Evaluation of the Prognosis of COVID-19 Patients According to the Presence of Underlying Diseases and Drug Treatment
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Data
2.2. Statistical Analyses
3. Results
3.1. Description of the Cohort
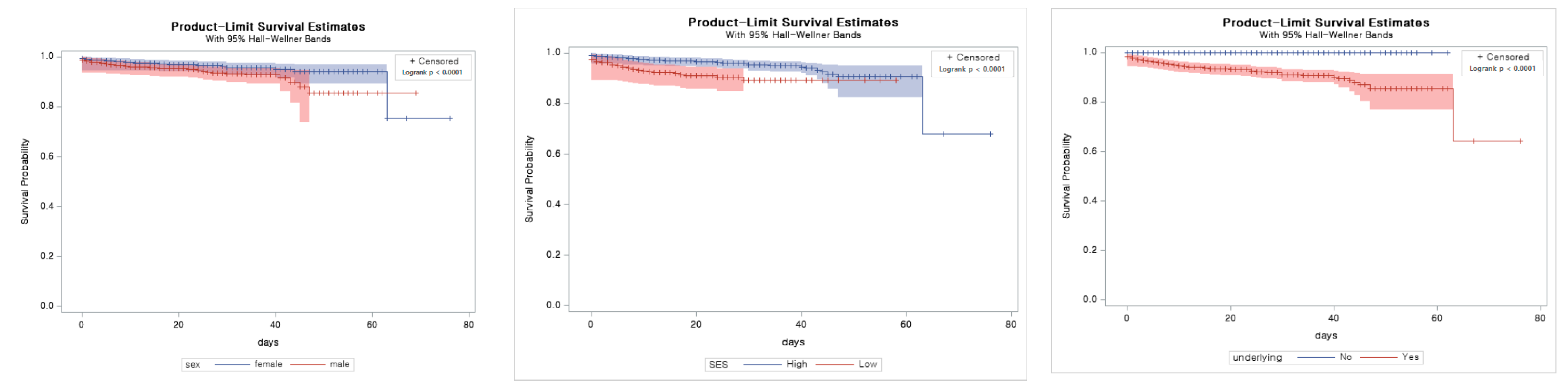
3.2. Univariable Analysis
3.3. Observation Time and Main Outcomes
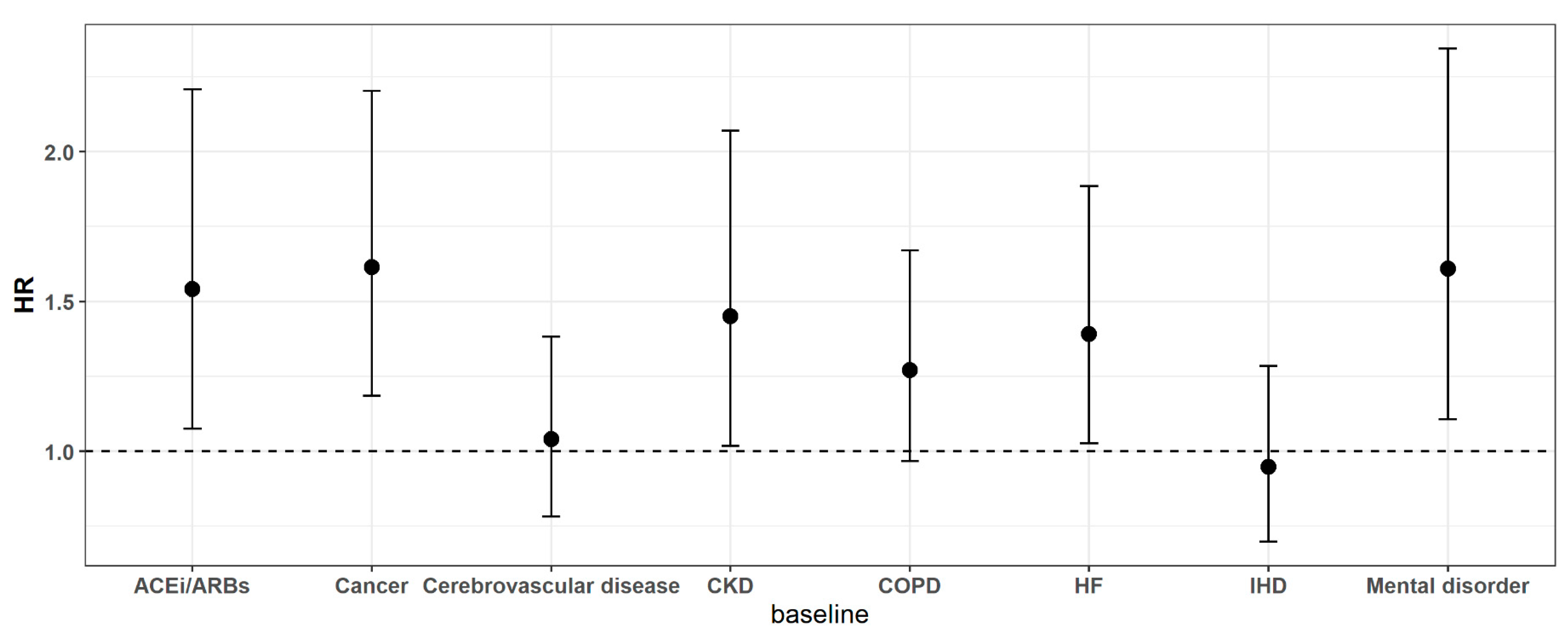
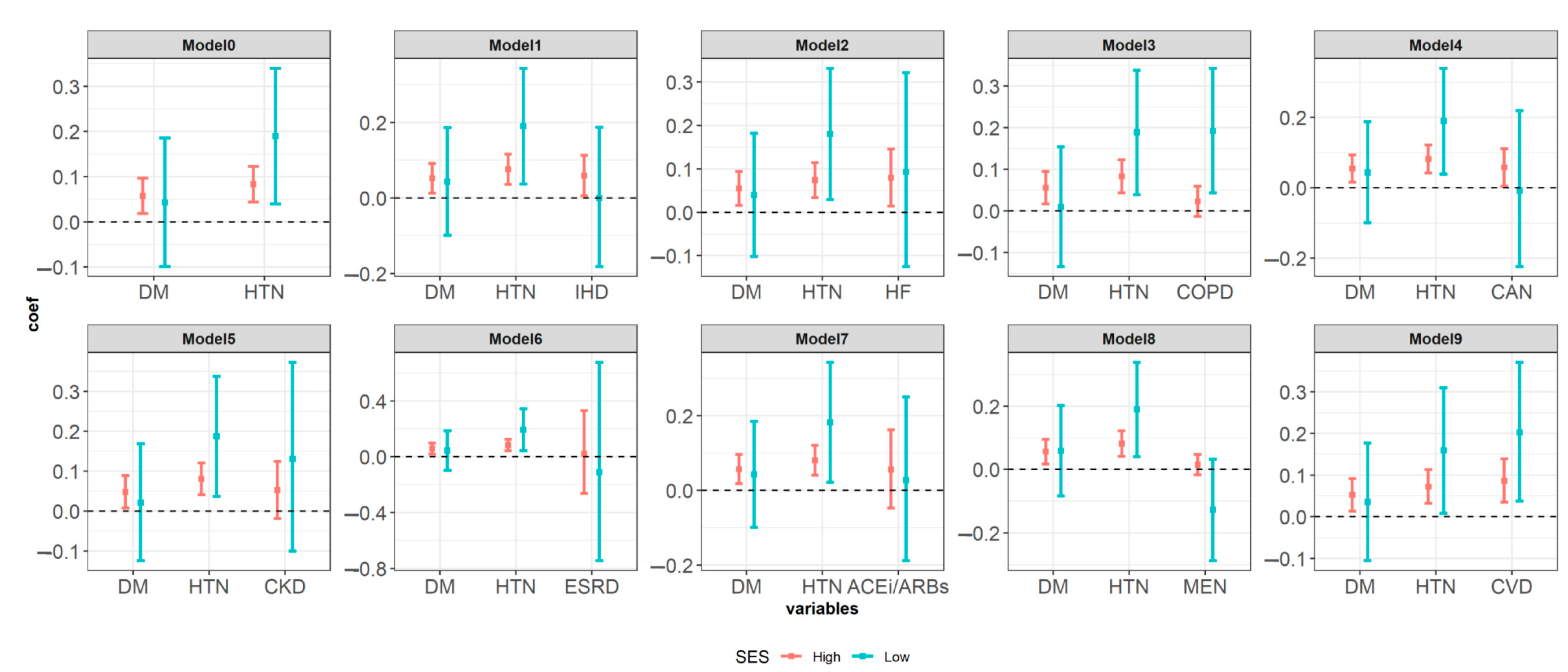
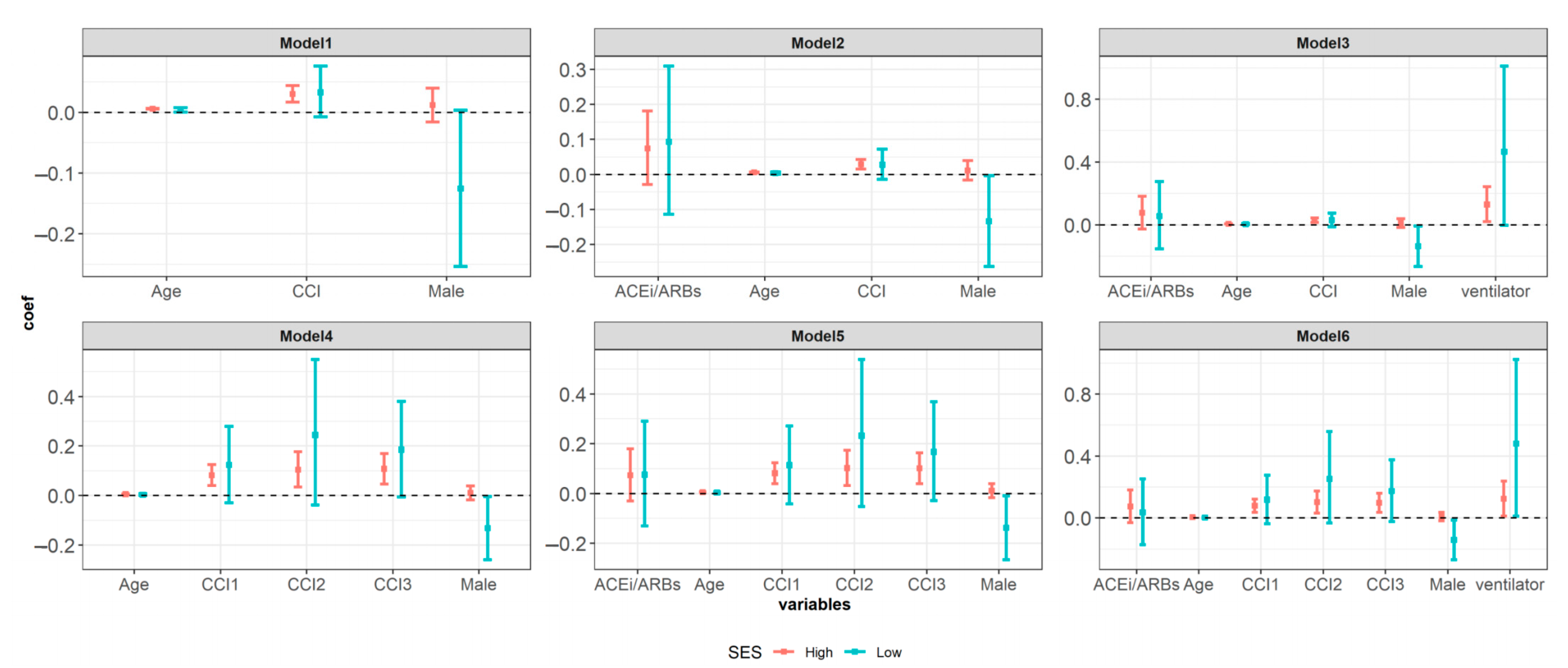
3.4. Multivariable Analysis
3.5. Subgroup Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jang, J.G.; Hur, J.; Choi, E.Y.; Hong, K.S.; Lee, W.; Ahn, J.H. Prognostic Factors for Severe Coronavirus Disease 2019 in Daegu, Korea. J. Korean Med. Sci. 2020, 35, e209. [Google Scholar] [CrossRef]
- CDC COVID-19 Response Team; Chow, N.; Fleming-Dutra, K.; Gierke, R.; Hall, A.; Hughes, M.; Pilishvili, T.; Ritchey, M.; Ritchey, K.; Skoff, T.; et al. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 382. [Google Scholar]
- Scheen, A.J.; Marre, M.; Thivolet, C. Prognostic factors in patients with diabetes hospitalized for COVID-19: Findings from the CORONADO study and other recent reports. Diabetes Metab. 2020, 46, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.H.; Ahn, H.; Ryu, H.S.; Kim, B.-J.; Jang, J.; Jung, M.; Kim, J.; Jeong, S.H. Clinical Characteristics and Disease Progression in Early-Stage COVID-19 Patients in South Korea: The Retrospective Cohort Study. SSRN Electron. J. 2020, 9, 1–19. [Google Scholar] [CrossRef]
- Pachiega, J.; Afonso, A.J.D.S.; Sinhorin, G.T.; De Alencar, B.T.; Araújo, M.D.S.M.D.; Longhi, F.G.; Zanetti, A.D.S.; Espinosa, O.A. Chronic heart diseases as the most prevalent comorbidities among deaths by COVID-19 in Brazil. Rev. Inst. Med. Trop. São Paulo 2020, 62, e45. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; Lippi, G. Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection. Int. Urol. Nephrol. 2020, 52, 1193–1194. [Google Scholar] [CrossRef]
- Parra-Bracamonte, G.M.; Lopez-Villalobos, N.; Parra-Bracamonte, F.E. Clinical characteristics and risk factors for mortality of patients with COVID-19 in a large data set from Mexico. Ann. Epidemiol. 2020, 52, 93–98.e2. [Google Scholar] [CrossRef]
- Rottoli, M.; Bernante, P.; Belvedere, A.; Balsamo, F.; Garelli, S.; Giannella, M.; Cascavilla, A.; Tedeschi, S.; Ianniruberto, S.; Del Turco, E.R.; et al. How important is obesity as a risk factor for respiratory failure, intensive care admission and death in hospitalised COVID-19 patients? Results from a single Italian centre. Eur. J. Endocrinol. 2020, 183, 389–397. [Google Scholar] [CrossRef]
