A Pilot Study of Airborne Hazards and Other Toxic Exposures in Iraq War Veterans
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Materials and Procedure
2.3. Measures and Covariates
2.4. Statistical Analysis
3. Results
3.1. Demographics
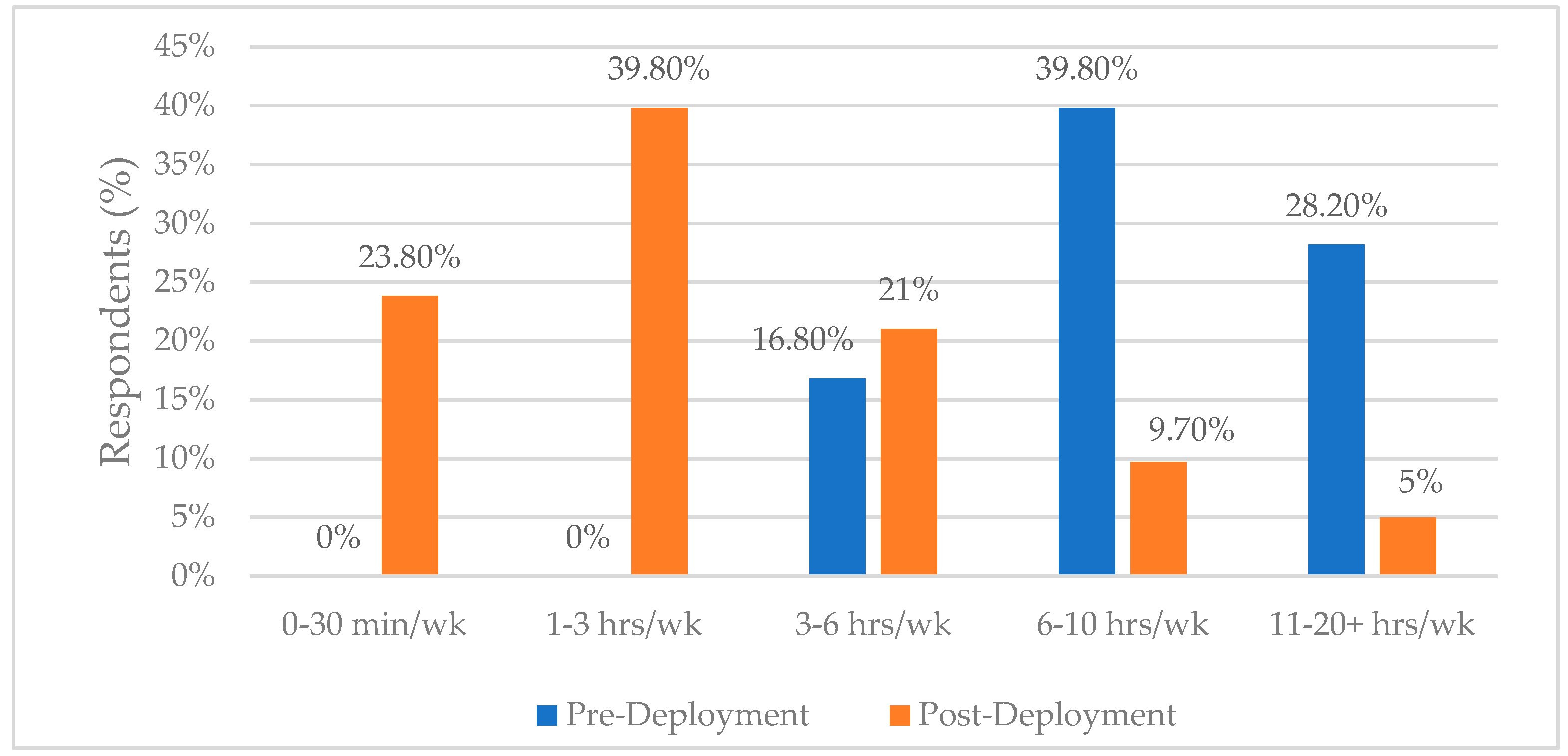
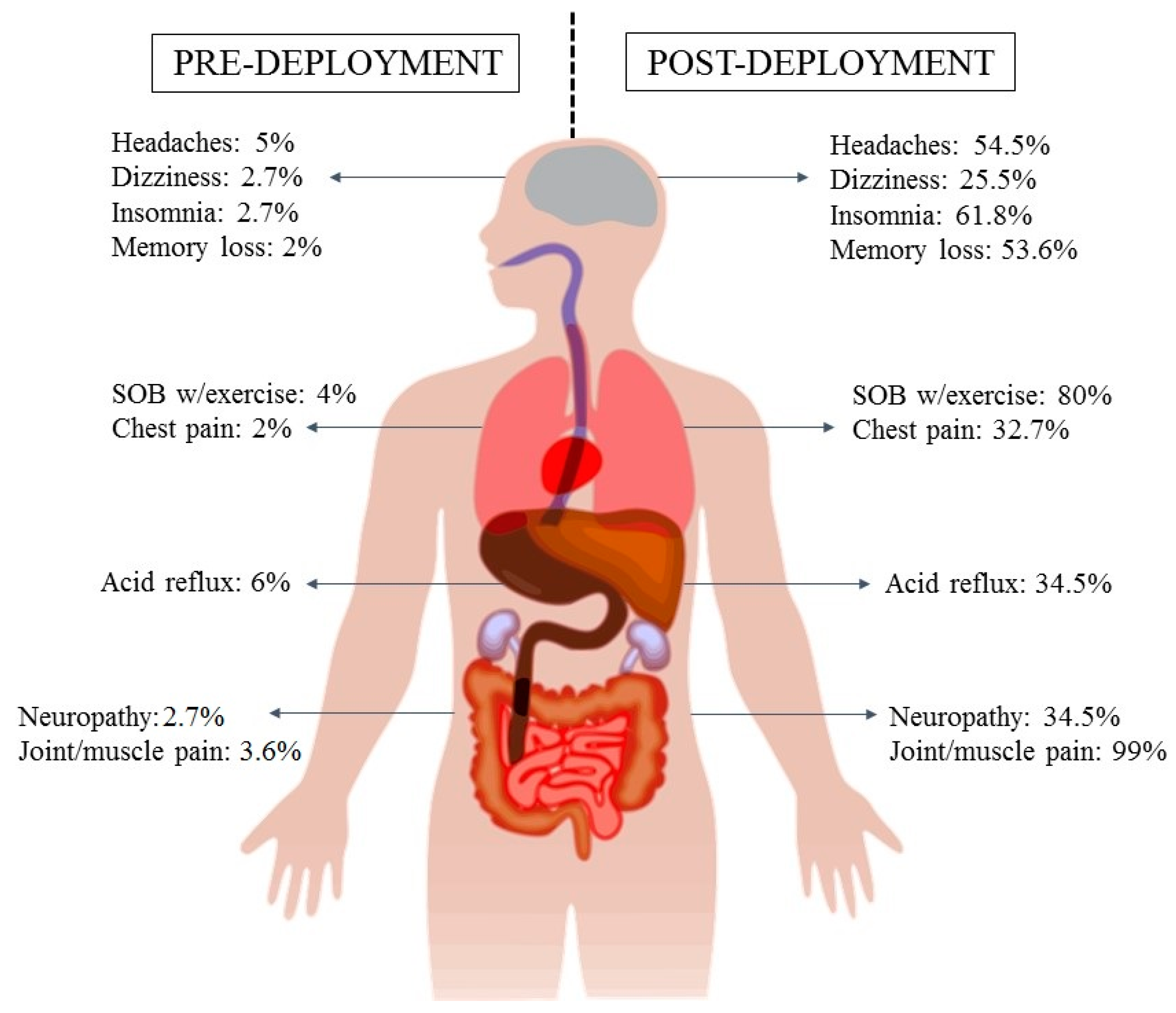
3.2. Symptoms and Deployment(s)
4. Discussion
4.1. Overview
4.2. Existing Literature on Long-Term and Persistent Effects of Exposure
4.3. Unique Aspects of the Iraq War
4.4. Unknown Threats to Health and Perceived Barriers to Care
4.5. Nursing Implications
4.6. The Health Belief Model
4.7. Limitations
4.8. Future Research
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Disclaimer
Appendix A
| Demographic | Response | Respondents (%) | National Data (%) * |
|---|---|---|---|
| Age | 25–34 years | 42 | 49 |
