Prioritizing Built Environmental Factors to Tackle Chronic and Infectious Diseases in Remote Northern Territory (NT) Communities of Australia: A Concept Mapping Study
Abstract
1. Introduction
- (1)
- consolidate built environmental indicators relevant to the development of chronic disease and infectious disease;
- (2)
- engage stakeholders to sort a set of consolidated built environmental indicators into conceptually meaningful groupings;
- (3)
- engage stakeholders to rate a set of consolidated built environmental indicators on perceived importance in relation to their influence on chronic disease and infectious disease; and
- (4)
- engage stakeholder organizations in the interpretation and utilization of the results to further inform environmental public health practice in remote Indigenous communities in the NT.
2. Materials and Methods
2.1. Study Context
2.2. Research Approach
2.3. Study Design: Concept Mapping
2.3.1. Preparation
2.3.2. Brainstorming
A list of built environmental living conditions that contribute to the development of preventable chronic disease and infectious disease in remote Indigenous communities is given below. This information is taken and summarized from the publicly available planning documents that were developed through community consultations. Please review the following list and refine/add further built environmental living conditions that you think contribute to the development of chronic disease and infectious diseases in Indigenous communities where you live and/or work ….
2.3.3. Sorting
2.3.4. Rating
Rating activity—chronic disease: For Aboriginal and Torres Strait Islander people living in remote communities, please rate on a scale of 1 to 5 how important each of the following statements are in relation to their influence on chronic disease (e.g., type 2 diabetes, kidney disease, heart disease). The influence of the environment on chronic disease can be direct or indirect.
Rating activity—infectious disease: For Aboriginal and Torres Strait Islander people living in remote communities, please rate on a scale of 1 to 5 how important each of the following statements are in relation to their influence on infectious disease (e.g., skin infection, ear infection, respiratory infection). The influence of the environment on infectious disease can be direct or indirect.
2.3.5. Analysis
2.3.6. Interpretation and Utilization
3. Results
3.1. Participant Characteristics
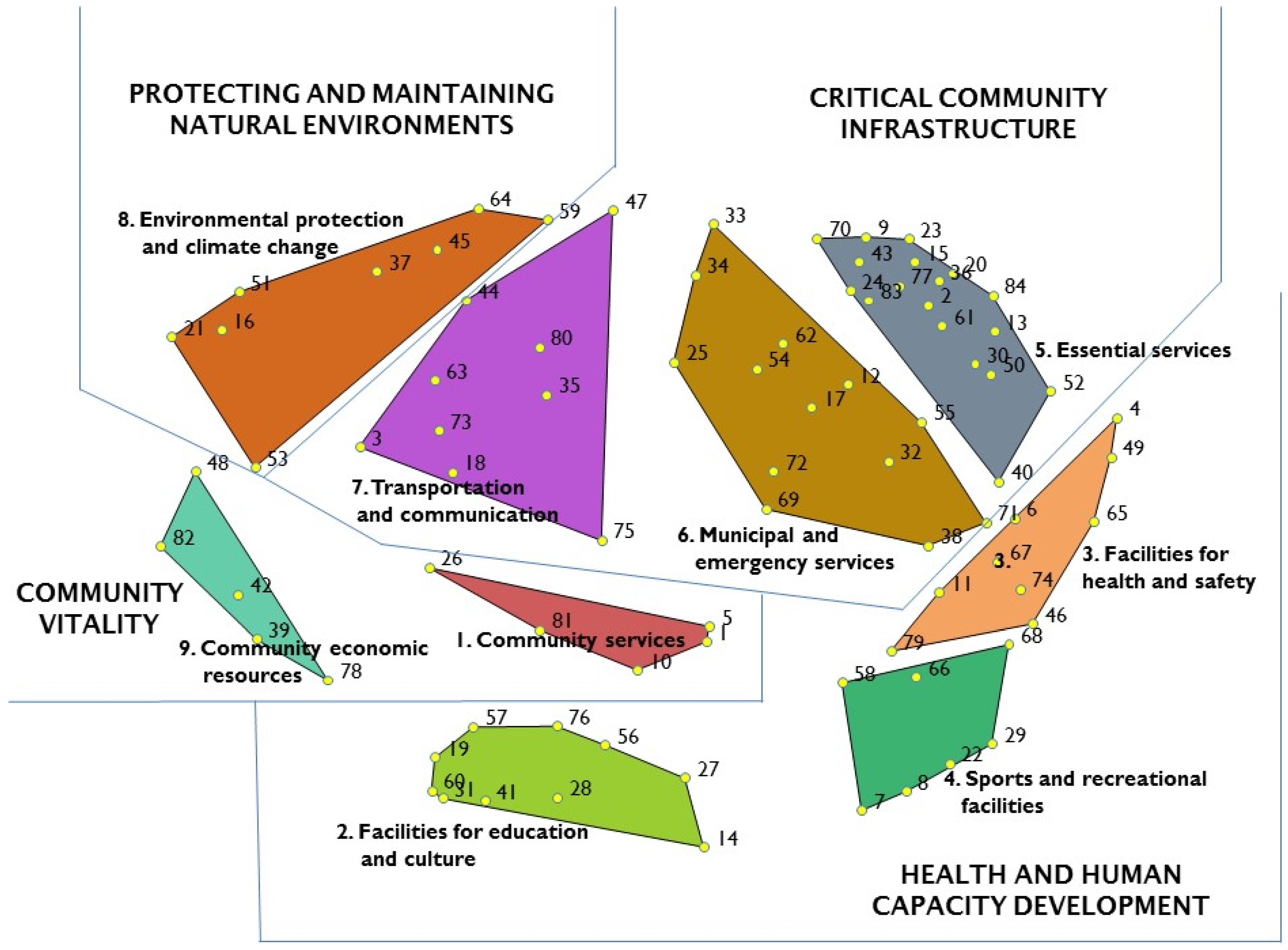
3.2. Sorting
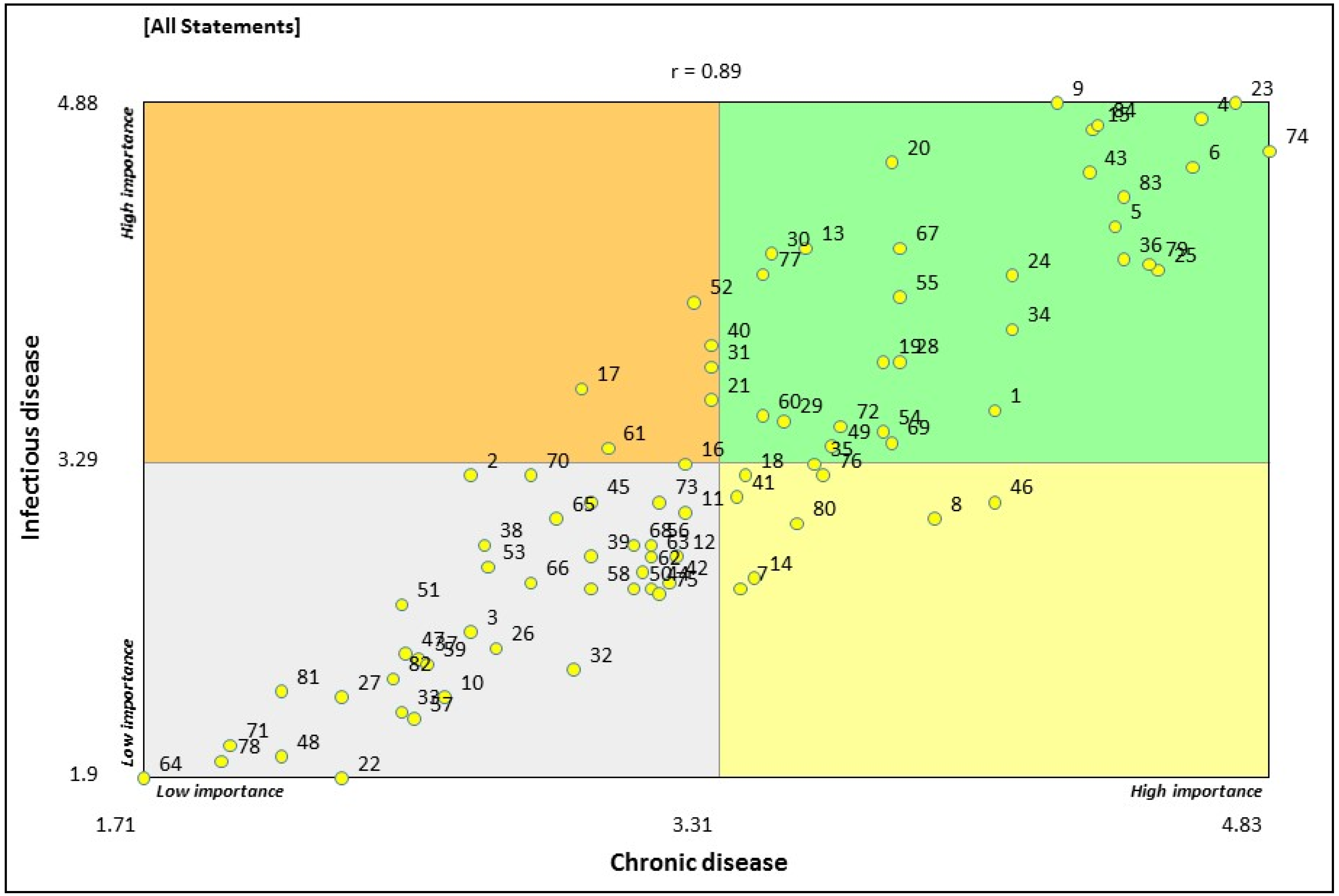
3.3. Rating
4. Discussion
4.1. Implications for Public and Environmental Health Policy and Practice
4.2. Strengths
