Post-Traumatic Stress Reactions in Caregivers of Children and Adolescents/Young Adults with Severe Diseases: A Systematic Review of Risk and Protective Factors
Abstract
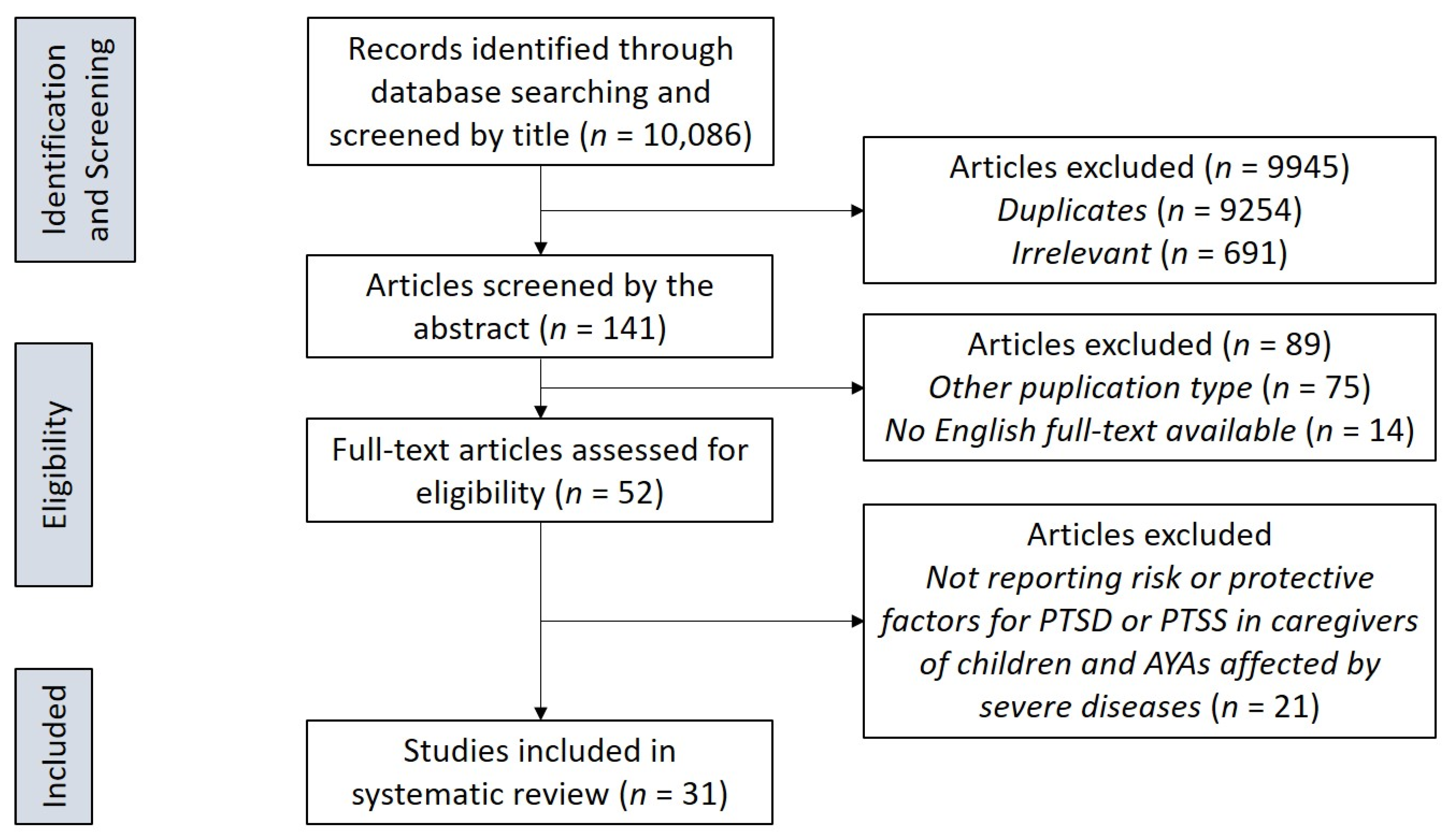
1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Eligibility Criteria
- Full-text publications reporting data related to PTSD and PTSS in caregivers of children and AYAs (aged between 0–25 years) affected by severe illnesses (i.e., chronic or acute, life threatening or disabling diseases).
- Articles assessing possible risk (positively associated) and/or protective (negatively associated) factors for PTSD and PTSS in caregivers.
- Articles available in English.
