Public Pension, Labor Force Participation, and Depressive Symptoms across Gender among Older Adults in Rural China: A Moderated Mediation Analysis
Abstract
1. Introduction
1.1. Public Pension and Depression
1.2. Public Pension, LFP, and Depression
1.3. Consideration of Gender
1.4. Current Study
2. Materials and Methods
2.1. Data Source and Study Population
2.2. Measurements
2.2.1. Depressive Symptoms
2.2.2. Labor Force Participation (LFP)
2.2.3. Pension Income
2.2.4. Covariates
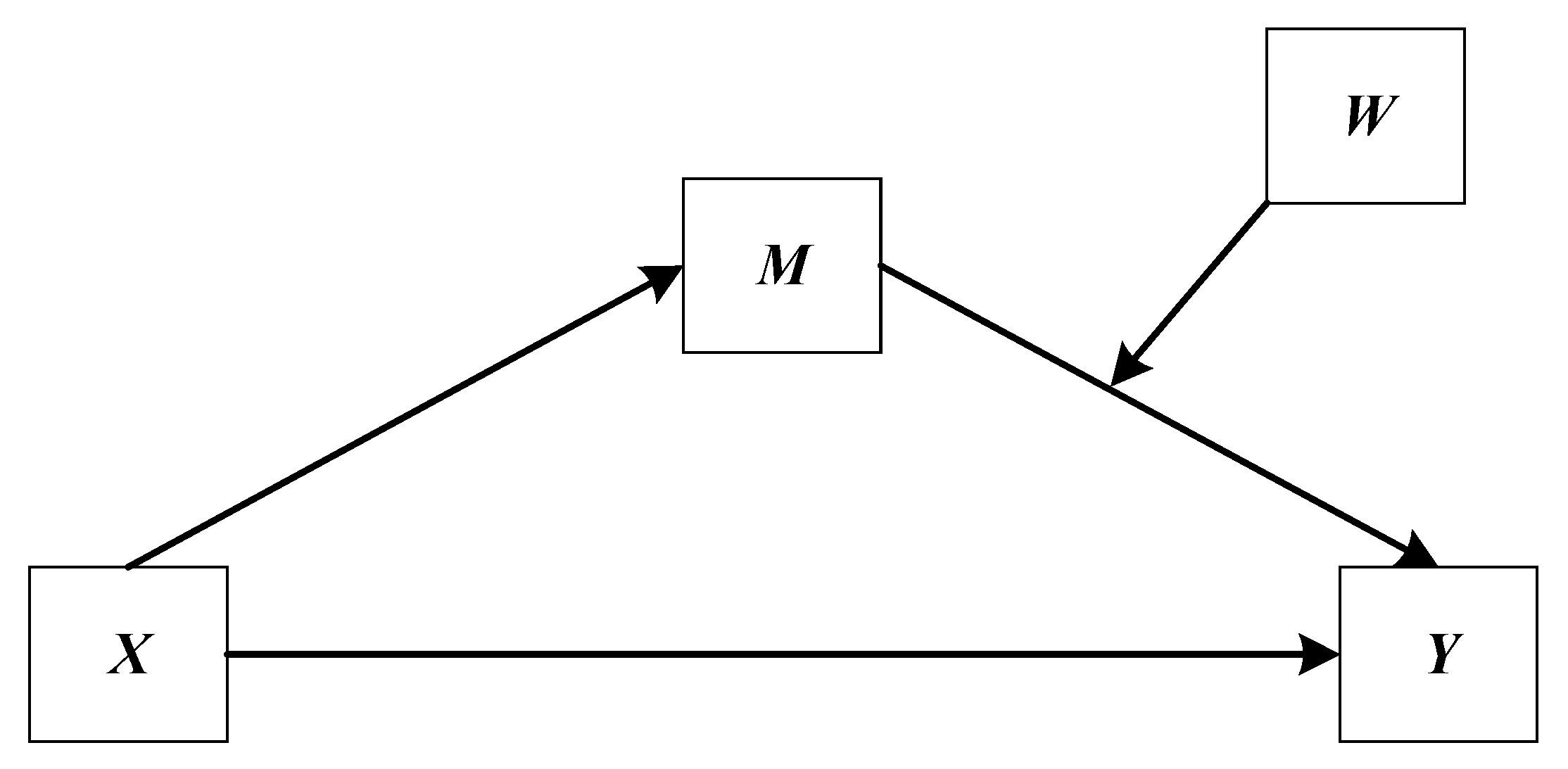
2.3. Analytical Strategy
3. Results
3.1. Preliminary Analysis
3.2. The Results of Mediation Estimates
3.3. The Results of Moderated Mediation Estimates
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wu, Z.; Schimmele, C.M.; Chappell, N.L. Aging and late-life depression. J. Aging Health 2012, 24, 3–28. [Google Scholar] [CrossRef] [PubMed]
- Willis, K.D.; Nelson, T.; Moreno, O. Death anxiety, religious doubt, and depressive symptoms across race in older adults. Int. J. Environ. Res. Public Health 2019, 16, 3645. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Ying, M.; Xie, L.; Chandrasekar, E.K.; Lu, H.; Wang, T.; Li, C. Late-life depression and cognitive function among older adults in the USA: The national health and nutrition examination survey, 2011–2014. J. Psychiatr. Res. 2019, 111, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Bhar, S.S.; Brown, G.K. Treatment of depression and suicide in older adults. Cogn. Behav. Pract. 2012, 19, 116–125. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health of Older Adults. Available online: https://www.who.int/en/news-room/fact-sheets/detail/mental-health-of-older-adults (accessed on 20 December 2019).
- World Health Organization. Depression. Available online: https://www.who.int/health-topics/depression#tab=tab_1 (accessed on 20 December 2019).
- Yu, J.; Li, J.; Cuijpers, P.; Wu, S.; Wu, Z. Prevalence and correlates of depressive symptoms in Chinese older adults: A population based study. Int. J. Geriatr. Psychiatry 2012, 27, 305–312. [Google Scholar] [CrossRef]
- Guo, Q.; Bai, X.; Feng, N. Social participation and depressive symptoms among Chinese older adults: A study on rural–urban differences. J. Affect. Disord. 2018, 239, 124–130. [Google Scholar] [CrossRef]
- Guo, J.; Guan, L.; Fang, L.; Liu, C.; Fu, M.; He, H.; Wang, X. Depression among Chinese older adults: A perspective from Hukou and health inequities. J. Affect. Disord. 2017, 223, 115–120. [Google Scholar] [CrossRef]
