Coping Mechanisms: Exploring Strategies Utilized by Japanese Healthcare Workers to Reduce Stress and Improve Mental Health during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Survey Items
2.3. Data Analysis
3. Results
3.1. Demographics
3.2. Severity of Mental Health Problems and Associated Factors
3.3. Resilience Factors for Mental Health Outcomes
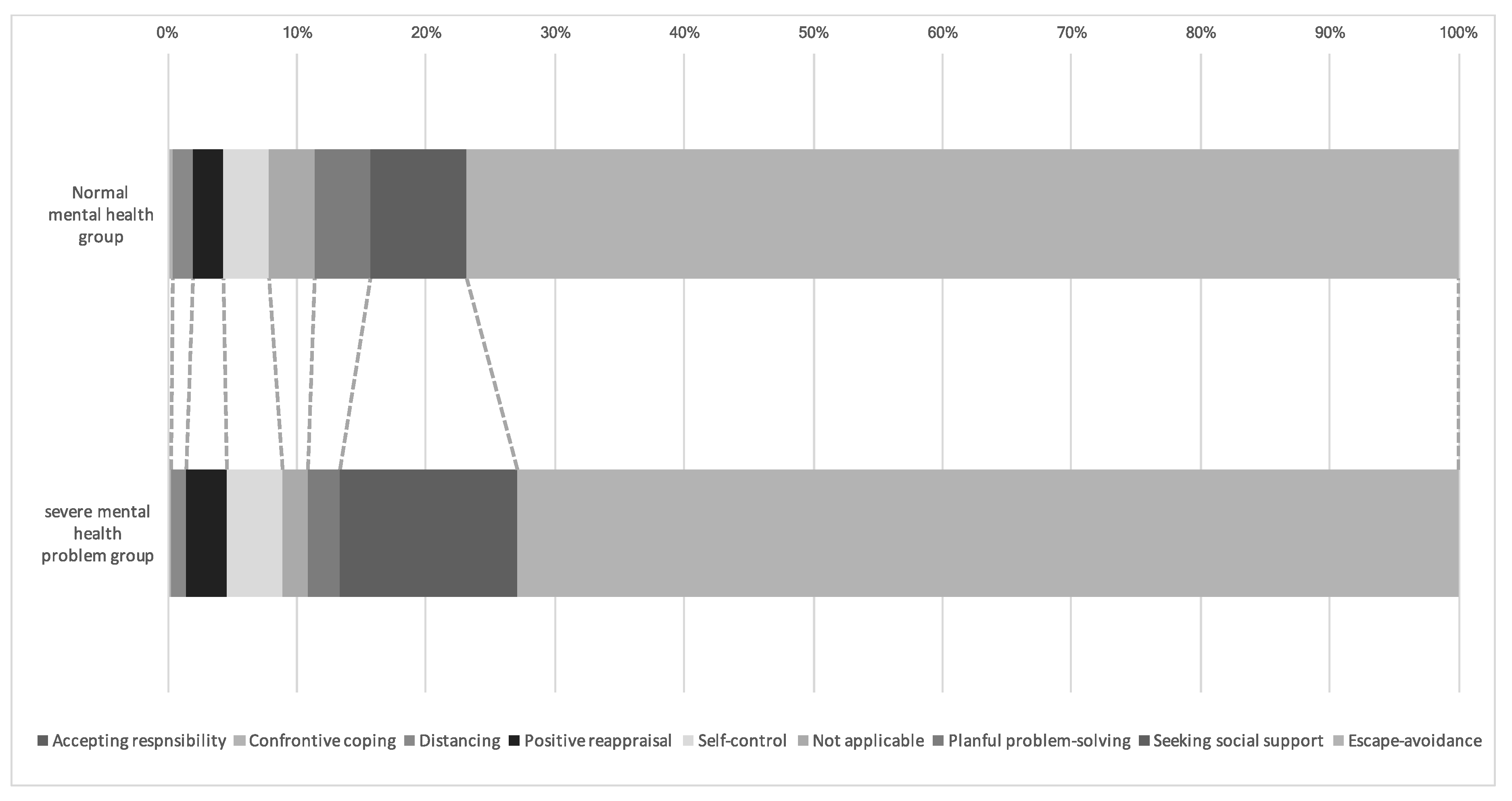
3.4. Coping Strategy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- The Case of the Coronavirus 31 March 2020. Updates on COVID-19 in Japan. Available online: https://www.mhlw.go.jp/content/10900000/000617550.pdf (accessed on 31 May 2020).
