Nutritional Status of Children 24–60 Months Attending Early Child Development Centres in a Semi-Rural Community in South Africa
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sampling
2.2. Dietary Intake
2.3. Anthropometric Measurements
2.4. Biochemical Measures
2.5. Ethics Approval and Consent to Participate
2.6. Data Management and Analysis
3. Results
3.1. Participant Profile
3.2. Nutrient Intake
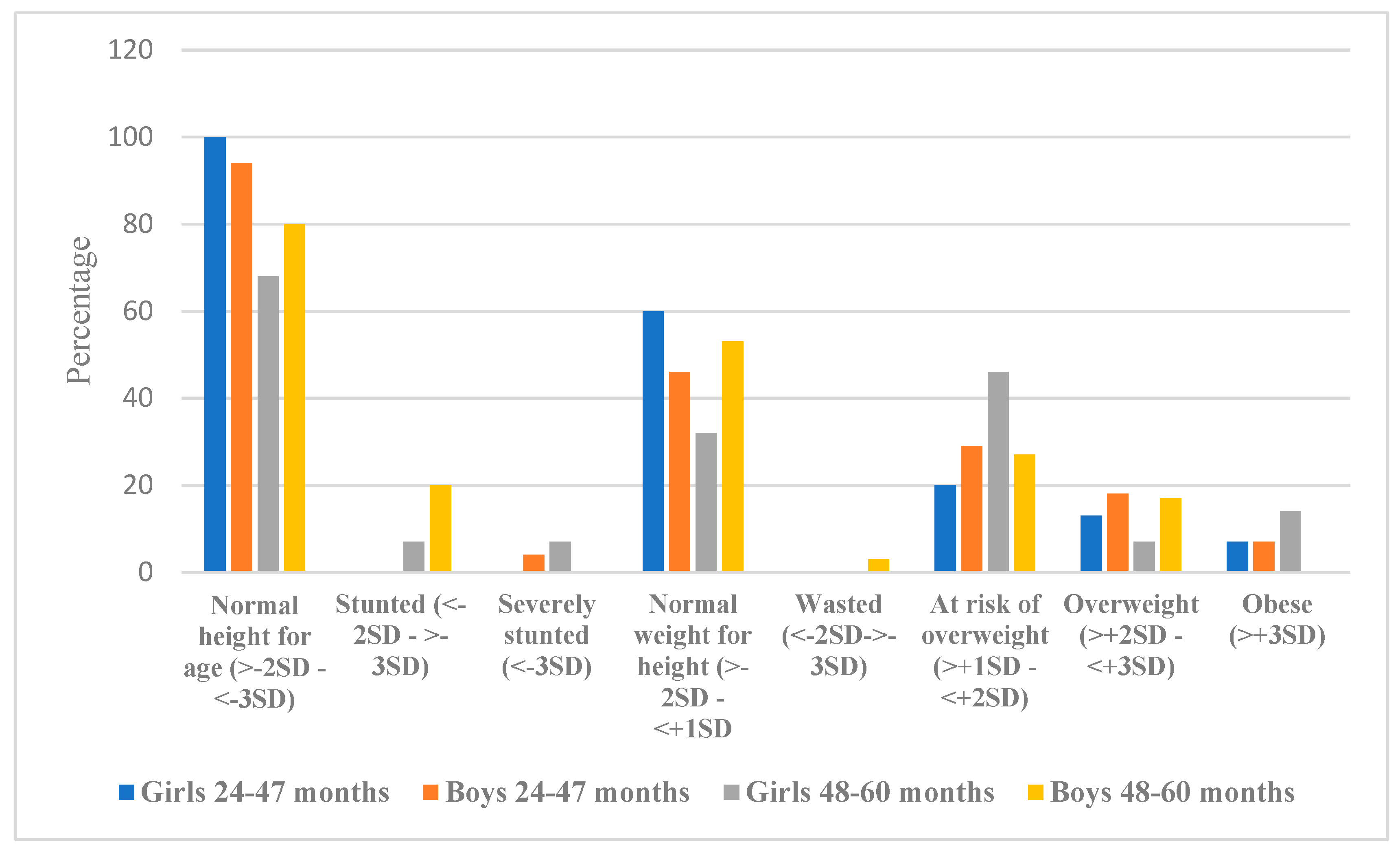
3.3. Anthropometric Status
3.4. Vitamin A and Iron Status
4. Discussion
5. Limitations
6. Conclusions
7. Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Global Nutrition Targets 2025: Policy Brief Series. Available online: https://apps.who.int/iris/bitstream/handle/10665/149018/WHO_NMH_NHD_14.2_eng.pdf?ua=1 (accessed on 10 May 2020).
