Emotional Experience and Feelings during First COVID-19 Outbreak Perceived by Physical Therapists: A Qualitative Study in Madrid, Spain
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Ethics
2.3. Research Team
2.4. Participants, Context, and Sampling Strategies
2.5. Data Collection
2.6. Data Analysis
2.7. Rigor
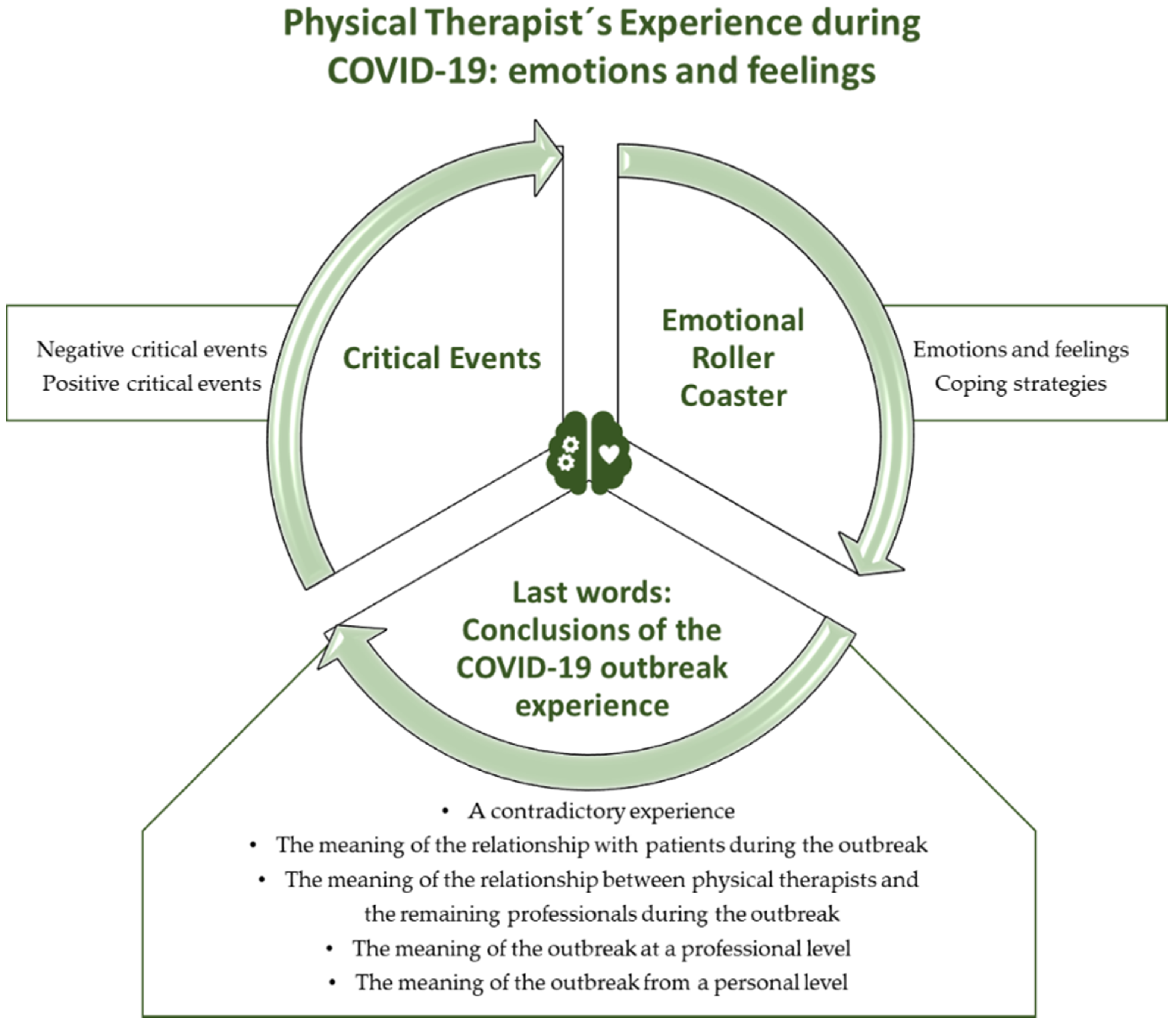
3. Results
3.1. Theme 1. Critical Events
3.1.1. Negative Critical Events
“.. the worst was not the fear of contagion, but the daily contact with the death.”(p3)
“For me it was a conflictive experience, you tried to be a professional and continue treating patients. But you knew that the next day they could have died.”(p12)
“The experience of the COVID-19 was brutal, without material, without space, people in the corridors, one person died, healthcare professional removed her/him and two minutes after another patient occupied the same bed.”(p16)
“The situation with a huge impact to me was is the human suffering. The numbers have not reflected the truth.”(p17)
“You faced the death each day, your patients were continually dying, you worked with the dead around you. You go to another room, and, more dead, patients lying covered with a sheet waiting to be taken to the mortuary.”(p23)
“When I entered to the library of the hospital, my breath stopped. The library was used to sedate patients who were going to die. I saw screens covering people who had died and were waiting to be picked up… I will never forget that picture.”(p27)
“I was really impressed when they said me that you had to “release the prone position” of a patient to release.” “This meant that the patient was going to die, and they released him from the prone position, placing him on his back, more comfortable, to die.”(p17)
“I will not forget the eyes of the patients. A look of disbelief, of not believing what is happening. The eyes of people being on the verge of death, and perceiving fear in their eyes, without being able to communicate because they cannot speak.”(p21)
3.1.2. Positive Critical Events
“For me it was incredible how everyone offered and helped. You felt that you were not alone.”(p24)
“Working in the hospital was working on the front-line of the war, you always felt overwhelmed, you go to work with fear, you cry and cry, but whatever happened, you were in the front-line against the virus.”(p5)
“The group of physical therapists, we worked together, in total synergy. We supported each other and tried to stay together against the adversity. The COVID-19 outbreak destroyed everything, your hope, your spirit.”(p14)
“It was incredible, the touch, the respect with which everyone tried to treat patients. They were extremely fragile; we didn’t want to harm them in any way.”(p5)
“Many times, at the end, you went to see or visit a patient. Typically, COVID-19 patients were alone. When I could, I tried to prolong my treatment to spend more time with them.”(p22)
“None hospital was ready for this. But if I’m honest, they adapted extremely fast, and, in two days, the entire hospital was transformed to deal with the COVID-19. I still don’t believe it.”(p19)
