Higher 90-Day Mortality after Surgery for Hip Fractures in Patients with COVID-19: A Case–Control Study from a Single Center in Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Case Definition
2.3. Control Definition
2.4. Statistical Analysis
3. Results
3.1. Patient Demographic
3.2. COVID-19 Patients Characteristics
3.3. Case–Control Comparison
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). COVID-19 Dashboard. 2021. Available online: https://coronavirus.jhu.edu/map.html (accessed on 7 May 2021).
- Yanez, N.D.; Weiss, N.S.; Romand, J.A.; Treggiari, M.M. COVID-19 mortality risk for older men and women. BMC Public Health 2020, 20, 1742. [Google Scholar] [CrossRef]
- Mallapaty, S. The coronavirus is most deadly if you are older and male-new data reveal the risks. Nature 2020, 585, 16–17. [Google Scholar] [CrossRef]
- Tarantino, U.; Cariati, I.; Tancredi, V.; Casamassima, D.; Piccirilli, E.; Iundusi, R.; Gasbarra, E. State of Fragility Fractures Management during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 7732. [Google Scholar] [CrossRef]
- Macera, M.; De Angelis, G.; Sagnelli, C.; Coppola, N.; Vanvitelli Covid-Group. Clinical Presentation of COVID-19: Case Series and Review of the Literature. Int. J. Environ. Res. Public Health 2020, 17, 5062. [Google Scholar] [CrossRef]
- Beaupre, L.; Khong, H.; Smith, C.; Kang, S.; Evens, L.; Jaiswal, P.; Powell, J. The impact of time to surgery after hip fracture on mortality at 30- and 90-days: Does a single benchmark apply to all? Injury 2019, 50, 950–955. [Google Scholar] [CrossRef] [PubMed]
- Haentjens, P. Meta-analysis: Excess mortality after hip fracture among older women and men. Ann. Intern. Med. 2010, 152, 380–390. [Google Scholar] [CrossRef] [PubMed]
- Hansen, L.; Mathiesen, A.S.; Vestergaard, P.; Ehlers, L.H.; Petersen, K.D. A health economic analysis of osteoporotic fractures: Who carries the burden? Arch. Osteoporos. 2013, 8, 126. [Google Scholar] [CrossRef]
- Canton, G.; Moghnie, A.; Cleva, M.; Kostoris, F.M.; Murena, L. Dual mobility total hip arthroplasty in the treatment of femoral neck fractures: A retrospective evaluation at mid-term follow-up. Acta Biomed. 2019, 90, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Moja, L.; Piatti, A.; Pecoraro, V.; Ricci, C.; Virgili, G.; Salanti, G.; Germagnoli, L.; Liberati, A.; Banfi, G. Timing matters in hip fracture surgery: Patients operated within 48 h have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS ONE 2012, 7, e46175. [Google Scholar] [CrossRef]
- Braithwaite, R.S.; Col, N.F.; Wong, J.B. Estimating hip fracture morbidity, mortality and costs. J. Am. Geriatr. Soc. 2003, 51, 364–370. [Google Scholar] [CrossRef]
- Pincus, D.; Ravi, B.; Wasserstein, D.; Huang, A.; Paterson, J.M.; Nathens, A.B.; Kreder, H.J.; Jenkinson, R.J.; Wodchis, W.P. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. J. Am. Med. Assoc. 2017, 318, 1994–2003. [Google Scholar] [CrossRef]
- Moran, C.G.; Wenn, R.T.; Sikand, M.; Taylor, A.M. Early mortality after hip fracture: Is delay before surgery important? J. Bone Jt. Surg. Am. 2005, 87, 483–489. [Google Scholar]
- Menéndez-Colino, R.; Misis, A.G.; Alarcon, T.; Díez-Sebastián, J.; De Bustamante, M.D.; Queipo, R.; Otero, A.; González-Montalvo, J.I. Development of a new comprehensive preoperative risk score for predicting 1-year mortality in patients with hip fracture: The HULP-HF score. Comparison with 3 other risk prediction models. HIP Int. 2020. Epub ahead of print. [Google Scholar] [CrossRef]
- Clement, N.D.; Ng, N.; Simpson, C.J.; Patton, R.F.L.; Hall, A.J.; Simpson, A.H.R.W.; Duckworth, A.D. The prevalence, mortality, and associated risk factors for developing COVID-19 in hip fracture patients: A systematic review and meta-analysis. Bone Jt. Res. 2020, 9, 873–883. [Google Scholar] [CrossRef]
- Clement, N.D.; Hall, A.J.; Makaram, N.S.; Robinson, P.G.; Patton, R.F.L.; Moran, M.; MacPherson, G.J.; Duckworth, A.D.; Jenkins, P.J. IMPACT-Restart: The influence of COVID-19 on postoperative mortality and risk factors associated with SARS-CoV-2 infection after orthopaedic and trauma surgery. Bone Jt. J. 2020, 102, 1774–1781. [Google Scholar] [CrossRef]