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Prüss-Üstün, A.; Wolf, J.; Corvalán, C.; Bos, R.; Neira, M. Preventing Disease through Healthy Environments: A Global Assessment of the Burden of Disease from Environmental Risks; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Aboriginal and Torres Strait Islander Social Justice Commissioner. Social Justice Report 2005; Report No. 3/2005; Australian Human Rights Commission: Canberra, Australia, 2005.
- Aboriginal and Torres Strait Islander Social Justice Commissioner. Social Justice and Native Title Report 2015; Human Rights Commission: Canberra, Australia, 2015.
- Paradies, Y.; Cunningham, J. Placing Aboriginal and Torres Strait Islander Mortality in an International Context. Aust. N. Z. J. Public Health 2002, 26, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Anderson, I.; Crengle, S.; Kamaka, M.L.; Chen, T.-H.; Palafox, N.; Jackson-Pulver, L. Indigenous Health in Australia, New Zealand, and the Pacific. Lancet 2006, 367, 1775–1785. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. The Health and Welfare of Australia’s Aboriginal and Torres Strait IslanderPeoples: 2015; Report No. IHW 147; AIHW: Canberra, Australia, 2015.
- Vos, T.; Barker, B.; Begg, S.; Stanley, L.; Lopez, A.D. Burden of Disease and Injury in Aboriginal and Torres Strait Islander Peoples: The Indigenous Health Gap. Int. J. Epidemiol. 2009, 38, 470–477. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Mortality Inequalities in Australia 2009–2011; Bulletin No. 124; AIHW: Canberra, Australia, 2014.