“I don’t know what other countries have done, but I have the feeling that here, no one was left behind. All patients were treated and received at the hospital. For me, it was an honor to be part of this.”(p16)
“Memories are like frames, images, not a sequence like a DVD movie, only images of what happened.”(p3)
3.2. Theme 2. Emotional Roller Coaster
3.2.1. Emotions and Feelings
“It was different. Entering an ICU was very scary, especially when you know that respirators may not be available for you.”(p20)
“You take fear home with you, even shopping, you have to force yourself.” (p8). “I do not remember having a particular moment that was mostly scared and marked me. The fear started with the first day of outbreak, it was like a constant horror movie. I’m still inside, I’m still inside, I’m still in “pandemic mode.” It is having constant fear.”(p29)
“You felt a lot of nerves and fear always. Other times you didn’t know if you were sick, it was just annoyances, or you had COVID -19. Others had moments of loneliness and suffering. A mess.”(p14)
“… It was living in a storm of feelings… positive and negative feelings, of all colors.”(p20)
3.2.2. Coping Strategies
“I prefer not to talk to anyone; people would not understand. You must have lived it. I don’t want to worry or scare my family.”(p27)
“When I was home in isolation, I received messages from all over the world. I felt very supported.”(p15)
“The first thing he did when he arrived to work was cry, he finished and was ready to work, another day.”(p20)
“You don’t think they are real and live people, with family, children, and a life. Otherwise, you could not continue working. Note that in a 7-h work schedule, up to 7 patients could die.. I suffered too much.”(p17)
“One day the father of a colleague was dying, and they called her to say him goodbye. At that moment I didn’t feel anything, I didn’t realize what I was experiencing. I realized after two days.. when I realized it, I burst into tears.”(p24)
“I want to focus on the journey I have made. I am not going to focus on specific things, I am not going to look back, I am only going to have a prospective vision.”(p3)
“I am not going to let the COVID-19 condition my whole life. The COVID-19 outbreak has been a moment in my life, nothing more. I have a lot of things to live.”(p23)
“My head went off, I got a psychosis from washing everything, disinfecting everything, I didn’t touch anything but I had gloves.”(p15)
“I know it was wrong to joke right now. But sometimes it was a relief, an evasion of all the human drama that was around the outbreak.”(p4)
3.3. Theme 3. Last Words: Conclusions of the Outbreak Experience
3.3.1. A Contradictory Experience
“I have conflicting feelings because people were suffering, but it was also a potential opportunity for physical therapy, as a science, to be able to advance and be able to help more people in the future.”(p7)
“The summary of the experience; enriching. On one hand it was a real tragedy, but on the other, it was enriching, because I was immersed in an interdisciplinary team with other professionals, working all together.”(p12)
“Everything was horrible, but at the same time I felt better than ever in my life, in my work. I feel 200%.”(p15)