- FAO; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2018: Building Climate Resilience for Food Security and Nutrition; FAO: Rome, Italy, 2018. [Google Scholar]
- FAO; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2019: Safeguarding Against Economic Slowdowns and Downturns; FAO: Rome, Italy, 2019. [Google Scholar]
- Okop, K.J.; Ndayi, K.; Tsolekile, L.; Sanders, D.; Puoane, T. Low intake of commonly available fruits and vegetables in socio-economically disadvantaged communities of South Africa: Influence of affordability and sugary drinks intake. BMC Public Health 2019, 19, 940. [Google Scholar] [CrossRef] [PubMed]
- Sinyolo, S.; Ndinda, C.; Murendo, C.; Sinyolo, A.S.; Neluheni, M. Access to information technologies and consumption of fruits and vegetables in South Africa: Evidence from nationally representative data. Int. J. Environ. Res. Public Health 2020, 17, 4880. [Google Scholar] [CrossRef] [PubMed]
- Nzama, P.; Napier, C.E. Nutritional adequacy of menus offered to children of 2–5 years in registered childcare facilities in Inanda, KwaZulu-Natal Province, South Africa. S. Afr. J. Child Health 2017, 11, 80–85. [Google Scholar] [CrossRef]
- Labadarios, D.; Steyn, N.P.; Maunder, E.; MacIntryre, U.; Gericke, G.; Swart, R.; Huskisson, J.; Dannhauser, A.; Vorster, H.H.; Nesmvuni, A.E.; et al. The National Food Consumption Survey (NFCS): South Africa, 1999. Public Health Nutr. 2005, 8, 533–543. [Google Scholar] [CrossRef] [PubMed]
- Shisana, O.; Labadarios, D.; Rehle, T.; Simbayi, L.; Zuma, K.; Dhansay, A.; Reddy, P.; Parker, W.; Hoosain, E.; Naidoo, P.; et al. The South African National Health and Nutrition Examination Survey, 2012: SANHANES-1: The Health and Nutritional Status of the Nation; HSRC Press: Cape Town, South Africa, 2013. [Google Scholar]
- Tran, T.D.; Biggs, B.A.; Holton, S.; Nguyen, H.T.M.; Hanieh, S.; Fisher, J. Co-morbid anaemia and stunting among children of pre-school age in low- and middle-income countries: A syndemic. Public Health Nutr. 2019, 22, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Department of Social Development Republic of South Africa. Guidelines for Early Child Development Services; CARICOM Secretariat: Chaguaramas, Trinidad and Tobago, 2008.
- Giese, S.B.D.; Berry, L.; Motlatla, S.; Zide, H. Government Funding for ECD: Can Those Who Need It Get It? DG Murray Trust: Claremont, South Africa, 2017. [Google Scholar]
- Department of Social Development of Republic of South Africa. Social Development Sets Up Workstreams to Conduct Risk Assessment and State of Readiness for the Early Childhood Development (ecd) Centres. Available online: https://www.dsd.gov.za/index.php/latest-news/21-latest-news/183-social-development-sets-up-workstreams-to-conduct-risk-assessment-and-state-of-readiness-for-the-early-childhood-development-ecd-centres (accessed on 15 December 2020).
- Frith, A. KwaNyuswa. Available online: https://census2011.adrianfrith.com/place/505004 (accessed on 3 August 2020).
- Oldewage-Theron, W.H.; Kruger, R. Food variety and dietary diversity as indicators of the dietary adequacy and health status of an elderly population in Sharpeville, South Africa. J. Nutr. Elder. 2008, 27, 101–133. [Google Scholar] [CrossRef] [PubMed]
- WHO; UNICEF. Recommendations for Data Collection, Analysis and Reporting on Anthropometric Indicators in Children Under 5 Years Old. Available online: https://apps.who.int/iris/handle/10665/324791 (accessed on 1 September 2020).
