Parental Stress, Anxiety and Depression Symptoms Associated with Self-Efficacy in Paediatric Type 1 Diabetes: A Literature Review
Abstract
1. Introduction
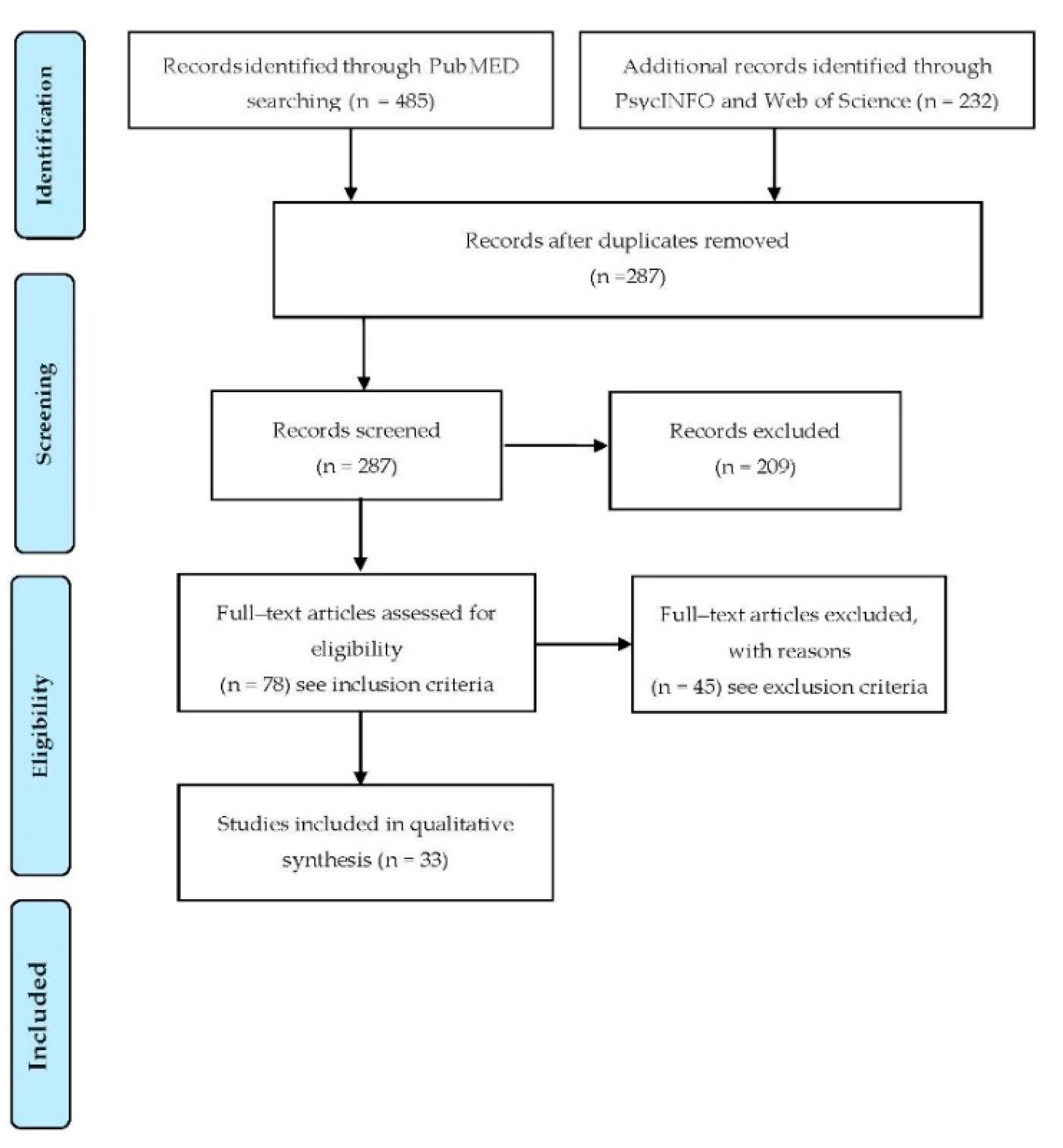
2. Materials and Methods
Search Strategy and Inclusion and Exclusion Criteria
3. Results
3.1. Parental Depression and Anxiety Symptoms
3.2. Parental Stress and Parenting Stress
3.3. The Role of Parental Self-Efficacy Related to Anxiety, Stress, and Depression Symptoms
3.4. Mothers Involvement in the Management of Children with T1DM
3.5. Fathers Involvement in the Management of Children with T1DM
4. Discussion
5. Conclusions
6. Limitations and Future Works of the Current Review
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States. U.S. Department of Health and Human Services; Atlanta. 2011. Available online: https://www.cdc.gov/diabetes/pubs/pdf/methods11.pdf (accessed on 2 October 2020).