- Haj Bloukh, S.; Edis, Z.; Shaikh, A.A.; Pathan, H.M. A Look Behind the Scenes at COVID-19: National Strategies of Infection Control and Their Impact on Mortality. Int. J. Environ. Res. Public Health 2020, 17, 5616. [Google Scholar] [CrossRef]
- Cross, M.; Ng, S.K.; Scuffham, P. Trading Health for Wealth: The Effect of COVID-19 Response Stringency. Int. J. Environ. Res. Public Health 2020, 17, 8725. [Google Scholar] [CrossRef] [PubMed]
- Benazzo, F.; Rossi, S.M.P.; Maniscalco, P.; Moretti, B.; Vaienti, E.; Ruggieri, P.; Massè, A.; Medici, A.; Formica, A.; Di Maggio, B.; et al. The orthopaedic and traumatology scenario during Covid-19 outbreak in Italy: Chronicles of a silent war. Int. Orthop. 2020, 44, 1453–1459. [Google Scholar] [CrossRef] [PubMed]
- Drago, L.; Lidgren, L.; Bottinelli, E.; Villafañe, J.H.; Berjano, P.; Banfi, G.; Romanò, C.L.; Sculco, T.P. Mapping of 303 Microbiological Procedures by the Members of the International Society of Orthopaedic Centers (ISOC) for Diagnosis of Periprosthetic Infections. J. Clin. Microbiol. 2016, 54, 1402–1403. [Google Scholar] [CrossRef]
- Chinese Clinical Guidance for COVID-19 Pneumonia Diagnosis and Treatment. Available online: https://www.acc.org/latest-in-cardiology/articles/2020/03/17/11/22/chinese-clinical-guidance-for-covid-19-pneumonia-diagnosis-and-treatment (accessed on 7 May 2021).
- WHO Reference Number: WHO/COVID-19/laboratory/2020.5. Available online: https://mca.essensys.ro/publications/m/item/molecular-assays-to-diagnose-covid-19-summary-table-of-available-protocols (accessed on 7 May 2021).
- Menendez, M.E.; Neuhaus, V.; van Dijk, N.C.; Ring, D. The Elixhauser Comorbidity Method Outperforms the Charlson Index in Predicting Inpatient Death after Orthopaedic Surgery. Clin. Orthop. Relat. Res. 2014, 472, 2878–2886. [Google Scholar] [CrossRef] [PubMed]
- Miguel, A.; Hernán, M.A. The hazards of hazard ratios. Epidemiology 2010, 21, 13–15. [Google Scholar] [CrossRef]
- Hirschmann, M.T.; Hart, A.; Henckel, J.; Sadoghi, P.; Seil, R.; Mouton, C. COVID-19 coronavirus: Recommended personal protective equipment for the orthopaedic and trauma surgeon. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 1690–1698. [Google Scholar] [CrossRef]
- Karia, M.; Gupta, V.; Zahra, W.; Dixon, J.; Tayton, E. The effect of COVID-19 on the trauma burden, theatre efficiency and training opportunities in a district general hospital: Planning for a future outbreak. Bone Jt. Open. 2020, 1, 494–499. [Google Scholar] [CrossRef]
- Catellani, F.; Coscione, A.; D’Ambrosi, R.; Usai, L.; Roscitano, C.; Fiorentino, G. Treatment of Proximal Femoral Fragility Fractures in Patients with COVID-19 during the SARS-CoV-2 Outbreak in Northern Italy. J. Bone Jt. Surg. Am. 2020, 17, e58. [Google Scholar] [CrossRef]
- Maestre-Muñiz, M.M.; Arias, Á.; Arias-González, L.; Angulo-Lara, B.; Lucendo, A.J. Prognostic Factors at Admission for In-Hospital Mortality from COVID-19 Infection in an Older Rural Population in Central Spain. J. Clin. Med. 2021, 16, 318. [Google Scholar] [CrossRef]
- Maniscalco, P.; Poggiali, E.; Quattrini, F. Proximal femur fractures in COVID-19 emergency: The experience of two Orthopedics and Traumatology Departments in the first eight weeks of the Italian epidemic. Acta Biomed. 2020, 91, 89–96. [Google Scholar] [CrossRef]
- Kayani, B.; Onochie, E.; Patil, V.; Begum, F.; Cuthbert, R.; Ferguson, D.; Bhamra, J.S.; Sharma, A.; Bates, P.; Haddad, F.S. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Jt. J. 2020, 102, 1136–1145. [Google Scholar] [CrossRef]
- Hall, A.J.; Clement, N.D.; MacLullich, A.M.J.; White, T.O.; Duckworth, A.D. IMPACT-Scot 2 report on COVID-19 in hip fracture patients. Bone Jt. J. 2021, 25, 1–10. [Google Scholar] [CrossRef]
- Wang, K.C.; Xiao, R.; Cheung, Z.B.; Barbera, J.P.; Forsh, D.A. Early mortality after hip fracture surgery in COVID-19 patients: A systematic review and meta-analysis. J. Orthop. 2020, 22, 584–591. [Google Scholar] [CrossRef]
- Citizens of the Metropolitan City of Bologna, Capital of the Emilia Romagna Region in Italy. Available online: https://statistica.regione.emilia-romagna.it/servizi-online/statistica-self-service/popolazione/popolazione-residente-dal-1861 (accessed on 7 May 2021).