- World Health Organisation Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV). Available online: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (accessed on 29 June 2020).
- Basic Policies for Novel Coronavirus Disease Control. Available online: https://corona.go.jp/en/news/pdf/000632651.pdf (accessed on 31 May 2020).
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Stuijfzand, S.; Deforges, C.; Sandoz, V.; Sajin, C.-T.; Jaques, C.; Elmers, J.; Horsch, A. Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: A rapid review. BMC Public Health 2020, 20, 1230. [Google Scholar] [CrossRef]
- Gu, J.; Zhong, Y.; Hao, Y.; Zhou, D.; Tsui, H.; Hao, C.; Gao, Q.; Ling, W.; Lau, J.T.F. Preventive Behaviors and Mental Distress in Response to H1N1 Among University Students in Guangzhou, China. Asia Pac. J. Public Health 2012, 27, NP1867–NP1879. [Google Scholar] [CrossRef] [PubMed]
- Nachega, J.B.; Morroni, C.; Zuniga, J.M.; Sherer, R.; Beyrer, C.; Solomon, S.; Schechter, M.; Rockstroh, J. HIV-Related Stigma, Isolation, Discrimination, and Serostatus Disclosure: A global survey of 2035 HIV-infected adults. J. Int. Assoc. Physicians AIDS Care 2012, 11, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Tam, C.W.C.; Pang, E.P.F.; Lam, L.C.W.; Chiu, H.F.K. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004, 34, 1197–1204. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Uchiumi, C.; Suzuki, N.; Yoshimoto, J.; Murillo-Rodriguez, E. The Psychological Impact of ‘Mild Lockdown’ in Japan during the COVID-19 Pandemic: A Nationwide Survey under a Declared State of Emergency. Int. J. Environ. Res. Public Health 2020, 17, 9382. [Google Scholar] [CrossRef]
- Suzuki, Y.; Maeda, N.; Hirado, D.; Shirakawa, T.; Urabe, Y. Physical Activity Changes and Its Risk Factors among Community-Dwelling Japanese Older Adults during the COVID-19 Epidemic: Associations with Subjective Well-Being and Health-Related Quality of Life. Int. J. Environ. Res. Public Health 2020, 17, 6591. [Google Scholar] [CrossRef]
- Sanghera, J.; Pattani, N.; Hashmi, Y.; Varley, K.F.; Cheruvu, M.S.; Bradley, A.; Burke, J.R. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting—A Systematic Review. J. Occup. Health 2020, 62, e12175. [Google Scholar] [CrossRef]
- Venkatesh, A.; Edirappuli, S. Social distancing in covid-19: What are the mental health implications? BMJ 2020, 369, m1379. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- Main, A.; Zhou, Q.; Ma, Y.; Luecken, L.J.; Liu, X. Relations of SARS-related stressors and coping to Chinese college students’ psychological adjustment during the 2003 Beijing SARS epidemic. J. Couns. Psychol. 2011, 58, 410–423. [Google Scholar] [CrossRef] [PubMed]
- Shih, F.-J.; Turale, S.; Lin, Y.-S.; Gau, M.-L.; Kao, C.-C.; Yang, C.-Y.; Liao, Y.-C. Surviving a life-threatening crisis: Taiwan’s nurse leaders’ reflections and difficulties fighting the SARS epidemic. J. Clin. Nurs. 2009, 18, 3391–3400. [Google Scholar] [CrossRef] [PubMed]