- Zhao, Y.; You, J.; Wright, J.; Guthridge, S.L.; Lee, A.H. Health Inequity in the Northern Territory, Australia. Int. J. Equity Health 2013, 12, 79. [Google Scholar] [CrossRef]
- Gracey, M.; King, M. Indigenous Health Part 1: Determinants and Disease Patterns. Lancet 2009, 374, 65–75. [Google Scholar] [CrossRef]
- Saggers, S.; Gray, D. Aboriginal Health and Society: The Traditional and Contemporary Aboriginal Struggle for Better Health; Allen & Unwin, Crows Nest: Sydney, Australia, 1991. [Google Scholar]
- Daniel, M.; Lekkas, P.; Cargo, M.; Stankov, I.; Brown, A. Environmental Risk Conditions and Pathways to Cardiometabolic Diseases in Indigenous Populations. Annu. Rev. Public Health 2011, 32, 327–347. [Google Scholar] [CrossRef]
- Gray, C.; Brown, A.; Thomson, N. Review of Cardiovascular Health among Indigenous Australians. Diabetes Care 2012, 23, 1794–1798. [Google Scholar]
- Ejere, H.; Alhassan, M.B.; Rabiu, M. Face Washing Promotion for Preventing Active Trachoma. Cochrane Database Syst. Rev. 2004, 3. [Google Scholar] [CrossRef]
- McDonald, E.; Bailie, R.; Brewster, D.; Morris, P. Are Hygiene and Public Health Interventions Likely to Improve Outcomes for Australian Aboriginal Children Living in Remote Communities? A Systematic Review of the Literature. BMC Public Health 2008, 8, 1–14. [Google Scholar] [CrossRef]
- Rose, G. Sick Individuals and Sick Populations. Int. J. Epidemiol. 2001, 30, 427–432. [Google Scholar] [CrossRef]
- Marmot, M. The Health Gap: The Challenge of an Unequal World. Lancet 2015, 386, 2442–2444. [Google Scholar] [CrossRef]
- Australian Institute of Health and Walfare. Health and the Environment: A Compilation of Evidence; Cat. no. PHE 136; AIHW: Canberra, Australia, 2011.
- Frank, L.D.; Saelens, B.E.; Powell, K.E.; Chapman, J.E. Stepping Towards Causation: Do Built Environments or Neighborhood and Travel Preferences Explain Physical Activity, Driving, and Obesity? Soc. Sci. Med. 2007, 65, 1898–1914. [Google Scholar] [CrossRef]
- Saelens, B.E.; Sallis, J.F.; Frank, L.D. Environmental Correlates of Walking and Cycling: Findings from the Transportation, Urban Design, and Planning Literatures. Ann. Behav. Med. 2003, 25, 80–91. [Google Scholar] [CrossRef]
- Høj, S.B.; Paquet, C.; Caron, J.; Daniel, M. Relative ‘Greenness’ and not Availability of Public Open Space Buffers Stressful Life Events and Longitudinal Trajectories of Psychological Distress. Health Place 2021, 68, 102501. [Google Scholar] [CrossRef]
- Carroll, S.J.; Dale, M.J.; Taylor, A.W.; Daniel, M. Contributions of Multiple Built Environment Features to 10-Year Change in Body Mass Index and Waist Circumference in a South Australian Middle-Aged Cohort. Int. J. Environ. Res. Public Health 2020, 17, 870. [Google Scholar] [CrossRef]
- Gal, C.L.; Dale, M.J.; Cargo, M.; Daniel, M. Built Environments and Cardiometabolic Morbidity and Mortality in Remote Indigenous Communities in the Northern Territory, Australia. Int. J. Environ. Res. Public Health 2020, 17, 769. [Google Scholar] [CrossRef]
- Carroll, S.J.; Turrell, G.; Dale, M.J.; Daniel, M. Associations between Supermarket Availability and Body Sze in Australia: A Cross-sectional Observational Study Comparing State and Territory Capital Cities. BMC Public Health 2021, 21, 407. [Google Scholar] [CrossRef]
- Ali, S.H.; Foster, T.; Hall, N.L. The Relationship between Infectious Diseases and Housing Maintenance in Indigenous Australian Households. Int. J. Environ. Res. Public Health 2018, 15, 2827. [Google Scholar] [CrossRef]
- Coffey, P.M.; Ralph, A.P.; Krause, V.L. The Role of Social Determinants of Health in the Risk and Prevention of Group A Streptococcal Infection, Acute Rheumatic Fever and Rheumatic Heart Disease: A Systematic Review. PLoS Negl. Trop. Dis. 2018, 12, e0006577. [Google Scholar] [CrossRef]
- Edmond, K.; Scott, S.; Korczak, V.; Ward, C.; Sanderson, C.; Theodoratou, E.; Clark, A.; Griffiths, U.; Rudan, I.; Campbell, H. Long Term Sequelae from Childhood Pneumonia; Systematic Review and Meta-analysis. PLoS ONE 2012, 7, e31239. [Google Scholar] [CrossRef]
- Cunningham, M.W. Autoimmunity and Molecular Mimicry in the Pathogenesis of Post-streptococcal Heart Disease. Front. Biosci. 2003, 8, S533–S543. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, J. Tackling Drug-resistant Infections Globally: Final Report and Recommendations: Review on Antimicrobial Resistance; HM Government and Welcome Trust: London, UK, 2016.
