Lessons from Disability Counting in Ecuador, with a Contribution from Primary Health Care
Abstract
1. Introduction
2. Materials and Methods
2.1. Part 1: A Comparison of National Cross-Sectional Disability Statistics in Ecuador
2.2. Part 2: A Case Study of Disability Counting in a PHC Setting
3. Results
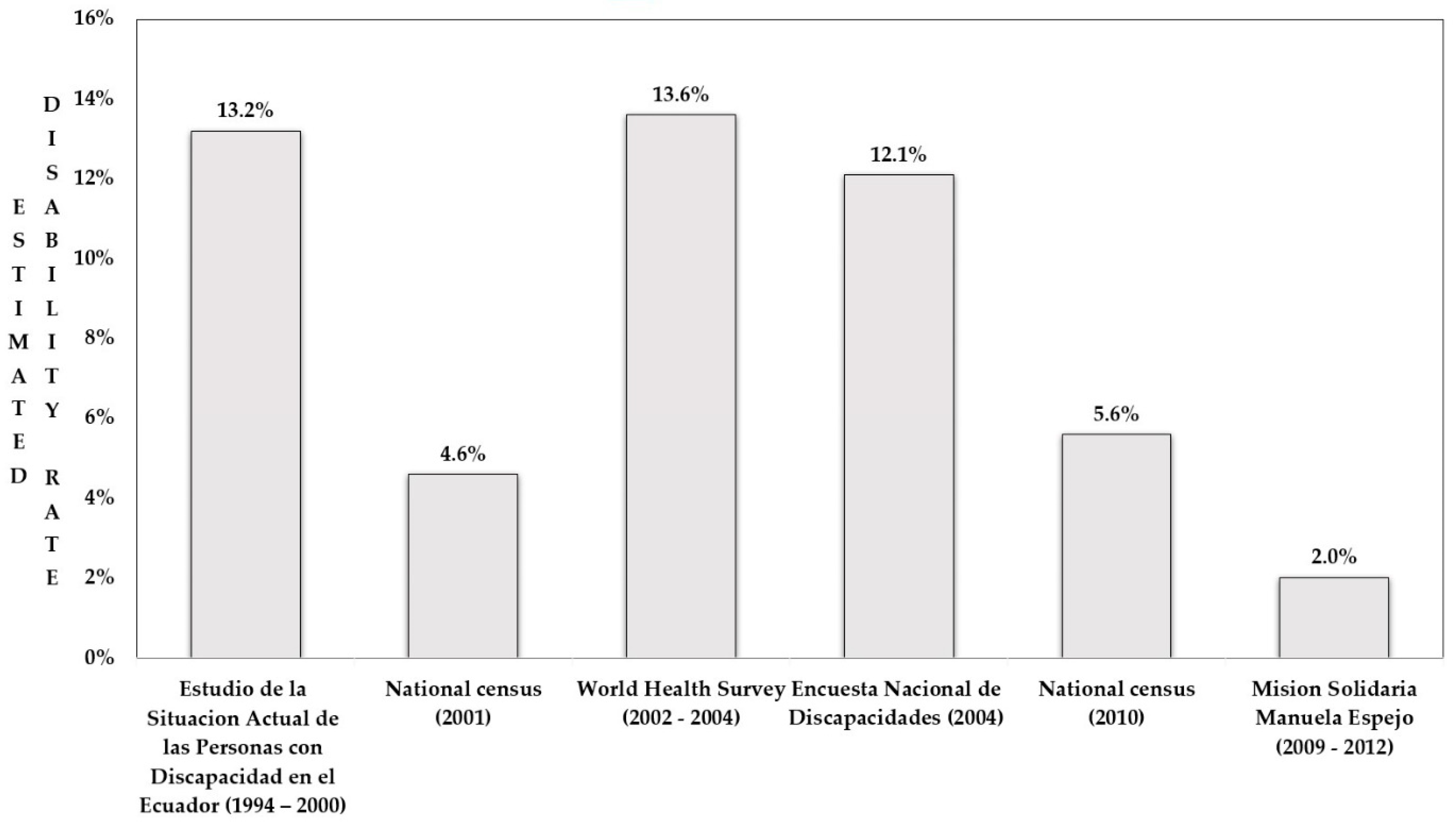
3.1. Part I: Ecuadorian Disability Rates from Six Cross-Sectional Studies
3.1.1. Estudio de la Situación Actual de las Personas con Discapacidad en el Ecuador—ESADE (1994–2000)
3.1.2. National Censuses (2001 and 2010)
3.1.3. World Health Survey (2002–2004)
3.1.4. Encuesta Nacional de Discapacidades (2004)
3.1.5. Misión Manuela Espejo (2009–2012)
3.1.6. Comparison of Results
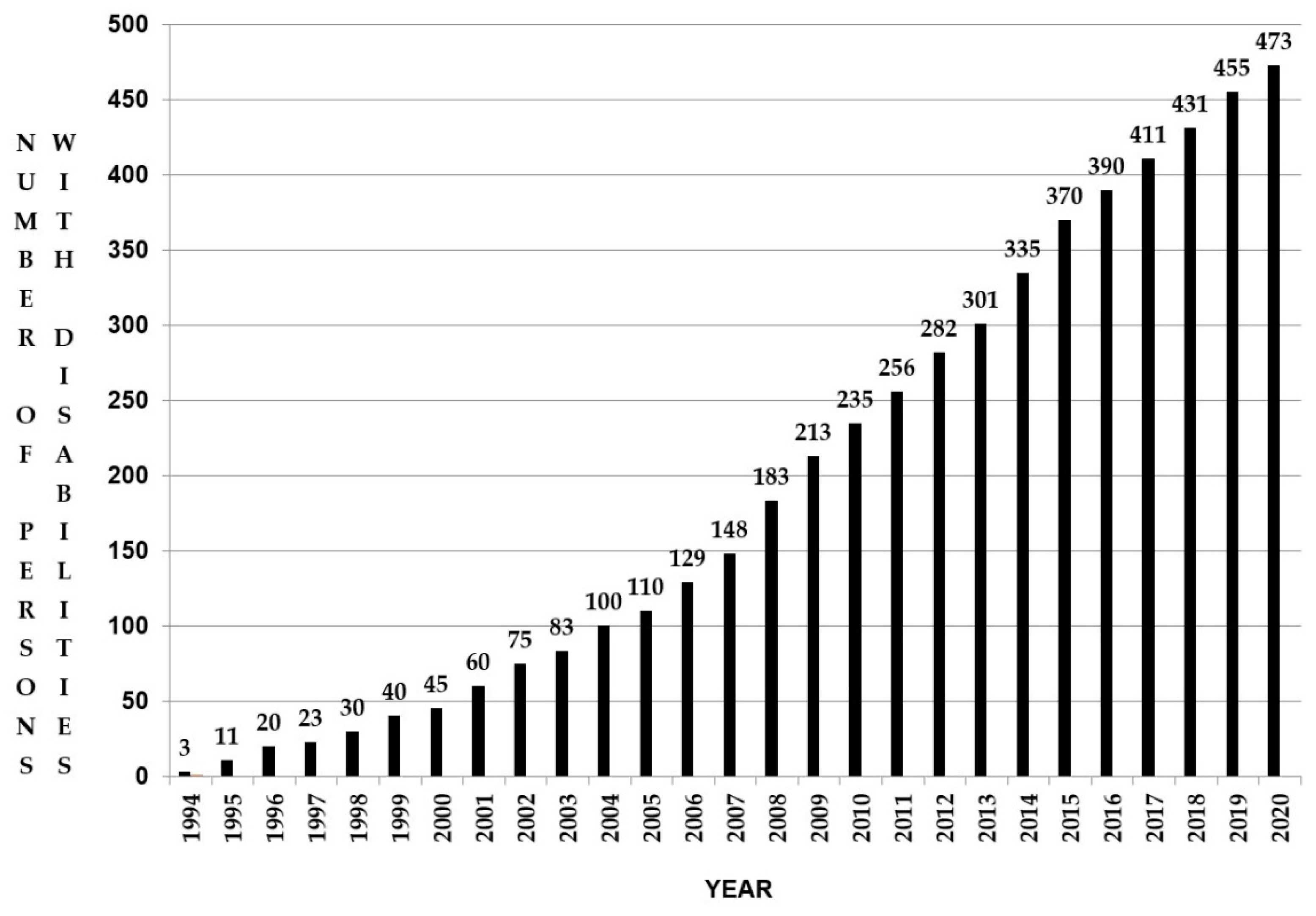
3.2. Part 2: The Case of Tapori: A Longitudinal Approach to Disability Counting in a PHC Setting (1994–2020)
3.2.1. Description of Disability-Related Service Implementation and Data Collection in the PHC Setting
3.2.2. Disability Period Prevalence in the Health Center
3.2.3. Reliability and Validity of Period Prevalence
4. Discussion
4.1. Disability Counting in Search for Balance Between Those Who Count and Those Who Are Counted
4.2. A Contribution to Disability Counting As a Collateral Result of Meeting Needs in Primary Health Care
4.3. Comparing Rates to Evaluate Disability Situations and Policy Implementation May Be a Walk on a Tightrope