- Iwata, N.; Okuyama, Y.; Kawakami, Y.; Saito, K. The twelve-item General Health Questionnaire among Japanese workers. J. Environ. Sci. Hokkaido Univ. 1988, 11, 1–10. [Google Scholar]
- Goldberg, D.P.; Gater, R.; Sartorius, N.; Ustun, T.B.; Piccinelli, M.; Gureje, O.; Rutter, C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 1997, 27, 191–197. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Oldehinkel, T.; Ormel, J. Why GHQ threshold varies from one place to another. Psychol. Med. 1998, 28, 915–921. [Google Scholar] [CrossRef]
- Nagasu, M.; Kogi, K.; Yamamoto, I. Association of socioeconomic and lifestyle-related risk factors with mental health conditions: A cross-sectional study. BMC Public Health 2019, 19, 1759. [Google Scholar] [CrossRef]
- Law, M.; Baptiste, S.; McColl, M.; Opzoomer, A.; Polatajko, H.; Pollock, N. The Canadian Occupational Performance Measure: An Outcome Measure for Occupational Therapy. Can. J. Occup. Ther. 1990, 57, 82–87. [Google Scholar] [CrossRef]
- Carswell, A.; McColl, M.A.; Baptiste, S.; Law, M.; Polatajko, H.; Pollock, N. The Canadian Occupational Performance Measure: A Research and Clinical Literature Review. Can. J. Occup. Ther. 2004, 71, 210–222. [Google Scholar] [CrossRef]
- Yoshikawa, H. Practice Guidebook of Copm and Amps to Better Un-Derstand Occupation; Igaku-Shoin Ltd.: Tokyo, Japan, 2014. [Google Scholar]
- Folkman, S.; Lazarus, R.S.; Dunkel-Schetter, C.; DeLongis, A.; Gruen, R.J. Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. J. Personal. Soc. Psychol. 1986, 50, 992. [Google Scholar] [CrossRef]
- Annual Report on Occupational Therapy. Available online: https://www.jaot.or.jp/files/page/wp-content/uploads/2010/08/OTwhitepepar2015.pdf (accessed on 7 December 2020).
- Japanese Physical Therapy Association. Available online: http://www.japanpt.or.jp/about/data/statistics/ (accessed on 7 December 2020).
- Bazazan, A.; Dianat, I.; Rastgoo, L.; Zandi, H. Relationships between dimensions of fatigue and psychological distress among public hospital nurses. Health Promot. Perspect. 2018, 8, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Zürcher, S.J.; Kerksieck, P.; Adamus, C.; Burr, C.M.; Lehmann, A.I.; Huber, F.K.; Richter, D. Prevalence of Mental Health Problems During Virus Epidemics in the General Public, Health Care Workers and Survivors: A Rapid Review of the Evidence. Front. Public Health 2020, 8, 560389. [Google Scholar] [CrossRef] [PubMed]
- Chew, Q.H.; Wei, K.C.; Vasoo, S.; Sim, K. Psychological and Coping Responses of Health Care Workers Toward Emerging Infectious Disease Outbreaks: A Rapid Review and Practical Implications for the COVID-19 Pandemic. J. Clin. Psychiatry 2020, 81. [Google Scholar] [CrossRef]
- Galea, S.; Merchant, R.M.; Lurie, N. The Mental Health Consequences of COVID-19 and Physical Distancing: The need for prevention and early intervention. JAMA Intern. Med. 2020, 180, 817–818. [Google Scholar] [CrossRef]