- Rastad, H.; Karim, H.; Ejtahed, H.-S.; Tajbakhsh, R.; Noorisepehr, M.; Babaei, M.; Azimzadeh, M.; Soleimani, A.; Inanloo, S.H.; Hassani, N.S.; et al. Risk and predictors of in-hospital mortality from COVID-19 in patients with diabetes and cardiovascular disease. Diabetol. Metab. Syndr. 2020, 12, 1–11. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Krüger, N.; Mueller, M.A.; Drosten, C.; Pöhlmann, S. The novel coronavirus 2019 (2019-nCoV) uses the SARS-coronavirus receptor ACE2 and the cellular protease TMPRSS2 for entry into target cells. BioRxiv 2020. [Google Scholar] [CrossRef]
- Ferrario, C.M.; Jessup, J.; Chappell, M.C.; Averill, D.B.; Brosnihan, K.; Bridget Tallant, E.; Ann Diz Debra, I.; Gallagher Patricia, E. Effect of Angiotensin-Converting Enzyme Inhibition and Angiotensin II Receptor Blockers on Cardiac Angiotensin-Converting Enzyme 2. Circulation 2005, 111, 2605–2610. [Google Scholar] [CrossRef] [PubMed]
- Sommerstein, R.; Kochen, M.M.; Messerli, F.H.; Gräni, C. Coronavirus Disease 2019 (COVID-19): Do Angiotensin-Converting Enzyme Inhibitors/Angiotensin Receptor Blockers Have a Biphasic Effect? J. Am. Hear. Assoc. 2020, 9, e016509. [Google Scholar] [CrossRef]
- Gupta, R.; Hussain, A.; Misra, A. Diabetes and COVID-19: Evidence, current status and unanswered research questions. Eur. J. Clin. Nutr. 2020, 74, 864–870. [Google Scholar] [CrossRef]
- Hartmann-Boyce, J.; Morris, E.; Goyder, C.; Kinton, J.; Perring, J.; Nunan, D.; Mahtani, K.; Buse, J.B.; Del Prato, S.; Ji, L.; et al. Diabetes and COVID-19: Risks, Management, and Learnings from Other National Disasters. Diabetes Care 2020, 43, 1695–1703. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.R.; Boulton, A.J. Diabetes and COVID 19 in South-East Asia. Diabetes Res. Clin. Pract. 2020, 166, 108292. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Byrne, C.D.; Zheng, M.-H.; Targher, G. Diabetes as a risk factor for greater COVID-19 severity and in-hospital death: A meta-analysis of observational studies. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1236–1248. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Vega, M.F.; Salinas-Escudero, G.; García-Peña, C.; Gutiérrez-Robledo, L.M.; Parra-Rodríguez, L. Early estimation of the risk factors for hospitalization and mortality by COVID-19 in Mexico. PLoS ONE 2020, 15, e0238905. [Google Scholar] [CrossRef]