2.3. Screening and Selection Process
3. Results
3.1. Risk Factors for PTSD/PTSS
3.1.1. Socio-Demographic and Socio-Economic Characteristics
3.1.2. Illness-Related Distress
3.1.3. Psychiatric Symptoms and Negative/Maladaptive Coping
3.2. Protective Factors for PTSD/PTSS
3.2.1. Social Status
3.2.2. Support
3.2.3. Positive Coping
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Celik, G.; Annagur, B.B.; Yılmaz, M.; Demir, T.; Kara, F. Are sleep and life quality of family caregivers affected as much as those of hemodialysis patients? Gen. Hosp. Psychiatry 2012, 34, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Olawale, K.O.; Mosaku, K.S.; Fatoye, O.; Mapayi, B.M.; Oginni, O.A. Caregiver burden in families of patients with depression attending Obafemi Awolowo University teaching hospitals complex Ile-Ife Nigeria. Gen. Hosp. Psychiatry 2014, 36, 743–747. [Google Scholar] [CrossRef] [PubMed]
- Jia, M.; Li, J.; Chen, C.; Cao, F. Post-traumatic stress disorder symptoms in family caregivers of adult patients with acute leukemia from a dyadic perspective. Psychooncology 2015, 24, 1754–1760. [Google Scholar] [CrossRef] [PubMed]
- Jasemi, M.; Aazami, S.; Zabihi, R.E. The effects of music therapy on anxiety and depression of cancer patients. Indian J. Palliat. Care 2016, 22, 455–458. [Google Scholar] [CrossRef] [PubMed]
- Richardson, A.E.; Morton, R.P.; Broadbent, E.A. Illness perceptions and coping predict post-traumatic stress in caregivers of patients with head and neck cancer. Support Care Cancer 2016, 24, 4443–4450. [Google Scholar] [CrossRef]
- Jansen, L.; Dauphin, S.; van den Akker, M.; De Burghgraeve, T.; Schoenmakers, B.; Buntinx, F. Prevalence and predictors of psychosocial problems in informal caregivers of older cancer survivors—A systematic review: Still major gaps in current research. Eur. J. Cancer Care 2018, 27, e12899. [Google Scholar] [CrossRef]
- Santos, G.D.; Ladeira, R.B.; Almeida, J.G.; Aprahamian, I.; Forlenza, O.V.; Lafer, B. Caregiver burden regarding elderly with bipolar disorder: An underrecognized problem. Gen. Hosp. Psychiatry 2018, 51, 134–135. [Google Scholar] [CrossRef]
- Meyers, E.E.; Shaffer, K.M.; Gates, M.; Lin, A.; Rosand, J.; Vranceanu, A.M. Baseline Resilience and Posttraumatic Symptoms in Dyads of Neurocritical Patients and Their Informal Caregivers: A Prospective Dyadic Analysis. Psychosomatics 2020, 61, 135–144. [Google Scholar] [CrossRef]
- Carmassi, C.; Foghi, C.; Dell’Oste, V.; Bertelloni, C.A.; Fiorillo, A.; Dell’Osso, L. Risk and Protective Factors for PTSD in Caregivers of Adult Patients with Severe Medical Illnesses: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 5888. [Google Scholar] [CrossRef]
- Brown, S.M.; Webb, A.; Mangoubi, R.; Dy, J. A sparse combined regression-classification formulation for learning a physiological alternative to clinical posttraumatic stress disorder scores. In Proceedings of the Twenty-Ninth AAAI Conference on Artificial Intelligence, Austin, TX, USA, 25–30 January 2015. [Google Scholar]
- Perkins-Porras, L.; Joekes, K.; Bhalla, N.; Sutherland, C.; Pollard, M. Reporting of posttraumatic stress disorder and cardiac misconceptions following cardiac rehabilitation. J. Cardiopulm. Rehabil. Prev. 2015, 35, 238–245. [Google Scholar] [CrossRef]
- Carmassi, C.; Bertelloni, C.A.; Dell’Oste, V.; Foghi, C.; Diadema, E.; Cordone, A.; Pedrinelli, V.; Dell’Osso, L. Post-traumatic stress burden in a sample of hospitalized patients with Bipolar Disorder: Which impact on clinical correlates and suicidal risk? J. Affect. Disord. 2019, 262, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Johnson, H.; Thompson, A. The development and maintenance of posttraumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: A review. Clin. Psychol. Rev. 2008, 28, 36–47. [Google Scholar] [CrossRef] [PubMed]
- Pelcovitz, D.; Goldenberg, B.; Kaplan, S.; Weinblatt, M.; Mandel, F.; Meyers, B.; Vinciguerra, V. Posttraumatic stress disorder in mothers of pediatric cancer survivors. Psychosomatics 1996, 37, 116–126. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, DSM-5; American Psychiatric Press: Washington, DC, USA, 2013. [Google Scholar]
- Friedman, M.J. Finalizing PTSD in DSM-5: Getting here from there and where to go next. J. Trauma Stress 2013, 26, 548–556. [Google Scholar] [CrossRef]
- Kilpatrick, D.G.; Resnick, H.S.; Milanak, M.E.; Miller, M.W.; Keyes, K.M.; Friedman, M.J. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV-TR and DSM-5 criteria. J. Trauma Stress 2013, 26, 537–547. [Google Scholar] [CrossRef]
