Sitting Posture during Prolonged Computer Typing with and without a Wearable Biofeedback Sensor
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
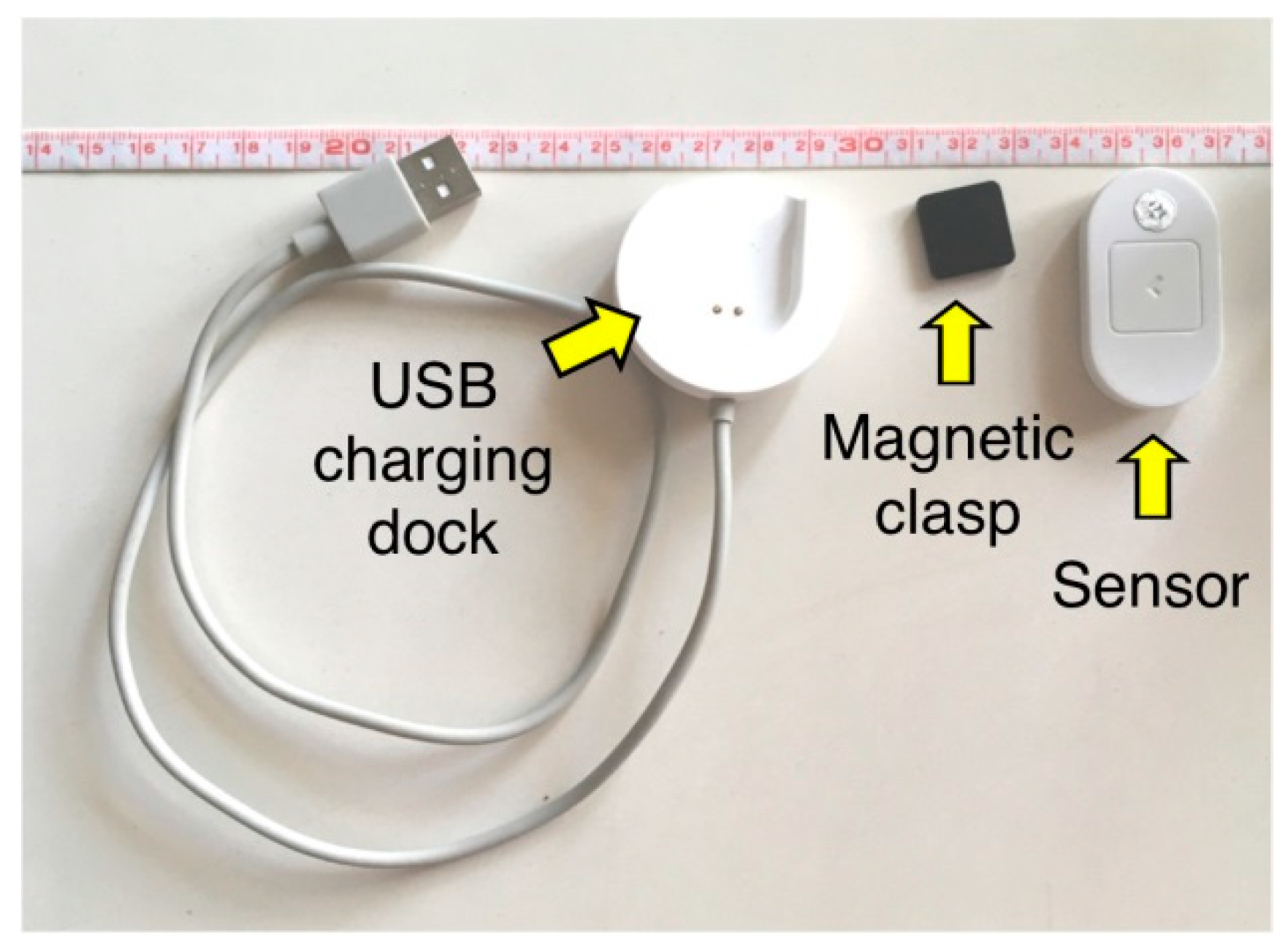
2.3. Instrumentation
2.4. Procedure
2.5. Data Analysis
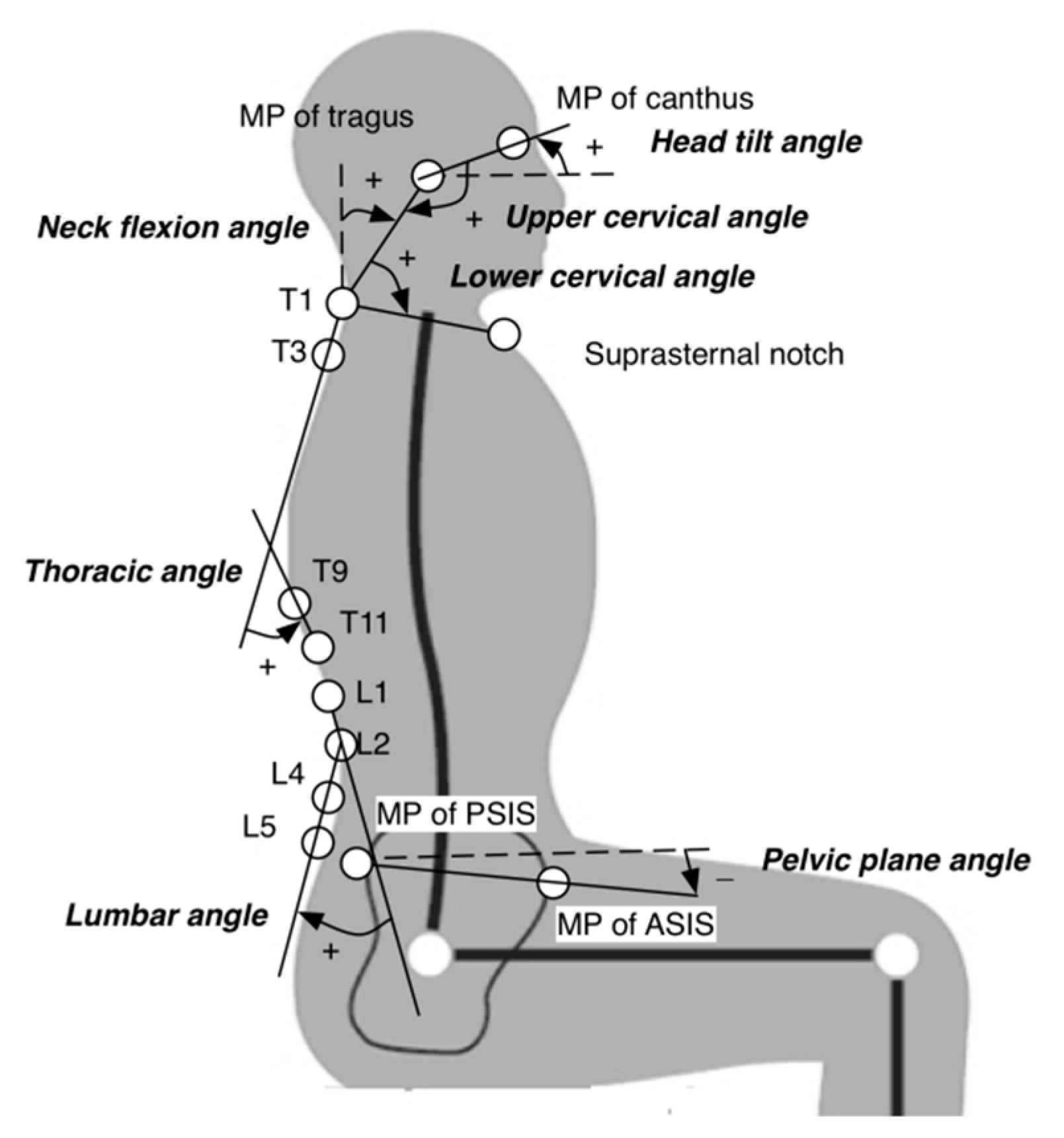
- (a)
- Head tilt angle: the segment of the mid-point of canthus and the mid-point of tragus relative to the horizontal plane.
- (b)
- Neck flexion angle: the segment formed by the mid-point of tragus and spinous process of T1 relative to the frontal plane.
- (c)
- Upper cervical angle: the angle between the mid-point of canthus, the mid-point of tragus and the T1 spinous process.