- Miller, G.F.; Coffield, E.; Leroy, Z.; Wallin, R. Prevalence and Costs of Five Chronic Conditions in Children. J. Sch. Nurs. 2016, 32, 357–364. [Google Scholar] [CrossRef]
- Nemani, R.R. American Diabetes Association, Standards of Medical Care in Diabetes. Abridged for Primary Care Providers. Clin. Diabetes 2015, 33, 97–111. [Google Scholar] [CrossRef]
- Sullivan-Bolyai, S.; Deatrick, J.; Gruppuso, P.; Tamborlane, W.; Grey, M. Constant vigilance: Mothers’ work parenting young children with type 1 diabetes. J. Pediatr. Nurs. 2003, 18, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Helgeson, V.S.; Becker, D.; Escobar, O.; Siminerio, L. Families with Children with Diabetes: Implications of Parent Stress for Parent and Child Health. J. Pediatr. Psychol. 2012, 37, 467–478. [Google Scholar] [CrossRef] [PubMed]
- Zysberg, L.; Lang, T. Supporting parents of children with type 1 diabetes mellitus: A literature review. Patient Intell. 2015, 7, 21–31. [Google Scholar] [CrossRef]
- Flynn, R. Coping with children with diabetes: Is this burden too great for parents to bear? J. Endocrinol. Metab. Diabetes S. Afr. 2013, 18, 82–86. [Google Scholar] [CrossRef]
- Landolt, M.; Vollrath, M.E.; Laimbacher, J.; Gnehm, H.E.; Sennhauser, F.H. Prospective Study of Posttraumatic Stress Disorder in Parents of Children With Newly Diagnosed Type 1 Diabetes. J. Am. Acad. Child Adolesc. Psychiatry 2005, 44, 682–689. [Google Scholar] [CrossRef]
- American Psychological Association Dictionary of Psychology. Available online: https://dictionary.apa.org/ (accessed on 9 December 2020).
- Phillips, A.C. Perceived Stress. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013. [Google Scholar] [CrossRef]
- Raphael, J.L.; Zhang, Y.; Liu, H.; Giardino, A.P. Parenting stress in US families: Implications for paediatric healthcare utilization. Child Care Health Dev. 2009, 36, 216–224. [Google Scholar] [CrossRef]
- Lowes, L.; Gregory, J.W.; Lyne, P. Newly diagnosed childhood diabetes: A psychosocial transition for parents? J. Adv. Nurs. 2005, 50, 253–261. [Google Scholar] [CrossRef]
- American Diabetes Association 1. Improving Care and Promoting Health in Populations: Standards of Medical Care in Diabetes—2019. Diabetes Care 2018, 42 (Suppl. 1), S7–S12. [Google Scholar] [CrossRef]
- Cline, G.D.; Schwartz, D.D.; Axelrad, M.E.; Anderson, B. A Pilot Study of Acute Stress Symptoms in Parents and Youth Following Diagnosis of Type I Diabetes. J. Clin. Psychol. Med. Settings 2011, 18, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self–Efficacy. In The Exercise of Control; Freeman: New York, NY, USA, 1994. [Google Scholar]
- Bodenheimer, T.; Lorig, K.; Holman, H.; Grumbach, K. Patient Self-management of Chronic Disease in Primary Care. JAMA 2002, 288, 2469–2475. [Google Scholar] [CrossRef] [PubMed]
- Fornasini, S.; Miele, F.; Piras, E.M. The Consequences of Type 1 Diabetes Onset on Family Life. An Integrative Review. J. Child Fam. Stud. 2019, 29, 1467–1483. [Google Scholar] [CrossRef]
- Hansen, J.A.; Weissbrod, C.; Schwartz, D.D.; Taylor, W.P. Paternal involvement in pediatric Type 1 diabetes: Fathers’ and mothers’ psychological functioning and disease management. Fam. Syst. Health 2012, 30, 47–59. [Google Scholar] [CrossRef]
- Moreira, H.; Frontini, R.; Bullinger, M.; Canavarro, M.C. Caring for a Child with Type 1 Diabetes: Links between Family Cohesion, Perceived Impact, and Parental Adjustment. J. Fam. Psychol. 2013, 27, 731–742. [Google Scholar] [CrossRef]
- Streisand, R.; Mackey, E.R.; Elliot, B.M.; Mednick, L.; Slaughter, I.M.; Turek, J.; Austin, A. Parental anxiety and depression associated with caring for a child newly diagnosed with type 1 diabetes: Opportunities for education and counseling. Patient Educ. Couns. 2008, 73, 333–338. [Google Scholar] [CrossRef]
- Whittemore, R.; Jaser, S.; Chao, A.; Jang, M.; Grey, M. Psychological experience of parents of children with type 1 diabetes: A systematic mixed–studies review. Diabetes Educ. 2012, 38, 562–579. [Google Scholar] [CrossRef]
- Robinson, E.M.; Weaver, P.; Chen, R.; Streisand, R.; Holmes, C.S. A model of parental distress and factors that mediate its link with parental monitoring of youth diabetes care, adherence, and glycemic control. Health Psychol. 2016, 35, 1373–1382. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Vesco, A.T.; Dolan, L.M.; Hood, K.K. From Caregiver Psychological Distress to Adolescent Glycemic Control: The Mediating Role of Perceived Burden around Diabetes Management. J. Pediatr. Psychol. 2010, 36, 196–205. [Google Scholar] [CrossRef]
- Moreira, H.; Frontini, R.; Bullinger, M.; Canavarro, M.C. Family Cohesion and Health-Related Quality of Life of Children with Type 1 Diabetes: The Mediating Role of Parental Adjustment. J. Child Fam. Stud. 2014, 23, 347–359. [Google Scholar] [CrossRef]
- Noser, A.; Dai, H.; Marker, A.M.; Raymond, J.K.; Majidi, S.; Clements, M.A.; Stanek, K.R.; Patton, S.R. Parental depression and diabetes-specific distress after the onset of type 1 diabetes in children. Health Psychol. 2019, 38, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Patton, S.R.; Dolan, L.M.; Smith, L.B.; Thomas, I.H.; Powers, S.W. Pediatric Parenting Stress and Its Relation to Depressive Symptoms and Fear of Hypoglycemia in Parents of Young Children with Type 1 Diabetes Mellitus. J. Clin. Psychol. Med. Settings 2011, 18, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, K.A.; Johnson, S.B.; Barker, D.; Quittner, A.L.; Deeb, L.C.; Geller, D.E.; Gondor, M.; Silverstein, J.H. Risk Factors Associated with Depressive Symptoms in Caregivers of Children with Type 1 Diabetes or Cystic Fibrosis. J. Pediatr. Psychol. 2010, 35, 814–822. [Google Scholar] [CrossRef] [PubMed]