“In conclusion, I have changed as a person. I’m not the same. Everything has changed. But not everything was bad. I have learned a lot as a professional and as a person.”(p9)
3.3.2. The Meaning of the Relationship with Patients during the Outbreak
“The most positive and precious thing during the outbreak were the video calls done with families. Everyone connected, you saw the relatives and the patient crying and laughing.. people felt grateful and they shared this emotion with you. They continually recognized your work.”(p28)
“The most brutal thing was loneliness… The loneliness of the patient, the loneliness of the healthcare professional looking impotent because we couldn’t save everyone … The fragility of people. Because of a bug that you cannot see, which is insignificant.”(p14)
3.3.3. The Meaning of the Relationship between Physical Therapists and the Remaining Professionals during the Outbreak
“There has been a change in all professionals, a great camaraderie, we all have the feeling of having won something together.”(p12)
“There were days when you couldn’t do anything more, it wasn’t just physical, it was more internal, like a loss of sense of everything.”(p23)
3.3.4. The Meaning of the Outbreak at a Professional Level
“This has been an opportunity to start from the beginning, doing things as well as you could. It’s a shame that a pandemic had to happen to do thing well.”(p17)
3.3.5. The Meaning of the Outbreak on a Personal Level
“In summary, 15% bad and 85% good, with a lot of personal and professional growth. I’m going to fight to do a good job, not a substitute .. I’m a better person than before.”(p10)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel coronavirus from patients with pneumonia in China. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Coronavirus Disease (COVID-19) out Break and Situation Reports. Available online: https://www.who.int (accessed on 1 November 2020).
- European Centre for Disease Prevention and Control (ECDC). Download Today’s Data on the Geographic Distribution of COVID-19 Cases Worldwide. 2020. Available online: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases (accessed on 25 November 2020).
- Xiao, X.; Zhu, X.; Fu, S.; Hu, Y.; Li, X.; Xiao, J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: A multi-center cross-sectional survey investigation. J. Affect. Disord. 2020, 274, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Lázaro-Pérez, C.; Martínez-López, J.Á.; Gómez-Galán, J.; López-Meneses, E. Anxiety about the risk of death of their patients in health professionals in Spain: Analysis at the peak of the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2020, 17, 5938. [Google Scholar] [CrossRef] [PubMed]
- de Sio, S.; Buomprisco, G.; la Torre, G.; Lapteva, E.; Perri, R.; Greco, E.; Mucci, N.; Cedrone, F. The impact of COVID-19 on doctors’ well-being: Results of a web survey during the lockdown in Italy. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 7869–7879. [Google Scholar] [PubMed]
- Radio y Televisión Española: Los Profesionales Sanitarios Contagiados de COVID-19 Superan los 76.000, 2.211 en la Última Semana. Available online: https://www.rtve.es/noticias/20201106/profesionales-sanitarios-contagiados-covid-19-superan-50000/2014047.shtml (accessed on 10 November 2020).