- Tedesco, D.; Gibertoni, D.; Rucci, P.; Hernandez-Boussard, T.; Rosa, S.; Bianciardi, L.; Rolli, M.; Fantini, M.P. Impact of rehabilitation on mortality and readmissions after surgery for hip fracture. BMC Health Serv. Res. 2018, 18, 701. [Google Scholar] [CrossRef]
- Italian Health Ministry Report. Available online: https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_18_giugno.pdf (accessed on 7 May 2021).
- D’Ascanio, M.; Innammorato, M.; Pasquariello, L.; Pizzirusso, D.; Guerrieri, G.; Castelli, S.; Pezzuto, A.; De Vitis, C.; Anibaldi, P.; Marcolongo, A.; et al. Age is not the only risk factor in COVID-19: The role of comorbidities and of long staying in residential care homes. BMC Geriatr. 2021, 21, 63. [Google Scholar] [CrossRef]
- Grasselli, G.; Greco, M.; Zanella, A. COVID-19 Lombardy ICU Network. Risk Factors Associated with Mortality among Patients with COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345–1355. [Google Scholar] [CrossRef]
- Lohia, P.; Kapur, S.; Benjaram, S.; Pandey, A.; Mir, T.; Seyoum, B. Metabolic Syndrome and clinical outcomes in patients infected with COVID-19: Does age, sex and race of the patient with Metabolic Syndrome matter? J. Diabetes 2021, 13, 420–429. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Lim, M.A.; Pranata, R. Coronavirus disease 2019 (COVID-19) markedly increased mortality in patients with hip fracture—A systematic review and meta-analysis. J. Clin. Orthop. Trauma 2020. Epub ahead of print. [Google Scholar] [CrossRef]
- Vives, J.M.M.; Jornet-Gibert, M.; Cámara-Cabrera, J.; Esteban, P.L.; Brunet, L.; Delgado-Flores, L.; Camacho-Carrasco, P.; Torner, P.; Marcano-Fernández, F. Mortality Rates of Patients with Proximal Femoral Fracture in a Worldwide Pandemic: Preliminary Results of the Spanish HIP-COVID Observational Study. J. Bone Jt. Surg. Am. 2020, 102, e69. [Google Scholar] [CrossRef]
- Grassi, A.; Pizza, N.; Tedesco, D.; Zaffagnini, S. The COVID-19 outbreak in Italy: Perspectives from an orthopaedic hospital. Int. Orthop. 2020, 44, 1543–1547. [Google Scholar] [CrossRef]