- Friedman, M.J.; Resick, P.A.; Bryant, R.A.; Brewin, C.R. Considering PTSD for DSM-5. Depress Anxiety 2011, 28, 750–769. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Bertelloni, C.A.; Cordone, A.; Cappelli, A.; Massimetti, E.; Dell’Oste, V.; Dell’Osso, L. Exploring mood symptoms overlap in PTSD diagnosis: ICD-11 and DSM-5 criteria compared in a sample of subjects with Bipolar Disorder. J. Affect. Disord. 2020, 276, 205–211. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Carmassi, C.; Massimetti, G.; Daneluzzo, E.; Di Tommaso, S.; Rossi, A. Full and partial PTSD among young adult survivors 10 months after the L’Aquila 2009 earthquake: Gender differences. J. Affect. Disord. 2011, 131, 79–83. [Google Scholar] [CrossRef]
- Bruce, M. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clin. Psychol. Rev. 2006, 26, 233–256. [Google Scholar] [CrossRef]
- Cernvall, M.; Alaie, I.; von Essen, L. The factor structure of traumatic stress in parents of children with cancer: A longitudinal analysis. J. Pediatr. Psychol. 2012, 37, 448–457. [Google Scholar] [CrossRef]
- Horsch, A.; McManus, F.; Kennedy, P. Cognitive and non-cognitive factors associated with posttraumatic stress symptoms in mothers of children with type 1 diabetes. Behav. Cogn. Psychother. 2012, 40, 400–411. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Corsi, M.; Gesi, C.; Bertelloni, C.A.; Faggioni, F.; Calderani, E.; Massimetti, G.; Saggese, G.; Bonuccelli, A.; Orsini, A.; et al. DSM-5 criteria for PTSD in parents of pediatric patients with epilepsy: What are the changes with respect to DSM-IV-TR? Epilepsy Behav. 2017, 70 Pt A, 97–103. [Google Scholar] [CrossRef]
- Carmassi, C.; Rossi, A.; Pedrinelli, V.; Cremone, I.M.; Dell’Oste, V.; Stratta, P.; Bertelloni, C.A.; Dell’Osso, L. PTSD in the aftermath of a natural disaster: What we learned from the Pisa-L’Aquila Collaboration Project. J. Psychopathol. 2020, 26, 99–106. [Google Scholar] [CrossRef]
- Carmassi, C.; Barberi, F.M.; Cordone, A.; Maglio, A.; Dell’Oste, V.; Dell’Osso, L. Trauma, PTSD and post-traumatic stress spectrum: 15 years’ experience on a multidimensional approach to trauma related psychopathology. J. Psychopathol. 2020, 26, 4–11. [Google Scholar] [CrossRef]
- Kazak, A.E.; Alderfer, M.; Rourke, M.T.; Simms, S.; Streisand, R.; Grossman, J.R. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J. Pediatr. Psychol. 2004, 29, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Pelcovitz, D.; Libov, B.; Mandel, F.; Kaplan, S.; Weinblatt, M.; Septimus, A. Posttraumatic stress disorder and family functioning in adolescent cancer. J. Trauma Stress 1998, 11, 205–221. [Google Scholar] [CrossRef] [PubMed]
- Stuber, M.L.; Christakis, D.; Houskamp, B.; Kazak, A.E. Posttraumatic symptoms in childhood leukemia survivors and their parents. Psychosomatics 1996, 37, 254–261. [Google Scholar] [CrossRef]
- ZafarianMoghaddam, E.; BehnamVashani, H.R.; Reihani, T.; NamaziZadegan, S. The Effect of Spiritual education on depression, anxiety, and stress of caregivers of children with leukemia. J. Torbat Heydariyeh Univ. Med Sci. 2016, 4, 1–7. [Google Scholar]
- Santacroce, S. Uncertainty, anxiety and symptoms of posttraumatic stress in parents of children recently diagnosed with cancer. J. Pediatr. Oncol. Nurs. 2002, 19, 104–111. [Google Scholar] [CrossRef]
- Salmani, N.; Ashketorab, T.; Hasanvand, S. The burden of caregiver and related factors of oncology patients of Shah Vali hospital. Adv. Nurs. Midwifery 2014, 24, 11–18. [Google Scholar]
- Rha, S.Y.; Park, Y.; Song, S.K.; Lee, C.E.; Lee, J. Caregiving burden and the quality of life of family caregivers of cancer patients: The relationship and correlates. Eur. J. Oncol. Nurs. 2015, 19, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Dell’Oste, V.; Barberi, F.M.; Pedrinelli, V.; Cordone, A.; Cappelli, A.; Cremone, I.M.; Rossi, R.; Bertelloni, C.A.; Dell’Osso, L. Do somatic symptoms relate to PTSD and gender after earthquake exposure? A cross-sectional study on young adult survivors in Italy. CNS Spectr. 2020, 1–7. [Google Scholar] [CrossRef]
- Carmassi, C.; Dell’Oste, V.; Pedrinelli, V.; Barberi, F.M.; Rossi, R.; Bertelloni, C.A.; Dell’Osso, L. Is Sexual Dysfunction in Young Adult Survivors to the L’Aquila Earthquake Related to Post-traumatic Stress Disorder? A Gender Perspective. J. Sex. Med. 2020, 17, 1770–1778. [Google Scholar] [CrossRef]
- Carmassi, C.; Dell’Oste, V.; Bertelloni, C.A.; Foghi, C.; Diadema, E.; Mucci, F.; Massimetti, G.; Rossi, A.; Dell’Osso, L. Disrupted Rhythmicity and Vegetative Functions Relate to PTSD and Gender in Earthquake Survivors. Front. Psychiatry 2020, 11, 492006. [Google Scholar] [CrossRef] [PubMed]