5. Implications of Findings
6. Study Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- General Assembly. Convention on the Rights of Persons with Disabilities; United Nations: New York, NY, USA, 2007. [Google Scholar]
- Fujiura, G.; Rutkowski-Kmitta, V. Counting Disability. In Handbook of Disability Studies; Albrecht, G., Seelman, K.D., Bury, M., Eds.; SAGE Publications, Inc.: Newbury Park, CA, USA, 2001; pp. 69–96. ISBN 978-0-7619-2874-4. [Google Scholar]
- World Health Organization; United Nations Economic and Social Commission for Asia and the Pacific. Training Manual on Disability Statistics; ST/ESCAP/2499; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- World Health Organization. World Report on Disability; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Maart, S.; Amosun, S.; Jelsma, J. Disability prevalence-context matters: A descriptive community-based survey. Afr. J. Disabil. 2019, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sabariego, C.; Oberhauser, C.; Posarac, A.; Bickenbach, J.; Kostanjsek, N.; Chatterji, S.; Officer, A.; Coenen, M.; Chhan, L.; Cieza, A. Measuring Disability: Comparing the Impact of Two Data Collection Approaches on Disability Rates. Int. J. Environ. Res. Public. Health 2015, 12, 10329–10351. [Google Scholar] [CrossRef] [PubMed]