- (d)
- Lower cervical angle: the angle between the mid-point of tragus, the T1 spinous process and the suprasternal notch.
- (e)
- Thoracic angle: the angle between the segments of T1–T3 and T9–T11.
- (f)
- Lumbar angle: the angle between the segments of L1–L2 and L4–L5.
- (g)
- Pelvic plane angle: the angle between the segment of the mid-point of anterior superior iliac spines and the mid-point of posterior superior iliac spines relative to the horizontal plane.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mielke, G.I.; Burton, N.W.; Turrell, G.; Brown, W.J. Temporal trends in sitting time by domain in a cohort of mid-age Australian men and women. Maturitas 2018, 116, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Matthews, C.E.; Chen, K.Y.; Freedson, P.S.; Buchowski, M.S.; Beech, B.M.; Pate, R.R.; Troiano, R.P. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am. J. Epidemiol. 2008, 167, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Lis, A.M.; Black, K.M.; Korn, H.; Nordin, M. Association between sitting and occupational LBP. Eur. Spine J. 2007, 16, 283–298. [Google Scholar] [CrossRef]
- Cote, P.; van der Velde, G.; Cassidy, J.D.; Carroll, L.J.; Hogg-Johnson, S.; Holm, L.W.; Carragee, E.J.; Haldeman, S.; Nordin, M.; Hurwitz, E.L.; et al. The burden and determinants of neck pain in workers: Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008, 33, S60–S74. [Google Scholar] [CrossRef] [PubMed]
- Janwantanakul, P.; Pensri, P.; Jiamjarasrangsri, V.; Sinsongsook, T. Prevalence of self-reported musculoskeletal symptoms among office workers. Occup. Med. 2008, 58, 436–438. [Google Scholar] [CrossRef]
- Juul-Kristensen, B.; Søgaard, K.; Strøyer, J.; Jensen, C. Computer users’ risk factors for developing shoulder, elbow and back symptoms. Scand J. Work Environ. Health 2004, 30, 390–398. [Google Scholar] [CrossRef]
- Bhardwaj, Y.; Mahajan, R. Prevalence of neck pain and disability in computer users. Int. J. Sci. Res. 2017, 6, 1288–1290. [Google Scholar]
- Hafeez, K.; Ahmed Memon, A.; Jawaid, M.; Usman, S.; Usman, S.; Haroon, S. Back Pain-Are Health Care Undergraduates At Risk? Iran. J. Public Health 2013, 42, 819–825. [Google Scholar]
- Hurwitz, E.L.; Randhawa, K.; Yu, H.; Côté, P.; Haldeman, S. The Global Spine Care Initiative: A summary of the global burden of low back and neck pain studies. Eur. Spine J. 2018, 27, 796–801. [Google Scholar] [CrossRef]
- March, L.; Smith, E.U.; Hoy, D.G.; Cross, M.J.; Sanchez-Riera, L.; Blyth, F.; Buchbinder, R.; Vos, T.; Woolf, A.D. Burden of disability due to musculoskeletal (MSK) disorders. Best Pract. Res. Clin. Rheumatol. 2014, 28, 353–366. [Google Scholar] [CrossRef]
- Dieleman, J.L.; Cao, J.; Chapin, A.; Chen, C.; Li, Z.; Liu, A.; Horst, C.; Kaldjian, A.; Matyasz, T.; Scott, K.W.; et al. US Health Care Spending by Payer and Health Condition, 1996–2016. JAMA 2020, 323, 863–884. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.; Kim, J.-W.; Heo, J.-H.; Jeon, H.-M.; Choi, E.-B.; Eom, G.