- Kazak, A.E.; Aldefer, M.; Streisand, R.; Simms, S.; Rourke, M.T.; Barakat, L.P.; Gallagher, P.; Cnaan, A. Treatment of posttraumatic stress symptoms in adolescent survivors of childhood cancer and their families: A randomized clinical trial. J. Fam. Psychol. 2004, 18, 493–504. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Kim, J.M.; Kim, S.W.; Kang, H.J.; Shin, I.S.; Shim, H.J.; Cho, S.H.; Chung, I.J.; Yoon, J.S. Determinants of a hopeful attitude among family caregivers in a palliative care setting. Gen. Hosp. Psychiatry 2014, 36, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Zale, E.L.; Heinhuis, T.J.; Tehan, T.; Salgueiro, D.; Rosand, J.; Vranceanu, A.M. Resiliency is independently associated with greater quality of life among informal caregivers to neuroscience intensive care unit patients. Gen. Hosp. Psychiatry 2018, 52, 27–33. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzla, J.; Altman, D.G. The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Landolt, M.; Vollrath, M.; Ribi, K.; Gnehm, H.; Sennhauser, F. Incidence and associations of parental and child posttraumatic stress symptoms in pediatric patients. J. Child Psychol. Psychiatry 2003, 44, 1199–1207. [Google Scholar] [CrossRef]
- Phipps, S.; Long, A.; Hudson, M.; Rai, S.N. Symptoms of post-traumatic stress in children with cancer and their parents: Effects of informant and time from diagnosis. Pediatr. Blood Cancer 2005, 45, 952–959. [Google Scholar] [CrossRef]
- Jurbergs, N.; Long, A.; Ticona, L.; Phipps, S. Symptoms of posttraumatic stress in parents of children with cancer: Are they elevated relative to parents of healthy children? J. Pediatr. Psychol. 2009, 34, 4–13. [Google Scholar] [CrossRef]
- Bruce, M.; Gumley, D.; Isham, L.; Fearon, P.; Phipps, K. Post-traumatic stress symptoms in childhood brain tumour survivors and their parents. Child Care Health Dev. 2011, 37, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Harper, F.W.; Peterson, A.M.; Uphold, H.; Albrecht, T.L.; Taub, J.W.; Orom, H.; Phipps, S.; Penner, L.A. Longitudinal study of parent caregiving self-efficacy and parent stress reactions with pediatric cancer treatment procedures. Psychooncology 2013, 22, 1658–1664. [Google Scholar] [CrossRef]
- Khalifa, A.S.; Bishry, Z.; Tantawy, A.A.; Ghanem, M.H.; Effat, S.M.; El Shahawy, H.; Ebeid, F.S. Psychiatric morbidity in Egyptian children with acute lymphoblastic leukemia and their care providers. Hematol. Oncol. Stem Cell Ther. 2014, 7, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Juth, V.; Silver, R.C.; Sender, L. The shared experience of adolescent and young adult cancer patients and their caregivers. Psychooncology 2015, 24, 1746–1753. [Google Scholar] [CrossRef] [PubMed]
- Malpert, A.V.; Kimberg, C.; Luxton, J.; Mullins, L.L.; Pui, C.-H.; Hudson, M.M.; Krull, K.R.; Brinkman, T.M. Emotional distress in parents of long-term survivors of childhood acute lymphoblastic leukemia. Psychooncology 2015, 24, 1116–1123. [Google Scholar] [CrossRef]
- McCarthy, M.C.; McNeil, R.; Drew, S.; Dunt, D.; Kosola, S.; Orme, L.; Sawyer, S.M. Psychological Distress and Posttraumatic Stress Symptoms in Adolescents and Young Adults with Cancer and Their Parents. J. Adolesc. Young Adult Oncol. 2016, 5, 322–329. [Google Scholar] [CrossRef]
- Masa’deh, R.; Jarrah, S. Post Traumatic Stress Disorder in Parents of Children With Cancer in Jordan. Arch. Psychiatr. Nurs. 2017, 31, 8–12. [Google Scholar] [CrossRef]
- Sawyer, S.M.; McNeil, R.; McCarthy, M.; Orme, L.; Thompson, K.; Drew, S.; Dunt, D. Unmet need for healthcare services in adolescents and young adults with cancer and their parent carers. Support Care Cancer 2017, 25, 2229–2239. [Google Scholar] [CrossRef]
- McCarthy, M.C.; McNeil, R.; Drew, S.; Orme, L.; Sawyer, S.M. Information needs of adolescent and young adult cancer patients and their parent-carers. Support Care Cancer 2018, 26, 1655–1664. [Google Scholar] [CrossRef]
- Perez, M.N.; Sharkey, C.M.; Tackett, A.P.; Delozier, A.M.; Bakula, D.M.; Gamwell, K.L.; Mayes, S.; McNall, R.; Chaney, J.M.; Clawson, A.H.; et al. Post-traumatic stress symptoms in parents of children with cancer: A mediation model. Pediatr. Hematol. Oncol. 2018, 35, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Perez, M.N.; Traino, K.A.; Bakula, D.M.; Sharkey, C.M.; Espeleta, H.C.; Delozier, A.M.; Mayes, S.; McNall, R.; Chaney, J.M.; Mullins, L.L. Barriers to care in pediatric cancer: The role of illness uncertainty in relation to parent psychological distress. Psychooncology 2020, 29, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Aftyka, A.; Rozalska, I. Post-traumatic stress symptoms in a partner as an essential predictor for post-traumatic stress symptoms in the mothers and fathers of children previously treated in NICU. JNN 2020, 26, 259–262. [Google Scholar] [CrossRef]
- Malin, K.J.; Johnson, T.S.; McAndrew, S.; Westerdahl, J.; Leuthner, J.; Lagatta, J. Infant illness severity and perinatal post-traumatic stress disorder after discharge from the neonatal intensive care unit. Early Hum. Dev. 2019, 140, 104930. [Google Scholar] [CrossRef]