| Variables Types | Variables | COVID-19 (n = 14) | Non-COVID-19 (n = 42) | p-Value |
|---|---|---|---|---|
| Matching variables | Sex; n (%) | 13 (93%), F | 39 (93%), F | >0.05 |
| 1 (7%), M | 3 (7%), M | |||
| Age; mean (SD), year | 82.9 (7.1) | 83.1 (6.6) | >0.05 | |
| ECI; n (%), comorbidities | 5 (36%), 0–1 | 15 (36%), 0–1 | >0.05 | |
| 9 (64%), ≥2 | 27 (64%), ≥2 | |||
| ICD-9-CM; n (%), code | 1 (7%), 79.15 | 3 (7%), 79.15 | >0.05 | |
| 6 (43%), 79.35 | 18 (43%), 79.35 | |||
| 2 (14%), 81.51 | 6 (4%), 81.51 | |||
| 5 (36%), 81.52 | 15 (36%), 81.52 | |||
| Descriptive variables | Diagnosis; n (%) | 7 (50%) femoral neck fractures | 21 (50%) femoral neck fractures | 1.000 |
| 7 (50%) intertrochanteric fractures | 21 (50%) intertrochanteric fractures | |||
| Procedure; n (%) | 5 (36%) hip endoprosthesis | 14 (33%) hip endoprosthesis | 0.856 | |
| 6 (43%) intramedullary femoral nail | 20 (47%) intramedullary femoral nail | |||
| 2 (14%) THA | 7 (17%) THA | |||
| 1 (7%) ORIF | 1 (3%) ORIF | |||
| Surgery time; mean (SD), minutes | 67.6 (25.0) | 69.0 (20.2) | 0.844 | |
| ASA; n (%) | 12 (86%) ASA 3 | 37 (88%) ASA 3 | 0.943 | |
| 1 (7%) ASA 4 | 2 (5%) ASA 4 | |||
| 1 (7%) ASA 2 | 3 (7%) ASA 2 | |||
| Fracture–surgery interval; mean (SD), days | 3.2 (2.4) | 2.8 (2.4) | 0.584 | |
| Admission–surgery interval; mean (SD), days | 2.7 (2.6) | 1.9 (1.5) | 0.168 | |
| Smokers; n (%) | 4 (29%) | 9 (21%) | 0.415 |
| Main Comorbidity | COVID-19 (n = 14) | Non-COVID-19 (n = 42) | p-Value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Cardiac arrhythmia | 6 | 42.9% | 8 | 19.0% | 0.080 |
| Chronic pulmonary disease | 4 | 28.6% | 3 | 7.1% | 0.058 |
| Hypertension uncomplicated | 3 | 21.4% | 16 | 38.1% | 0.210 |
| Dementia | 3 | 21.4% | 11 | 26.2% | 0.512 |
| Congestive heart failure | 2 | 14.3% | 6 | 14.3% | 0.651 |
| Solid tumor without metastasis | 1 | 7.1% | 7 | 16.7% | 0.349 |
| Diabetes uncomplicated | 1 | 7.1% | 4 | 9.5% | 0.633 |
| Depression | 1 | 7.1% | 4 | 9.5% | 0.633 |
| Hypothyroidism | 1 | 7.1% | 3 | 7.1% | 0.695 |