- World Health Organization (WHO). Blood Collection and Handling—Dried Blood Spot (DBS); WHO: Geneva, Switzerland, 2005. [Google Scholar]
- Craft, N.E.; Haitema, T.; Brindle, L.K.; Yamini, S.; Humphrey, J.H.; West, K.P., Jr. Retinol analysis in dried blood spots by HPLC. J. Nutr. 2000, 130, 882–885. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity Vitamin and Mineral Nutrition Information System; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- SANS 10248-1. Management of Healthcare Waste. Available online: https://store.sabs.co.za/pdfpreview.php?hash=75951170a020c6a3aba42e6a518d8f79f0ac7a84&preview=yes (accessed on 10 July 2020).
- Medical Research Council. Food Finder3: Dietary Analysis Software Program, Version 1.0.7; Medical Research Council: Cape Town, South Africa, 2002.
- Bowley, N.A.; Pentz-Kluyts, M.A.; Bourne, L.T.; Marino, L.V. Feeding the 1 to 7-year-old child. A support paper for the South African paediatric food-based dietary guidelines. Matern. Child Nutr. 2007, 3, 281–291. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO AnthroPlus for Personal Computers Manual: Software for Assessing Growth of the World’s Children and Adolescent; WHO: Geneva, Switzerland, 2009. [Google Scholar]
- Institute of Medicine. AMDR Tables. Available online: http://nationalacademies.org/hmd/Activities/Nutrition/SummaryDRIs/DRI-Tables.aspx (accessed on 1 June 2020).
- World Health Organization (WHO). Improving Early Childhood Development: WHO Guideline; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Shung-King, M.; Lake, L.; Sanders, D.; Hendricks, M. South African Child Gauge 2019; Children’s Institute, University of Cape Town: Cape Town, South Africa, 2019. [Google Scholar]
- Faber, M.; Jogessar, V.B.; Benade, A.J. Nutritional status and dietary intakes of children aged 2-5 years and their caregivers in a rural South African community. Int. J. Food Sci. Nutr. 2001, 52, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.; Sambu, W.; Almeleh, C.; Mabaso, K.; Giese, S.; Proudlock, P. South African Early Childhood Review 2019; Ilifa Labantwana: Claremont, Cape Town, 2019. [Google Scholar]
- Raggio, L.; Gámbaro, A. Study of the reasons for the consumption of each type of vegetable within a population of school-aged children. BMC Public Health 2018, 18, 1163. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, A. The double burden of undernutrition and overnutrition in developing countries: An update. Curr. Obes. Rep. 2015, 4, 337–349. [Google Scholar] [CrossRef] [PubMed]
- Dukhi, N.; Sartorius, B.; Taylor, M. Stunting in children (0–59 months): What is the current trend in South Africa? Early Child Dev. Care 2017, 187, 1874–1886. [Google Scholar] [CrossRef]
- Schoeman, S.; Faber, M.; Adams, V.; Smuts, C.; Ford-Ngomane, N.; Laubscher, J.; Dhansay, M. Adverse social, nutrition and health conditions in rural districts of the KwaZulu-Natal and Eastern Cape provinces, South Africa. S. Afr. J. Clin. Nutr. 2010, 23, 140–147. [Google Scholar] [CrossRef]
- Department of Health. South Africa Demographic and Health Survey 2016; National Department of Health: Pretoria, South Africa, 2019.