- Li, J.; Huang, D.Q.; Zou, B.; Yang, H.; Hui, W.Z.; Rui, F.; Yee, N.T.S.; Liu, C.; Nerurkar, S.N.; Kai, J.C.Y.; et al. Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J. Med. Virol. 2021, 93, 1449–1458. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.-C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding Algorithms for Defining Comorbidities in ICD-9-CM and ICD-10 Administrative Data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Kim, K.-H. Comparative study on three algorithms of the ICD-10 Charlson comorbidity index with myocardial infarction patients. J. Prev. Med. Public Health 2010, 43, 42–49. [Google Scholar] [CrossRef]
- Docherty, A.B.; Harrison, E.M.; Green, C.A.; Hardwick, H.E.; Pius, R.; Norman, L.; Holden, K.A.; Read, J.M.; Dondelinger, F.; Carson, G.; et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ 2020, 369, m1985. [Google Scholar] [CrossRef]
- Iftimie, S.; López-Azcona, A.F.; Vicente-Miralles, M.; Descarrega-Reina, R.; Hernández-Aguilera, A.; Riu, F.; Simó, J.M.; Garrido, P.; Joven, J.; Camps, J.; et al. Risk factors associated with mortality in hospitalized patients with SARS-CoV-2 infection. A prospective, longitudinal, unicenter study in Reus, Spain. PLoS ONE 2020, 15, e0234452. [Google Scholar] [CrossRef]
- Pan, A.; Liu, L.; Wang, C.; Guo, H.; Hao, X.; Wang, Q.; Huang, J.; He, N.; Yu, H.; Lin, X.; et al. Association of Public Health Interventions with the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA 2020, 323, 1915. [Google Scholar] [CrossRef]
- Zhang, S.-Y.; Lian, J.-S.; Hu, J.-H.; Zhang, X.-L.; Lu, Y.-F.; Cai, H.; Gu, J.-Q.; Ye, C.-Y.; Jin, C.-L.; Yu, G.-D.; et al. Clinical characteristics of different subtypes and risk factors for the severity of illness in patients with COVID-19 in Zhejiang, China. Infect. Dis. Poverty 2020, 9, 1–10. [Google Scholar] [CrossRef]
- Yu, C.; Lei, Q.; Li, W.; Wang, X.; Liu, W.; Fan, X.; Li, W. Clinical Characteristics, Associated Factors, and Predicting COVID-19 Mortality Risk: A Retrospective Study in Wuhan, China. Am. J. Prev. Med. 2020, 59, 168–175. [Google Scholar] [CrossRef]
- Zhu, Z.; Cai, T.; Fan, L.; Lou, K.; Hua, X.; Huang, Z.; Gao, G. Clinical value of immune-inflammatory parameters to assess the severity of coronavirus disease 2019. Int. J. Infect. Dis. 2020, 95, 332–339. [Google Scholar] [CrossRef]
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345–1355. [Google Scholar] [CrossRef]
- Lee, H.; Lee, J.-R.; Jung, H.; Lee, J.Y. Power of universal health coverage in the era of COVID-19: A nationwide observational study. Lancet Reg. Heal. West. Pac. 2021, 7, 100088. [Google Scholar] [CrossRef]