-M. The effect of sitting posture on the loads at cervico-thoracic and lumbosacral joints. Technol. Health Care 2018, 26, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Patwardhan, A.G.; Khayatzadeh, S.; Havey, R.M.; Voronov, L.I.; Smith, Z.A.; Kalmanson, O.; Ghanayem, A.J.; Sears, W. Cervical sagittal balance: A biomechanical perspective can help clinical practice. Eur. Spine J. 2018, 27, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Florencio, L.L.; Ferracni, G.N.; Chaves, T.C.; Palacios-Ceña, M.; Ordás-Bandera, C.; Speciali, J.G.; Grossi, D.B.; Fernández-de-Las-Peñas, C. Analysis of Head Posture and Activation of the Cervical Neck Extensors During a Low-Load Task in Women with Chronic Migraine and Healthy Participants. J. Manip. Physiol. Ther. 2018, 41, 762–770. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, N.F.; Hassan, K.A.; Abdelmajeed, S.F.; Moustafa, I.M.; Silva, A.G. The Relationship Between Forward Head Posture and Neck Pain: A Systematic Review and Meta-Analysis. Curr. Rev. Musculoskelet Med. 2019, 12, 562–577. [Google Scholar] [CrossRef] [PubMed]
- Poitras, S.; Blais, R.; Swaine, B.; Rossignol, M. Management of work-related low back pain: A population-based survey of physical therapists. Phys. Ther. 2005, 85, 1168–1181. [Google Scholar] [CrossRef] [PubMed]
- Kendall, F.P.; McCreary, E.K.; Provance, P.G.; Rodgers, M.M.; Romani, W.A. Muscles Testing and Function with Posture and Pain; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2005. [Google Scholar]
- Falla, D.; Jull, G.; Russell, T.; Vicenzino, B.; Hodges, P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys. Ther. 2007, 87, 408–417. [Google Scholar] [CrossRef]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Is ‘ideal’ sitting posture real? Measurement of spinal curves in four sitting postures. Man. Ther. 2009, 14, 404–408. [Google Scholar] [CrossRef]
- Annetts, S.; Coales, P.; Colville, R.; Mistry, D.; Moles, K.; Thomas, B.; van Deursen, R. A pilot investigation into the effects of different office chairs on spinal angles. Eur. Spine J. 2012, 21, 165–170. [Google Scholar] [CrossRef]
- Baumgartner, D.; Zemp, R.; List, R.; Stoop, M.; Naxera, J.; Elsig, J.P.; Lorenzetti, S. The Spinal Curvature of Three Different Sitting Positions Analysed in an Open MRI Scanner. Sci. World J. 2012, 2012, 184016. [Google Scholar] [CrossRef] [PubMed]
- Grondin, D.E.; Triano, J.J.; Tran, S.; Soave, D. The effect of a lumbar support pillow on lumbar posture and comfort during a prolonged seated task. Chiropr. Man. Ther. 2013, 21, 21. [Google Scholar] [CrossRef]
- Ward, J.; Coats, J. Comparison of the BackJoy SitSmart Relief and Spine Buddy LT1 H/C Ergonomic Chair Supports on Short-Term Neck and Back Pain. J. Manip. Physiol. Ther. 2017, 40, 41–49. [Google Scholar] [CrossRef]
- Celenay, S.T.; Kaya, D.O.; Ozudogru, A. Spinal postural training: Comparison of the postural and mobility effects of electrotherapy, exercise, biofeedback trainer in addition to postural education in university students. J. Back Musculoskelet. Rehabil. 2015, 28, 135–144. [Google Scholar] [CrossRef]
- Yoo, W.G.; Park, S.Y. Effects of posture-related auditory cueing (PAC) program on muscles activities and kinematics of the neck and trunk during computer work. Work 2015, 50, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Yoo, W.G.; Yi, C.H.; Kim, M.H. Effects of a proximity-sensing feedback chair on head, shoulder, and trunk postures when working at a visual display terminal. J. Occup. Rehabil. 2006, 16, 631–637. [Google Scholar] [CrossRef]