- Eckshtain, D.; Ellis, D.A.; Kolmodin, K.; Naar-King, S. The Effects of Parental Depression and Parenting Practices on Depressive Symptoms and Metabolic Control in Urban Youth with Insulin Dependent Diabetes. J. Pediatr. Psychol. 2009, 35, 426–435. [Google Scholar] [CrossRef] [PubMed]
- Jaser, S.S.; Whittemore, R.; Ambrosino, J.M.; Lindemann, E.; Grey, M. Mediators of Depressive Symptoms in Children with Type 1 Diabetes and their Mothers. J. Pediatr. Psychol. 2007, 33, 509–519. [Google Scholar] [CrossRef]
- Hilliard, M.E.; Monaghan, M.; Cogen, F.R.; Streisand, R. Parent stress and child behaviour among young children with type 1 diabetes. Child Care Health Dev. 2010, 37, 224–232. [Google Scholar] [CrossRef]
- Van Gampelaere, C.; Vervoort, T.; Luyckx, K.; De Paepe, A.; Van Aken, S.; Goubert, L. Maternal distress in the context of their child’s type 1 diabetes: Exploring the role of adaptive maternal emotion regulation on child outcomes. Psychol. Health Med. 2017, 23, 337–346. [Google Scholar] [CrossRef]
- Lewin, A.B.; Storch, E.A.; Silverstein, J.H.; Baumeister, A.L.; Strawser, M.S.; Geffken, G.R. Validation of the Pediatric Inventory for Parents in Mothers of Children With Type 1 Diabetes: An Examination of Parenting Stress, Anxiety, and Childhood Psychopathology. Fam. Syst. Health 2005, 23, 56–65. [Google Scholar] [CrossRef]
- Casaña–Granell, S.; Lacomba–Trejo, L.; Valero–Moreno, S.; Prado–Gasco, V.; Montoya–Castilla, I.; Pérez–Marín, M. A brief version of the Pediatric Inventory for Parents (PIP) in Spanish population: Stress of main family carers of chronic pediatric patients. PLoS ONE 2018, 13, e0201390. [Google Scholar] [CrossRef]
- Di Riso, D.; Bassi, G.; Mancinelli, E.; Zaffani, S.; Salcuni, S.; Claudio, M. Mothers and Fathers Parenting Stress and Their Perception of Children’s Psychosocial Functioning in Paediatric Diabetes: A Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 4734. [Google Scholar] [CrossRef]
- Monaghan, M.; Herbert, L.J.; Cogen, F.R.; Streisand, R. Sleep Behaviours and Parent Functioning in Young Children With Type 1 Diabetes. Child. Health Care 2012, 41, 246–259. [Google Scholar] [CrossRef] [PubMed]
- Schaaijk, N.M.M.-V.; Roeleveld-Versteegh, A.B.C.; Van Baar, A.L. The Interrelationships among Paternal and Maternal Parenting Stress, Metabolic Control, and Depressive Symptoms in Adolescents with Type 1 Diabetes Mellitus. J. Pediatr. Psychol. 2012, 38, 30–40. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Streisand, R.; Swift, E.; Wickmark, T.; Chen, R.; Holmes, C.S. Pediatric Parenting Stress Among Parents of Children with Type 1 Diabetes: The Role of Self-Efficacy, Responsibility, and Fear. J. Pediatr. Psychol. 2005, 30, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Noser, A.E.; Patton, S.R.; Van Allen, J.; Nelson, M.B.; Clements, M.A. Evaluating parents’ self-efficacy for diabetes management in paediatric type 1 diabetes. J. Pediatr. Psychol. 2017, 42, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Jaser, S.S.; Whittemore, R.; Ambrosino, J.M.; Lindemann, E.; Grey, M. Coping and Psychosocial Adjustment in Mothers of Young Children with Type 1 Diabetes. Child. Health Care 2009, 38, 91–106. [Google Scholar] [CrossRef] [PubMed]
- Clayton, K.M.; Stewart, S.M.; Wiebe, D.J.; McConnel, C.E.; Hughes, C.W.; White, P.C. Maternal depressive symptoms predict adolescent healthcare utilization and charges in youth with Type 1 diabetes (T1D). Health Psychol. 2013, 32, 1013–1022. [Google Scholar] [CrossRef]
- Wiebe, D.J.; Gelfand, D.; Butler, J.M.; Korbel, C.; Fortenberry, K.T.; McCabe, J.E.; Berg, C.A. Longitudinal Associations of Maternal Depressive Symptoms, Maternal Involvement, and Diabetes Management Across Adolescence. J. Pediatr. Psychol. 2011, 36, 837–846. [Google Scholar] [CrossRef]
- Hood, K.K. The Influence of Caregiver Depressive Symptoms on Proxy Report of Youth Depressive Symptoms: A Test of the Depression-Distortion Hypothesis in Pediatric Type 1 Diabetes. J. Pediatr. Psychol. 2008, 34, 294–303. [Google Scholar] [CrossRef]
- Rumburg, T.M.; Lord, J.H.; Savin, K.L.; Jaser, S.S. Maternal diabetes distress is linked to maternal depressive symptoms and adolescents’ glycemic control. Pediatr. Diabetes 2015, 18, 67–70. [Google Scholar] [CrossRef]
- Jaser, S.S.; Linsky, R.; Grey, M. Coping and Psychological Distress in Mothers of Adolescents with Type 1 Diabetes. Matern. Child. Health J. 2014, 18, 101–108. [Google Scholar] [CrossRef]
- Jaser, S.S.; Grey, D.R.M. A Pilot Study of Observed Parenting and Adjustment in Adolescents with Type 1 Diabetes and their Mothers. J. Pediatr. Psychol. 2009, 35, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Cameron, L.D.; Young, M.J.; Wiebe, D.J. Maternal trait anxiety and diabetes control in adolescents with type I diabetes. J. Pediatr. Psychol. 2007, 32, 733–744. [Google Scholar] [CrossRef] [PubMed]
- Mackey, E.; Struemph, K.; Powell, P.; Chen, R.; Streisand, R.; Holmes, C. Maternal Depressive Symptoms and Disease Care Status in Youth with Type 1 Diabetes. Health Psychol. 2014, 33, 783–791. [Google Scholar] [CrossRef]
- Mitchell, S.J.; Hilliard, M.E.; Mednick, L.; Henderson, C.; Cogen, F.R.; Streisand, R. Stress among fathers of young children with type 1 diabetes. Fam. Syst. Health 2009, 27, 314–324. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.M.; Berg, C.A.; King, P.; Gelfand, D.; Fortenberry, K.; Foster, C.; Wiebe, D.J. Parental negative affect and adolescent efficacy for diabetes management. J. Fam. Psychol. 2009, 23, 611–614. [Google Scholar] [CrossRef] [PubMed]
- Monaghan, M.C.; Hilliard, M.E.; Cogen, F.R.; Streisand, R. Supporting parents of very young children with type 1 diabetes: Results from a pilot study. Patient Educ. Couns. 2011, 82, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Mackey, E.R.; Herbert, L.; Monaghan, M.; Cogen, F.; Wang, J.; Streisand, R. The feasibility of a pilot intervention for parents of young children newly diagnosed with type 1 diabetes. Clin. Pract. Pediatr. Psychol. 2016, 4, 35–50. [Google Scholar] [CrossRef]