| Fluid and electrolyte disorders | 1 | 7.1% | 2 | 4.8% | 0.586 |
| Diabetes complicated | 1 | 7.1% | 0 | 0.0% | 0.250 |
| Liver disease | 1 | 7.1% | 0 | 0.0% | 0.250 |
| Deficiency anemia | 1 | 7.1% | 0 | 0.0% | 0.250 |
| Other neurological disorders | 0 | 0.0% | 6 | 14.3% | 0.162 |
| Valvular disease | 0 | 0.0% | 5 | 11.9% | 0.223 |
| Renal failure | 0 | 0.0% | 3 | 7.1% | 0.414 |
| Blood loss anemia | 0 | 0.0% | 3 | 7.1% | 0.414 |
| Hypertension complicated | 0 | 0.0% | 3 | 7.1% | 0.414 |
| Metastatic cancer | 0 | 0.0% | 1 | 2.4% | 0.750 |
| Rheumatoid arthritis/collagen | 0 | 0.0% | 1 | 2.4% | 0.750 |
| Obesity | 0 | 0.0% | 1 | 2.4% | 0.750 |
| Peripheral vascular disorders | 0 | 0.0% | 1 | 2.4% | 0.750 |
| Patient | ASA | Comorbidities | Orthopedic Diagnosis and Treatment | Admission–Surgery Interval | Length of Hospitalization | COVID-19 Diagnosis | Timing of Diagnosis | Clinical Symptoms | Laboratory Test Alterations | ABG Results | HRCT | Treatment | Exitus |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F, 90 y | II | HT, CHD, K | Femoral neck fracture Hip endoprosthesis | 1 day | 9 | Positive RT-PCR molecular test | Admission | Fever for 5 days | LC: Y; LP: N; LyP: N; PLT: 227; C: 0.73; IL-6: NA; LDH: NA; PCR: 15 | NA | NEG | O2, LMWH, Antibiotic | no |
| F, 81 y | III | HT, COPD, D | Femoral neck fracture THA | 1 day | 22 | Positive RT-PCR molecular test | 22 days | Asymptomatic | LC: Y; LP: N; LyP: N; PLT: 400; C: 1.6; IL-6: NA; LDH: NA; PCR: 1.6 | NA | NEG | LMWH, Antibiotic | no |
| F, 90 y | II | HT, DM, CHD | Intertrochanteric fracture Femoral intramedullary nail | 1 day | 10 | Positive RT-PCR molecular test | 11 days | Asymptomatic | LC: N; LP: N; LyP: N; PLT: 265; C: 0.58; IL-6: NA; LDH: NA; PCR: 5.9 | SaO2: 93; PaO2: 52; PaCO2: 34; PF: 267 | NEG | LMWH | no |
| F, 73 y | III | HT, COPD, K | Femoral neck fracture THA | 2 days | 8 | Positive RT-PCR molecular test | Admission | Fever for 3 days Cough Desaturation | LC: Y; LP: N; LyP: Y; PLT: 248; C: 0.74; IL-6: NA; LDH: 336; PCR: 3.7 | SaO2: 96; PaO2: 60; PaCO2: 33; PF: 286 | NEG | O2, CPAP, HCQ, LMWH | no |