- Eide, A.H.; Loeb, M. Counting Disabled People: Historical Perspectives and the Challenges of Disability Statistics. In Disability in the Global South: The Critical Handbook; Grech, S., Soldatic, K., Eds.; Springer International Publishing: Cham, Switzerland, 2016; pp. 51–68. ISBN 978-3-319-42488-0. [Google Scholar]
- Cieza, A.; Sabariego, C.; Bickenbach, J.; Chatterji, S. Rethinking Disability. BMC Med. 2018, 16, 14. [Google Scholar] [CrossRef] [PubMed]
- Mactaggart, I.; Kuper, H.; Murthy, G.V.S.; Oye, J.; Polack, S. Measuring Disability in Population Based Surveys: The Interrelationship between Clinical Impairments and Reported Functional Limitations in Cameroon and India. PLoS ONE 2016, 11, e0164470. [Google Scholar] [CrossRef] [PubMed]
- Madden, R.H.; Bundy, A. The ICF has made a difference to functioning and disability measurement and statistics. Disabil. Rehabil. 2019, 41, 1450–1462. [Google Scholar] [CrossRef] [PubMed]
- Sprunt, B.; McPake, B.; Marella, M. The UNICEF/Washington Group Child Functioning Module—Accuracy, Inter-Rater Reliability and Cut-Off Level for Disability Disaggregation of Fiji’s Education Management Information System. Int. J. Environ. Res. Public. Health 2019, 16, 806. [Google Scholar] [CrossRef] [PubMed]
- Bowen, G.A. Document Analysis as a Qualitative Research Method. Qual. Res. J. 2009, 9, 27–40. [Google Scholar] [CrossRef]
- Atlas Ecuador. Available online: https://knoema.es//atlas/Ecuador (accessed on 29 March 2021).