- Liang, L.; Ren, H.; Cao, R.; Hu, Y.; Qin, Z.; Li, C.; Mei, S. The Effect of COVID-19 on Youth Mental Health. Psychiatr. Q. 2020, 91, 11–12. [Google Scholar] [CrossRef]
- Bai, Y.-M.; Lin, C.-C.; Lin, C.-Y.; Chao-Cheng, L.; Chue, C.-M.; Chou, P. Survey of Stress Reactions Among Health Care Workers Involved With the SARS Outbreak. Psychiatr. Serv. 2004, 55, 1055–1057. [Google Scholar] [CrossRef]
- Ramaci, T.; Barattucci, M.; Ledda, C.; Rapisarda, V. Social Stigma during COVID-19 and its Impact on HCWs Outcomes. Sustainability 2020, 12, 3834. [Google Scholar] [CrossRef]
- Satici, B.; Gocet-Tekin, E.; Deniz, M.E.; Satici, S.A. Adaptation of the Fear of COVID-19 Scale: Its Association with Psychological Distress and Life Satisfaction in Turkey. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef]
- Albert, K.; Pruessner, J.; Newhouse, P.A. Estradiol levels modulate brain activity and negative responses to psychosocial stress across the menstrual cycle. Psychoneuroendocrinology 2015, 59, 14–24. [Google Scholar] [CrossRef]
- Mushtaq, R.; Shoib, S.; Shah, T.; Mushtaq, S. Relationship Between Loneliness, Psychiatric Disorders and Physical Health ? A Review on the Psychological Aspects of Loneliness. J. Clin. Diagn. Res. 2014, 8, WE01–WE04. [Google Scholar] [CrossRef] [PubMed]
- E Beutel, M.; Klein, E.M.; Brähler, E.; Reiner, I.C.; Jünger, C.; Michal, M.; Wiltink, J.; Wild, P.S.; Münzel, T.; Lackner, K.J.; et al. Loneliness in the general population: Prevalence, determinants and relations to mental health. BMC Psychiatry 2017, 17. [Google Scholar] [CrossRef] [PubMed]
- Faragher, E.B.; Cass, M.; Cooper, C.L. The relationship between job satisfaction and health: A meta-analysis. Occup. Environ. Med. 2005, 62, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Foster, K.; Roche, M.; Delgado, C.; Cuzzillo, C.; Giandinoto, J.; Furness, T. Resilience and mental health nursing: An integrative review of international literature. Int. J. Ment. Health Nurs. 2019, 28, 71–85. [Google Scholar] [CrossRef]
- Toyoshima, M.; Kaneko, Y.; Motohashi, Y. Leisure-time activities and psychological distress in a suburban community in Japan. Prev. Med. Rep. 2016, 4, 1–5. [Google Scholar] [CrossRef]
- Puyat, J.H.; Kazanjian, A.; Wong, H.; Goldner, E. Comorbid Chronic General Health Conditions and Depression Care: A Population-Based Analysis. Psychiatr. Serv. 2017, 68, 907–915. [Google Scholar] [CrossRef]
- Tugade, M.M.; Fredrickson, B.L. Resilient Individuals Use Positive Emotions to Bounce Back From Negative Emotional Experiences. J. Pers. Soc. Psychol. 2004, 86, 320–333. [Google Scholar] [CrossRef]
- Wang, H.; Xia, Q.; Xiong, Z.; Li, Z.; Xiang, W.; Yuan, Y.; Liu, Y.; Li, Z. The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: A web-based survey. PLoS ONE 2020, 15, e0233410. [Google Scholar] [CrossRef]
- Blake, H.; Bermingham, F.; Johnson, G.; Tabner, A. Mitigating the Psychological Impact of COVID-19 on Healthcare Workers: A Digital Learning Package. Int. J. Environ. Res. Public Health 2020, 17, 2997. [Google Scholar] [CrossRef]