| F, 70 y | III | K | Intertrochanteric fracture Femoral intramedullary nail | 2 days | 11 | Clinical criteria | 2 days | Desaturation | LC: Y; LP: N; LyP: N; PLT: 420; C: 0.53; IL-6: NA; LDH: 232; PCR: 1.6 | SaO2: 91; PaO2: 80; PaCO2: 23; PF: 857 | POS | O2, HCQ, AZA, LMWH, Antibiotic | no |
| F, 72 y | III | HT, COPD | Femoral neck fracture Hip endoprosthesis | 8 days | 14 | Positive RT-PCR molecular test | 11 days | Asymptomatic | LC: N; LP: N; LyP: N; PLT: 87; C: 1.27; IL-6: NA; LDH: 228; PCR: 24 | NA | NEG | LMWH, Antibiotic | no |
| F, 86 y | IV | HT, D, K | Intertrochanteric fracture Femoral intramedullary nail | 3 days | 8 | Positive RT-PCR molecular test | Admission | Fever Cough | LC: N; LP: N; LyP: Y; PLT: 260; C: 0.85; IL-6: 66.6; LDH: NA; PCR: 4.6 | SaO2: 98; PaO2: 69; PaCO2: 32; PF: 328 | POS | O2, HCQ, AZA, LMWH, Antibiotic | no |
| F, 80 y | III | HT, S, COPD, D | Femoral neck fracture Hip endoprosthesis | 2 days | 11 | Positive RT-PCR molecular test | 2 days | Asymptomatic | LC: N; LP: N; LyP: N; PLT: 123; C: 0.89; IL-6: NA; LDH: NA; PCR: 5.6 | SaO2: 91; PaO2: 68; PaCO2: 45; PF: 283 | NEG | O2, HCQ, LMWH | no |
| F, 86 y | III | HT | Intertrochanteric fracture Femoral intramedullary nail | 1 day | 8 | Positive RT-PCR molecular test | Admission | Asymptomatic | LC: N; LP: N; LyP: N; PLT: 278; C: 0.64; IL-6: NA; LDH: NA; PCR: NA | SaO2: 98; PaO2: 94; PaCO2: 34; PF: 448 | NEG | HCQ, LMWH | no |
| F, 90 y | IV | HT, COPD, D, K | Femoral neck fracture Hip endoprosthesis | 7 days | 10 | Positive RT-PCR molecular test | Admission | Cough | LC: N; LP: N; LyP: Y; PLT: 368; C: 0.53; IL-6: NA; LDH: NA; PCR: NA | SaO2: 98; PaO2: 71;PaCO2: 44; PF: 371 | NEG | O2, LMWH | Yes (14-day postop) |
| F, 89 y | III | DM, CHD, COPD, D | Intertrochanteric fracture Femoral intramedullary nail | 1 day | 7 | Positive RT-PCR molecular test | 8 days | Asymptomatic | LC: N; LP: N; LyP: N; PLT: 272; C: 0.73; IL-6: NA; LDH: NA; PCR: 5.6 | NA | NEG | LMWH | Yes (33-day postop) |