- Información Censal [2010 Census Information]; Instituto Nacional de Estadistica y Censos: Quito, Ecuador, 2010.
- Consejo Nacional de Discapacidades; Universidad Central del Ecuador; Instituto de Migraciones y Servicios Sociales de España. Situación Actual de Las Personas Con Discapacidad En El Ecuador—Modulo N° 1—Marco Conceptual y Metodológico Del Proyecto ESADE [Current Situation of the Persons with Disabilities in Ecuador—Module N° 1–Conceptual and Methodological Framework of the ESADE Project]; Consejo Nacional de Discapacidades: Quito, Ecuador, 2000. [Google Scholar]
- Información Censal 2001 [2001 Census Information]; Instituto Nacional de Estadística y Censos: Quito, Ecuador, 2001.
- World Health Organization. Report of Ecuador—World Health Survey 2003; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Cazar Flores, R.; Molina Yépez, D.; Moreno Pramatárova, M. Ecuador: La Discapacidad en Cifras: “Análisis De Los Resultados de la Encuesta Nacional de Discapacidades”; Consejo Nacional de Discapacidades: Quito, Ecuador, 2005. [Google Scholar]
- Misión Solidaria Manuela Espejo. Memorias: Estudio Biopsicosocial Clínico y Genético de Las Personas Con Discapacidad en Ecuador; Vicepresidencia del Ecuador: Quito, Ecuador, 2012. [Google Scholar]
- Consejo Nacional de Discapacidades; Universidad Central del Ecuador; Instituto de Migraciones y Servicios Sociales de España. Situación Actual de Las Personas Con Discapacidad en El Ecuador—Modulo N° 4—Resumen Ejecutivo de La Fase Epidemiológica Del Proyecto ESADE [Current Situation of the Persons with Disabilities in Ecuador—Module N° 4—Executive Summary of the Epidemiological Phase of the ESADE Project]; Consejo Nacional de Discapacidades: Quito, Ecuador, 2000. [Google Scholar]
- Mont, D. Measuring Disability Prevalence; World Bank Group: Washington, DC, USA, 2007. [Google Scholar]
- Schneider, M. The difference a word makes: Responding to questions on ‘disability’ and ‘difficulty’ in South Africa. Disabil. Rehabil. 2009, 31, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Sorsdahl, K.R.; Kakuma, R.; Wilson, Z.; Stein, D.J. The internalized stigma experienced by members of a mental health advocacy group in South Africa. Int. J. Soc. Psychiatry 2012, 58, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Worldometer Ecuador Population. Available online: https://www.worldometers.info/world-population/ecuador-population/ (accessed on 28 April 2021).
- World Health Organization. WHO Multi-Country Studies Data Archive. Available online: https://apps.who.int/healthinfo/systems/surveydata/index.php/catalog/whs/about (accessed on 28 April 2021).
- World Bank. Políticas de Discapacidad en Ecuador; World Bank Group: Washington, DC, USA, 2013. [Google Scholar]
- Granizo Rodríguez, S.E. Análisis Sociológico de la Misión Solidaria “Manuela Espejo”: Guayaquil 2009–2012 y Su Sostenibilidad al 2015 [Sociological Analysis of the “Manuela Espejo” Solidarity Mission: Guayaquil 2009–2012 and Its Sustainability to 2015]. Ph.D. Thesis, Universidad Nacional Mayor de San Marcos, Lima, Peru, 2017. [Google Scholar]
- Plan Nacional de Desarrollo 2017–2021. Toda Una Vida [National Development Plan 2017–2021. A Lifetime]; Secretaria Nacional de Planificación y Desarrollo: Quito, Ecuador, 2017.
