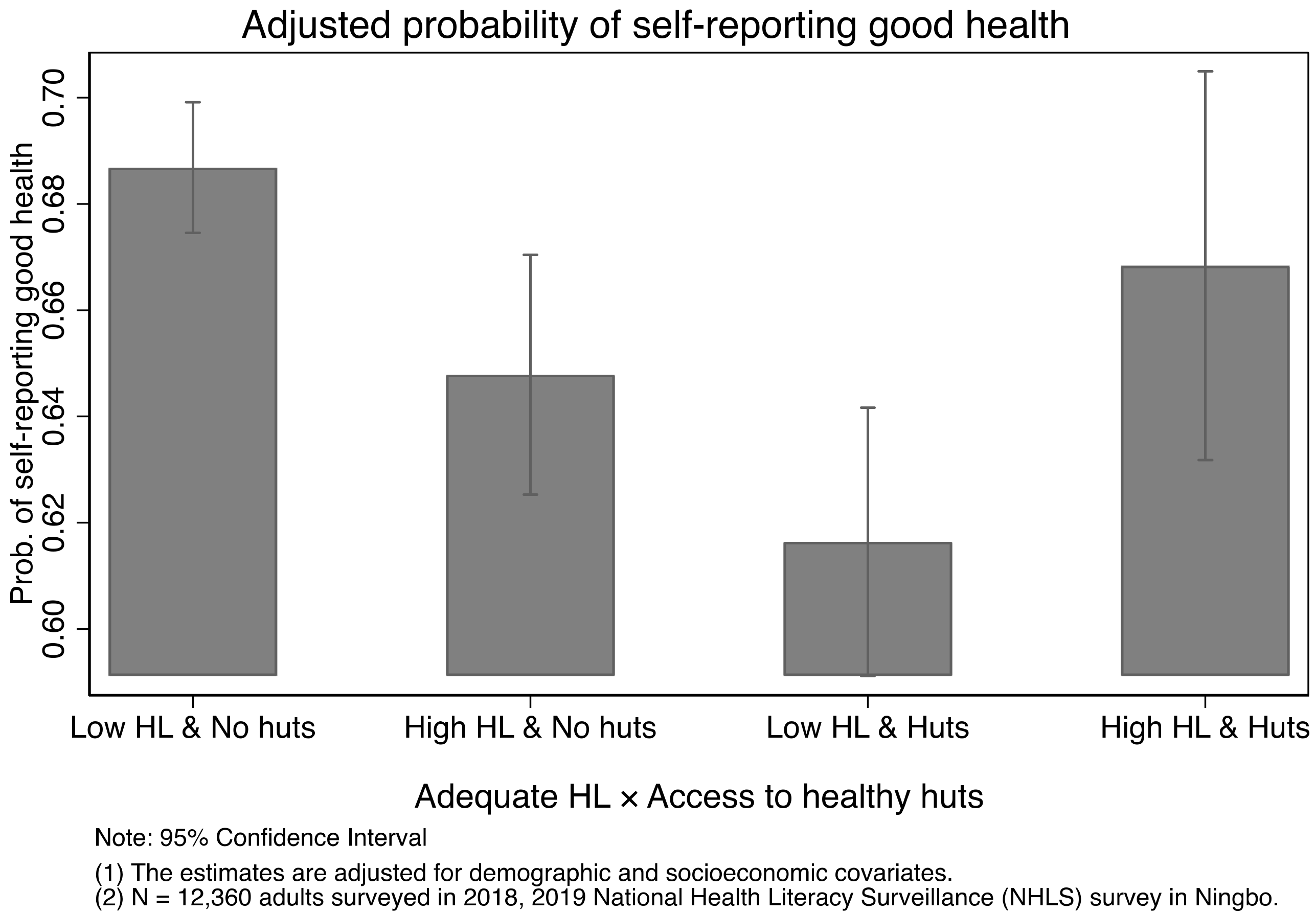
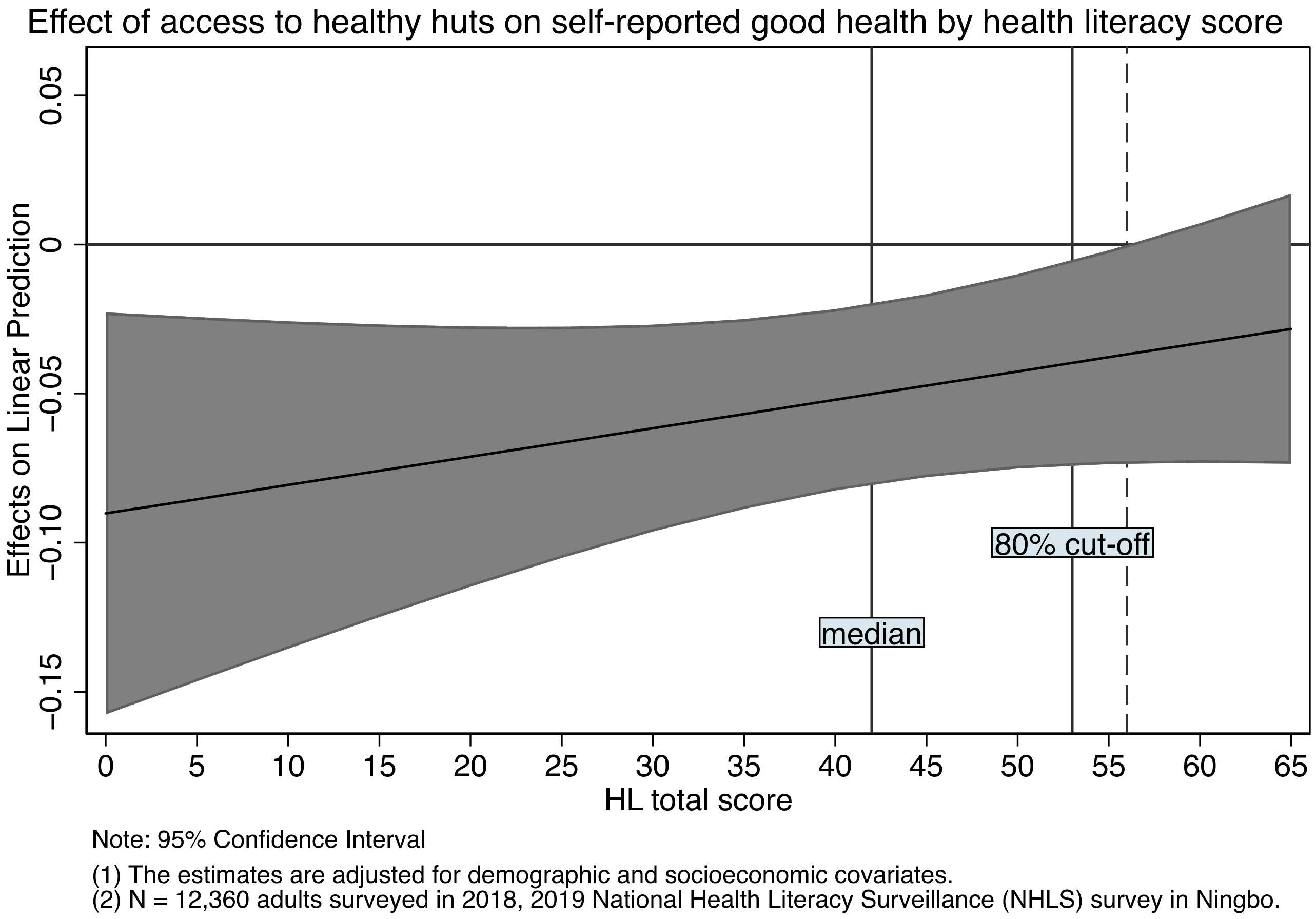
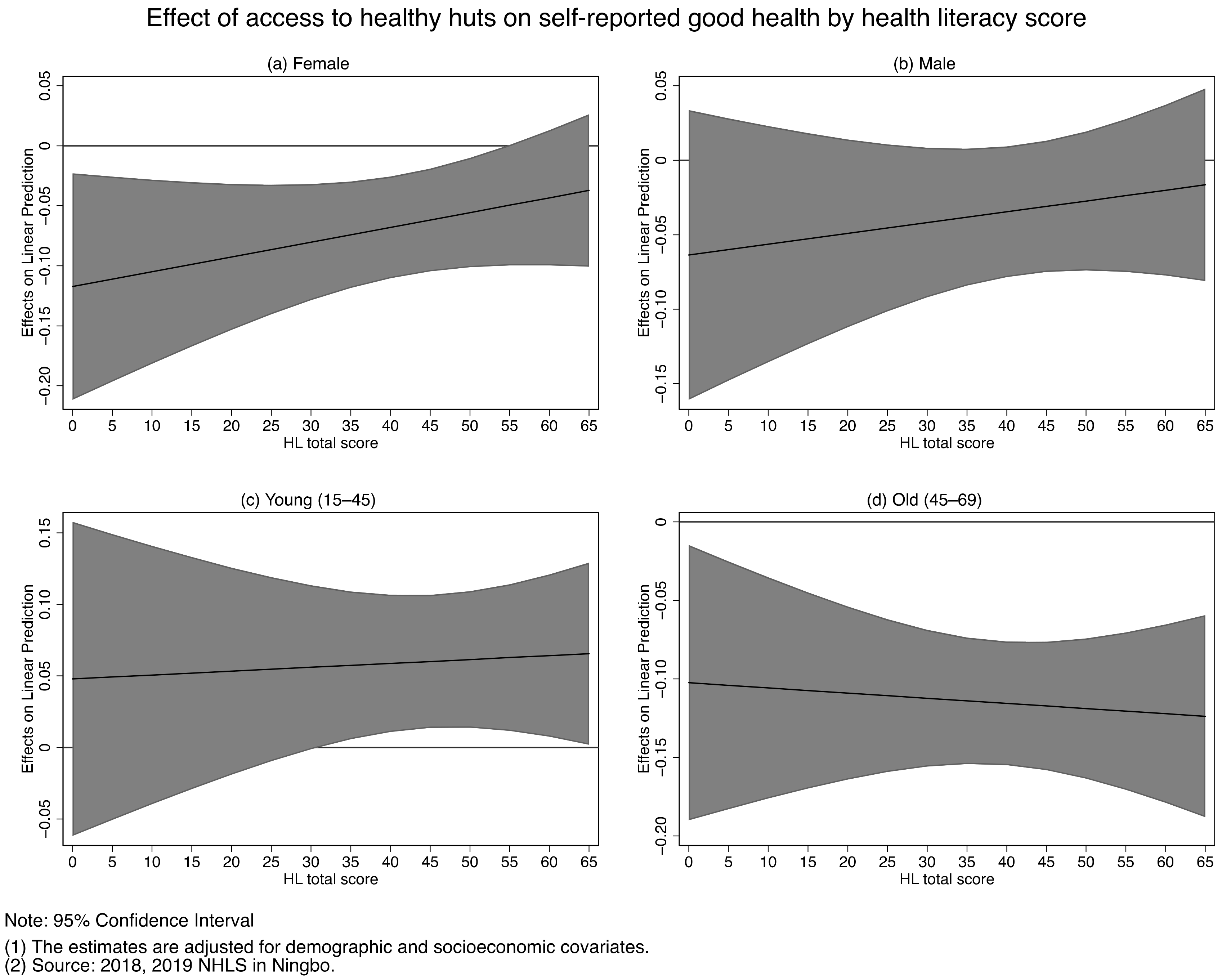
The role of HL is different when it comes to the effects of healthy huts. It appears that access to healthy huts is negatively associated with people’s self-reported health status, but only among those with inadequate HL. This might arise because people with adequate HL are more likely to use the services in healthy huts. We lack the data to test this hypothesis as HL of the respondents are not measured before and after their access to healthy huts. In addition, most services in healthy huts are self-service, it is not impossible residents with inadequate HL might misuse or misinterpret the testing results without some prior knowledge. On the other hand, we find the effect of HL is significantly greater among residents with healthy huts. This might arise because HL could improve after the diagnosis of chronic diseases [
25]. There is evidence that a negative health event can prompt individuals to adopt risk-reducing behaviors [
41,
42]. Similarly, the diagnosis of chronic disease might expose individuals to more disease-related information. This improved health knowledge might help them prevent a new disease or promote their health and well-being. In other words, HL is a condition that residents benefit from healthy huts.