- Whittemore, R.; Coleman, J.; Delvy, R.; Zincavage, R.; Ambrosoli, J.A.; Shi, L.; Kato, B.; Marceau, L. An eHealth Program for Parents of Adolescents with T1DM Improves Parenting Stress: A Randomized Control Trial. Diabetes Educ. 2019, 46, 62–72. [Google Scholar] [CrossRef]
| Author/Year | Sample (N); Gender (N or %) | Parental Symptoms in Paediatric Diabetes Management | Main Results | Measurement Tools (Considered Cut-Off) |
|---|---|---|---|---|
| [18] * | n = 125 parents (82 mothers and 43 fathers) of children (age ranged between 7–14 years) with T1DM comprising a total of n = 89 families. | Stress; depression; anxiety; parents diabetes management | 55% of mothers and 22% of fathers met the cut-off for anxiety disorder, while for depression disorder 26% of mothers and 19% of fathers fell above the cut-off. Maternal perceptions of fathers’ helpfulness associates with decreased maternal depression symptoms and a better child regimen adherence Paternal perception of their own amount of involvement was related to increased paediatric parenting stress and anxiety. Their own perception of helpfulness was associated with poorer glycaemic control | Pediatric Inventory for Parents (PIP): self-report assessing parents’ parenting stress specific to caring for a child with a chronic disease. It assesses both the Difficulty and Frequency of the stress-eliciting situations. Hospital Anxiety and Depression Scale (HADS): self-report assessing anxiety and depression symptoms aimed at the general population (clinical cut-off: 8). Self-Care Inventory (SCI): self-report assessing parents’ adherence to diabetes regiment in their children with T1DM. |
| [19] * | n = 104 of parents (90.4% mothers) of children with T1DM (age ranged of 8 to 18 years); n = 142 parents (95.8% mothers) of healthy children (control group) (age ranged of 8 to 18 years). | Parental stress; anxiety; depression | 29.8% of parents scored within the moderate range or above the severe cut-off for anxiety disorders, while there was no significant difference in depression symptoms compared to the control group | Hospital Anxiety and Depression Scale (HADS): self-report assessing anxiety and depression symptoms aimed at the general population (symptoms severity: “normal” 0–7; “mild” 8–10; “moderate” 11–14; “severe” 15–21). Parenting Stress Index-Short Form (PSI-SF), Parental Distress subscale: self-report assessing parents distress referred to caring and rearing a child. |
| [20] * | n = 102 parents (62.61% mothers) of children (mean age = 9.7 years) with T1DM. | Anxiety; depression; parental stress; self-efficacy | Parents experienced especially high number of depression symptoms. 74% of parents met criteria for mild depression and 61% of the total sample met criteria for clinically significant depression. Parental clinical depression and anxiety were associated with paediatric parenting stress, and with lower self-efficacy for diabetes care. | State-Trait Anxiety Inventory (STAI): self-report assessing state and trait anxiety symptoms (clinical total score cut-off: 40). Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical total score cut-off: 22). Pediatric Inventory for Parents (PIP): self-report assessing parents’ parenting stress specific to caring for a child with a chronic disease. It assesses both the Difficulty and Frequency of the stress-eliciting situations. Self-Efficacy for Diabetes scale (SED): self-report adopted to assess parent perceived capacity (self-efficacy) to manage their children diabetes. |
| [21] **** | n = 34 articles included (systematic mixed–studies review) regarding parents, children and adolescents with T1DM. | Anxiety; depression; parenting stress; parental distress; parents diabetes management | Parental psychological distress ranged between 10% to 74% after the children’s diagnosis. Parental psychological distress also had negative effects on diabetes management. Themes of the qualitative synthesis indicated that parents perceived T1DM as a difficult diagnosis that contributed to significant family disruption. | N/A |
| [22] * | n = 257 preadolescents (age ranged of 11 to 14 years) with T1DM and their primary caregivers (91% mothers). | Parental distress (sum of depression, anxiety and stress symptoms); parental self-efficacy; parents diabetes management | Parents reported experiencing depression symptoms. Less distress indirectly related to greater monitoring through higher parental self-efficacy and more authoritative parenting then leading to better HbA1c. | Beck Depression Inventory-Second Ed. (BDI-II): self-report assessing depression symptoms (clinical total score cut-off: 29). Pediatric Inventory for Parents (PIP): self-report assessing parents’ parenting stress specific to caring for a child with a chronic disease. It assesses both the Difficulty and Frequency of the stress-eliciting situations. Hypoglycemic Fear Survey-Parents (HFS-P): self-report assessing anxiety referred to hypoglycemia. Self-Efficacy for Diabetes Self-Management Scale-Parent (SEDSM-P): self-report assessing parents perceived self-efficacy regarding diabetes tasks-related management. Parental Monitoring Diabetes Care Scale (PMDC): self-report assessing the frequency with which parents monitor specific diabetes-related tasks. 24-h DI: interview assessing the percentage of parents’ blood glucose check. Glycemic Control: glycosylated Hemoglobin (A1c) indexes average blood glucose levels. |