- Hu, H.; Cao, Q.; Shi, Z.; Lin, W.; Jiang, H.; Hou, Y. Social support and depressive symptom disparity between urban and rural older adults in China. J. Affect. Disord. 2018, 237, 104–111. [Google Scholar] [CrossRef]
- Williamson, J.B.; Fang, L.; Calvo, E. Rural pension reform in China: A critical analysis. J. Aging Stud. 2017, 41, 67–74. [Google Scholar] [CrossRef]
- Kaushal, N. How public pension affects elderly labor supply and well-being: Evidence from India. World Dev. 2014, 56, 214–225. [Google Scholar] [CrossRef]
- Evangelista de Carvalho, I.F. Old-age benefits and retirement decisions of rural elderly in Brazil. J. Dev. Econ. 2008, 86, 129–146. [Google Scholar] [CrossRef]
- Fernández-Niño, J.A.; Bonilla-Tinoco, L.J.; Manrique-Espinoza, B.S.; Romero-Martínez, M.; Sosa-Ortiz, A.L. Work status, retirement, and depression in older adults: An analysis of six countries based on the Study on Global Ageing and Adult Health (SAGE). SSM Popul. Health 2018, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Shu, L. The effect of the new rural social pension insurance program on the retirement and labor supply decision in China. J. Econ. Ageing 2018, 12, 135–150. [Google Scholar] [CrossRef]
- Buys, L.; Roberto, K.A.; Miller, E.; Blieszner, R. Prevalence and predictors of depressive symptoms among rural older Australians and Americans. Aust. J. Rural Health 2008, 16, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Golberstein, E. The effects of income on mental health: Evidence from the social security notch. J. Ment. Health Policy Econ. 2015, 18, 27–37. [Google Scholar]
- Barrientos, A.; Gorman, M.; Heslop, A. Old age poverty in developing countries: Contributions and dependence in later life. World Dev. 2003, 31, 555–570. [Google Scholar] [CrossRef]
- Mirowsky, J.; Ross, C.E. Age and the effect of economic hardship on depression. J. Health Soc. Behav. 2001, 42, 132–150. [Google Scholar] [CrossRef]
- Baicker, K.; Taubman, S.; Allen, H.; Bernstein, M.; Gruber, J.; Newhouse, J.; Schneider, E.; Wright, B.; Zaslavsky, A.; Finkelstein, A.; et al. The oregon experiment—Effects of medicaid on clinical outcomes. N. Engl. J. Med. 2013, 368, 1713–1722. [Google Scholar] [CrossRef]
- Chen, X.; Wang, T.; Busch, S.H. Does money relieve depression: Evidence from social pension expansions in China. Soc. Sci. Med. 2019, 220, 411–420. [Google Scholar] [CrossRef]
- Cheng, L.; Liu, H.; Zhang, Y.; Zhao, Z. The health implications of social pensions: Evidence from China’s new rural pension scheme. J. Comp. Econ. 2018, 46, 53–57. [Google Scholar] [CrossRef]