- Department of Health. Australian Health Sector Emergency Response Plan for Novel Corronavirus (COVID-19): Management and Operational Plan for Aborginal and Torres Strait Islander Populations Canberra: Australian Government. 2020. Available online: https://www.health.gov.au/sites/default/files/documents/2020/07/management-plan-for-aboriginal-and-torres-strait-islander-populations.pdf (accessed on 27 January 2021).
- Productivity Commission. Indigenous Evaluation Strategy; Australian Government: Canberra, Australia, 2020.
- Australian Institute of Health and Welfare. Rural Regional and Remote Health: A Guide to Remoteness Classifications; AIHW: Canberra, Australia, 2004.
- ABS. 2016 Census of Population and Housing, Northern Territory: Aboriginal and Torres Strait Islander Peoples Profile: Australian Bureau of Statistics (ABS). 2016. Available online: https://www.abs.gov.au/websitedbs/D3310114.nsf/Home/2016%20search%20by%20geography (accessed on 12 December 2020).
- Graham, I.D.; Kothari, A.; McCutcheon, C. Moving Knowledge into Action for more Effective Practice, Programmes and Policy: Protocol for a Research Programme on Integrated Knowledge Translation. Implement. Sci. 2018, 13, 22. [Google Scholar] [CrossRef] [PubMed]
- Kothari, A.; McCutcheon, C.; Graham, I.D. Defining Integrated Knowledge Translation and Moving Forward: A Response to Recent Commentaries. Int. J. Health Policy Manag. 2017, 6, 299. [Google Scholar] [CrossRef] [PubMed]
- Trochim, W.M.; McLinden, D. Introduction to a Special Issue on Concept Mapping. Eval. Program Plan. 2017, 60, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Trochim, W.M. Hindsight is 20/20: Reflections on the Evolution of Concept Mapping. Eval. Program Plan. 2017, 60, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, L.M.; Jones, J.R.; Booth, E.; Burke, J.G. Concept Mapping Methodology and Community-Engaged Research: A Perfect Pairing. Eval. Program Plan. 2017, 60, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Kane, M.; Trochim, W.M. Concept Mapping for Planning and Evaluation; Sage: Thousand Oaks, CA, USA, 2007. [Google Scholar]
- Dawson, A.P.; Cargo, M.; Stewart, H.; Chong, A.; Daniel, M. Aboriginal Health Workers Experience Multilevel Barriers to Quitting Smoking: A Qualitative Study. Int. J. Equity Health 2012, 11, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Stankov, I.; Howard, N.; Daniel, M.; Cargo, M. Policy, Research and Residents’ Perspectives on Built Environments Implicated in Heart Disease: A Concept Mapping Approach. Int. J. Environ. Res. Public Health 2017, 14, 170. [Google Scholar] [CrossRef]
- Cargo, M.; Potaka-Osborne, G.; Cvitanovic, L.; Warner, L.; Clarke, S.; Judd, J.; Chakraborty, A.; Boulton, A. Strategies to Support Culturally Safe Health and Wellbeing Evaluations in Indigenous Settings in Australia and New Zealand: A Concept Mapping Study. Int. J. Equity Health 2019, 18, 194. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, A.; Daniel, M.; Howard, N.J.; Chong, A.; Slavin, N.; Brown, A.; Cargo, M. Identifying Environmental Determinants Relevant to Health and Wellbeing in Remote Australian Indigenous Communities: A Scoping Review of Grey Literature. Int. J. Environ. Res. Public Health 2021, 18, 4167. [Google Scholar] [CrossRef]