- Luceño-Moreno, L.; Talavera-Velasco, B.; García-Albuerne, Y.; Martín-García, J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5514. [Google Scholar] [CrossRef] [PubMed]
- Shreffler, J.; Petrey, J.; Huecker, M. The impact of COVID-19 on healthcare worker wellness: A scoping review. West J. Emerg. Med. 2020, 21, 1059–1066. [Google Scholar] [CrossRef]
- Shalev, D.; Shapiro, P.A. Epidemic psychiatry: The opportunities and challenges of COVID-19. Gen. Hosp. Psychiatry 2020, 64, 68–71. [Google Scholar] [CrossRef]
- Liu, Q.; Luo, D.; Haase, J.E.; Guo, Q.; Wang, X.Q.; Liu, S.; Xia, L.; Liu, Z.; Yang, J.; Yang, B.X. The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. Lancet Glob. Health 2020, 8, e790–e798. [Google Scholar] [CrossRef]
- Sun, N.; Wei, L.; Shi, S.; Jiao, D.; Song, R.; Ma, L.; Wang, H.; Wang, C.; Wang, Z.; You, Y.; et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control 2020, 48, 592–598. [Google Scholar] [CrossRef]
- Galehdar, N.; Kamran, A.; Toulabi, T.; Heydari, H. Exploring nurses’ experiences of psychological distress during care of patients with COVID-19: A qualitative study. BMC Psychiatry 2020, 20, 489. [Google Scholar] [CrossRef]
- Ardebili, D.M.E.; Naserbakht, D.M.; Colleen, D.B.; Alazmani-Noodeh, M.F.; Hakimi, M.H.; Ranjbar, D.H. Healthcare providers experience of working during the COVID-19 pandemic: A qualitative study. Am. J. Infect. Control 2020. [Google Scholar] [CrossRef]
- Xiong, Y.; Peng, L. Focusing on health-care providers’ experiences in the COVID-19 crisis. Lancet Glob. Health 2020, 8, e740–e741. [Google Scholar] [CrossRef]
- Korstjens, I.; Moser, A. Series: Practical guidance to qualitative research. Part 2: Context, research questions and designs. Eur. J. Gen. Pract. 2017, 23, 274–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [Green Version]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for reporting qualitative research: A synthesis of recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef]
- Carpenter, C.; Suto, M. Qualitative Research for Occupational and Physical Therapist; Blackwell Publishing: Oxford, UK, 2008. [Google Scholar]
- Moser, A.; Korstjens, I. Series: Practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. Eur. J. Gen. Pract. 2018, 24, 9–18. [Google Scholar] [CrossRef] [Green Version]
- Turner-Bowker, D.M.; Lamoureux, R.E.; Stokes, J.; Litcher-Kelly, L.; Galipeau, N.; Yaworsky, A.; Solomon, J.; Shields, A.L. Informing a priori Sample Size Estimation in Qualitative Concept Elicitation Interview Studies for Clinical Outcome Assessment Instrument Development. Value Health 2018, 21, 839–842. [Google Scholar] [CrossRef] [Green Version]
- Gobierno de España. Real Decreto 463/2020, de 14 de Marzo, por el que se Declara el Estado de Alarma para la Gestión de la Situación de Crisis Sanitaria Ocasionada por el COVID-19. Available online: https://www.boe.es/diario_boe/txt.php?id=BOE-A-2020-3692 (accessed on 10 November 2020).