| 35–44 years | 41 | 23 | |
| Gender | Male | 84 | 88 |
| Female | 16 | 12 | |
| Blood Type | A+ | 37 | 34 |
| O+ | 36 | 38 | |
| Allergies | Yes | 41 | 40 |
| No | 59 | 60 | |
| Branch of Service | Army | 84 | 54 |
| Navy | 5 | 17 | |
| Marine Corps | 7 | 14 | |
| Air Force | 6 | 15 | |
| Currently Serving | Yes | 29 | n/a |
| No | 71 | ||
| Avg. time in Service | 6–8 years | 21 | n/a |
| 14–16 years | 17 | ||
| 20+ years | 18 | ||
| Avg. Rank | E-5 | 27 | Enlisted: 85 |
| E-6 | 24 | ||
| E-4 | 19 | ||
| Avg. MOS ** | Infantry | 21 | n/a |
| Mechanic | 15 | ||
| Mil. Police | 9 | ||
| Field Artillery | 8 | ||
| Transportation | 8 | ||
| MOB Station *** | Rose Barracks, GE | 13 | n/a |
| Camp Shelby, MS | 9 | ||
| Fort Dix, NJ | 8 | ||
| Ft. Lewis, WA | 6 | ||
| Ft. Bragg, NC | 6 | ||
| Immunization(s) | Anthrax | 90 | n/a |