| [23] ** | n = 147 parents (130 mothers, 13 fathers, 2 grandmothers, and 2 aunts) of adolescents (age ranged of 13 to 18 years) with T1DM. | Parental Distress (sum of depression and anxiety symptoms); Parents diabetes management | The relationship between parents’ psychological distress and HbA1C levels were stronger for symptoms of depression compared to symptoms of anxiety. | State-Trait Anxiety Inventory (STAI-T)—Trait subscale: self-report assessing trait anxiety symptoms (clinical total score cut-off: 40). Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical total score cut-off: 16). Pediatric Assessment in Diabetes-Parent version (PAID-P): self-report assessing the burden related to the child diabetes management. [parental distress]. Glycemic Control: Hemoglobin A1c values measured through the DCA 2000. |
| [24] * | n = 88 dyads (92% mothers) comprising children with T1DM (56.8% girls; age ranged of 8 to 18 years), and one parent (age ranged of 29 to 59 years). n = 121 (94.2% mothers) dyads, comprising healthy children (55.4% girls; age ranged of 8 to 18 years) and one parent (age ranged of 30 to 59 years). | Family cohesion, parental stress, and emotional adjustment (anxiety and depression symptoms) | Parental diabetes-specific distress negatively impacts upon family cohesion and vice versa. | Family Environment Scale (FES)—Cohesion subscale: self-report assessing perceived commitment toward the family and of the family members supportiveness and helpfulness. Hospital Anxiety and Depression Scale (HADS): self-report assessing anxiety and depression symptoms aimed at the general population. Parenting Stress Index-Short Form (PSI-SF), Parental Distress subscale: self-report assessing parents distress referred to caring and rearing a child. |
| [25] ** | n = 125 families of 5- to 9-years-old children with new-onset T1DM completed study measures at baseline, n = 102 at 6-month follow-up, and n = 89 at 12-month follow-up. | Depression; T1DM-specific distress concerning daily T1DM management; worries about the future and long-term complications | Most of parents experienced paediatric specific distress after their children diagnosis of T1DM, which seems to be exacerbated by parental depression symptoms. Parents with depression symptoms reported lower levels of daily T1DM-specific distress compared to parents without these symptoms at baseline. Parents who experience depression symptom at baseline showed a smaller reduction of them at follow-up. | The Problems Ares in Diabetes Survey—Parent Revised Version (PAID-PR): self-report assessing parents distress specific to the burden associated to T1DM. Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical total score cut-off: 16). Glycemic Control: Hemoglobin A1c indexing average blood glucose levels in the preceding three months. |
| [26] * | n = 38 parents (32 mothers, 6 fathers) of children with T1DM (age ranged of 2 to 7 years). | Parental stress; depression | Parents report ranging between mild to moderate depression symptoms. Paediatric parenting stress is common in parents of young children with T1DM. | Pediatric Inventory for Parents (PIP): self-report assessing parents’ parenting stress specific to caring for a child with a chronic disease. It assesses both the Difficulty and Frequency of the stress-eliciting situations. Beck Depression Inventory-Second Ed. (BDI-II): self-report assessing depression symptoms. Hypoglycemia Fear Survey-Parents of Young Children (HFS-PSYC): self-report adapted to measure the anxiety related to hypoglycemia in parents of young children with diabetes. |
| [27] * | n = 195 parents of children (less than 12 years old) with T1DM. | Depression; stress | Several caregivers reported elevated symptoms of depression. The best predictors of depression symptoms for caregivers: lower caregivers’ education level, higher family stress, children older age, and poorer glycaemic control. | Family Stress Scale (FSS): self-report developed to assess illness-related stress and adapted to parents with children with T1DM. Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical total score cut-off: 16). Glycemic Control: Hemoglobin A1C (HbA1C) indexing average blood glucose levels in the preceding three months. Higher levels index worst control. |
| [28] * | n = 61 parents of children and adolescents (age ranged of 10 to 17 years) with T1DM. | Depression; parents diabetes management | Parental depression symptoms indirectly effect children and adolescents’ depressive symptoms and children and adolescents’ metabolic control through parental involvement and monitoring. Higher levels of parental depression relate to lower monitoring, inconsistent discipline, and lower parental involvement/warmth diabetes management. | Brief Symptoms Inventory 18 (BSI 18)—depression subscale: self-report assessing depression symptoms (clinical cut-off: 65). Alabama Parenting Questionnaire: self-report assessing general parenting skills. Considered subscales are “poor monitoring”, “involvement” and “inconsistent discipline”. Higher scores index greater warmth. Glycemic Control: Hemoglobin A1C (HbA1C) indexing average blood glucose levels in the preceding three months. |
| [29] * | n = 108 mothers (age ranged of 28 to 52 years) and their children with T1DM (60% females; age ranged of 8 to 12 years) | Depression | High levels of family general stress results as one of the risk factors for the onset of depression symptoms in parents. Maternal depression negatively affects children adjustment through its influence on children’s quality of life, coping, and family functioning. | Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical total score cut-off: 16). Diabetes Responsability and Conflict Scale (DRCS): self-report assessing the perceived distribution of diabetes-management related responsibilities and conflict between parents and children. |