- Archibald, M.M.; Ambagtsheer, R.C.; Casey, M.G.; Lawless, M. Using zoom videoconferencing for qualitative data collection: Perceptions and experiences of researchers and participants. Int. J. Qual. Methods 2019, 18, 1609406919874596. [Google Scholar] [CrossRef] [Green Version]
- Creswell, J.W.; Poth, C.N. Qualitative Inquiry and Research Design: Choosing among Five Approaches, 4th ed.; Sage: Thousand Oaks, CA, USA, 2018. [Google Scholar]
- Miles, M.; Huberman, A.; Saldaña, J. Qualitative Data Analysis: A Method Sourcebook, 3rd ed.; Sage: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Korstjens, I.; Moser, A. Series: Practical guidance to qualitative research. Part 4: Trustworthiness and publishing. Eur. J. Gen. Pract. 2018, 24, 120–124. [Google Scholar] [CrossRef] [Green Version]
- Giusti, E.M.; Pedroli, E.; D’Aniello, G.E.; Badiale, C.S.; Pietrabiss, A.G.; Manna, C.; Badiale, M.S.; Riva, G.; Castelnuovo, G.; Molinari, E. The psychological impact of the covid-19 outbreak on health professionals: A cross-sectional study. Front. Psychol. 2020, 11, 1684. [Google Scholar] [CrossRef]
- Barello, S.; Falcó-Pegueroles, A.; Rosa, D.; Tolotti, A.; Graffigna, G.; Bonetti, L. The psychosocial impact of flu influenza pandemics on healthcare workers and lessons learnt for the COVID-19 emergency: A rapid review. Int. J. Public Health 2020, 65, 1205–1216. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Yang, L.; Zhang, C.; Xiang, Y.T.; Liu, Z.; Hu, S.; Zhang, B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e17–e18. [Google Scholar] [CrossRef]
- Negrini, S.; Ferriero, G.; Kiekens, C.; Boldrini, P. Facing in real time the challenges of the Covid-19 epidemic for rehabilitation. Eur. J. Phys. Rehabil. Med. 2020, 56, 313–315. [Google Scholar] [CrossRef] [PubMed]
- Fauzi, M.F.M.; Yusoff, H.M.; Robat, R.M.; Saruan, N.A.M.; Ismail, K.I.; Haris, A.F.M. Doctors’ mental health in the midst of COVID-19 pandemic: The roles of work demands and recovery experiences. Int. J. Environ. Res. Public Health 2020, 17, 7340. [Google Scholar] [CrossRef]
- Zhang, Y.; Xie, S.; Wang, P.; Wang, G.; Zhang, L.; Cao, X.; Wu, W.; Bian, Y.; Huang, F.; Luo, N.; et al. Factors influencing mental health of medical workers during the COVID-19 outbreak. Front. Public Health 2020, 8, 491. [Google Scholar] [CrossRef]
- Martínez-López, J.Á.; Lázaro-Pérez, C.; Gómez-Galán, J.; Fernández-Martínez, M.D.M. Psychological impact of COVID-19 emergency on health professionals: Burnout incidence at the most critical period in Spain. J. Clin. Med. 2020, 9, 3029. [Google Scholar] [CrossRef]
- Iglesias-Sánchez, P.P.; Witt, G.F.V.; Cabrera, F.E.; Jambrino-Maldonado, C. The contagion of sentiments during the COVID-19 pandemic crisis: The case of isolation in Spain. Int. J. Environ. Res. Public Health 2020, 17, 5918. [Google Scholar] [CrossRef]
- Zhang, M.M.; Niu, N.; Zhi, X.X.; Zhu, P.; Wu, B.; Wu, B.N.; Meng, A.F.; Zhao, Y. Nurses’ psychological changes and coping strategies during home isolation for the 2019 novel coronavirus in China: A qualitative study. J. Adv. Nurs. 2020, 77, 308–317. [Google Scholar] [CrossRef]
- Paiano, M.; Jaques, A.E.; Nacamura, P.A.B.; Salci, M.A.; Radovanovic, C.A.T.; Carreira, L. Mental health of healthcare professionals in China during the new coronavirus pandemic: An integrative review. Rev. Bras. Enferm. 2020, 73, e20200338. [Google Scholar] [CrossRef]
- Schroeder, K.; Norful, A.A.; Travers, J.; Aliyu, S. Nursing perspectives on care delivery during the early stages of the covid-19 pandemic: A qualitative study. Int. J. Nurs. Stud. Adv. 2020, 2, 100006. [Google Scholar] [CrossRef]
- Alizadeh, A.; Khankeh, H.R.; Barati, M.; Ahmadi, Y.; Hadian, A.; Azizi, M. Psychological distress among Iranian health-care providers exposed to coronavirus disease 2019 (COVID-19): A qualitative study. BMC Psychiatry 2020, 20, 494. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, F.B.; Misol, R.C.; Alonso, M.D.C.F.; Tizón, J.L. COVID-19 pandemic and mental health: Initial considerations from Spanish primary health care. Aten. Primaria 2020, 53, 89–101. [Google Scholar]