- Marks, E.; Cargo, M.D.; Daniel, M. Constructing a Health and Social Indicator Framework for Indigenous Community Health Research. Soc. Indic. Res. 2007, 82, 93–110. [Google Scholar] [CrossRef]
- Daniel, M.; Cargo, M.; Marks, E.; Paquet, C.; Simmons, D.; Williams, M.; Rowley, K.; O’Dea, K. Rating Health and Social Indicators for Use with Indigenous Communities: A Tool for Balancing Cultural and Scientific Utility. Soc. Indic. Res. 2009, 94, 241–256. [Google Scholar] [CrossRef]
- Kruskal, J.B.; Wish, M. Multidimensional Scaling; Sage: Thousand Oaks, CA, USA, 1978. [Google Scholar]
- Lebel, A.; Cantinotti, M.; Pampalon, R.; Thériault, M.; Smith, L.A.; Hamelin, A.-M. Concept Mapping of Diet and Physical Activity: Uncovering Local Stakeholders Perception in the Quebec City Region. Soc. Sci. Med. 2011, 72, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Rosas, S.R.; Kane, M. Quality and Rigor of the Concept Mapping Methodology: A Pooled Study Analysis. Eval. Pogram Plan. 2012, 35, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Bailie, R.S.; Wayte, K.J. Housing and Health in Indigenous Communities: Key Issues for Housing and Health Improvement in Remote Aboriginal and Torres Strait Islander Communities. Aust. J. Rural. Health 2006, 14, 178–183. [Google Scholar] [CrossRef]
- McMullen, C.; Eastwood, A.; Ward, J. Environmental Attributable Fractions in Remote Australia: The Potential of a New Approach for Local Public Health Action. Aust. N. Z. J. Public Health 2015, 40, 174–180. [Google Scholar] [CrossRef]
- Melody, S.; Bennett, E.; Clifford, H.; Johnston, F.; Shepherd, C.; Alach, Z.; Lester, M.; Wood, L.J.; Franklin, P.; Zosky, G.R. A Cross-sectional Survey of Environmental Health in Remote Aboriginal Communities in Western Australia. Int. J. Environ. Health Res. 2016, 26, 525–535. [Google Scholar] [CrossRef]
- Foster, T.; Hall, N.L. Housing Conditions and Health in Indigenous Australian Communities: Current Status and Recent Trends. Int. J. Environ. Health Res. 2021, 31, 325–343. [Google Scholar] [CrossRef]
- Bailie, R.S.; Stevens, M.; McDonald, E.L. The Impact of Housing Improvement and Socio-environmental Factors on Common Childhood Illnesses: A Cohort Study in Indigenous Australian Communities. J. Epidemiol. Community Health 2012, 66, 821–831. [Google Scholar] [CrossRef]
- Bailie, C.; Matthews, V.; Bailie, J.; Burgess, P.; Copley, K.; Kennedy, C.; Moore, L.; Larkins, S.; Thompson, S.; Bailie, R.S. Determinants and Gaps in Preventive Care Delivery for Indigenous Australians: A Cross-sectional Analysis. Front. Public Health 2016, 4, 34. [Google Scholar] [CrossRef]
- Ware, V.-A. Improving the Accessibility of Health Services in Urban and Regional Settings for Indigenous People; Australian Institute of Health and Walfare: Canberra, Australia, 2013; Resource sheet no. 27.