| Small Pox | 89 | ||
| H1N1 Influenza | 66 | ||
| Anti-Malaria | 56 | ||
| Number of Deployments | 1-deployment | 44 | 57 |
| 2-deployment | 24 | 27 | |
| 3-deployment | 21 | 10 | |
| Smoking/Nicotine Use | Current Smoker | 22 | n/a |
| Smoked during Deployment | 42 | ||
| Non-Smoker/Never | 36 | ||
| Exercise Stress-Test Post-Deployment | No | 55 | n/a |
| Yes | 34 | ||
| Unknown | 11 | ||
| Sleep Apnea Study Test | No | 64 | n/a |
| Yes | 34 | ||
| Unknown | 0 |
Appendix B
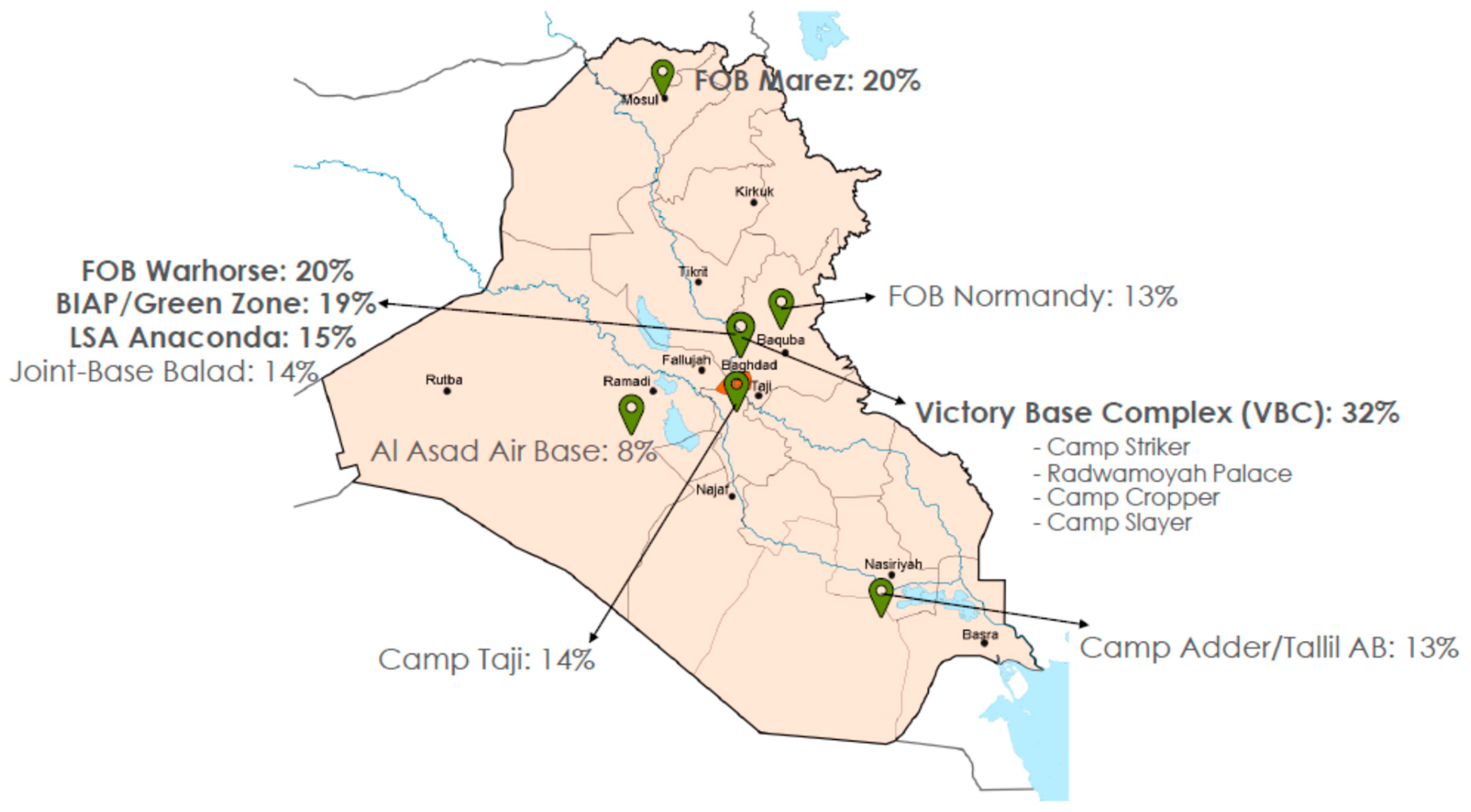
| Base Name | Location | Respondents (%) |
|---|---|---|
| Victory Base Complex | Baghdad, Iraq | 32 |
| FOB Warhorse | Baqubah, Iraq | 20 |
| FOB Marez | Mosul, Iraq | 20 |
| BIAP/Green Zone | Baghdad, Iraq | 16 |
| LSA Anaconda | Baghdad, Iraq | 15 |
| Joint-Base Balad | Balad, Iraq | 14 |
| Camp Taji | Taji, Iraq | 14 |
| FOB Normandy | Baqubah, Iraq | 13 |
| Camp Adder/Tallil AB | Tallil, Iraq | 13 |
| Al Asad AB | Al Asad, Iraq | 8 |
| Camp Fallujah | Fallujah, Iraq | 8 |
| Camp Falcon | Baghdad, Iraq | 7 |
| Camp Speicher | Tikrit, Iraq | 6 |
| FOB Q-West | Qayyarah, Iraq | 3 |
References
- Costs of War: Watson Institute for International and Public Affairs. Brown University: Providence, RI, USA, 2015. [updated January 2015]. Available online: https://watson.brown.edu/costsofwar/costs/human/veterans (accessed on 1 March 2020).
- Miller, R. Respiratory Disorders Following Service in Iraq. Costs of War—Watson Institute of International and Public Affairs. 2013. Available online: https://watson.brown.edu/costsofwar/papers/2013/respiratory-disorders-following-service-iraq (accessed on 1 March 2020).