- Rodrigues Ferreira Faisting, A.L.; de Oliveira Sato, T. Effectiveness of ergonomic training to reduce physical demands and musculoskeletal symptoms-An overview of systematic reviews. Int. J. Ind. Ergon. 2019, 74, 102845. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Brink, Y.; Louw, Q.; Grimmer, K.; Schreve, K.; van der Westhuizen, G.; Jordaan, E. Development of a cost effective three-dimensional posture analysis tool: Validity and reliability. BMC Musculoskelet. Disord. 2013, 14, 335. [Google Scholar] [CrossRef] [PubMed]
- Brink, Y.; Louw, Q.; Grimmer, K.; Jordaan, E. The spinal posture of computing adolescents in a real-life setting. BMC Musculoskelet Disord. 2014, 15, 212. [Google Scholar] [CrossRef]
- Kuo, Y.L.; Tully, E.A.; Galea, M.P. Video analysis of sagittal spinal posture in healthy young and older adults. J. Manip. Physiol. Ther. 2009, 32, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Yip, C.H.; Chiu, T.T.; Poon, A.T. The relationship between head posture and severity and disability of patients with neck pain. Man. Ther. 2008, 13, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Szeto, G.P.; Straker, L.; Raine, S. A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Appl. Ergon. 2002, 33, 75–84. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics; SAGE: London, UK, 2013. [Google Scholar]
- Kim, H.-Y. Statistical notes for clinical researchers: Effect size. Restor. Dent. Endod. 2015, 40, 328–331. [Google Scholar] [CrossRef]
- Hestbaek, L.; Leboeuf-Yde, C.; Kyvik, K.O.; Manniche, C. The course of low back pain from adolescence to adulthood: Eight-year follow-up of 9600 twins. Spine 2006, 31, 468–472. [Google Scholar] [CrossRef] [PubMed]
- Proske, U.; Gandevia, S.C. The Proprioceptive Senses: Their Roles in Signaling Body Shape, Body Position and Movement, and Muscle Force. Physiol. Rev. 2012, 92, 1651–1697. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.S.; Cholewicki, J.; Reeves, N.P.; Zazulak, B.T.; Mysliwiec, L.W. Comparison of trunk proprioception between patients with low back pain and healthy controls. Arch. Phys. Med. Rehabil. 2010, 91, 1327–1331. [Google Scholar] [CrossRef] [PubMed]
- Stanton, T.R.; Leake, H.B.; Chalmers, K.J.; Moseley, G.L. Evidence of Impaired Proprioception in Chronic, Idiopathic Neck Pain: Systematic Review and Meta-Analysis. Phys. Ther. 2016, 96, 876–887. [Google Scholar] [CrossRef]
- Ribeiro, D.C.; Sole, G.; Abbott, J.H.; Milosavljevic, S. Extrinsic feedback and management of low back pain: A critical review of the literature. Man. Ther. 2011, 16, 231–239. [Google Scholar] [CrossRef]
- Huang, H.; Wolf, S.L.; He, J. Recent developments in biofeedback for neuromotor rehabilitation. J. Neuroeng. Rehabil. 2006, 3, 11. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, R.; Wrisberg, C. Motor Learning and Performance: A Situation-Based Learning Approach, 4th ed.; Human Kinetics: Champaign, IL, USA, 2008. [Google Scholar]
- Cramer, H.; Mehling, W.E.; Saha, F.J.; Dobos, G.; Lauche, R. Postural awareness and its relation to pain: Validation of an innovative instrument measuring awareness of body posture in patients with chronic pain. BMC Musculoskelet. Disord. 2018, 19, 109. [Google Scholar] [CrossRef]