- Alqahtani, J.S.; Oyelade, T.; Aldhahir, A.M.; Alghamdi, S.M.; Almehmadi, M.; Alqahtani, A.S.; Quaderi, S.; Mandal, S.; Hurst, J.R. Prevalence, Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS ONE 2020, 15, e0233147. [Google Scholar] [CrossRef]
- Zhang, X.; Yu, J.; Pan, L.-Y.; Jiang, H.-Y. ACEI/ARB use and risk of infection or severity or mortality of COVID-19: A systematic review and meta-analysis. Pharmacol. Res. 2020, 158, 104927. [Google Scholar] [CrossRef]
- Wang, Q.; Zhang, Y.; Wu, L.; Niu, S.; Song, C.; Zhang, Z.; Lu, G.; Qiao, C.; Hu, Y.; Yuen, K.Y.; et al. Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell 2020, 181, 894–904.e9. [Google Scholar] [CrossRef]
- Sommerstein, R.; Gräni, C. Preventing a COVID-19 pandemic: ACE inhibitors as a potential risk factor for fatal COVID-19. BMJ 2020, 368, m810. [Google Scholar]
- Patel, A.B.; Verma, A. COVID-19 and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: What is the evidence. JAMA 2020, 323, 1769–1770. [Google Scholar] [CrossRef]
| Variables | Category | N 7590 | % | Death 225 | % | HR | 95%CI | p-Value | |
|---|---|---|---|---|---|---|---|---|---|
| Sex | Male | 3095 | 40.78 | 121 | 53.78 | 1.105 | 1.095–1.116 | <0.0001 | |
| Female | 4495 | 59.22 | 104 | 46.22 | |||||
| Age | Mean ± SD | 46.65 ± 19.76 | 1.107 | 1.096–1.117 | <0.0001 | ||||
| Age group | ~59 | 5458 | 71.91 | 16 | 7.11 | ||||
| 60~69 | 1116 | 14.7 | 32 | 14.22 | 9.956 | 5.463–18.144 | <0.0001 | ||
| 70~79 | 606 | 7.98 | 64 | 28.44 | 36.237 | 20.938–62.715 | <0.0001 | ||
| 80~99 | 343 | 4.52 | 93 | 41.33 | 99.050 | 58.244–168.446 | <0.0001 | ||
| 90~ | 67 | 0.88 | 20 | 8.89 | 85.127 | 44.053–164.498 | <0.0001 | ||
| Socioeconomic status | High | 6961 | 91.71 | 184 | 81.78 | ||||
| Low | 629 | 8.29 | 41 | 18.22 | 2.575 | 1.835–3.613 | <0.0001 | ||
| Baseline condition | |||||||||
| Underlying disease | No | 3247 | 42.78 | 2 | 0.89 | ||||
| Yes | 4343 | 57.22 | 223 | 99.11 | 86.88 | 21.60–349.53 | <0.0001 | ||
| Chronic kidney disease | No | 184 | 7229 | 95.24 | 81.78 | ||||
| Yes | 361 | 4.76 | 41 | 18.22 | 4.565 | 3.238–6.435 | <0.0001 | ||
| ESRD | No | 7570 | 99.74 | 220 | 97.78 | ||||
| Yes | 20 | 0.26 | 5 | 2.22 | 12.11 | 4.975–29.46 | |||
| KT | No | 7584 | 99.92 | 224 | 99.56 | ||||
| Yes | 6 | 0.08 | 1 | 0.44 | 5.68 | 0.80–40.55 | <0.0831 | ||
| Hypertension | No | 5633 | 74.22 | 45 | 20.00 | ||||
| Yes | 1957 | 25.78 | 180 | 80.00 | 11.56 | 8.33–16.03 | <0.0001 | ||
| Diabetic mellitus | No | 5955 | 78.46 | 82 | 36.44 | ||||