- Wang, J.; Mann, F.; Lloyd-Evans, B.; Ma, R.; Johnson, S. Associations between loneliness and perceived social support and outcomes of mental health problems: A systematic review. BMC Psychiatry 2018, 18, 156. [Google Scholar] [CrossRef]
- Parry, D.; Oeppen, R.; Amin, M.S.A.; Brennan, P. Could exercise improve mental health and cognitive skills for surgeons and other healthcare professionals? Br. J. Oral Maxillofac. Surg. 2018, 56, 367–370. [Google Scholar] [CrossRef] [PubMed]
- Mouradian, L.E.; Degrace, B.W.; Thompson, D.M. Art-Based Occupation Group Reduces Parent Anxiety in the Neonatal Intensive Care Unit: A Mixed-Methods Study. Am. J. Occup. Ther. 2013, 67, 692–700. [Google Scholar] [CrossRef] [PubMed]
- Chew, Q.H.; Wei, K.C.; Vasoo, S.; Chua, H.C.; Sim, K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: Practical considerations for the COVID-19 pandemic. Singap. Med. J. 2020, 61, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Penley, J.A.; Tomaka, J.; Wiebe, J.S. The Association of Coping to Physical and Psychological Health Outcomes: A Meta-Analytic Review. J. Behav. Med. 2002, 25, 551–603. [Google Scholar] [CrossRef] [PubMed]
- Folkman, S.; Lazarus, R.S. An analysis of coping in a middle-aged community sample. J. Health Soc. Behav. 1980, 21, 219–239. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, N.; Tein, J.-Y.; Sandler, I.N.; Friedman, R.J. On the Limits of Coping: Interaction between stress and coping for inner-city adolescents. J. Adolesc. Res. 2001, 16, 372–395. [Google Scholar] [CrossRef]
- Hoare, E.; Milton, K.; Foster, C.; Allender, S. The associations between sedentary behaviour and mental health among adolescents: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 108. [Google Scholar] [CrossRef]
- McNicol, M.L.; Thorsteinsson, E.B. Internet Addiction, Psychological Distress, and Coping Responses Among Adolescents and Adults. Cyberpsychology Behav. Soc. Netw. 2017, 20, 296–304. [Google Scholar] [CrossRef]
- Lesser, I.A.; Nienhuis, C.P. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef]
| Characteristics | Number (%) |
|---|---|
| Gender | |
| Men | 307 (46.4) |
| Women | 354 (53.6) |
| Age, years | |
| 21–25 | 164 (24.8) |
| 26–30 | 201 (30.4) |
| 31–40 | 198 (30.0) |
| >40 | 98 (14.8) |
| Marital status | |
| Single | 380 (57.5) |
| Married | 281 (42.5) |
| Occupation | |
| Physician | 8 (1.2) |
| Nurse | 8 (1.2) |
| Physical therapist | 122 (18.5) |
| Occupational therapist | 507 (76.7) |
| Speech therapist | 16 (2.4) |
| Workplace clinical phase | |
| Acute | 219 (33.1) |
| Subacute | 215 (32.5) |
| Chronic | 227 (34.3) |
| Region of residence | |
| Alert region a | 506 (76.6) |
| Non-alert region | 155 (23.4) |
| Clinical experience, years | |
| 1–5 | 255 (38.6) |
| 6–10 | 197 (29.8) |
| 11–20 | 163 (24.7) |
| >20 | 46 (7.0) |
| Number of household members | |
| 1 (participant only) | 195 (29.5) |
| 2 people | 145 (21.9) |
| ≥3 | 321 (48.6) |
| Children ≤ 18 years in household | |
| Yes | 200 (30.3) |