- Carmassi, C.; Corsi, M.; Bertelloni, C.A.; Carpita, B.; Gesi, C.; Pedrinelli, V.; Massimetti, G.; Peroni, D.G.; Bonuccelli, A.; Orsini, A.; et al. Mothers and fathers of children with epilepsy: Gender differences in post-traumatic stress symptoms and correlations with mood spectrum symptoms. Neuropsychiatr. Dis. Treat. 2018, 14, 1371–1379. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Corsi, M.; Gesi, C.; Bertelloni, C.A.; Massimetti, G.; Peroni, D.; Bonuccelli, A.; Orsini, A.; Carmassi, C. Adult Autism Subthreshold Spectrum (AdAS Spectrum) in parents of pediatric patients with epilepsy: Correlations with post-traumatic stress symptoms. Compr. Psychiatry 2018, 83, 25–30. [Google Scholar] [CrossRef]
- Odar, C.; Kirschman, K.J.; Pelley, T.J.; Butz, C.; Besner, G.E.; Fabia, R.B. Prevalence and correlates of posttraumatic stress in parents of young children postburn. J. Burn Care Res. 2013, 34, 299–306. [Google Scholar] [CrossRef]
- De Young, A.C.; Hendrikz, J.; Kenardy, J.A.; Cobham, V.E.; Kimble, R.M. Prospective evaluation of parent distress following pediatric burns and identification of risk factors for young child and parent posttraumatic stress disorder. J. Child Adolesc. Psychopharmacol. 2014, 24, 9–17. [Google Scholar] [CrossRef]
- Hawkins, L.; Centifanti, L.C.M.; Holman, N.; Taylor, P. Parental Adjustment following Pediatric Burn Injury: The Role of Guilt, Shame, and Self-Compassion. J. Pediatr. Psychol. 2019, 44, 229–237. [Google Scholar] [CrossRef]
- Pasterski, V.; Mastroyannopoulou, K.; Wright, D.; Zucker, K.J.; Hughes, I.A. Predictors of posttraumatic stress in parents of children diagnosed with a disorder of sex development. Arch. Sex. Behav. 2014, 43, 369–375. [Google Scholar] [CrossRef]
- Perez, M.N.; Delozier, A.M.; Aston, C.E.; Austin, P.; Baskin, L.; Chan, Y.-M.; Cheng, E.Y.; Diamond, D.A.; Fried, A.; Greenfield, S.; et al. Predictors of Psychosocial Distress in Parents of Young Children with Disorders of Sex Development. J. Urol. 2019, 202, 1046–1051. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, D.M.; Sidora-Arcoleo, K.; Serebrisky, D.; Feldman, J.M. The relationship between caregivers’ post-traumatic stress disorder and their asthma health beliefs in an ethnic minority inner-city sample. J. Asthma 2012, 49, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Young, G.S.; Mintzer, L.L.; Seacord, D.; Castañeda, M.; Mesrkhani, V.; Stuber, M.L. Symptoms of posttraumatic stress disorder in parents of transplant recipients: Incidence, severity, and related factors. Pediatrics 2003, 111 Pt 1, e725–e731. [Google Scholar] [CrossRef]
- Ingerski, L.M.; Shaw, K.; Gray, W.N.; Janicke, D.M. A pilot study comparing traumatic stress symptoms by child and parent report across pediatric chronic illness groups. J. Dev. Behav. Pediatr. 2010, 31, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Virtue, S.M.; Manne, S.L.; Mee, L.; Bartell, A.; Sands, S.; Gajda, T.M.; Darabos, K. Psychological distress and psychiatric diagnoses among primary caregivers of children undergoing hematopoietic stem cell transplant: An examination of prevalence, correlates, and racial/ethnic differences. Gen. Hosp. Psychiatry 2014, 36, 620–626. [Google Scholar] [CrossRef] [PubMed]
- Taskiran, G.; Surer Adanir, A.; Ozatalay, E. Living with the unknown: Posttraumatic stress disorder in pediatric bone marrow transplantation survivors and their mothers. Pediatr. Hematol. Oncol. J. 2016, 33, 209–218. [Google Scholar] [CrossRef]
- Casey, L.B.; Zanksas, S.; Meindl, J.N.; Parra, G.R.; Cogdal, P.; Powell, K. Parental symptoms of posttraumatic stress following a child’s diagnosis of autism spectrum disorder: A pilot study. Res. Autism Spectr. Disord. 2012, 6, 1186–1193. [Google Scholar] [CrossRef]
- Tutus, D.; Goldbeck, L. Posttraumatic symptoms and cognitions in parents of children and adolescents with PTSD. Eur. Child Adolesc. Psychiatr 2016, 25, 997–1005. [Google Scholar] [CrossRef]
- Stewart, M.; Schnabel, A.; Hallford, D.J.; McGillivray, J.A.; Forbes, D.; Foster, M.; Shandley, K.; Gardam, M.; Austin, D.W. Challenging child behaviours positively predict symptoms of posttraumatic stress disorder in parents of children with Autism Spectrum Disorder and Rare Diseases. Res. Autism Spectr. Disord. 2020, 69, 101467. [Google Scholar] [CrossRef]
- Weiss, D.S. The impact of event Scale-revised. In Assessing Psychological Trauma and PTSD, 2nd ed.; Wilson, J.P., Keane, T.M., Eds.; Guilford Press: New York, NY, USA, 2004; pp. 168–189. [Google Scholar]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM-5 (PCL-5); National Center for PTSD: Washington, DC, USA, 2013. Available online: www.ptsd.va.gov (accessed on 18 December 2020).