| Yes | 1635 | 21.54 | 143 | 63.56 | 6.51 | 4.96–8.55 | <0.0001 | ||
| Ischemic heart disease | No | 6290 | 91.17 | 164 | 72.89 | ||||
| Yes | 670 | 8.83 | 61 | 27.11 | 3.97 | 2.96–5.34 | <0.0001 | ||
| Heart failure | No | 7180 | 94.60 | 158 | 70.22 | ||||
| Yes | 410 | 5.40 | 67 | 29.78 | 7.71 | 5.78–10.27 | <0.0001 | ||
| Cancer | No | 7021 | 92.5 | 171 | 76.00 | ||||
| Yes | 569 | 7.5 | 54 | 24.00 | 4.06 | 2.96–5.51 | <0.0001 | ||
| COPD | No | 5778 | 76.13 | 93 | 41.33 | ||||
| Yes | 1812 | 23.87 | 132 | 58.67 | 4.56 | 3.49–5.95 | <0.0001 | ||
| Mental disorder | No | 4391 | 64.97 | 41 | 18.22 | ||||
| Yes | 2659 | 35.03 | 184 | 81.78 | 8.54 | 6.08–11.99 | <0.0001 | ||
| Cerebrovascular disease | No | 6586 | 90.33 | 142 | 63.11 | ||||
| Yes | 734 | 9.67 | 83 | 36.89 | 5.50 | 4.18–7.22 | <0.0001 | ||
| ACE inhibitor or ARBs | No | 7395 | 97.43 | 185 | 82.22 | 0.12 | 0.08–0.16 | <0.0001 | |
| Yes | 195 | 2.57 | 40 | 17.78 | |||||
| CCI | Mean ± SD | 0.505 ± 1.164 | 1.447 | 1.389–1.507 | <0.0001 | ||||
| CCI group | 0 | 5604 | 73.84 | 61 | 27.11 | ||||
| 1 | 1173 | 15.45 | 62 | 27.56 | 4.91 | 3.447–6.996 | <0.0001 | ||
| 2 | 314 | 4.14 | 18 | 8.00 | 5.359 | 3.165–9.075 | <0.0001 | ||
| 3 | 499 | 6.57 | 84 | 37.33 | 16.805 | 12.074–23.389 | <0.0001 | ||
| Events of post covid-19 Dx | |||||||||
| ICU Ventilator * | No | 7479 | 98.54 | 195 | 86.67 | ||||
| Yes | 111 | 1.46 | 30 | 38.67 | 26.75 | 20.12–35.57 | <0.0001 | ||
| Cardiac arrest | No | 7556 | 99.55 | 192 | 85.33 | ||||
| Yes | 34 | 0.45 | 33 | 14.67 | 55.74 | 38.15–81.44 | <0.0001 | ||
| Pneumonia | No | 5017 | 67.29 | 61 | 27.11 | ||||
| Yes | 2483 | 32.71 | 164 | 72.89 | 5.49 | 4.08–29.46 | <0.0001 | ||
| Arrhythmia | No | 7571 | 99.75 | 218 | 96.89 | ||||
| Yes | 19 | 0.25 | 7 | 3.11 | 12.46 | 5.86–26.5 | <0.0001 | ||
| Hospitalization | Mean ± SD | 22.71 ± 13.94 | |||||||
| Q1 (~13) | 1705 | 105 | 46.67 | ||||||
| Q2 (14~20) | 2036 | 49 | 21.78 | 0.22 | 0.15–0.31 | <0.0001 | |||
| Q3 (21~29) | 1914 | 32 | 14.22 | 0.13 | 0.08–0.20 | <0.0001 | |||
| Q4 (>29) | 1935 | 39 | 17.33 | 0.10 | 0.06–0.16 | <0.0001 | |||
| Length of ICU stay | Mean ± SD | 22.38 ± 13.92 | |||||||
| Q1 (~9) | 7469 | 181 | 80.44 | ||||||
| Q2 (10~22) | 39 | 14 | 6.22 | 22.03 | 12.75–38.07 | <0.0001 | |||
| Q3 (23~30) | 37 | 13 | 5.78 | 18.54 | 10.54–32.60 | <0.0001 | |||
| Q4 (>30) | 45 | 17 | 7.56 | 14.58 | 8.79–24.19 | <0.0001 | |||
| Medicines | |||||||||
| No medicine | 3973 | 52.35 | 25 | 11.11 | |||||
| Medicine | 3617 | 47.65 | 200 | 88.89 | 8.24 | 5.43–12.50 | <0.0001 | ||