It is worth noting, one of the aims of building healthy huts is to facilitate the dissemination of health knowledge and improve individuals’ ability to make health-related decisions [
8]. In other words, healthy huts are built to improve residents’ HL. This improved HL may in turn help their use of the services and adopt a healthy lifestyle. If we assume there are two channels through which HL can be acquired—passive pathway through diagnosis of diseases and active pathway through health education, we believe healthy huts promote the health of residents by helping residents to gain health knowledge via an active pathway. Indeed, we find in our descriptive statistics that residents living in communities with healthy huts on average have a higher level of HL. However, this difference disappears after we control for community level and individual level covariates (see
Table A2 in the
Appendix A).
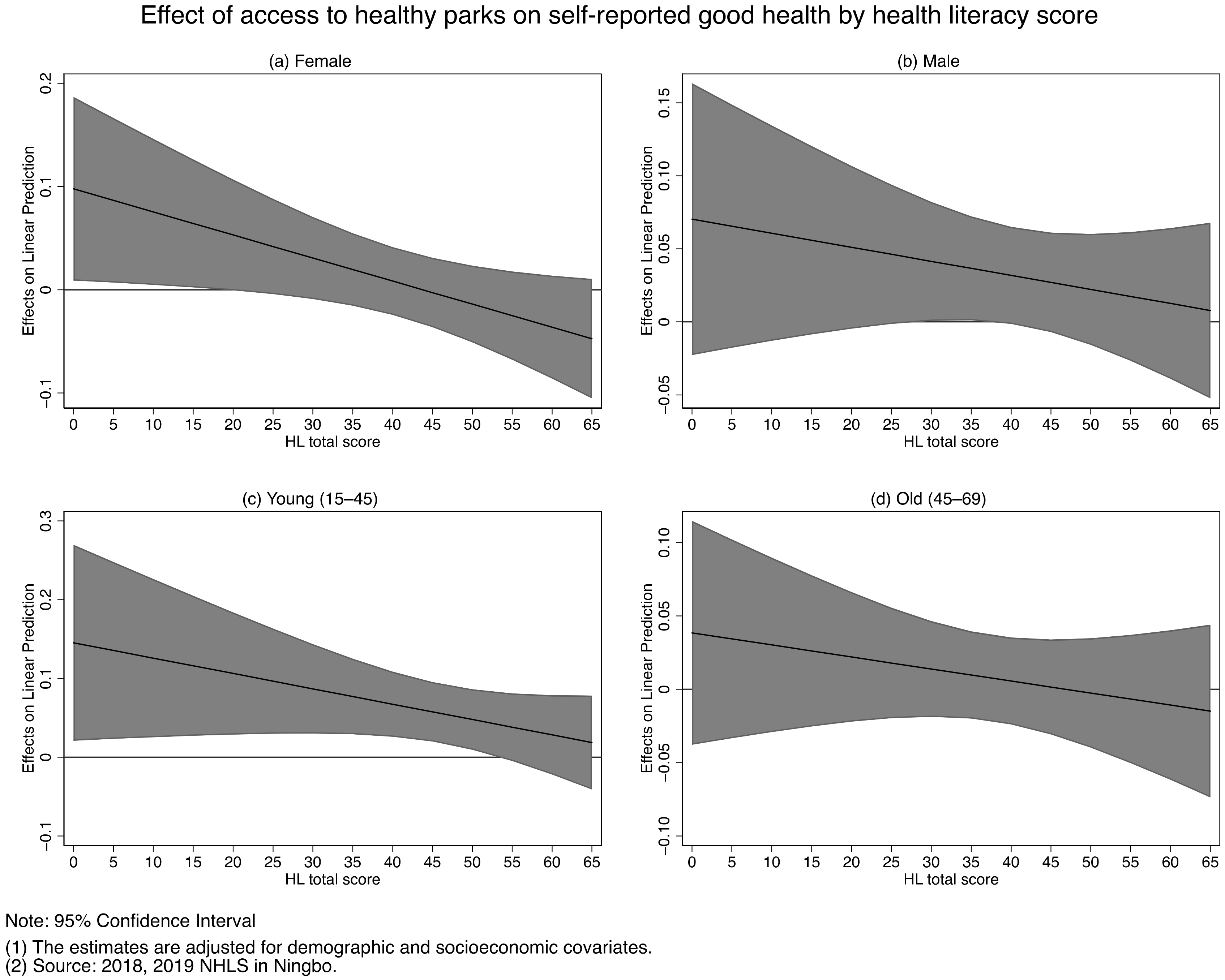
As a robustness check, we examine the extent to which the health supporting environments effects vary with the gender and age of the residents (see
Table A3 in the
Appendix A). It appears the male and young samples are more likely to experience the positive effect of access to healthy parks. The positive effect of access to healthy trails does not differ by gender but is only significant in the old sample. The negative effect of healthy huts varies by gender and age of the residents and is more likely to be pronounced in females and the old sample. In contrast, the effect of access to healthy huts is positive in the young sample. In light of our earlier observation in
Table 1, it might be because younger residents on average have a higher level of HL, and thus, are more likely to benefit from using healthy huts. We also study the interaction effect between access to healthy parks and HL score and the results are illustrated in
Figure A6 and
Figure A7 in the
Appendix B.