| [30] * | n = 73 parents (97% mothers) of young child (age ranged of 2 to 6 years) with T1DM. | Parental stress; anxiety; parents diabetes management | Greater general anxiety and paediatric parenting stress associates with parents’ report of more problematic child behaviour while HbA1c monitoring was not influenced. | Pediatric Inventory for Parents (PIP): self-report assessing parents’ parenting stress specific to caring for a child with a chronic disease. It assesses both the Difficulty and Frequency of the stress-eliciting situations. State-Trait Anxiety Inventory (STAI): self-report assessing state and trait anxiety symptoms (clinical total score cut-off: 1 standard deviation above the sample mean). 24-h recall interview: two interviews assessing completion of diabetes-related tasks. |
| [31] * | n = 43 mothers-children dyads (age ranged of 8 to 15 years) with T1DM. | Parental distress; parenting stress | Maternal distress variables were strongly interrelated, with depression resulting as the greatest predictor of negative outcome for the children’s diabetes compared to anxiety. | Pediatric Inventory for Parents (PIP): self-report assessing parents’ parenting stress specific to caring for a child with a chronic disease. It assesses both the Difficulty and Frequency of the stress-eliciting situations. Hospital Anxiety and Depression Scale (HADS): self-report assessing anxiety and depression symptoms aimed at the general population. |
| [32] * | n = 28 mothers-children with T1DM dyads (11 boys; 17 girls; age ranged of 8 to 19 years). | Parental stress; anxiety | Greater maternal stress associates to both internalizing and externalizing symptoms of the child with T1DM | Pediatric Inventory for Parents (PIP): self-report assessing parents’ parenting stress specific to caring for a child with a chronic disease. It assesses both the Difficulty and Frequency of the stress-eliciting situations. |
| [33] * | n = 465 (85.2% mothers) main caregivers of children and adolescents with T1DM (age ranged of 9 and 18 years). | Stress; anxiety; Depression | Caregivers of children and adolescents diagnosed with diabetes were those with the highest levels of stress compared to parents of healthy children and adolescents. Age negatively associates with anxiety symptoms. | Pediatric Inventory for Parents (PIP): self-report assessing parents’ parenting stress specific to caring for a child with a chronic disease. It assesses both the Difficulty and Frequency of the stress-eliciting situations. Hospital Anxiety and Depression Scale (HADS): self-report assessing anxiety and depression symptoms aimed at the general population. |
| [34] * | n = 12 parental couples (Mothers. mean age = 40.25, SD = 6.58; Fathers, mean age = 42.5, SD = 6.38) of children with T1DM aged of 7 to 11 years (mean age = 8.8, SD = 0.996). | Parenting stress | Mothers and fathers seem to report comparable stress levels related to parenting a child with diabetes. Mothers seem to be more preoccupied with the internal suffering of their children with T1DM as they typically show greater feelings of sadness and anxiety compared to fathers. Scarce metabolic control, mediated by fathers’ perception of their children’s behavioural problems, seem to influence a specific aspect of parenting stress related to the parent-child dyad’s dysfunctional interaction | Parenting Stress-Fourth Edition- Index-Short Form (PSI-4-SF): self-report assessing parents distress referred to caring and rearing a child. |
| [35] * | n = 24 parents (females 88%; married 92%; mean age = 34.80 years) of children with T1DM (55% males; mean age = 4.1 years). | Parental stress; anxiety; depression | Children sleep issues and behavioural insomnia associates with increased parental stress, anxiety and depression symptoms, also affecting the intense insulin regimen. No association between anxiety and depression symptoms and children’s diabetes specific issues related to sleep. | Pediatric Inventory for Parents (PIP): self-report assessing parents’ parenting stress specific to caring for a child with a chronic disease. It assesses both the Difficulty and Frequency of the stress-eliciting situations. State-Trait Anxiety Inventory (STAI): self-report assessing state and trait anxiety symptoms. Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms. |
| [36] * | n = 229 parents (126 mothers and 103 fathers) of adolescents with T1DM (age ranged of 12 to 18 years) and a comparison group n = 126 (106 mothers and 55 fathers). | Parenting Stress | Fathers of adolescents with T1DM report significantly more parenting stress compared to mothers. | Parenting Stress-Index-Short Form (PSI-SF): self-report assessing parents stress referred to caring and rearing a child. |
| [37] * | n = 134 parents (86% mothers) of children with T1DM (age ranged of 9 to 17 years). | Parental stress; self-efficacy; parents diabetes management | Parenting stress negatively relaters to children’s age and positively relates to regimen status. Perception of lower self-efficacy and greater responsibility towards diabetes management in parents. | Self-Efficacy for Diabetes scale (SED): self-report adopted to assess parent perceived capacity (self-efficacy) to manage their children diabetes. Pediatric Inventory for Parents (PIP): self-report assessing parents’ parenting stress specific to caring for a child with a chronic disease. It assesses both the Difficulty and Frequency of the stress-eliciting situations. Diabetes Family Responsability Questionnaire (DFRQ): self-report assessing parents’ level of involvement and responsibility in their children diabetes management. |
| [38] | n = 135 families (82% mothers; 16% fathers; 1% caregivers) and children with T1DM (age ranged of 10 to 16 years). | Parental self–efficacy; diabetes management | High parental self-efficacy for diabetes management and the teaching of management skills may positively influence youth’s confidence for diabetes self-management. | Maternal Self-Efficacy for Diabetes Management Scale (MSED): self-report assessing the caregiver self-efficacy regarding the daily management of diabetes-related tasks. |