- Lloyd-Sherlock, P.; Barrientos, A.; Moller, V.; Saboia, J. Pensions, poverty and wellbeing in later life: Comparative research from South Africa and Brazil. J. Aging Stud. 2012, 26, 243–252. [Google Scholar] [CrossRef]
- Tong, Y.; Chen, F.; Su, W. Living arrangements and older People’s labor force participation in Hong Kong, 1986–2016. Soc. Sci. Med. 2019, 229, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Chaaya, M.; Sibai, A.M.; Tabbal, N.; Chemaitelly, H.; Roueiheb, Z.E.; Slim, Z.N. Work and mental health: The case of older men living in underprivileged communities in Lebanon. Ageing Soc. 2010, 30, 25–40. [Google Scholar] [CrossRef]
- Robeyns, I. Sen’s capability approach and gender inequality: Selecting relevant capabilities. Fem. Econ. 2003, 9, 61–92. [Google Scholar] [CrossRef]
- Zunzunegui, M.V.; Alvarado, B.E.; Ser, T.D.; Otero, A. Social networks, social integration, and social engagement determine cognitive decline in community-dwelling Spanish older adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2003, 58, S93–S100. [Google Scholar] [CrossRef]
- Golden, J.; Conroy, R.M.; Bruce, I.; Denihan, A.; Greene, E.; Kirby, M.; Lawlor, B.A. Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. Int. J. Geriatr. Psychiatry 2009, 24, 694–700. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Smith, T.B.; Layton, J.B. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef]
- Wang, R.; Chen, Z.; Zhou, Y.; Shen, L.; Zhang, Z.; Wu, X. Melancholy or mahjong? Diversity, frequency, type, and rural-urban divide of social participation and depression in middle- and old-aged Chinese: A fixed-effects analysis. Soc. Sci. Med. 2019, 238, 112518. [Google Scholar] [CrossRef]
- Ruhm, C. Do pensions increase the labor supply of older men? J. Public Econ. 1996, 59, 157–175. [Google Scholar] [CrossRef]
- Ning, M.; Gong, J.; Zheng, X.; Zhuang, J. Does new rural pension scheme decrease elderly labor supply? Evidence from CHARLS. China Econ. Rev. 2016, 41, 315–330. [Google Scholar] [CrossRef]
- Fields, G.S.; Mitchell, O.S. Economic determinants of the optimal retirement age: An empirical investigation. J. Hum. Resour. 1984, 19, 245–262. [Google Scholar] [CrossRef]
- Van der Klaauw, W.; Wolpin, K.I. Social security and the retirement and savings behavior of low income households. J. Econom. 2008, 145, 21–42. [Google Scholar] [CrossRef] [PubMed]
- Grogan, L.; Summerfield, F. Government transfers, work, and wellbeing: Evidence from the Russian old-age pension. J. Popul. Econ. 2019, 32, 1247–1292. [Google Scholar] [CrossRef]