- Debrouwere, I.; Lebeer, J.; Prinzie, P. The Use of the International Classification of Functioning, Disability and Health in Primary Care: Findings of Exploratory Implementation Throughout Life. Disabil. CBR Incl. Dev. 2016, 27, 57–76. [Google Scholar] [CrossRef]
- Ingstad, B.; Reynolds Whyte, S. Disability and Culture: An overview. In Disability and Culture; Ingstad, B., Reynolds Whyte, S., Eds.; University of California Press: Berkeley, CA, USA, 1995; pp. 3–32. ISBN 978-0-520-08362-2. [Google Scholar]
- Priestley, M. Concepts: Disability, generation, the Life course. In Disability: A Life Course Approach; Polity Press: Cambridge, UK; pp. 11–34.
- Kostanjsek, N.; Good, A.; Madden, R.H.; Üstün, T.B.; Chatterji, S.; Mathers, C.D.; Officer, A. Counting disability: Global and national estimation. Disabil. Rehabil. 2013, 35, 1065–1069. [Google Scholar] [CrossRef] [PubMed]
- Shakespeare, T.; Bright, T.; Kuper, H. Access to Health for Persons with Disabilities; United Nations High Commissioner for Human Rights: Geneva, Switzerland, 2018. [Google Scholar]
- Washington Group on Disability Statistics. An Introduction to the Washington Group on Disability Statistics Question Sets; The Washington Group Primer: New York, NY, USA, 2020. [Google Scholar]
- World Health Organization. Model Disability Survey. Available online: http://www.who.int/disabilities/data/mds/en/ (accessed on 28 April 2021).
- Truyers, C.; Goderis, G.; Dewitte, H.; van den Akker, M.; Buntinx, F. The Intego database: Background, methods and basic results of a Flemish general practice-based continuous morbidity registration project. BMC Med. Inform. Decis. Mak. 2014, 14, 48. [Google Scholar] [CrossRef] [PubMed]
- Grech, S. Disability and Poverty: Complex Interactions and Critical Reframings. In Disability in the Global South: The Critical Handbook; Grech, S., Soldatic, K., Eds.; Springer International Publishing: Cham, Switzerland, 2016; pp. 217–235. ISBN 978-3-319-42488-0. [Google Scholar]
- Trani, J.-F.; Loeb, M. Poverty and disability: A vicious circle? Evidence from Afghanistan and Zambia. J. Int. Dev. 2012, 24, 19–52. [Google Scholar] [CrossRef]
- Madans, J.H.; Loeb, M. Methods to improve international comparability of census and survey measures of disability. Disabil. Rehabil. 2012, 35, 1070–1073. [Google Scholar] [CrossRef] [PubMed]
| Study | Purpose of Disability Counting | Disability Paradigm | Age | Sampling Method and Sample Size | Data Collection Method | Result (Disability Rate) |
|---|---|---|---|---|---|---|
| Estudio de la Situación Actual de las Personas con Discapacidad en Ecuador (ESADE) 1994–2000 [15] | Descriptive study about the situation of persons with disabilities, in order to identify needs and for service planning | Biomedical unilateral causation; No information on thresholds | Older than 5 years | Stratified sampling at national level, survey of 68,000 persons in 16,800 households | General questionnaire on deficiencies (head of the household) + Specific questionnaire for the identified persons with impairments, equated with disability type(s) | 13.2% Approximately 1,600,000 persons with disabilities |
| VI National Census in 2001 [16] VII National Census in 2010 [14] | A priori disability screener as starting point for national disability policy, for in-depth survey sampling, and for evaluation of disability situation at national and aggregate level | No initial disability definition; After initial disability identification: biomedical focus on disability types; No thresholds | All ages | General population sample at national level 2001: 12,156,608 persons 2010: 14,483,499 persons | Self-reporting by answering “yes” or “no” to the question “Do you present permanent disability for longer than a year?” If yes—answer: questions on type of impairment | 2001: 565,560 persons = 4.6% 2010: 816,156 persons = 5.63% |