- Heath, C.; Sommerfield, A.; von Ungern-Sternberg, B.S. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: A narrative review. Anaesthesia 2020, 75, 1364–1371. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.C.C.; Thampi, S.; Chan, H.P.; Khoo, D.; Chin, B.Z.B.; Foo, D.P.X.; Lua, C.B.; Lewin, B.; Jacob, R. Psychological distress during the COVID-19 pandemic amongst anaesthesiologists and nurses. Br. J. Anaesth. 2020, 125, e384–e386. [Google Scholar] [CrossRef] [PubMed]
|
| Criteria | Techniques Performed and Application Procedures |
|---|---|
| Credibility | Investigator triangulation: each interview was analyzed by two researchers. Thereafter, team meetings were performed in which the analyses were compared and categories and themes were identified. Participant triangulation: the study included participants belonging to different hospitals. Thus, multiple perspectives were obtained with a common link (the emotional experiences and feeling of physical therapists during the first COVID-19 outbreak). Triangulation of methods of data collection: semistructured interviews were conducted and researcher field notes were kept. Participant validation: this consisted of asking the participants to confirm the data obtained at the stages of data collection. All participants were offered the opportunity to review the audio and/or video records to confirm their experience. None of the participants made additional comments. |
| Transferability | In-depth descriptions of the study performed, providing details of the characteristics of researchers, participants, contexts, sampling strategies, and the data collection and analysis procedures. |
| Dependability | Audit by an external researcher: an external researcher assessed the research protocol, focusing on aspects concerning the methods applied and study design. Additionally, an external researcher specifically checked the description of the coding tree, the major themes, participants’ quotations, quotations’ identification, and themes’ descriptions |
| Confirmability | Investigator triangulation, participant triangulation, and data collection triangulation. Researcher reflexivity was encouraged via the performance of reflexive reports and by describing the rationale behind the study. |
| Themes | Categories |
|---|---|
| Critical events | Negative critical events Positive critical events |
| Emotional Roller Coaster | Emotions and feelings Coping strategies |
| Last words: Conclusions of the COVID-19 outbreak experience | A contradictory experience The meaning of the relationship with patients during the outbreak The meaning of the relationship between physical therapists and the remaining professionals during the outbreak The meaning of the outbreak at a professional level The meaning of the outbreak from a personal level |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palacios-Ceña, D.; Fernández-de-las-Peñas, C.; Florencio, L.L.; de-la-Llave-Rincón, A.I.; Palacios-Ceña, M. Emotional Experience and Feelings during First COVID-19 Outbreak Perceived by Physical Therapists: A Qualitative Study in Madrid, Spain. Int. J. Environ. Res. Public Health 2021, 18, 127. https://doi.org/10.3390/ijerph18010127
Palacios-Ceña D, Fernández-de-las-Peñas C, Florencio LL, de-la-Llave-Rincón AI, Palacios-Ceña M. Emotional Experience and Feelings during First COVID-19 Outbreak Perceived by Physical Therapists: A Qualitative Study in Madrid, Spain. International Journal of Environmental Research and Public Health. 2021; 18(1):127. https://doi.org/10.3390/ijerph18010127
Chicago/Turabian StylePalacios-Ceña, Domingo, César Fernández-de-las-Peñas, Lidiane L. Florencio, Ana I. de-la-Llave-Rincón, and María Palacios-Ceña. 2021. "Emotional Experience and Feelings during First COVID-19 Outbreak Perceived by Physical Therapists: A Qualitative Study in Madrid, Spain" International Journal of Environmental Research and Public Health 18, no. 1: 127. https://doi.org/10.3390/ijerph18010127
APA StylePalacios-Ceña, D., Fernández-de-las-Peñas, C., Florencio, L. L., de-la-Llave-Rincón, A. I., & Palacios-Ceña, M. (2021). Emotional Experience and Feelings during First COVID-19 Outbreak Perceived by Physical Therapists: A Qualitative Study in Madrid, Spain. International Journal of Environmental Research and Public Health, 18(1), 127. https://doi.org/10.3390/ijerph18010127