- Sánchez, R.V.; Argimón, I.; Botella, M.; González, C.I. Old age pensions and retirement in Spain. SERIEs 2013, 4, 273–307. [Google Scholar] [CrossRef]
- Dantas, R.G.; Perracini, M.R.; Guerra, R.O.; Ferriolli, E.; Dias, R.C.; Padula, R.S. What are the sociodemographic and health determinants for older adults continue to participate in work? Arch. Gerontol. Geriatr. 2017, 71, 136–141. [Google Scholar] [CrossRef]
- Öztürk, A.; Şimşek, T.T.; Yümin, E.T.; Sertel, M.; Yümin, M. The relationship between physical, functional capacity and quality of life (QoL) among elderly people with a chronic disease. Arch. Gerontol. Geriatr. 2011, 53, 278–283. [Google Scholar] [CrossRef]
- Lunau, T.; Wahrendorf, M.; Dragano, N.; Siegrist, J. Work stress and depressive symptoms in older employees: Impact of national labour and social policies. BMC Public Health 2013, 13, 1086. [Google Scholar] [CrossRef]
- Aryee, S.; Luk, V.; Leung, A.; Lo, S. Role stressors, interrole conflict, and well-being: The moderating influence of spousal support and coping behaviors among employed parents in Hong Kong. JVB 1999, 54, 259–278. [Google Scholar] [CrossRef]
- Luppa, M.; Luck-Sikorski, C.; Luck, T.; Ehreke, L.; Konnopka, A.; Wiese, B.; Weyerer, S.; König, H.-H.; Riedel-Heller, S. Age- and gender-specific prevalence of depression in latest-life—Systematic review and meta-analysis. J. Affect. Disord. 2016, 136, 212–221. [Google Scholar] [CrossRef]
- Abrams, L.R.; Mehta, N.K. Changes in depressive symptoms over age among older Americans: Differences by gender, race/ethnicity, education, and birth cohort. SSM Popul. Health 2019, 7, 100399. [Google Scholar] [CrossRef]
- Lin, B.; Lin, Z.; Zhang, Y.Y.; Lu, W. The impact of the new rural pension scheme on retirement sustainability in China: Evidence of regional differences in formal and informal labor supply. Sustainability 2018, 10, 4366. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- BOEY, K.W. Cross-validation of a short form of the CES-D in Chinese elderly. Int. J. Geriatr. Psychiatry 1999, 14, 608–617. [Google Scholar] [CrossRef]
- Chen, X.; Eggleston, K.; Sun, A. The impact of social pensions on intergenerational relationships: Comparative evidence from China. J. Econ. Ageing 2018, 12, 225–235. [Google Scholar] [CrossRef]
- Chen, T.; Turner, J.A. Fragmentation in social security old-age benefit provision in China. J. Aging Soc. Policy 2015, 27, 107–122. [Google Scholar] [CrossRef]
- The Central People’s Government of the People’s Republic of China. Available online: http://www.gov.cn/zwgk/2014–02/26/content_2621907.htm (accessed on 28 December 2019).