| F, 87 y | IV | CHD, COPD, D | Intertrochanteric fracture Femoral intramedullary nail | 9 days | 10 | Clinical criteria | 2 days | Fever for 3 days | LC: Y; LP: N; LyP: Y; PLT: 189; C: 0.69; IL-6: NA; LDH: 379; PCR: 26 | SaO2: 83; PaO2: 48; PaCO2: 68; PF: 229 | POS | O2, CPAP, HCQ, AZA, LMWH, Antibiotic | Yes (1-day postop) |
| F, 88 y | III | HT, DM, CHD, D, K | Femoral neck fracture Hip endoprosthesis | 1 day | 10 | Positive RT-PCR molecular test | 4 days | Dyspnea for 6 days | LC: N; LP: N; LyP: Y; PLT: 186; C: 1.20; IL-6: NA; LDH: NA; PCR: 8 | SaO2: 86; PaO2: 44; PaCO2: 31; PF: 210 | NEG | O2, LMWH | Yes (9-day postop) |
| M, 79 y | III | COPD, D | Femoral neck fracture ORIF | 0 days | 21 | Clinical criteria | 10 days | Fever for 11 days Dyspnea Desaturation | LC: Y; LP: N; LyP: Y; PLT: 300; C: 1.6; IL-6: 78; LDH: NA; PCR: 40 | SaO2: 80; PaO2: 53; PaCO2: 31; PF: 252 | POS | O2, CPAP, LMWH, Antibiotic | Yes (21-day postop) |
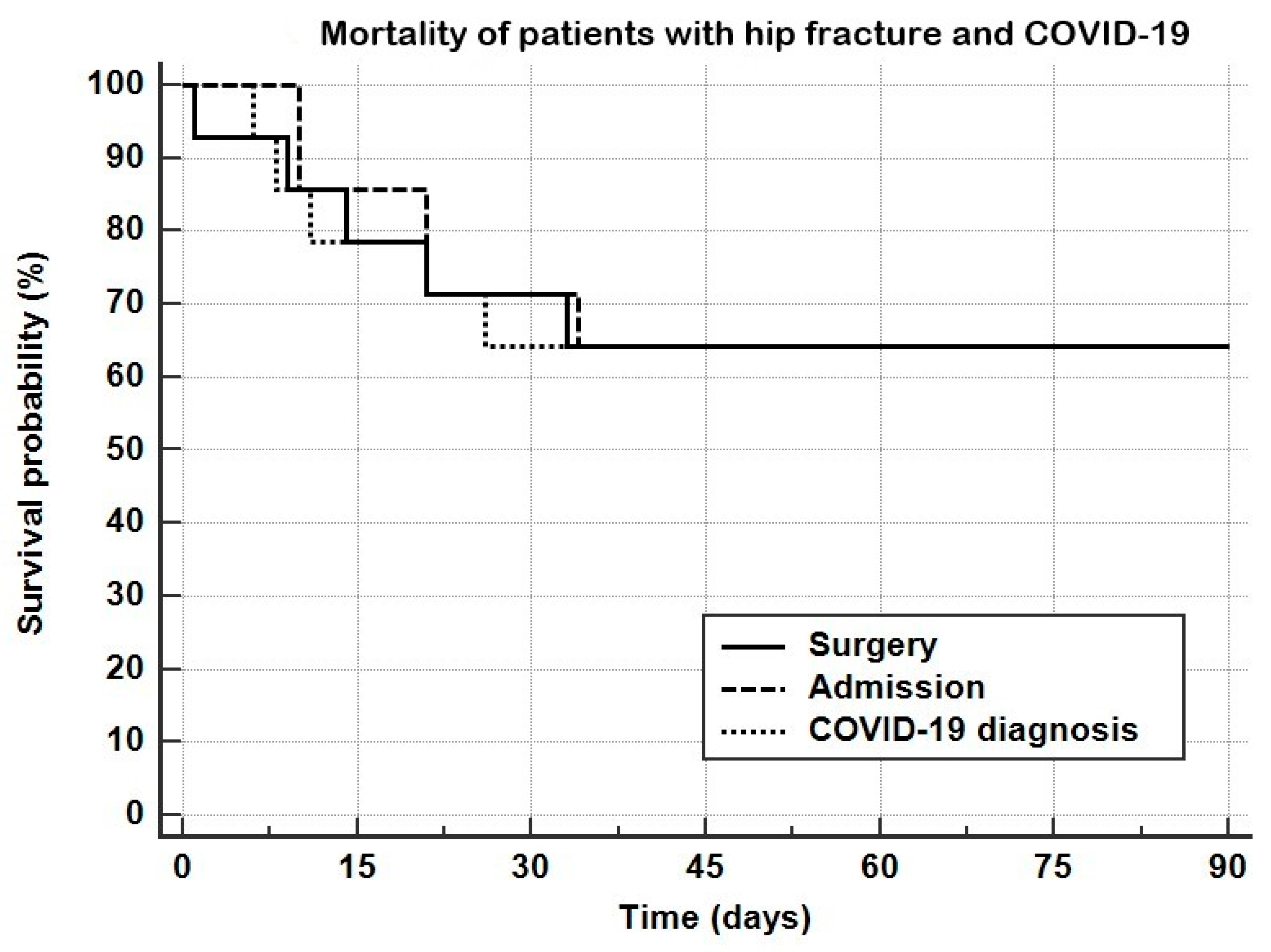
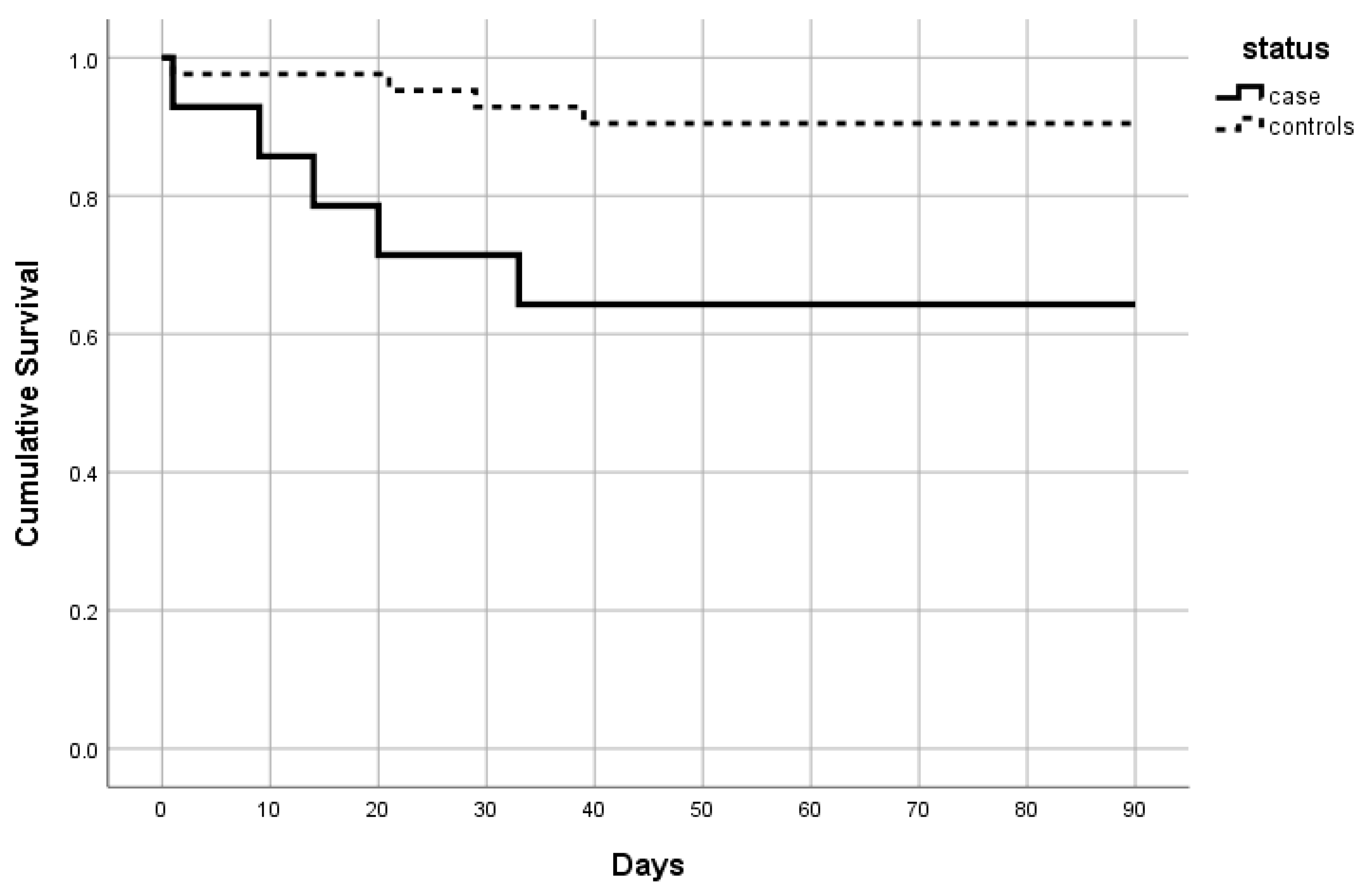
| Time Points and Outcome Measures | Mortality Rates and Risk Measures | |||||
|---|---|---|---|---|---|---|
| 7-Day | 14-Day | 30-Day | 45-Day | 90-Day | ||
| Mortality rate | COVID-19 Positive | |||||
| Time from Admission | 0.0% | 14.3% | 28.6% | 35.7% | 35.7% | |
| Time from Surgery | 7.1% | 21.4% | 28.6% | 35.7% | 35.7% | |
| Time from COVID-19 Diagnosis | 7.1% | 21.4% | 35.7% | 35.7% | 35.7% | |
| Control Group | ||||||
| Admission | 2.4% | 2.4% | 7.1% | 9.5% | 9.5% | |
| Surgery | 2.4% | 2.4% | 7.1% | 9.5% | 9.5% | |
| 7-day | 14-day | 30-day | 45-day | 90-day | ||
| Risk Measures | Hazard Ratios | |||||
| Value | 3.1 | 9.6 | 4.5 | 4.5 | 4.5 | |
| 95% CI | 0.12–78.0 | 0.9–95.6 | 1.0–20.2 | 1.2–16.7 | 1.2–16.7 | |
| p-Value | =0.3972 | =0.0766 | =0.0490 * | =0.0250 * | =0.0250 * | |
| Odds Ratios | ||||||
| Value | 3.1 | 11.2 | 5.2 | 5.2 | 5.2 | |
| 95% CI | 0.2–54.0 | 1.1–119.3 | 1.0–27.1 | 1.2–23.7 | 1.2–23.7 | |
| p-Value | =0.4281 | =0.0449 * | =0.0502 | =0.0300 * | =0.0300 * | |
| 90-Day Survival | Patients’ Characteristics | COVID-19 Cases (n = 14) | Controls (n = 42) |