- Tolin, D.F.; Foa, E.B. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychol. Bull. 2006, 132, 959–992. [Google Scholar] [CrossRef] [PubMed]
- Tekin, A.; Karadağ, H.; Süleymanoğlu, M.; Tekin, M.; Kayran, Y.; Alpak, G.; Şar, V. Prevalence and gender differences in symptomatology of posttraumatic stress disorder and depression among Iraqi Yazidis displaced into Turkey. Eur. J. Psychotraumatol. 2016, 7, 28556. [Google Scholar] [CrossRef]
- Carpita, B.; Muti, D.; Muscarella, A.; Dell’Oste, V.; Diadema, E.; Massimetti, G.; Signorelli, M.S.; Fusar Poli, L.; Gesi, C.; Aguglia, E.; et al. Sex Differences in the Relationship between PTSD Spectrum Symptoms and Autistic Traits in a Sample of University Students. Clin. Pract. Epidemiol. Ment. Health 2019, 15, 110–119. [Google Scholar] [CrossRef]
- Inslicht, S.S.; Metzler, T.J.; Garcia, N.M.; Pineles, S.L.; Milad, M.R.; Orr, S.P.; Marmar, C.R.; Neylan, T.C. Sex differences in fear conditioning in posttraumatic stress disorder. J. Psychiatr. Res. 2013, 47, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Grinyer, A. Contrasting parental perspectives with those of teenagers and young adutls with cancer: Comparing the findings from two qualitative studies. Eur. J. Oncol. Nurs. 2009, 13, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Tackett, A.P.; Cushing, C.C.; Suorsa, K.I.; Mullins, A.J.; Gamwell, K.L.; Mayes, S.; McNall-Knapp, R.; Chaney, J.M.; Mullins, L.L. Illness uncertainty, global psychological distress, and posttraumatic stress in pediatric cancer: A preliminary examination using a path analysis approach. J. Pediatr. Psychol. 2015, 41, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Molzon, E.S.; Mullins, L.L.; Cushing, C.C.; Chaney, J.M.; McNall, R.; Mayes, S. The relationship between barriers to care, caregiver distress, and child health-related quality of life in caregivers of children with cancer: A structural equation modeling approach. Child Health Care 2018, 47, 1–15. [Google Scholar] [CrossRef]
- Diamond, L.M.; Aspinwall, L.G. Emotion regulation across the life span: An integrative perspective emphasizing self-regulation, positive affect, and dyadic processes. Motiv. Emot. 2003, 27, 125–156. [Google Scholar] [CrossRef]
- Aldao, A.; Nolen-Hoeksema, S.; Schweizer, S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef]
- Michael, T.; Halligan, S.L.; Clark, D.M.; Ehlers, A. Rumination in posttraumatic stress disorder. Depress Anxiety 2007, 24, 307–317. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Cremone, I.M.; Carpita, B.; Dell’Oste, V.; Muti, D.; Massimetti, G.; Barlati, S.; Vita, A.; Fagiolini, A.; Carmassi, C.; et al. Rumination, posttraumatic stress disorder, and mood symptoms in borderline personality disorder. Neuropsychiatr. Dis. Treat. 2019, 15, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Bertelloni, C.A.; Salarpi, G.; Diadema, E.; Avella, M.T.; Dell’Oste, V.; Dell’Osso, L. Is There a Major Role for Undetected Autism Spectrum Disorder with Childhood Trauma in a Patient with a Diagnosis of Bipolar Disorder, Self-Injuring, and Multiple Comorbidities? Case Rep. Psychiatry 2019, 4703795. [Google Scholar] [CrossRef] [PubMed]
- Clohessy, S.; Ehlers, A. PTSD symptoms, response to intrusive memories and coping in ambulance service workers. Br. J. Clin. Psychol. 1999, 38, 251–265. [Google Scholar] [CrossRef]
- Murray, J.; Ehlers, A.; Mayou, R.A. Dissociation and post-traumatic stress disorder: Two prospective studies of road traffic accident survivors. Br. J. Psychiatry 2002, 180, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Bertelloni, C.A.; Gesi, C.; Conversano, C.; Stratta, P.; Massimetti, G.; Rossi, A.; Dell’Osso, L. New DSM-5 PTSD guilt and shame symptoms among Italian earthquake survivors: Impact on maladaptive behaviors. Psychiatry Res. 2017, 251, 142–147. [Google Scholar] [CrossRef]
- Tangney, J.P. Conceptual and methodological issues in the assessment of shame and guilt. Behav. Res. Ther. 1996, 34, 741–754. [Google Scholar] [CrossRef]
- Øktedalen, T.; Hagtvet, K.A.; Hoffart, A.; Langkaas, T.F.; Smucker, M. The trauma related shame inventory: Measuring trauma-related shame among patients with PTSD. J. Psychopathol. Behav. Assess 2014, 36, 600–615. [Google Scholar] [CrossRef]
- Hibbard, J.H.; Greene, J. What the evidence shows about patient activation: Better health outcomes and care experience; fewer data on costs. Health Aff. 2013, 32, 207–214. [Google Scholar] [CrossRef]
- Allard, C.B.; Norman, S.B.; Thorp, S.R.; Browne, K.C.; Stein, M.B. Mid-Treatment Reduction in Trauma-Related Guilt Predicts PTSD and Functioning Following Cognitive Trauma Therapy for Survivors of Intimate Partner Violence. J. Interpers. Violence 2018, 33, 3610–3629. [Google Scholar] [CrossRef]
- McNeil, R.; McCarthy, M.C.; Dunt, D.; Thompson, K.; Kosola, S.; Orme, L.; Drew, S.; Sawyer, S.M. Financial challenges of cancer for adolescents and young adults and their parent caregivers. Soc. Work. Res. 2019, 43, 17–30. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy: The Exercise of Control; Freeman: New York, NY, USA, 1997. [Google Scholar]