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Hayes, A.F.; Preacher, K.J. Statistical mediation analysis with a multicategorical independent variable. Brit. J. Math. Stat. Psychiatry 2014, 67, 451–470. [Google Scholar] [CrossRef]
- Hayes, A.F. An index and test of linear moderated mediation. Multivar. Behav. Res. 2015, 50, 1–22. [Google Scholar] [CrossRef]
- Preacher, K.J.; Rucker, D.D.; Hayes, A.F. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivar. Behav. Res. 2007, 42, 185–227. [Google Scholar] [CrossRef]
- Darlilngton, R.B.; Hayes, A.F. Regression Analysis and Linear Models: Concepts, Applications, and Implementation; Guilford Press: New York, NY, USA, 2017; p. 513. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Cole, M.G.; Dendukuri, N. Risk factors for depression among elderly community subjects: A systematic review and meta-analysis. Am. J. Psychiatry 2003, 160, 1147–1156. [Google Scholar] [CrossRef]
- Chen, Y. Investigation of prevalence and associated risk factors of depressive symptoms following acute ischemic stroke (PSD) in the aged. Psychology 2011, 2, 522–525. [Google Scholar] [CrossRef][Green Version]
- Cvjetkovic-Bosnjak, M.M.; Soldatovic-Stajic, B.S.; Babovic, S.S.; Sakac, V. Gender differences in depressive symptoms among inpatients. Klinik Psikofarmakoloji Bulteni 2016, 26, 215–328. [Google Scholar] [CrossRef]
- Peplinski, B.; McClelland, R.; Szklo, M. Associations between socioeconomic status markers and depressive symptoms by race and gender: Results from the multi-ethnic study of atherosclerosis (MESA). Ann. Epidemiol. 2018, 28, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Chun, H.; Khang, Y.H.; Kim, I.H.; Cho, S.I. Explaining gender differences in Illhealth in South Korea: The roles of socio-structural, psychosocial, and behavioral factors. Soc. Sci. Med. 2008, 67, 988–1001. [Google Scholar] [CrossRef] [PubMed]
- Martikainen, P.; Adda, J.; Ferrie, J.E.; Smith, G.D.; Marmot, M. Effects of income and wealth on GHQ depression and poor self rated health in white collar women and men in the Whitehall II study. J Epidemiol Commun. Health 2003, 57, 718–723. [Google Scholar] [CrossRef]
- Chang, Q.; Conwell, Y.; Wu, D.; Guo, Y.; Yip, P.S.F. A study on household headship, living arrangement, and recipient of pension among the older adults in association with suicidal risks. J. Affect. Disord. 2019, 256, 618–626. [Google Scholar] [CrossRef]
- Risman, B.J.; Davis, G. From sex roles to gender structure. Curr. Sociol. 2013, 61, 733–755. [Google Scholar] [CrossRef]
- Jaehn, P.; Bobrova, N.; Saburova, L.; Kudryavtsev, A.V.; Malyutina, S.; Cook, S. The relation of gender role attitudes with depression and generalised anxiety disorder in two Russian cities. J. Affect. Disord. 2020, 264, 348–357. [Google Scholar] [CrossRef]
- Kim, E.; Park, H.J.; Hogge, I. Examination of the Adlerian constructs of activity and social interest with depression among recent Korean retirees: Meaning in life as a mediator. Arch. Gerontol. Geriatr. 2015, 61, 378–383. [Google Scholar] [CrossRef]
- Zhang, W.; Feng, Q.; Lacanienta, J.; Zhen, Z. Leisure participation and subjective well-being: Exploring gender differences among elderly in Shanghai, China. Arch. Gerontol. Geriatr. 2017, 69, 45–54. [Google Scholar] [CrossRef]



| Variables | Total (N = 2709) | Men (n = 1189) | Women (n = 1520) | Men vs. Women | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ES | |
| Age | 68.3 | 6.1 | 68.7 | 6.2 | 68.0 | 6.0 | 0.127 |