Although the rural–urban difference in health outcomes and HL is evident in other studies and is also observed in our data (see
Table A4 in the
Appendix A for the summary statistics of the rural and urban sub-samples), we do not think it is appropriate to examine the effects of health supporting environments separately in the rural and urban data. As mentioned earlier, the national geographic distribution of health supporting environments is not equal and there are more accredited constructions in (more developed) eastern provinces than in (less developed) middle/western provinces. This pattern is also true between rural and urban regions in our data. In
Table A4, we find the urban residents on average have a higher level of HL as well as better health than their rural counterparts. The fraction of access to healthy parks, healthy trails, and healthy huts is also significantly greater in the urban sample. For example, over 40% of urban residents are living in communities with healthy huts. In contrast, only 3% of rural residents have access to healthy huts. The estimates would be misleading if we restrict to the rural/urban sub-samples, because the rural-urban split is a key factor that determines the distribution of health supporting environments. Despite this, we report the estimates of this exercise for illustration purpose in
Table A5. For ease of comparison, in column (1) we repeat our estimates for the full sample from
Table 2. Here, the effect in the full sample (e.g., 0.020 for the access to healthy parks) is hardly a weighted average of the effects in the two subsamples (i.e., −0.064 for the rural sample and 0.013 for the urban sample), an indication that it is inappropriate to use the partitioned data here. However, it does not mean reducing the rural-urban disparity in health supporting environments is not important. With the growth in urbanization, we do not think the growth in health supporting environments would be an independent process with reducing the rural-urban disparity in health outcomes.
Another problem is we use community to define residents’ access to health supporting environments. We assume settings are available to all residents living in the same community, who also have equal likelihood to use the settings. This might not apply to all residents, whose willingness to use the settings cannot be recorded by our data. Theoretically, residents living beyond a community can also access the settings, but due to the geographical proximity, the associated cost should be greater (e.g., transportation cost). Although we do not think it is reasonable to define access to healthy setting at a higher-level geographic entity involving only 10 districts/counties, we repeat our estimations using district level health supporting environments. We find none of three settings are significant except for the access to healthy trails (a positive effect). Furthermore, we consider the level of health supporting environment using binary classification, discarding the information that some communities have more than one healthy setting. Our main findings are unchanged if we use the number instead of the presence (coded 0/1) of health supporting environments. With the trend in the growth of health supporting environments, we consider it a potential area for future research to use geographics data to classify the level of health supporting environments at individual level (i.e., an individual is assigned a unique value based on the size of the environments proportional to the meter circular buffer of their residential address predefined) so to better evaluate and quantify the health supporting environments effects.
There are several limitations in our study, and our findings should be interpreted with caution. Firstly, this is a cross-sectional study. There might exist factors that influence a resident’s health and the accessibility of health supporting environments. For example, residents might choose to move to neighborhoods with better healthy supporting environments for the sake of their health. In addition, although we have controlled a series of community level characteristics (e.g., resident population and district/county dummies), it is likely the location of health supporting environments is correlated with some community characteristics that we do not control for but determine the residents’ health and well-being at the same time, which is likely to undermine the effects of healthy parks we observe. Secondly, our data are not representative nationally, and Ningbo represents one of the cities with better economic development in China. We do not think our findings apply to all regions in China. Lastly, our HL measurement can be limited in measuring HL which is an evolving concept [
43] and is not comparable with measures used in other countries. Despite their reliability and construct validity we mentioned earlier, the construct instruments included in the questionnaire are basically unchanged in the past few years. It implies respondents with higher score of HL may not be more knowledgeable, but simply better at taking tests than those who achieved lower scores.