- Zundel, C.G.; Krengel, M.H.; Heeren, T.; Yee, M.K.; Grasso, C.M.; Janulewicz Lloyd, P.A.; Coughlin, S.S.; Sullivan, K. Rates of chronic medical conditions in 1991 Gulf War Veterans compared to the general population. Int. J. Environ. Res. Public Health 2019, 16, 949. [Google Scholar] [CrossRef] [PubMed]
- White, R.F.; Steele, L.; O’Callaghan, J.P.; Sullivan, K.; Binns, J.H.; Golomb, B.A.; Bloom, F.E.; Bunker, J.A.; Crawford, F.; Graves, J.C.; et al. Recent research on Gulf War illness and other health problems in Veterans of the 1991 Gulf War: Effects of toxicant exposures during deployment. Cortex 2016, 74, 449–475. [Google Scholar] [CrossRef] [PubMed]
- Proctor, S.P.; Heeren, T.; White, R.F.; Wolfe, J.; Borgos, M.S.; Davis, J.D.; Pepper, L.; Clapp, R.; Sutker, P.B.; Vasterling, J.J.; et al. Health status of Persian Gulf War Veterans: Self-reported symptoms, environmental exposures and the effect of stress. Int. J. Epidemiol. 1998, 27, 1000–1010. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Lezama, N.; Gasper, J.; Kawata, J.; Morley, S.; Helmer, D.; Ciminera, P. Burn pit emissions exposure and respiratory and cardiovascular conditions among Airborne Hazards and Open Burn Pit Registry participants. J. Occup. Environ. Med. 2016, 58, e249–e255. [Google Scholar] [CrossRef] [PubMed]
- Teichman, R. Exposures of concern to veterans returning from Afghanistan and Iraq. J. Occup. Environ. Med. 2012, 54, 677–681. [Google Scholar] [CrossRef]
- Lim, P.; Tayyeb, A. Critical analysis of the healthcare response to burn-pit-related illnesses for post-9/11 Iraq and Afghanistan Veterans. Open J. Emerg. Med. 2019, 7, 17–27. [Google Scholar] [CrossRef]
- National Academies of Sciences. Engineering, and Medicine 11: Generational Health Effects of Serving in the Gulf War; National Academies Press: Washington, DC, USA, 2018. [Google Scholar]
- Curtis, D.L.; Elliott, J.R. Burn Pit Health Hazards. [Memorandum for 332 EAMDS/SGP]; Department of the Air Force, 332D Air Expeditionary Wing: Balad Air Base, Iraq, 2006. [Google Scholar]
- Ritchie, G.; Still, K.; Rossi, J., 3rd; Bekkedal, M.; Bobb, A.; Arfsten, D. Biological and health effects of exposure to kerosene-based jet fuels and performance additives. J. Toxicol. Environ. Health B Crit. Rev. 2003, 6, 357–451. [Google Scholar] [CrossRef]
- Guthrie, O.W.; Xu, H.; Wong, B.A.; McInturf, S.M.; Reboulet, J.E.; Ortiz, P.A.; Mattie, D.R. Exposure to low levels of jet-propulsion fuel impairs brainstem encoding of stimulus intensity. J. Toxicol. Environ. Health A 2014, 77, 261–280. [Google Scholar] [CrossRef]
- VA’s Airborne Hazards and Open Burn Pit Registry: U.S. Department of Veterans Affairs. Available online: https://www.publichealth.va.gov/exposures/burnpits/registry.asp (accessed on 1 March 2020).
- Franklin, K.A.; Lindberg, E. Obstructive sleep apnea is a common disorder in the population—A review on the epidemiology of sleep apnea. J. Thorac. Dis. 2015, 7, 1311–1322. [Google Scholar] [CrossRef]
- Dempsey, T.M.; Scanlon, P.D. Pulmonary function tests for the generalist: A brief review. Mayo Clin. Proc. 2018, 93, 763–771. [Google Scholar] [CrossRef]
- Armed Forces Health Surveillance Center. Background Information on Deployments to OEF/OIF; Armed Forces Health Surveillance Center: Silver Springs, MD, USA, 2009. [Google Scholar]
- Amaral, E.F.L.; Pollard, M.; Mendelsohn, J.; Cefalu, M. Current and future demographics of the Veteran population, 2014–2024. Popul. Rev. 2018, 57, 28–60. [Google Scholar] [CrossRef]
- Wong, S.S.; Sun, N.N.; Miller, H.B.; Witten, M.L.; Burgess, J.L. Acute changes in sputum collected from exposed human subjects in mining conditions. Inhal. Toxicol. 2010, 22, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Committee on the Development of a Consensus Case Definition for Chronic Multisymptom Illness in 1990–1991 Gulf War Veterans; Board on the Health of Select Populations; Institute of Medicine. Chronic Multisymptom Illness in Gulf War Veterans: Case Definitions Reexamined. 2, Case Definitions; National Academies Press: Washington, DC, USA, 2014. Available online: https://www.ncbi.nlm.nih.gov/books/NBK268884/ (accessed on 1 March 2020).