- Kwok, S.; Wong, D. Mental health of parents with young children in Hong Kong: The roles of parenting stress and parenting self-efficacy. Child Fam. Soc. Work. 2000, 5, 57–65. [Google Scholar] [CrossRef]
- Best, M.; Streisand, R.; Catania, L.; Kazak, A.E. Parental distress during pediatric leukemia and posttraumatic stress symptoms (PTSS) after treatment ends. J. Pediatr. Psychol. 2001, 26, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Neff, K.D. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self Identity 2003, 2, 85–101. [Google Scholar] [CrossRef]
- Neff, K.D.; Kirkpatrick, K.L.; Rude, S.S. Selfcompassion and adaptive psychological functioning. J. Res. Pers. 2007, 41, 139–154. [Google Scholar] [CrossRef]
- Gray, D.E. ‘Everybody just freezes. Everybody is just embarrassed’: Felt and enacted stigma among parents of children with high functioning autism. Sociol. Health Illn. 2002, 24, 734–749. [Google Scholar] [CrossRef]
- Micali, N.; Chakrabarti, S.; Fombonne, E. The Broad Autism Phenotype. Autism 2004, 8, 21–37. [Google Scholar] [CrossRef]
- Sawyer, M.; Bittman, M.; La Greca, A.; Crettenden, A.; Harchak, T.; Martin, J. Time Demands of Caring for Children with Autism: What are the Implications for Maternal Mental Health? J. Autism Dev. Disord. 2010, 40, 620–628. [Google Scholar] [CrossRef]
- Sharpe, D.L.; Baker, D.L. The Financial Side of Autism: Private and Public Costs. In A Comprehensive Book on Autism Spectrum Disorders; Mohammadi, M.R., Ed.; InTech: Rijeka, Croatia, 2011; pp. 275–296. [Google Scholar]
- Hayes, S.; Watson, S. The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism Spectrum disorder. J. Autism Dev. Disord. 2013, 43, 629–642. [Google Scholar] [CrossRef]
- Nereo, N.E.; Fee, R.J.; Hinton, V.J. Parental stress in mothers of boys with Duchenne Muscular Dystrophy. J. Pediatr. Psychol. 2003, 28, 473–484. [Google Scholar] [CrossRef]
- McClintock, K.; Hall, S.; Oliver, C. Risk markers associated with challenging behaviours in people with intellectual disabilities: A meta-analytic study. J. Intellect. Disabil. Res. 2003, 47, 405–416. [Google Scholar] [CrossRef]
- Mayes, S.D.; Gorman, A.A.; Hillwig-Garcia, J.; Syed, E. Suicide ideation and attempts in children with Autism. Res. Autism Spectr. Disord. 2013, 7, 109–119. [Google Scholar] [CrossRef]
- Mayes, S.D.; Zickgraf, H. Atypical eating behaviors in children and adolescents with autism, ADHD, other disorders, and typical development. Res. Autism Spectr. Disord. 2019, 64, 76–83. [Google Scholar] [CrossRef]
- Schnabel, A.; Hallford, D.J.; Stewart, M.; McGillivray, J.A.; Forbes, D.; Austin, D.W. An Initial Examination of Post-Traumatic Stress Disorder in Mothers of Children with Autism Spectrum Disorder: Challenging Child Behaviors as Criterion A Traumatic Stressors. Autism Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, C.T.; Fairclough, D.L.; Noll, R.B. Problem-solving skills training for mothers of children recently diagnosed with autism spectrum disorder: A pilot feasibility study. Autism 2016, 20, 55–64. [Google Scholar] [CrossRef] [PubMed]
| Study | Year | Country | Sample | PTSD/PTSS Measures | PTSD/PTSS Rates | Risk/Protective Factors |
|---|---|---|---|---|---|---|
| Longitudinal studies | ||||||
| De Young et al. [60] | 2014 | Australia | 120 parents of children with burn injuries | PDS | PTSD: 22% at 1 month post-injury 5% at 6 months | Risk factors:
|
| Harper et al. [45] | 2013 | USA | 75 parents of pediatric cancer patients on the day of each of three medical procedures | IES-R | Not reported | Protective factors:
|
| Malin et al. [56] | 2019 | USA | 162 parents three months after discharge from ≥14 days of NICU | PPQ | PTSD: 25% | Risk factors:
|
| Young et al. [65] | 2003 | USA | 170 caregivers of pediatric transplant recipients | PDS | PTSD: 27.1% | Risk factors:
|
| Cross-sectional studies | ||||||
| Aftyka and Rozalska [55] | 2020 | Poland | 82 parents of infants previously treated in NICU | IES-R | PTSD: 68.5% fathers, 82.9% mothers | Risk factors:
|
| Bruce et al. [44] | 2011 | UK | 52 parents of children with brain tumor | IES-R | PTSD: 29% | Risk factors:
|
| Carmassi et al. [57] | 2018 | Italy | 134 Parents of children with a diagnosis of epilepsy | SCID-5 TALS-SR | PTSD: 10.4% parents (13.3% of the mothers and 4.5% of the fathers). Partial PTSD 37.3% (mothers 43.3% and fathers 25.0%) | Risk factors:
|
| Casey et al. [69] | 2012 | USA | 265 parents of children with ASD | IES-R | PTSS: 20% | Risk factors:
|
| Dell’Osso et al. [58] | 2018 | Italy | 134 parents (90 mothers and 44 fathers), of patients aged below 18 years old diagnosed with an epileptic syndrome | SCID-5; TALS-SR | PTSD: 10.4% (13.3% mothers and 4.5% fathers); 37.3% (43.3% of the mothers and 25.0% of the fathers) partial PTSD | Risk factors:
|