| Hydroxychloroquine | No | 5494 | 72.38 | 85 | 37.78 | ||||
| Yes | 2096 | 27.62 | 140 | 62.22 | 3.88 | 2.96–5.08 | <0.0001 | ||
| Lopinavir/ritonavir (Kaletra) | No | 4927 | 64.91 | 67 | 29.78 | ||||
| Yes | 2663 | 35.09 | 158 | 70.22 | 4.33 | 3.25–5.77 | <0.0001 | ||
| Rivabirin | No | 7586 | 99.95 | 223 | 99.11 | ||||
| Yes | 4 | 0.05 | 2 | 0.89 | 53.33 | 13.10–217.16 | <0.0001 | ||
| Interferon | No | 7527 | 99.17 | 197 | 87.56 | ||||
| Yes | 63 | 0.83 | 28 | 12.44 | 20.07 | 13.49–29.87 | <0.0001 | ||
| Steroid | No | 7200 | 94.86 | 91 | 40.44 | ||||
| Yes | 390 | 5.14 | 134 | 59.56 | 31.05 | 23.73–40.65 | <0.0001 | ||
| Immunoglobulin (IVIG) | No | 7560 | 99.6 | 205 | 91.11 | ||||
| Yes | 30 | 0.4 | 20 | 8.89 | 31.53 | 19.89–49.98 | <0.0001 | ||
| Medicines | Hydroxychloroquine | Lopinavir/Ritonavir (Kaletra) | Rivabirin | Steroid | Immunoglobulin (IVIG) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Category | HR | 95 | CI | HR | 95 | CI | HR | 95 | CI | HR | 95 | CI | HR | 95 | CI |
| Model1 | ||||||||||||||||
| Age | 1.101 | 1.087 | 1.114 | 1.1 | 1.087 | 1.114 | 1.102 | 1.088 | 1.115 | 1.084 | 1.070 | 1.098 | 1.098 | 1.085 | 1.112 | |
| Sex | Male | 2.385 | 1.823 | 3.120 | 2.344 | 1.792 | 3.066 | 2.387 | 1.825 | 3.122 | 1.825 | 1.391 | 2.395 | 2.22 | 1.694 | 2.910 |
| Socioeconomic status | Low | 1.574 | 1.118 | 2.217 | 1.62 | 1.150 | 2.282 | 1.588 | 1.127 | 2.238 | 1.592 | 1.126 | 2.252 | 1.504 | 1.065 | 2.123 |
| Hypertension | Yes | 1.406 | 0.972 | 2.034 | 1.425 | 0.987 | 2.058 | 1.396 | 0.965 | 2.019 | 1.388 | 0.955 | 2.017 | 1.607 | 1.114 | 2.319 |
| Diabetic mellitus | Yes | 1.656 | 1.231 | 2.228 | 1.617 | 1.200 | 2.179 | 1.67 | 1.241 | 2.249 | 1.455 | 1.079 | 1.961 | 1.517 | 1.124 | 2.049 |
| Ischemic heart disease | Yes | 0.79 | 0.568 | 1.098 | 0.774 | 0.557 | 1.076 | 0.795 | 0.571 | 1.106 | 0.742 | 0.535 | 1.030 | 0.809 | 0.583 | 1.123 |
| Heart failure | Yes | 1.417 | 1.021 | 1.968 | 1.366 | 0.984 | 1.896 | 1.418 | 1.020 | 1.971 | 1.296 | 0.929 | 1.807 | 1.38 | 0.993 | 1.917 |
| Chronic obstructive pulmonary disease | Yes | 1.196 | 0.904 | 1.584 | 1.21 | 0.915 | 1.600 | 1.195 | 0.902 | 1.582 | 1.12 | 0.843 | 1.487 | 1.137 | 0.856 | 1.510 |
| Cancer | Yes | 1.539 | 1.125 | 2.106 | 1.532 | 1.121 | 2.096 | 1.543 | 1.128 | 2.112 | 1.675 | 1.221 | 2.298 | 1.677 | 1.223 | 2.299 |
| Chronic kidney disease | Yes | 1.377 | 0.963 | 1.969 | 1.327 | 0.926 | 1.901 | 1.404 | 0.982 | 2.009 | 1.236 | 0.863 | 1.772 | 1.332 | 0.929 | 1.910 |