- Roberts, K.V.; Maguire, G.P.; Brown, A.; Atkinson, D.N.; Remenyi, B.; Wheaton, G.; Ilton, M.; Carapetis, J. Rheumatic Heart Disease in Indigenous Children in Northern Australia: Differences in Prevalence and the Challenges of Screening. Med. J. Aust. 2015, 203, 221. [Google Scholar] [CrossRef]
- Crooks, K.; Casey, D.; Ward, J. First Nations People Leading the Way in COVID-19 Pandemic Planning, Response and Management. Med. J. Aust. 2020, 213, 151–152. [Google Scholar] [CrossRef] [PubMed]
- Moss, R.; Wood, J.; Brown, D.; Shearer, F.; Black, A.J.; Cheng, A.; McCaw, J.M.; McVernon, J. Modelling the Impact of COVID-19 in Australia to Inform Transmission Reducing Measures and Health System Preparedness. medRXiv 2020. [Google Scholar] [CrossRef]
- Artuso, S.; Cargo, M.; Brown, A.; Daniel, M. Factors Influencing Health Care Utilisation among Aboriginal Cardiac Patients in Central Australia: A Qualitative Study. BMC Health Serv. Res. 2013, 13, 83. [Google Scholar] [CrossRef] [PubMed]
- Bailie, J.; Schierhout, G.; Laycock, A.; Kelaher, M.; Percival, N.; O’Donoghue, L.; McNeair, T.; Bailie, R. Determinants of Access to Chronic Illness Care: A Mixed-methods Evaluation of a National Multifaceted Chronic Disease Package for Indigenous Australians. BMJ Open 2015, 5. [Google Scholar] [CrossRef] [PubMed]
- Price Waterhouse Coopers. Indigenous Housing: Findings of the Review of the Community Housing and Infrastructure Programme; Department of Families, Community Services and Indigenous Affairs: Canberra, Australia, 2007.
- Bailie, R.S.; Stevens, M.R.; McDonald, E.; Halpin, S.; Brewster, D.; Robinson, G.; Guthridge, S. Skin Infection, Housing and Social Circumstances in Children Living in Remote Indigenous Communities: Testing Conceptual and Methodological Approaches. BMC Public Health 2005, 5, 1–12. [Google Scholar] [CrossRef]
- Holt, D.C.; McCarthy, J.S.; Carapetis, J.R. Parasitic Diseases of Remote Indigenous Communities in Australia. Int. J. Parasitol. 2010, 40, 1119–1126. [Google Scholar] [CrossRef]
- Jacklin, K. Diversity within: Deconstructing Aboriginal Community Health in Wikwemikong Unceded Indian Reserve. Soc. Sci. Med. 2009, 68, 980–989. [Google Scholar] [CrossRef]
- United Nations. State of the World’s Indigenous Peoples; Report No. ST/ESA/328; Contract No.: ST/ESA/328; United Nations: New York, NY, USA, 2009. [Google Scholar]
- Leal, C.; Chaix, B. The Influence of Geographic Life Environments on Cardiometabolic Risk Factors: A Systematic Review, a Methodological Assessment and a Research Agenda. Obes. Rev. 2011, 12, 217–230. [Google Scholar] [CrossRef]
- Powell, L.M.; Auld, M.C.; Chaloupka, F.J.; O’Malley, P.M.; Johnston, L.D. Access to Fast Food and Food Prices: Relationship with Fruit and Vegetable Consumption and Overweight among Adolescents. In The Economics of Obesity; Emerald Group Publishing Limited: Bingley, UK, 2006; pp. 23–48. [Google Scholar]
- Sturm, R.; Datar, A. Body Mass Index in Elementary School Children, Metropolitan Area Food Prices and Food Outlet Density. Public Health 2005, 119, 1059–1068. [Google Scholar] [CrossRef]
- Brimblecombe, J.K.; Ferguson, M.M.; Liberato, S.C.; O’Dea, K. Characteristics of the Community-level Diet of Aboriginal People in Remote Northern Australia. Med. J. Aust. 2013, 198, 380–384. [Google Scholar] [CrossRef]
- Henryks, J.; Brimblecombe, J. Mapping Point-of-Purchase Influencers of Food Choice in Australian Remote Indigenous Communities. SAGE Open 2016, 6, 1–11. [Google Scholar] [CrossRef]
- Race, D.; Mathew, S.; Campbell, M.; Hampton, K. Understanding Climate Adaptation Investments for Communities Living in Desert Australia: Experiences of Indigenous Communities. Clim. Chang. 2016, 139, 461–475. [Google Scholar] [CrossRef]
- Turner, L.R.; Connell, D.; Tong, S. The Effect of Heat Waves on Ambulance Attendances in Brisbane, Australia. Prehospital Disaster Med. 2013, 28, 482–487. [Google Scholar] [CrossRef]
- Momperousse, D.; Delnevo, C.; Lewis, M. Exploring the Seasonality of Cigarette-smoking Behaviour. Tob. Control. 2007, 16, 69–70. [Google Scholar] [CrossRef]
- Department of Health. Environmental Health Standards for Remote Communities in the Northern Territory Darwin: Department of Health. 2001. Available online: http://digitallibrary.health.nt.gov.au/prodjspui/handle/10137/874?mode=full (accessed on 26 April 2017).