- McLean, L. The effect of postural correction on muscle activation amplitudes recorded from the cervicobrachial region. J. Electromyogr. Kinesiol. 2005, 15, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Haller, M.; Richter, C.; Brandl, P.; Gross, S.; Schossleitner, G.; Schrempf, A.; Nii, H.; Sugimoto, M.; Inami, M. Finding the Right Way for Interrupting People Improving Their Sitting Posture; Human-Computer Interaction–INTERACT 2011; Campos, P., Graham, N., Jorge, J., Nunes, N., Palanque, P., Winckler, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2011; pp. 1–17. [Google Scholar]
| Angles | Device | T5 | T15 | T25 | T35 | T45 | T55 | Condition (C) | Time (T) | Interaction (C × T) |
|---|---|---|---|---|---|---|---|---|---|---|
| Head tilt | Without | 12.7 ± 7.4 | 11.7 ± 8.0 | 11.6 ± 8.8 | 11.4 ± 8.6 | 13.7 ± 9.5 | 11.3 ± 9.4 | p = 0.434 | p = 0.582 | p = 0.079 |
| With | 12.2 ± 8.9 | 12.5 ± 9.7 | 13.1 ± 9.7 | 12.9 ± 8.7 | 12.3 ± 9.4 | 12.9 ± 10.2 | ||||
| Neck flexion | Without | 59.3 ± 5.3 | 60.2 ± 6.2 | 59.7 ± 6.5 | 59.8 ± 6.3 | 59.0 ± 6.6 | 60.3 ± 6.2 | p < 0.001 * | p = 0.619 | p = 0.201 |
| With | 57.2 ± 5.7 | 57.4 ± 5.7 | 56.8 ± 5.8 | 56.5 ± 5.8 | 57.1 ± 6.0 | 56.6 ± 5.9 | ||||
| Upper cervical | Without | 155.1 ± 8.2 | 154.9 ± 9.0 | 154.1 ± 9.7 | 153.9 ± 8.9 | 155.7 ± 10.5 | 154.4 ± 10.7 | p = 0.004 * | p = 0.650 | p = 0.334 |
| With | 151.6 ± 7.2 | 152.3 ± 8.5 | 152.3 ± 8.1 | 151.7 ± 7.7 | 151.6 ± 8.1 | 151.6 ± 8.8 | ||||
| Lower cervical | Without | 62.3 ± 8.6 | 61.8 ± 8.0 | 61.5 ± 7.9 | 61.4 ± 8.3 | 62.2 ± 9.5 | 61.4 ± 8.6 | p = 0.012 * | p = 0.688 | p = 0.149 |
| With | 60.3 ± 7.6 | 60.7 ± 7.5 | 60.9 ± 8.1 | 60.4 ± 7.7 | 60.5 ± 7.5 | 60.9 ± 8.1 | ||||
| Thoracic | Without | 28.9 ± 7.8 | 29.7 ± 8.0 | 28.8 ± 9.0 | 29.0 ± 8.3 | 29.3 ± 9.6 | 29.6 ± 8.0 | p = 0.033 * | p = 0.816 | p = 0.613 |
| With | 27.2 ± 8.1 | 27.6 ± 8.4 | 27.2 ± 8.2 | 27.5 ± 9.5 | 27.9 ± 9.1 | 26.6 ± 8.7 | ||||
| Lumbar | Without | 8.6 ± 4.9 | 9.4 ± 4.9 | 9.3 ± 4.6 | 8.9 ± 5.2 | 8.9 ± 4.5 | 8.4 ± 5.2 | p = 0.217 | p = 0.094 | p = 0.516 |
| With | 7.2 ± 4.8 | 9.0 ± 5.0 | 8.1 ± 5.4 | 7.1 ± 4.7 | 8.1 ± 5.0 | 8.5 ± 5.1 | ||||
| Pelvic plane | Without | 7.3 ± 6.6 | 7.0 ± 7.3 | 7.7 ± 6.8 | 6.8 ± 6.4 | 8.8 ± 8.8 | 6.7 ± 8.4 | p = 0.021 * | p = 0.566 | p = 0.501 |
| With | 5.7 ± 6.3 | 5.2 ± 7.1 | 5.8 ± 6.5 | 4.1 ± 5.6 | 4.8 ± 6.8 | 5.5 ± 5.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuo, Y.-L.; Huang, K.-Y.; Kao, C.-Y.; Tsai, Y.-J. Sitting Posture during Prolonged Computer Typing with and without a Wearable Biofeedback Sensor. Int. J. Environ. Res. Public Health 2021, 18, 5430. https://doi.org/10.3390/ijerph18105430
Kuo Y-L, Huang K-Y, Kao C-Y, Tsai Y-J. Sitting Posture during Prolonged Computer Typing with and without a Wearable Biofeedback Sensor. International Journal of Environmental Research and Public Health. 2021; 18(10):5430. https://doi.org/10.3390/ijerph18105430
Chicago/Turabian StyleKuo, Yi-Liang, Kuo-Yuan Huang, Chieh-Yu Kao, and Yi-Ju Tsai. 2021. "Sitting Posture during Prolonged Computer Typing with and without a Wearable Biofeedback Sensor" International Journal of Environmental Research and Public Health 18, no. 10: 5430. https://doi.org/10.3390/ijerph18105430
APA StyleKuo, Y.-L., Huang, K.-Y., Kao, C.-Y., & Tsai, Y.-J. (2021). Sitting Posture during Prolonged Computer Typing with and without a Wearable Biofeedback Sensor. International Journal of Environmental Research and Public Health, 18(10), 5430. https://doi.org/10.3390/ijerph18105430