| No | 461 (69.7) |
| Financial situation | |
| No change | 505 (76.4) |
| Worse than usual | 66 (10.0) |
| Better than usual | 90 (13.6) |
| Communication with family | |
| Same as usual | 324 (49.0) |
| Less than usual | 114 (17.2) |
| More than usual | 223 (33.7) |
| Communication with friends | |
| Same as usual | 192 (29.0) |
| Less than usual | 403 (61.0) |
| More than usual | 66 (10.0) |
| Gender | Workplace Phase | Place of Residence | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | |||||||||
| Measurements | Total | Men | Women | p Value | Acute | Subacute | Chronic | p Value | Alert Region a | Non-Alert Region | p Value |
| GHQ-12 | 5 (3–7) | 4 (2–7) | 6 (3–7.75) | <0.001 | 5 (2–7) | 5 (2–7) | 6 (3–8) | 0.85 | 5 (3–7) | 5 (3–7) | 0.79 |
| Anxiety over COVID-19 | 9 (7–10) | 8 (7–10) | 9 (8–10) | <0.001 | 9 (7–10) | 8 (7–10) | 9 (7–10) | 0.75 | 8 (7–10) | 9 (7–10) | 0.91 |
| Health status | 7 (5–9) | 7 (5–9) | 7 (5–8) | 0.22 | 7 (5–9) | 7 (5–9) | 7 (4.5–8) | 0.26 | 7 (5–8) | 7 (5–9) | 0.74 |
| Satisfaction with daily life | |||||||||||
| Satisfaction with leisure | 2 (1–3) | 3 (1–4) | 2 (1–3) | <0.001 | 2 (1–3) | 2 (1–3.5) | 2 (1–4) | 0.73 | 2 (1–3.5) | 2 (1–3) | 0.32 |
| Satisfaction with work | 6 (3–8) | 6 (3–8) | 5 (3.3–7) | 0.22 | 5 (3–7) | 6 (4–8) | 5 (3–7) | 0.01 | 5 (3.5–7) | 6 (3–8) | 0.59 |
| Satisfaction with daily life activities | 4 (3–7) | 5 (3–7) | 4 (3–7) | 0.34 | 5 (3–7) | 4 (3–6) | 5 (3–7) | 0.20 | 4 (3–7) | 4 (3–7) | 0.84 |
| Satisfaction with new activities | 6 (3–8) | 6 (2–8) | 6 (3–8) | 0.25 | 6 (3–8) | 6 (3–8) | 6 (3–8) | 0.73 | 6 (2–8) | 6 (3–8) | 0.45 |
| Characteristics | Normal (n = 221), Number (%) | Severe (n = 440), Number (%) |
|---|---|---|
| Gender | ||
| Men | 130 (58.8) | 177 (40.2) |
| Women | 91 (41.2) | 263 (59.8) |
| Age, years | ||
| 21–25 | 47 (21.3) | 117 (26.6) |
| 26–30 | 70 (31.7) | 131 (29.8) |
| 31–40 | 71 (32.1) | 127 (28.9) |
| >40 | 33 (14.9) | 65 (14.8) |
| Marital status | ||
| Single | 112 (50.7) | 268 (60.9) |
| Married | 109 (49.3) | 172 (39.1) |
| Occupation | ||
| Physician | 5 (2.3) | 3 (0.7) |
| Nurse | 2 (0.9) | 6 (1.4) |
| Physical therapist | 50 (22.6) | 72 (16.4) |
| Occupational therapist | 160 (72.4) | 347 (78.9) |
| Speech therapist | 4 (1.8) | 12 (2.7) |
| Workplace clinical phase | ||
| Acute | 74 (33.5) | 145 (33.0) |
| Subacute | 78 (35.3) | 137 (31.1) |
| Chronic | 69 (31.2) | 158 (35.9) |
| Region of residence | ||
| Alert region a | 170 (76.9) | 336 (76.4) |
| Non-alert region | 51 (23.1) | 104 (23.6) |
| Clinical experience, years | ||
| 1–5 | 76 (34.4) | 179 (40.7) |
| 6–10 | 72 (32.6) | 125 (29.4) |
| 11–20 | 59 (26.7) | 104 (23.6) |
| >20 | 14 (6.3) | 32 (7.3) |
| Household members | ||
| 1 | 48 (21.7) | 147 (33.4) |
| 2 | 53 (24.0) | 92 (20.9) |
| ≥3 | 120 (54.3) | 201 (45.7) |
| Children ≤ 18 years in household | ||
| Yes | 81 (36.7) | 119 (27.0) |
| No | 140 (63.3) | 321 (73.0) |
| Financial situation | ||
| No change | 177 (80.1) | 328 (74.5) |