| medicine | Yes | 1.16 | 0.879 | 1.529 | 1.614 | 1.208 | 2.157 | 17.62 | 4.273 | 72.628 | 7.175 | 5.401 | 9.530 | 5.579 | 3.435 | 9.062 |
| Model2: Model1 + ACEi/ARBs | ||||||||||||||||
| Age | 1.1 | 1.086 | 1.113 | 1.099 | 1.086 | 1.113 | 1.101 | 1.087 | 1.114 | 1.083 | 1.070 | 1.097 | 1.097 | 1.084 | 1.111 | |
| Sex | Male | 2.345 | 1.792 | 3.068 | 2.293 | 1.752 | 3.000 | 2.346 | 1.793 | 3.069 | 1.801 | 1.372 | 2.363 | 2.178 | 1.662 | 2.855 |
| Socioeconomic status | Low | 1.562 | 1.109 | 2.200 | 1.622 | 1.151 | 2.286 | 1.577 | 1.119 | 2.222 | 1.577 | 1.115 | 2.229 | 1.481 | 1.048 | 2.091 |
| Hypertension | Yes | 1.354 | 0.933 | 1.966 | 1.364 | 0.941 | 1.977 | 1.337 | 0.920 | 1.943 | 1.332 | 0.912 | 1.944 | 1.53 | 1.056 | 2.216 |
| Diabetic mellitus | Yes | 1.618 | 1.200 | 2.180 | 1.568 | 1.161 | 2.118 | 1.628 | 1.207 | 2.195 | 1.429 | 1.059 | 1.928 | 1.469 | 1.086 | 1.988 |
| Ischemic heart disease | Yes | 0.775 | 0.557 | 1.078 | 0.760 | 0.547 | 1.057 | 0.779 | 0.559 | 1.085 | 0.735 | 0.530 | 1.017 | 0.789 | 0.568 | 1.097 |
| Heart failure | Yes | 1.365 | 0.980 | 1.901 | 1.308 | 0.939 | 1.822 | 1.365 | 0.980 | 1.903 | 1.251 | 0.895 | 1.748 | 1.317 | 0.945 | 1.835 |
| Chronic obstructive pulmonary disease | Yes | 1.195 | 0.903 | 1.582 | 1.206 | 0.912 | 1.595 | 1.192 | 0.901 | 1.578 | 1.125 | 0.848 | 1.493 | 1.132 | 0.853 | 1.504 |
| Cancer | Yes | 1.549 | 1.132 | 2.118 | 1.545 | 1.130 | 2.112 | 1.555 | 1.137 | 2.127 | 1.696 | 1.237 | 2.325 | 1.695 | 1.236 | 2.323 |
| Chronic kidney disease | Yes | 1.36 | 0.951 | 1.945 | 1.311 | 0.915 | 1.877 | 1.385 | 0.968 | 1.980 | 1.205 | 0.839 | 1.729 | 1.322 | 0.923 | 1.894 |
| medicine | Yes | 1.127 | 0.853 | 1.490 | 1.630 | 1.219 | 2.180 | 18.4 | 4.461 | 75.924 | 7.138 | 5.373 | 9.483 | 5.854 | 3.600 | 9.520 |
| ACEi/ARBs | Yes | 1.448 | 1.004 | 2.088 | 1.505 | 1.046 | 2.166 | 1.487 | 1.033 | 2.141 | 1.391 | 0.967 | 2.000 | 1.577 | 1.095 | 2.272 |
| Model3: Model2 + Ventilator | ||||||||||||||||
| Age | 1.105 | 1.091 | 1.120 | 1.104 | 1.089 | 1.118 | 1.104 | 1.090 | 1.118 | 1.093 | 1.078 | 1.107 | 1.104 | 1.090 | 1.118 | |
| sex | Male | 2.226 | 1.695 | 2.925 | 2.211 | 1.683 | 2.906 | 2.235 | 1.701 | 2.937 | 1.898 | 1.443 | 2.496 | 2.239 | 1.701 | 2.947 |
| Socioeconomic status | Low | 1.965 | 1.385 | 2.788 | 1.989 | 1.400 | 2.824 | 1.967 | 1.386 | 2.791 | 1.89 | 1.329 | 2.688 | 1.961 | 1.383 | 2.783 |
| Hypertension | Yes | 1.362 | 0.944 | 1.966 | 1.344 | 0.930 | 1.941 | 1.343 | 0.930 | 1.940 | 1.319 | 0.911 | 1.910 | 1.35 | 0.934 | 1.951 |