- Said-Mohamed, R.; Micklesfield, L.K.; Pettifor, J.M.; Norris, S.A. Has the prevalence of stunting in South African children changed in 40 years? A systematic review. BMC Public Health 2015, 15, 534. [Google Scholar] [CrossRef] [PubMed]
- Coutsoudis, A.; Sanders, D.; Dhansay, M.A.; van Stuijvenberg, M.E.; Benn, C.S. Is it time for South Africa to end the routine high-dose vitamin A supplementation programme? S. Afr. Med. J. 2019, 109, 907–910. [Google Scholar] [CrossRef] [PubMed]
- Van Stuijvenberg, M.E.; Dhansay, M.A.; Nel, J.; Suri, D.; Grahn, M.; Davis, C.R.; Tanumihardjo, S.A. South African preschool children habitually consuming sheep liver and exposed to vitamin A supplementation and fortification have hypervitaminotic A liver stores: A cohort study. Am. J. Clin. Nutr. 2019, 110, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Hermoso, M.; Hermoso, M.; Vucic, V.; Vollhardt, C.; Arsic, A.; Roman-Viñas, B.; Iglesia-Altaba, I.; Gurinovic, M.; Koletzko, B. The effect of iron on cognitive development and function in infants, children and adolescents: A systematic review. Ann. Nutr. Metab. 2011, 59, 154–165. [Google Scholar] [CrossRef] [PubMed]
| Girls and Boys 24–47 Months (n = 58) | Girls and Boys 48–60 Months (n = 58) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Nutrient | Girls Mean Nutrient Intake n = 30 (SD) | % Girls < 100% of DRI | Boys Mean Nutrient Intake n = 28 (SD) | % Boys < 100% of DRI | p Value | Girls Mean Nutrient Intake n = 28 (SD) | % Girls < 100% of DRI | Boys Mean Nutrient Intake n = 30 (SD) | % Boys < 100% of DRI | p Value |
| Energy kJ * | 4906.2 (292.6) | 40 | 4997.9 (734.7) | 17.8 | 0.541 | 5936.4 (701.4) | 82 | 5621.2 (339.8) | 96.6 | 0.038 |
| Protein (g) ** | 33.1 (2.9) | 0 | 36.7 (4.2) | 0 | 0.001 | 41.3(0.4) | 0 | 39.2 (0.9) | 0 | 0.000 |
| CHO (g) ** | 167.5(5.1) | 0 | 176.6(17.1) | 0 | 0.011 | 201.1 (36.1) | 0 | 193.5 (15.7) | 0 | 0.316 |
| Total fat (g) | 35.4 (18.4) | - | 34.9 (9.3) | - | 0.842 | 42.8 (30.4) | - | 38.3 (9.4) | - | 0.342 |
| Total dietary fibre (g) *** | 10.7 (1.3) | 100 | 13.4(1.4) | 82 | 0.307 | 13.6 (1.9) | 100 | 14.4(1.7) | 100 | 0.118 |
| Calcium (mg) *** | 248.3 (20.6) | 97 | 307.1 (7.6) | 86 | 0.000 | 346.9 (40.9) | 100 | 241.2 (288.7) | 97 | 0.056 |
| Iron (mg) ** | 8.4 (1.0) | 0 | 9.9(0.9) | 0 | 0.000 | 10.4 (1.3) | 0 | 10.6(1.2) | 0 | 0.641 |
| Zinc (mg) ** | 6.15 (0.7) | 0 | 7.7 (0.0) | 0 | 0.000 | 8.1 (0.9) | 0 | 7.9 (1.2) | 0 | 0.538 |
| Vitamin A (µg) ** | 456.2 (59.6) | 0 | 551.3 (85.3) | 14 | 0.000 | 608.7 (134.4) | 11 | 506.3 (186.0) | 23 | 0.019 |
| Riboflavin (mg) | 1.6 (0.0) | 0 | 1.5 (0.0) | 0 | 0.000 | 2.2 (1.0) | 0 | 2.1 (0.4) | 0 | 0.477 |
| Vitamin B6 (mg) ** | 1.8 (0.1) | 0 | 2.3 (0.1) | 0 | 0.000 | 2.4 (0.6) | 0 | 2.3 (0.7) | 0 | 0.900 |
| Folate (µg) | 207.1 (32.4) | 7 | 256.0 (20.2) | 0 | 0.000 | 251.8 (25.2) | 11 | 273.0 (10.9) | 0 | 0.000 |
| Vitamin B12 (µg) ** | 2.45(0.6) | 0 | 2.6 (0.5) | 0 | 0.164 | 2.8 (0.7) | 7 | 2.4 (0.4) | 0 | 0.031 |
| Girls 24–47 Months (n = 30) | Boys 24–47 Months (n = 28) | p Value | Girls 48–60 Months (n = 28) | Boys 48–60 Months (n = 30) | p Value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean Intake (g) (SD) | Per Capita | Mean Intake (g) (SD) | Per Capita | Mean Intake (g) (SD) | Per Capita | Mean Intake (g) (SD) | Per Capita | |||
| Fruit and vegetables | 63.8 (13.2) | 74.0 | 69.5 (5.4) | 74.5 | 0.037 | 68.3 (8.4) | 98.8 | 74.4 (13.0) | 94.4 | 0.038 |