| Hawkins et al. [61] | 2019 | UK | 91 parents and primary caregivers (63 mothers, 25 fathers, 3 other) of children during the first 8 weeks following child’s burn injury | IES-R | PTSD: 32.8% of women, 40% of men | Risk factors:
|
| Ingerski et al. [66] | 2010 | USA | 64 parents of children with chronic illnesses | IES-R | PTSD: 12.9% (14.3% transplantation, 7.7% HIV, 14.3% SCD) | Risk factors:
|
| Jurbergs et al. [43] | 2009 | USA | 199 parents of children with cancer | IES-R | Not reported | Risk factors:
|
| Juth et al. [47] | 2015 | USA | 110 caregivers of AYAs cancer patients | PCL | Not reported | Risk factors:
|
| Khalifa et al. [46] | 2014 | Egypt | 96 parents of children with acute lymphoblastic leukemia and 22 parents of healthy controls. Patients divided into five groups according to disease phase | PTSD Assessment Scale | Not reported | Risk factors:
|
| Landolt et al. [41] | 2003 | Switzerland | 355 parents of children 5–6 weeks after an accident or a new diagnosis of cancer or diabetes mellitus type 1 | PDS | PTSD: 39.9% (16% fathers and 23.9% mothers) | Risk factors:
|
| Malpert et al. [48] | 2015 | USA | 127 parents of long-term survivors of childhood Acute Lymphoblastic Leukemia | IES-R | PTSS: 3.9% | Risk factors:
|
| Masa’deh and Jarrah [50] | 2017 | Jordan | 416 parents of children with cancer | PCL-C | Not reported | Risk factors:
|
| McCarthy et al. [49] | 2016 | Australia | 204 parent caregivers of AYAs diagnosed with cancer | PCL-S | PTSS: 42% | Risk factors:
|
| McCarthy et al. [52] | 2018 | Australia | 204 parent caregivers of AYAs diagnosed with cancer | PCL-S | Not reported | Risk factors:
|
| Odar et al. [59] | 2013 | USA | 45 parents of children with burn injuries | PCL-S | PTSD: 4.44% | Risk factors:
|
| Pasterski et al. [62] | 2014 | UK | 47 parents of children diagnosed with disorders of sex development | IES-R | PTSD: 49% | Risk factors:
|
| Perez et al. [53] | 2018 | USA | 59 caregivers of pediatric cancer patients | IES-R | PTSS: 25.42% | Risk factors:
|
| Perez et al. [63] | 2019 | USA | 139 parents (76 mothers and 63 fathers) of children with disorders of sex development | IES-R | PTSS: 17% | Risk factors:
|
| Perez et al. [54] | 2020 | USA | 145 caregivers of children diagnosed with cancer | IES-R | PTSS: 27.4% | Risk factors:
|
| Phipps et al. [42] | 2005 | USA | 120 parents of children with cancer | IES-R | Not reported | Risk factors:
|
| Sawyer et al. [51] | 2017 | Australia | 204 parents of AYAs with cancer | PCL-S | Not reported | Risk factors:
|
| Steinberg et al. [64] | 2012 | USA | 120 caregivers of children with asthma | SCID-I | PTSD: 20.83% (lifetime diagnosis, prior to the past 12-months) | Risk factors:
|
| Stewart et al. [71] | 2020 | Australia | 395 parents of children with ASD and rare diseases | PCL-5 | PTSD: 40.8% (ASD 23.5%; Rare diseases: 17.3%) | Risk factors:
|
| Taskiran et al. [68] | 2016 | Turkey | 27 mothers of children who underwent bone marrow transplantation | CAPS | PTSD: 57.6% | Risk factors:
|
| Tutus & Goldbeck [70] | 2016 | Germany | 113 parents of children and adolescents with PTSD | PDS | PTSS: 48.6% | Risk factors:
|
| Virtue et al. [67] | 2014 | USA | 215 caregivers of children undergoing hematopoietic stem cell transplant (HSCT) | IES-R | PTSS: 54% | Risk factors:
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carmassi, C.; Dell’Oste, V.; Foghi, C.; Bertelloni, C.A.; Conti, E.; Calderoni, S.; Battini, R.; Dell’Osso, L. Post-Traumatic Stress Reactions in Caregivers of Children and Adolescents/Young Adults with Severe Diseases: A Systematic Review of Risk and Protective Factors. Int. J. Environ. Res. Public Health 2021, 18, 189. https://doi.org/10.3390/ijerph18010189
Carmassi C, Dell’Oste V, Foghi C, Bertelloni CA, Conti E, Calderoni S, Battini R, Dell’Osso L. Post-Traumatic Stress Reactions in Caregivers of Children and Adolescents/Young Adults with Severe Diseases: A Systematic Review of Risk and Protective Factors. International Journal of Environmental Research and Public Health. 2021; 18(1):189. https://doi.org/10.3390/ijerph18010189
Chicago/Turabian StyleCarmassi, Claudia, Valerio Dell’Oste, Claudia Foghi, Carlo Antonio Bertelloni, Eugenia Conti, Sara Calderoni, Roberta Battini, and Liliana Dell’Osso. 2021. "Post-Traumatic Stress Reactions in Caregivers of Children and Adolescents/Young Adults with Severe Diseases: A Systematic Review of Risk and Protective Factors" International Journal of Environmental Research and Public Health 18, no. 1: 189. https://doi.org/10.3390/ijerph18010189
APA StyleCarmassi, C., Dell’Oste, V., Foghi, C., Bertelloni, C. A., Conti, E., Calderoni, S., Battini, R., & Dell’Osso, L. (2021). Post-Traumatic Stress Reactions in Caregivers of Children and Adolescents/Young Adults with Severe Diseases: A Systematic Review of Risk and Protective Factors. International Journal of Environmental Research and Public Health, 18(1), 189. https://doi.org/10.3390/ijerph18010189