| [39] * | n = 67 mothers and children with T1DM (less than 8 years old) dyads. | Anxiety; depression; parents diabetes management | 21% of mothers reported clinically significant levels of anxiety symptoms. 24% of mothers reported clinically significant levels of depression symptoms. Maternal symptoms were not related to children’s metabolic control. | State-Trait Anxiety Inventory (STAI): self-report assessing state and trait anxiety symptoms (cut-off for high anxiety: 44). Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical cut-off: 16). Glycemic Control: Hemoglobin A1C (HbA1C) indexing average blood glucose levels in the preceding three months and assessed through the DCA 2000. |
| [40] ** | n = 220 mothers and children with T1DM dyads (age ranged of 11 to 19 years) of which n = 187 dyad (control group) it was used only the utilization/charge data while for the other n = 118 dyad CES-D and utilization/charge data. | Depression; parents diabetes management | Maternal depression does not associate with glycaemic control; however, adolescents of mothers with high depression symptoms were twice as likely to have an emergency room visit and three times as likely to be hospitalized | Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical cut-off: 16). Glycemic Control: Hemoglobin A1C (HbA1C) indexing average blood glucose levels in the preceding 3 months. |
| [41] ** | n = 82 mothers-adolescents with T1DM dyads (adolescents mean age = 12.79 years at baseline; mean age = 14.16 years at follow-up). | Depression; parents diabetes management | Parental depressive symptoms show a significant indirect effect on children depressive symptoms when the parental involvement was considered. The impact of maternal involvement varies as a function of their levels of depression symptoms and the adolescent age. | Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical cut-off: 16). Diabetes Responsability and Conflict Scale (DRCS): self-report assessing the perceived distribution of diabetes-management related responsibilities and conflict between parents and children. Glycemic Control: Hemoglobin A1C (HbA1C) indexing average blood glucose levels in the preceding 3 months. Higher levels index worse glycaemic control. |
| [42] * | n = 187 parents (82% mothers) of children and adolescents (age ranged of 10 to 18 years) with T1DM. | Depression | Caregivers with high scores on depression symptoms report high levels of youth depression symptoms at both high and low levels of youth-reported depression symptoms. | Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical cut-off: 16). |
| [43] * | n = 81 mothers of adolescents (age ranged of 10 to 16 years) with T1DM. | Depression; parental diabetes-distress | Most common diagnosis was depression in parents with children with T1DM. Maternal depression was the only significant predictor of adolescents’ glycaemic control. | Parent Diabetes Distress Scale (P-DDS): self-report assessing the distress referred to the self, the teen child, the relationships with the teen child and the teen child healthcare team. (moderate distress: 2–3 [mean score]; high distress: < or = 3 [mean score]). Patient Health Questionnaire (PHQ-9): self-report assessing depression symptoms as referred to DSM-V major depressive disorder. (mild depression = 5–9; moderate depression = 10–14; moderately severe depression = 15–19; severe depression = 20–27). |
| [44] * | n = 118 mothers-adolescents with T1DM (age ranged of 10 to 16 years) dyads. | Parental stress; parental distress (sum of depression anche anxiety symptoms); parents diabetes management | Mothers report diabetes-related-stress. Maternal coping is not significantly associated with adolescents’ health outcomes. | Responses to Stress Questionnaire (RSQ): self-report assessing the frequency of experiencing diabetes-related stress referred to diabetes task-related management. Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical cut-off: 16). State-Trait Anxiety Inventory (STAI): self-report assessing state and trait anxiety symptoms (range indicating high anxiety: 20–80). Diabetes Responsability and Conflict Scale (DRCS): self-report assessing the perceived distribution of diabetes-management related responsibilities and conflict between parents and children (range for greater parent-child conflict = 15–75). Glycemic Control: Hemoglobin A1C (HbA1C) indexing average blood glucose levels in the preceding 3 months and measured through the DCS 2000. |
| [45] * | n = 30 adolescents (age ranged of 10 to 16 years) with T1DM and their mothers (NA). | Diabetes-related stress; anxiety; depression; parents diabetes management | Maternal anxiety and depression symptoms were related to lower levels of child–centred parenting and higher level of hostility. Higher levels of observed parental influence (i.e., attempts to regulate or control children’s behaviour) is related to greater symptoms of depression and poorer quality of life in adolescents. | Responses to Stress Questionnaire (RSQ): self-report assessing the frequency of experiencing diabetes-related stress referred to diabetes task-related management [the items were considered to assess parent-child interaction]. Iowa Family Interaction Rating Scale (IFIRS): observational measure aimed at assessing parents’ behaviour [considered dimension: hostility; parental influence; sensitivity/child centered; positive reinforcement]. Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical cut-off: 16). State-Trait Anxiety Inventory (STAI): self-report assessing state and trait anxiety symptoms (cut off for high anxiety: 44). Glycemic Control: Hemoglobin A1C (HbA1C) indexing average blood glucose levels in the preceding 3 months and measured through the DCA 2000. |