| Girls 24–47 Months (n = 30) | Boys 24–47 Months (n = 28) | Girls 48–60 Months (n = 28) | Boys 48–60 Months (n = 30) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ITEM | Mean Intake (g) (SD) | Capita Intake (g) | ITEM | Mean Intake (g) (SD) | Capita Intake (g) | ITEM | Mean Intake (g) (SD) | Capita Intake (g) | ITEM | Mean Intake (g) (SD) | Capita Intake (g) |
| Maize meal | 2491.1 (2114.0) | 83 | Maize meal | 2577.6 (2414.0) | 92 | Maize meal | 2151.3 (294.6) | 77 | Maize meal | 3086.1 (2621.7) | 103 |
| Diluted squash cold drink | 1695.8 (866.2) | 56 | Diluted squash cold drink | 1408.1 (1019.4) | 50 | Rice | 1576.0 (731.6) | 56 | Rice | 1770.9 (1419.2) | 59 |
| Rice | 1468.3 (1393.9) | 48 | Rice | 860.8 (1296.6) | 31 | Diluted squash cold drink | 1547 (−27.8) | 55 | Diluted squash cold drink | 1091.6 (408.9) | 36 |
| Instant porridge | 942.3 (−548.2) | 31 | Instant porridge | 865 (−229.5) | 31 | Instant porridge | 1454.6 (803.2) | 52 | Milk | 1455.8 (365.3) | 49 |
| Bread | 691.6 (549.1) | 23 | Bread | 1654.1 (469.0) | 59 | Bread | 765 (−139) | 27 | Instant porridge | 1027.3 (646.7) | 34 |
| Tea | 654.1 (218.0) | 22 | Milk | 914.3 (−984) | 33 | Milk | 725.0 (370.0) | 26 | Bread | 617.5 (124.9) | 21 |
| Milk | 538.83 (526.3) | 18 | Tea | 484.1 (−684.7) | 17 | Apple | 457.0 (41.9) | 16 | Apple | 283.3 (10.6) | 9 |
| Pilchard curry | 384.5 (328.8) | 13 | Apple | 430 (−438.4) | 15 | Chicken curry | 275.0 (181.4) | 10 | Phuthu and maas | 778.3 (601.5) | 26 |
| Sausage curry | 375.0 (275.7) | 13 | Pilchard curry | 243 (−343.6) | 9 | Savoury snack | 265.1 (121.3) | 9 | Tea | 425.3 (400.6) | 14 |
| Apple | 360.0 (325.2) | 12 | Sausage curry | 225 (−318.1) | 8 | Banana | 248.1 (350.9) | 9 | Potato stew | 231.1 (77.0) | 8 |
| Girls 24–47 Months (n = 17) for Serum Retinol, (n = 22) for Hb (%) | Boys 24–47 Months (n = 22) for Serum Retinol, (n = 23) for Hb (%) | Girls 48–60 Months (n = 24) for Serum Retinol, (n = 28) for Hb (%) | Boys 48–60 Months (n = 27) for Serum Retinol, (n = 28) for Hb (%) | ||
|---|---|---|---|---|---|
| Serum retinol levels | >0.070 µmol/L | 100 | 90.9 | 91.7 | 92.6 |
| <0.070 µmol/L | 0 | 9.1 | 8.3 | 7.2 | |
| Hb levels | >11.0 g/dL | 50.0 | 69.6 | 71.4 | 60.7 |
| <11.0 g/dL | 50.0 | 30.4 | 28.6 | 39.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makanjana, O.; Naicker, A. Nutritional Status of Children 24–60 Months Attending Early Child Development Centres in a Semi-Rural Community in South Africa. Int. J. Environ. Res. Public Health 2021, 18, 261. https://doi.org/10.3390/ijerph18010261
Makanjana O, Naicker A. Nutritional Status of Children 24–60 Months Attending Early Child Development Centres in a Semi-Rural Community in South Africa. International Journal of Environmental Research and Public Health. 2021; 18(1):261. https://doi.org/10.3390/ijerph18010261
Chicago/Turabian StyleMakanjana, Onwaba, and Ashika Naicker. 2021. "Nutritional Status of Children 24–60 Months Attending Early Child Development Centres in a Semi-Rural Community in South Africa" International Journal of Environmental Research and Public Health 18, no. 1: 261. https://doi.org/10.3390/ijerph18010261
APA StyleMakanjana, O., & Naicker, A. (2021). Nutritional Status of Children 24–60 Months Attending Early Child Development Centres in a Semi-Rural Community in South Africa. International Journal of Environmental Research and Public Health, 18(1), 261. https://doi.org/10.3390/ijerph18010261