| Worse than usual | 18 (8.1) | 48 (10.9) |
| Better than usual | 26 (11.8) | 64 (14.5) |
| Communication with family | ||
| Same as usual | 123 (55.7) | 201 (45.7) |
| Less than usual | 24 (10.9) | 90 (20.5) |
| More than usual | 74 (33.5) | 149 (33.9) |
| Communication with friends | ||
| Same as usual | 95 (43.0) | 97 (22.0) |
| Less than usual | 101 (45.7) | 302 (68.6) |
| More than usual | 25 (11.3) | 41 (9.3) |
| Measurements | Median (IQR) | Median (IQR) |
| Anxiety over COVID-19 | 8 (7–9) | 9 (8–10) |
| Health condition | 8 (7–9) | 6 (4–8) |
| Satisfaction with daily life | ||
| Satisfaction with leisure | 3 (2–5) | 2 (1–3) |
| Satisfaction with work | 7 (5–8) | 5 (3–7) |
| Satisfaction with daily life activities | 6 (4–8) | 4 (2–6) |
| Satisfaction with new activities | 7 (4–8) | 6 (2–7) |
| p Value | ||||
|---|---|---|---|---|
| Variables | No. with Mental Health Problems/Total No. (%) | Adjusted OR (95% CI) | Category | Overall |
| Characteristics | ||||
| Gender | ||||
| Men | 177/307 (57.8) | 1 (Reference) | NA | 0.002 |
| Women | 263/354 (74.3) | 1.83 (1.25–2.70) | 0.002 | |
| No. of household members | ||||
| 1 | 147/195 (75.4) | 1 (Reference) | NA | 0.007 |
| 2 | 92/145 (63.4) | 0.47 (0.27–0.80) | 0.006 | |
| ≥3 | 201/321 (62.6) | 0.52 (0.33–0.82) | 0.005 | |
| Communication with friends | ||||
| Same as usual | 97/192 (50.5) | 1 (Reference) | NA | <0.001 |
| Less than usual | 302/403 (74.9) | 2.29 (1.51–3.46) | <0.001 | |
| More than usual | 41/66 (62.1) | 1.29 (0.67–2.50) | 0.45 | |
| Measurements | ||||
| Anxiety over COVID-19 | - | 1.20 (1.08–1.34) | - | 0.001 |
| Health condition | - | 0.76 (0.69–0.83) | - | <0.001 |
| Satisfaction with work | - | 0.82 (0.75–0.90) | - | <0.001 |
| Satisfaction with new activities | - | 0.92(0.86–0.99) | - | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tahara, M.; Mashizume, Y.; Takahashi, K. Coping Mechanisms: Exploring Strategies Utilized by Japanese Healthcare Workers to Reduce Stress and Improve Mental Health during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 131. https://doi.org/10.3390/ijerph18010131
Tahara M, Mashizume Y, Takahashi K. Coping Mechanisms: Exploring Strategies Utilized by Japanese Healthcare Workers to Reduce Stress and Improve Mental Health during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(1):131. https://doi.org/10.3390/ijerph18010131
Chicago/Turabian StyleTahara, Masatoshi, Yuki Mashizume, and Kayoko Takahashi. 2021. "Coping Mechanisms: Exploring Strategies Utilized by Japanese Healthcare Workers to Reduce Stress and Improve Mental Health during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 1: 131. https://doi.org/10.3390/ijerph18010131
APA StyleTahara, M., Mashizume, Y., & Takahashi, K. (2021). Coping Mechanisms: Exploring Strategies Utilized by Japanese Healthcare Workers to Reduce Stress and Improve Mental Health during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(1), 131. https://doi.org/10.3390/ijerph18010131