| [46] * | n = 47 fathers and mothers of adolescents with T1DM (age ranged of 13 to 18 years). | Anxiety; parents diabetes management | Trait–anxious mothers report more responsibility referred to diabetes management tasks and perceive their adolescents as having poorer management skills. Results differ based on children age. Intervention should address maternal anxiety. | Illness Perceptions Scale-Revised: self-report assessing the distress related to diabetes. Diabetes Responsability and Conflict Scale (DRCS): self-report assessing the perceived distribution of diabetes-management related responsibilities and conflict between parents and children. State-Trait Anxiety Inventory (STAI): self-report assessing state and trait anxiety symptoms. Glycemic Control: Hemoglobin A1C (HbA1C) indexing average blood glucose levels in the preceding 3 months. Higher levels index worse glycaemic control. |
| [47] *** | n = 225 mothers and their young adolescents with T1DM (age ranged of 11 to 14 years) | Depression | More maternal depressive symptoms were directly related to less parental monitoring and more conflict, which in turn each were related to lower adherence | Beck Depression Inventory-Second Ed. (BDI-II): self-report assessing depression symptoms (clinical total score cut-off: 29). Parent Monitoring of Diabetes Scale (PMDS): self-report assessing the monitoring of diabetes-care related behaviours on the part of parents. 24-h recall interview: two interviews assessing completion of diabetes-related tasks. |
| [48] * | n = 43 fathers of children (age ranged of 2 to 6 years) with T1DM. | Parental stress; parents diabetes management; anxiety; self-efficacy. | Fathers’ paediatric parenting stress is positively associated with state anxiety and mother-reported difficult child behaviour. Fathers report higher self-efficacy and hope that mothers. | Pediatric Inventory for Parents (PIP): self-report assessing parents’ parenting stress specific to caring for a child with a chronic disease. It assesses both the Difficulty and Frequency of the stress-eliciting situations. 24-h recall interview: two interviews assessing completion of diabetes-related tasks. Self-Efficacy for Diabetes scale (SED): self-report adopted to assess parent perceived capacity (self-efficacy) to manage their children diabetes. Hypoglycemic Fear Survey-Parents (HFS-P): self-report assessing anxiety referred to hypoglycemia. State-Trait Anxiety Inventory-State subscale (STAI-S): self-report assessing state anxiety symptoms. Glycemic Control: Hemoglobin A1C (HbA1C) indexing average blood glucose levels in the preceding 3 months. |
| [49] * | n = 188 fathers and mothers of adolescents with T1DM. | Depression; anxiety; self-efficacy | Association between their the paternal perceptions of self-efficacy and the adolescent self-efficacy. Mothers’ perceptions were not reported. | Parents Self-efficacy: assessed by answering questions referred to the capacity of their teen child to manage their diabetes. State-Trait Anxiety Inventory-State subscale (STAI-T): self-report assessing trait anxiety symptoms. Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms (clinical cut-off: 16). |
| [5] ** | n = 132 adolescents with T1DM (53% females; age ranged of 10.7 to 14.21 years) with one primary caregiver (92% mothers, 7% fathers, 1% grandmother). | Parental general stress; parent diabetes-specific stress; depression; parents diabetes management | Greater parent general stress and greater parent diabetes-specific stress were associated with poorer parent mental health. General stress predicted an increase in parental depression symptoms. Parental diabetes-specific stress was associated with more frequent HbA1c monitoring and better self-care behaviours as reported by the child. | Norris & Uhl’s chronic stress measure- financial, marital, parenting stress subscales: self-report assessing parents general stress in the past 6 months. Impact on Family Scale (IFS)-family strain, personal strain, social strain subscales: self-report measure assessing the stress referred to caring for a child with a chronic illness. Center for Epidemiologic Studies Depression (CESD): self-report assessing depression symptoms. Glycemic Control: Hemoglobin A1C (HbA1C). Higher levels index worse glycemic control. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bassi, G.; Mancinelli, E.; Di Riso, D.; Salcuni, S. Parental Stress, Anxiety and Depression Symptoms Associated with Self-Efficacy in Paediatric Type 1 Diabetes: A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 152. https://doi.org/10.3390/ijerph18010152
Bassi G, Mancinelli E, Di Riso D, Salcuni S. Parental Stress, Anxiety and Depression Symptoms Associated with Self-Efficacy in Paediatric Type 1 Diabetes: A Literature Review. International Journal of Environmental Research and Public Health. 2021; 18(1):152. https://doi.org/10.3390/ijerph18010152
Chicago/Turabian StyleBassi, Giulia, Elisa Mancinelli, Daniela Di Riso, and Silvia Salcuni. 2021. "Parental Stress, Anxiety and Depression Symptoms Associated with Self-Efficacy in Paediatric Type 1 Diabetes: A Literature Review" International Journal of Environmental Research and Public Health 18, no. 1: 152. https://doi.org/10.3390/ijerph18010152
APA StyleBassi, G., Mancinelli, E., Di Riso, D., & Salcuni, S. (2021). Parental Stress, Anxiety and Depression Symptoms Associated with Self-Efficacy in Paediatric Type 1 Diabetes: A Literature Review. International Journal of Environmental Research and Public Health, 18(1), 152. https://doi.org/10.3390/ijerph18010152