| Marital Status | 0.122 | ||||||
| Have a life partner (N, %) | 2132 | 78.7 | 1003 | 84.4 | 1129 | 74.3 | |
| Have no spouse (N, %) | 577 | 21.3 | 186 | 15.6 | 391 | 25.7 | |
| Education Years | 3.0 | 3.3 | 4.3 | 3.3 | 2.0 | 2.8 | 0.768 |
| Functional Limitations | 6.9 | 1.9 | 6.8 | 1.8 | 7.0 | 2.0 | −0.095 |
| PI (Ln + 1) | 4.4 | 0.5 | 4.4 | 0.5 | 4.4 | 0.5 | −0.022 ns |
| PI (RMB) | 104.9 | 172.7 | 105.5 | 188.8 | 104.4 | 159.0 | 0.006 ns |
| LFP (Ln + 1) | 3.7 | 3.5 | 4.3 | 3.4 | 3.3 | 3.4 | 0.312 |
| LFP (Hours) | 779.0 | 1159.5 | 967.9 | 1277.3 | 631.3 | 1035.0 | 0.293 |
| Depressive Symptoms | 10.2 | 6.9 | 9.0 | 6.3 | 11.2 | 7.1 | −0.322 |
| Variables | Unstandardized Coefficients | SE | Standardized Coefficients (β) | t | p | R2 | |
|---|---|---|---|---|---|---|---|
| Outcome: LFP (ln + 1) | |||||||
| Constant | 17.52 | 0.89 | 19.76 | 0.0000 | 0.1237 | ||
| PI (Ln + 1) | −0.31 | 0.12 | −0.047 | −2.59 | 0.0098 | ||
| Outcome: Depressive Symptoms | |||||||
| Constant | 13.62 | 1.88 | 7.23 | 0.0000 | 0.1252 | ||
| PI (Ln + 1) | −1.30 | 0.24 | −0.098 | −5.41 | 0.0000 | ||
| LFP (Ln + 1) | 0.07 | 0.04 | 0.035 | 1.81 | 0.0707 | ||
| Unstandardized Indirect Effect | BootSE | LLCI | ULCI | ||||
| −0.0216 | 0.0157 | −0.0580 | 0.0023 | ||||
| Variables | Unstandardized Coefficients | SE | Standardized Coefficients (β) | t | p | R2 |
|---|---|---|---|---|---|---|
| Outcome: LFP (ln + 1) | ||||||
| Constant | 13.80 | 0.89 | 15.56 | 0.0000 | 0.1237 | |
| PI (Ln + 1) | −0.31 | 0.12 | −0.047 | −2.59 | 0.0098 | |
| Outcome: Depressive Symptoms | ||||||
| Constant | 12.56 | 1.84 | 6.82 | 0.0000 | 0.1381 | |
| PI (Ln + 1) | −1.34 | 0.24 | −0.101 | −5.66 | 0.0000 | |
| LFP (Ln + 1) | 0.11 | 0.04 | 0.054 | 2.79 | 0.0053 | |
| Gender | 1.61 | 0.27 | 0.117 | 5.92 | 0.0000 | |
| LFP (Ln + 1) *Gender | 0.16 | 0.07 | 0.039 | 2.17 | 0.0304 | |
| Index of Moderated Mediation (Difference between conditional indirect effects) | Index | BootSE | LLCI | ULCI | ||
| −0.0490 | 0.0312 | −0.1210 | −0.0009 | |||
| Conditional Indirect Effects | Gender | Effect | BootSE | LLCI | ULCI | |
| PI—LFP—Depressive Symptoms | Men | −0.0060 | 0.0183 | −0.0456 | 0.0311 | |
| Women | −0.0550 | 0.0276 | −0.1141 | −0.0092 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gao, X.; Feng, T. Public Pension, Labor Force Participation, and Depressive Symptoms across Gender among Older Adults in Rural China: A Moderated Mediation Analysis. Int. J. Environ. Res. Public Health 2020, 17, 3193. https://doi.org/10.3390/ijerph17093193
Gao X, Feng T. Public Pension, Labor Force Participation, and Depressive Symptoms across Gender among Older Adults in Rural China: A Moderated Mediation Analysis. International Journal of Environmental Research and Public Health. 2020; 17(9):3193. https://doi.org/10.3390/ijerph17093193
Chicago/Turabian StyleGao, Xin, and Tieying Feng. 2020. "Public Pension, Labor Force Participation, and Depressive Symptoms across Gender among Older Adults in Rural China: A Moderated Mediation Analysis" International Journal of Environmental Research and Public Health 17, no. 9: 3193. https://doi.org/10.3390/ijerph17093193
APA StyleGao, X., & Feng, T. (2020). Public Pension, Labor Force Participation, and Depressive Symptoms across Gender among Older Adults in Rural China: A Moderated Mediation Analysis. International Journal of Environmental Research and Public Health, 17(9), 3193. https://doi.org/10.3390/ijerph17093193