| World Health Survey (WHS) 2002–2004 [17] | Monitoring and evaluating national disability policy and cross-country comparison of data | Components of health classification, synchronized with the ICF; Use of degree of functioning difficulties and “a posteriori” cutoff | 18 years and older | Stratified sampling at national level, survey in 6135 households | Open questioning in face-to-face household survey, with questionnaire on 8 health and functioning core domains | 13.6% |
| Encuesta Nacional de Discapacidades (END) 2004 [18] | To complement the information of the ESADE study with the social vision of the ICF and to meet the need for universal language for comparison at aggregate level | Biopsychosocial disability paradigm (ICF) “a posteriori” division in mild to moderate and severe limitations | All ages | Random sampling at national level, using the INEC national sampling frame, survey of 83,043 persons in 19,608 households | Open questioning in a base survey and in-depth module for persons with impairment, activity limitations and participation restrictions | 12.14% 1,608,334 persons |
| Misión Solidaria Manuela Espejo (MSME) 2009–2012 [19] | Action research for immediate service implementation in response to critical cases | No initial disability definition; Biomedical “defectology” focus; Only severe functioning limitations were included | All ages | General population sample at national level, with 1,167,893 households visited | Self-reporting in response to a national call for disability identification + Health and impairment-based survey with closed questions | 2.02% 293,743 persons |
| Deficiency Type | Frequency of Deficiencies | Percentages |
|---|---|---|
| Hearing | 73,600 | 4.6% |
| Speech and language | 113,600 | 7.1% |
| Visual | 80,000 | 5% |
| Musculoskeletal | 144,000 | 9% |
| Visceral | 83,200 | 5.2% |
| Disfiguring | 49,600 | 3.1% |
| Intellectual | 432,000 | 27% |
| Psychological | 624,000 | 39% |
| TOTAL | 1,600,000 | 100% |
| Persons with Disabilities | Number | Percentages |
|---|---|---|
| Persons with disabilities, younger than five, who present activity limitation and participation restriction | 17,838 | 1.11% |
| Persons with disabilities, five years and older, who present impairment | 702,793 | 43.7% |
| Persons with disabilities, five years and older, who present mild to moderate limitation | 247,520 | 15.39% |
| Persons with disabilities, five years and older, who present severe limitation | 640,183 | 39.8% |
| TOTAL | 1,608,334 | 100% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Debrouwere, I.; Álvarez Vera, P.C.; Pavón Benítez, X.d.C.; Rosero Arboleda, C.K.; Prinzie, P.; Lebeer, J. Lessons from Disability Counting in Ecuador, with a Contribution from Primary Health Care. Int. J. Environ. Res. Public Health 2021, 18, 5103. https://doi.org/10.3390/ijerph18105103
Debrouwere I, Álvarez Vera PC, Pavón Benítez XdC, Rosero Arboleda CK, Prinzie P, Lebeer J. Lessons from Disability Counting in Ecuador, with a Contribution from Primary Health Care. International Journal of Environmental Research and Public Health. 2021; 18(10):5103. https://doi.org/10.3390/ijerph18105103
Chicago/Turabian StyleDebrouwere, Inge, Pedro Celestino Álvarez Vera, Ximena del Carmen Pavón Benítez, Celia Katherine Rosero Arboleda, Peter Prinzie, and Jo Lebeer. 2021. "Lessons from Disability Counting in Ecuador, with a Contribution from Primary Health Care" International Journal of Environmental Research and Public Health 18, no. 10: 5103. https://doi.org/10.3390/ijerph18105103
APA StyleDebrouwere, I., Álvarez Vera, P. C., Pavón Benítez, X. d. C., Rosero Arboleda, C. K., Prinzie, P., & Lebeer, J. (2021). Lessons from Disability Counting in Ecuador, with a Contribution from Primary Health Care. International Journal of Environmental Research and Public Health, 18(10), 5103. https://doi.org/10.3390/ijerph18105103