| Diabetic mellitus | Yes | 1.343 | 0.988 | 1.824 | 1.332 | 0.980 | 1.811 | 1.346 | 0.990 | 1.829 | 1.278 | 0.943 | 1.733 | 1.348 | 0.990 | 1.835 |
| Ischemic heart disease | Yes | 0.932 | 0.668 | 1.298 | 0.927 | 0.666 | 1.292 | 0.932 | 0.669 | 1.299 | 0.854 | 0.613 | 1.191 | 0.931 | 0.668 | 1.298 |
| Heart failure | Yes | 1.072 | 0.759 | 1.513 | 1.091 | 0.774 | 1.538 | 1.1 | 0.780 | 1.552 | 1.129 | 0.799 | 1.596 | 1.091 | 0.774 | 1.538 |
| Chronic obstructive pulmonary disease | Yes | 1.068 | 0.804 | 1.418 | 1.06 | 0.799 | 1.407 | 1.059 | 0.798 | 1.406 | 1.043 | 0.785 | 1.387 | 1.063 | 0.800 | 1.411 |
| Cancer | Yes | 1.787 | 1.302 | 2.453 | 1.796 | 1.308 | 2.465 | 1.793 | 1.306 | 2.462 | 1.841 | 1.339 | 2.530 | 1.774 | 1.291 | 2.439 |
| Chronic kidney disease | Yes | 1.227 | 0.848 | 1.775 | 1.194 | 0.826 | 1.728 | 1.216 | 0.841 | 1.757 | 1.136 | 0.785 | 1.643 | 1.213 | 0.839 | 1.755 |
| medicine | Yes | 0.836 | 0.627 | 1.115 | 1.168 | 0.861 | 1.586 | 2.728 | 0.652 | 11.412 | 4.345 | 3.141 | 6.011 | 0.9 | 0.526 | 1.540 |
| ACEi/ARBs | Yes | 1.531 | 1.055 | 2.223 | 1.504 | 1.038 | 2.179 | 1.5 | 1.035 | 2.174 | 1.412 | 0.976 | 2.043 | 1.479 | 1.016 | 2.151 |
| Ventilator | Yes | 13.454 | 9.776 | 18.515 | 12.265 | 8.883 | 16.936 | 12.614 | 9.220 | 17.257 | 4.818 | 3.379 | 6.870 | 13.243 | 9.396 | 18.665 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, E.; Kim, Y.C.; Park, J.Y.; Jung, J.; Lee, J.P.; Kim, H. Evaluation of the Prognosis of COVID-19 Patients According to the Presence of Underlying Diseases and Drug Treatment. Int. J. Environ. Res. Public Health 2021, 18, 5342. https://doi.org/10.3390/ijerph18105342
Kim E, Kim YC, Park JY, Jung J, Lee JP, Kim H. Evaluation of the Prognosis of COVID-19 Patients According to the Presence of Underlying Diseases and Drug Treatment. International Journal of Environmental Research and Public Health. 2021; 18(10):5342. https://doi.org/10.3390/ijerph18105342
Chicago/Turabian StyleKim, Ejin, Yong Chul Kim, Jae Yoon Park, Jiyun Jung, Jung Pyo Lee, and Ho Kim. 2021. "Evaluation of the Prognosis of COVID-19 Patients According to the Presence of Underlying Diseases and Drug Treatment" International Journal of Environmental Research and Public Health 18, no. 10: 5342. https://doi.org/10.3390/ijerph18105342
APA StyleKim, E., Kim, Y. C., Park, J. Y., Jung, J., Lee, J. P., & Kim, H. (2021). Evaluation of the Prognosis of COVID-19 Patients According to the Presence of Underlying Diseases and Drug Treatment. International Journal of Environmental Research and Public Health, 18(10), 5342. https://doi.org/10.3390/ijerph18105342