|---|---|---|---|
| Alive (%) | 9 (64.3) | 38 (90.5) | |
| Mean age (SD) | 80.8 (7.7) | 82.5 (6.6) | |
| Female (%) | 9 (100) | 35 (92.1) | |
| Mean ECI (SD) | 1.7 (1.5) | 2.1 (1.9) | |
| Deceased (%) | 5 (35.7) | 4 (9.5) | |
| Mean age (±SD) | 86.6 (4.4) | 89.0 (1.4) | |
| Female (%) | 4 (80) | 4 (100) | |
| Mean ECI (SD) | 2.2 (1.1) | 1.5 (1.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grassi, A.; Andriolo, L.; Golinelli, D.; Tedesco, D.; Rosa, S.; Gramegna, P.; Ciaffi, J.; Meliconi, R.; Landini, M.P.; Filardo, G.; et al. Higher 90-Day Mortality after Surgery for Hip Fractures in Patients with COVID-19: A Case–Control Study from a Single Center in Italy. Int. J. Environ. Res. Public Health 2021, 18, 5205. https://doi.org/10.3390/ijerph18105205
Grassi A, Andriolo L, Golinelli D, Tedesco D, Rosa S, Gramegna P, Ciaffi J, Meliconi R, Landini MP, Filardo G, et al. Higher 90-Day Mortality after Surgery for Hip Fractures in Patients with COVID-19: A Case–Control Study from a Single Center in Italy. International Journal of Environmental Research and Public Health. 2021; 18(10):5205. https://doi.org/10.3390/ijerph18105205
Chicago/Turabian StyleGrassi, Alberto, Luca Andriolo, Davide Golinelli, Dario Tedesco, Simona Rosa, Pasquale Gramegna, Jacopo Ciaffi, Riccardo Meliconi, Maria Paola Landini, Giuseppe Filardo, and et al. 2021. "Higher 90-Day Mortality after Surgery for Hip Fractures in Patients with COVID-19: A Case–Control Study from a Single Center in Italy" International Journal of Environmental Research and Public Health 18, no. 10: 5205. https://doi.org/10.3390/ijerph18105205
APA StyleGrassi, A., Andriolo, L., Golinelli, D., Tedesco, D., Rosa, S., Gramegna, P., Ciaffi, J., Meliconi, R., Landini, M. P., Filardo, G., Fantini, M. P., & Zaffagnini, S. (2021). Higher 90-Day Mortality after Surgery for Hip Fractures in Patients with COVID-19: A Case–Control Study from a Single Center in Italy. International Journal of Environmental Research and Public Health, 18(10), 5205. https://doi.org/10.3390/ijerph18105205