- Chen, Y.; Meyer, J.N.; Hill, H.Z.; Lange, G.; Condon, M.R.; Klein, J.C.; Ndirangu, D.; Falvo, M.J. Role of mitochondrial DNA damage and dysfunction in Veterans with Gulf War illness. PLoS ONE 2017, 12, e0184832. [Google Scholar] [CrossRef]
- Koslik, H.J.; Hamilton, G.; Golomb, B.A. Mitochondrial dysfunction in Gulf War illness revealed by 31phosphorus magnetic resonance spectroscopy: A case-control study. PLoS ONE 2014, 9, e92887. [Google Scholar] [CrossRef]
- Golomb, B. Oxidative stress and mitochondrial injury in chronic multisymptom conditions: From Gulf War illness to autism spectrum disorder. Nat. Preced. 2012, 7. [Google Scholar] [CrossRef]
- Golomb, B.A.; Allison, M.; Koperski, S.; Koslik, H.J.; Devaraj, S.; Ritchie, J.B. Coenzyme Q10 benefits symptoms in Gulf War Veterans: Results of a randomized double-blind study. Neural Comput. 2014, 26, 2594–2651. [Google Scholar] [CrossRef]
- Latimer, J.J.; Alhamed, A.; Sveiven, S.; Almutairy, A.; Klimas, N.G.; Abreu, M.; Sullivan, K.; Grant, S.G. Preliminary evidence for a hormetic effect on DNA nucleotide excision repair in Veterans with Gulf War illness. Mil. Med. 2020, 185, e47–e52. [Google Scholar] [CrossRef]
- Janulewicz, P.A.; Seth, R.K.; Carlson, J.M.; Ajama, J.; Quinn, E.; Heeren, T.; Klimas, N.; Lasley, S.M.; Horner, R.D.; Sullivan, K.; et al. The gut-microbiome in Gulf War Veterans: A preliminary report. Int. J. Environ. Res. Public Health 2019, 16, 3751. [Google Scholar] [CrossRef]
- Seth, R.K.; Maqsood, R.; Mondal, A.; Bose, D.; Kimono, D.; Holland, L.A.; Janulewicz Lloyd, P.; Klimas, N.; Horner, R.D.; Sullivan, K.; et al. Gut DNA virome diversity and its association with host bacteria regulate inflammatory phenotype and neuronal immunotoxicity in experimental Gulf War illness. Viruses 2019, 11, 968. [Google Scholar] [CrossRef]
- McAndrew, L.M.; Helmer, D.A.; Phillips, L.A.; Chandler, H.K.; Ray, K.; Quigley, K.S. Iraq and Afghanistan Veterans report symptoms consistent with chronic multisymptom illness one year after deployment. J. Rehabil. Res. Dev. 2016, 53, 59–70. [Google Scholar] [CrossRef]
- DeBeer, B.B.; Davidson, D.; Meyer, E.C.; Kimbrel, N.A.; Gulliver, S.B.; Morissette, S.B. The association between toxic exposures and chronic multisymptom illness in Veterans of the Wars of Iraq and Afghanistan. J. Occup. Environ. Med. 2017, 59, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Falvo, M.J.; Osinubi, O.Y.; Sotolongo, A.M.; Helmer, D.A. Airborne hazards exposure and respiratory health of Iraq and Afghanistan Veterans. Epidemiol. Rev. 2015, 37, 116–130. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.C.; Powell, T.M.; Jacobson, I.G.; Smith, B.; Hooper, T.I.; Boyko, E.J.; Gackstetter, G.D. Chronic multisymptom illness: A comparison of Iraq and Afghanistan deployers with Veterans of the 1991 Gulf War. Am. J. Epidemiol. 2014, 180, 1176–1187. [Google Scholar] [CrossRef] [PubMed]
- Clauw, D.J. Potential mechanisms in chemical intolerance and related conditions. Ann. N. Y. Acad. Sci. 2001, 933, 235–253. [Google Scholar] [CrossRef] [PubMed]
- Katoh, T. Multiple chemical sensitivity (MCS): History, epidemiology and mechanism. Nihon Eiseigaku Zasshi 2018, 73, 1–8. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mawson, A.R.; Croft, A.M. Gulf War illness: Unifying hypothesis for a continuing health problem. Int. J. Environ. Res. Public Health 2019, 16, 111. [Google Scholar] [CrossRef] [PubMed]