- Fraser, E.D.G.; Dougill, A.J.; Mabee, W.E.; Reed, M.; McAlpine, P. Bottom Up and Top Down: Analysis of Participatory Processes for Sustainability Indicator Identification as a Pathway to Community Empowerment and Sustainable Environmental Management. J. Environ. Manag. 2006, 78, 114–127. [Google Scholar] [CrossRef]

| Categories | Sorting (n = 29) | Rating (n = 42) |
|---|---|---|
| Type of organization | ||
| Government | 26 (90%) | 36 (85%) |
| Aboriginal and Torres Strait Islander Community Controlled | 3 (10%) | 4 (10%) |
| Other non-government organization | 0 (0%) | 2 (5%) |
| Areas of work | ||
| NT mostly remote | 18 (62%) | 24 (57%) |
| NT mostly rural | 4 (14%) | 5 (12%) |
| NT mostly urban | 7 (24%) | 9 (21%) |
| Other remote | 0 (0%) | 4 (10%) |
| Indigenous status | ||
| Aboriginal | 9 (31%) | 10 (24%) |
| Neither Aboriginal or Torres Strait Islander | 20 (69%) | 32 (76%) |
| Duration in the position | ||
| <6 years | 9 (31%) | 13 (31%) |
| 6–9 years | 2 (7%) | 5 (12%) |
| ≥10 years | 18 (62%) | 24 (57%) |
| Position or role | ||
| Frontline worker | 18 (62%) | 25 (60%) |
| Project Officer | 4 (14%) | 4 (10%) |
| Program Manager | 1 (3%) | 6 (14%) |
| Policy Officer | 2 (7%) | 2 (5%) |
| Other managerial or policy level position | 4 (14%) | 5 (11%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chakraborty, A.; Howard, N.J.; Daniel, M.; Chong, A.; Slavin, N.; Brown, A.; Cargo, M. Prioritizing Built Environmental Factors to Tackle Chronic and Infectious Diseases in Remote Northern Territory (NT) Communities of Australia: A Concept Mapping Study. Int. J. Environ. Res. Public Health 2021, 18, 5178. https://doi.org/10.3390/ijerph18105178
Chakraborty A, Howard NJ, Daniel M, Chong A, Slavin N, Brown A, Cargo M. Prioritizing Built Environmental Factors to Tackle Chronic and Infectious Diseases in Remote Northern Territory (NT) Communities of Australia: A Concept Mapping Study. International Journal of Environmental Research and Public Health. 2021; 18(10):5178. https://doi.org/10.3390/ijerph18105178
Chicago/Turabian StyleChakraborty, Amal, Natasha J. Howard, Mark Daniel, Alwin Chong, Nicola Slavin, Alex Brown, and Margaret Cargo. 2021. "Prioritizing Built Environmental Factors to Tackle Chronic and Infectious Diseases in Remote Northern Territory (NT) Communities of Australia: A Concept Mapping Study" International Journal of Environmental Research and Public Health 18, no. 10: 5178. https://doi.org/10.3390/ijerph18105178
APA StyleChakraborty, A., Howard, N. J., Daniel, M., Chong, A., Slavin, N., Brown, A., & Cargo, M. (2021). Prioritizing Built Environmental Factors to Tackle Chronic and Infectious Diseases in Remote Northern Territory (NT) Communities of Australia: A Concept Mapping Study. International Journal of Environmental Research and Public Health, 18(10), 5178. https://doi.org/10.3390/ijerph18105178