- Proctor, S.P.; Heaton, K.J.; White, R.F.; Wolfe, J. Chemical sensitivity and chronic fatigue in Gulf War Veterans: A brief report. J. Occup. Environ. Med. 2001, 43, 259–264. [Google Scholar] [CrossRef]
- Kerr, K.J. Gulf War illness: An overview of events, most prevalent health outcomes, exposures, and clues as to pathogenesis. Rev. Environ. Health 2015, 30, 273–286. [Google Scholar] [CrossRef]
- Thomas, H.V.; Stimpson, N.J.; Weightman, A.L.; Dunstan, F.; Lewis, G. Systematic review of multi-symptom conditions in Gulf War Veterans. Psychol. Med. 2006, 36, 735–747. [Google Scholar] [CrossRef]
- Locker, A.R.; Michalovicz, L.T.; Kelly, K.A.; Miller, J.V.; Miller, D.B.; O’Callaghan, J.P. Corticosterone primes the neuroinflammatory response to Gulf War illness-relevant organophosphates independently of acetylcholinesterase inhibition. J. Neurochem. 2017, 142, 444–455. [Google Scholar] [CrossRef]
- Savitz, D.; Styka, A.; Butler, D. Assessment of the Department of Veterans Affairs Airborne Hazards and Open Burn Pit Registry; The National Academies Press: Washington, DC, USA, 2017. [Google Scholar]
- White, M. Casualties in the Afghanistan War and Iraq War. 2020. Available online: http://icasualties.org/ (accessed on 1 March 2020).
- Watts, J.; Nimer, S. Recent advances in the understanding and treatment of acute myeloid leukemia. F1000Research 2018, 7. [Google Scholar] [CrossRef] [PubMed]
- Beehler, G.P.; Rodrigues, A.E.; Kay, M.A.; Kiviniemi, M.T.; Steinbrenner, L. Perceptions of barriers and facilitators to health behavior change among veteran cancer survivors. Mil. Med. 2014, 179, 998–1005. [Google Scholar] [CrossRef] [PubMed]
- Glanz, K.; Rimer, B.; Viswanath, K. Health Behavior: Theory, Research, and Practice, 5th ed.; Jossey-Bass Publishers: San Francisco, CA, USA, 2015. [Google Scholar]
- Powell, T.M.; Smith, T.C.; Jacobson, I.G.; Boyko, E.J.; Hooper, T.I.; Gackstetter, G.D.; Phillips, C.J.; Smith, B. Prospective assessment of chronic multisymptom illness reporting possibly associated with open-air burn pit smoke exposure in Iraq. J. Occup. Environ. Med. 2012, 54, 682–688. [Google Scholar] [CrossRef] [PubMed]

| Age (mean) | 37 years |
| Gender (Male) | 82% |
| Still Serving | 30% |
| New-onset Allergies | 41% |
| Polysomnogram | 35% |
| Pulmonary Function Test | 34% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poisson, C.; Boucher, S.; Selby, D.; Ross, S.P.; Jindal, C.; Efird, J.T.; Bith-Melander, P. A Pilot Study of Airborne Hazards and Other Toxic Exposures in Iraq War Veterans. Int. J. Environ. Res. Public Health 2020, 17, 3299. https://doi.org/10.3390/ijerph17093299
Poisson C, Boucher S, Selby D, Ross SP, Jindal C, Efird JT, Bith-Melander P. A Pilot Study of Airborne Hazards and Other Toxic Exposures in Iraq War Veterans. International Journal of Environmental Research and Public Health. 2020; 17(9):3299. https://doi.org/10.3390/ijerph17093299
Chicago/Turabian StylePoisson, Chelsey, Sheri Boucher, Domenique Selby, Sylvia P. Ross, Charulata Jindal, Jimmy T. Efird, and Pollie Bith-Melander. 2020. "A Pilot Study of Airborne Hazards and Other Toxic Exposures in Iraq War Veterans" International Journal of Environmental Research and Public Health 17, no. 9: 3299. https://doi.org/10.3390/ijerph17093299
APA StylePoisson, C., Boucher, S., Selby, D., Ross, S. P., Jindal, C., Efird, J. T., & Bith-Melander, P. (2020). A Pilot Study of Airborne Hazards and Other Toxic Exposures in Iraq War Veterans. International Journal of Environmental Research and Public Health, 17(9), 3299. https://doi.org/10.3390/ijerph17093299






