Testing the Preliminary Validity of a Multidimensional Framework for Studying the Effects of Cancer Health Literacy on Cancer Screening Behaviors among Diverse Populations
Abstract
1. Introduction
2. Materials and Methods
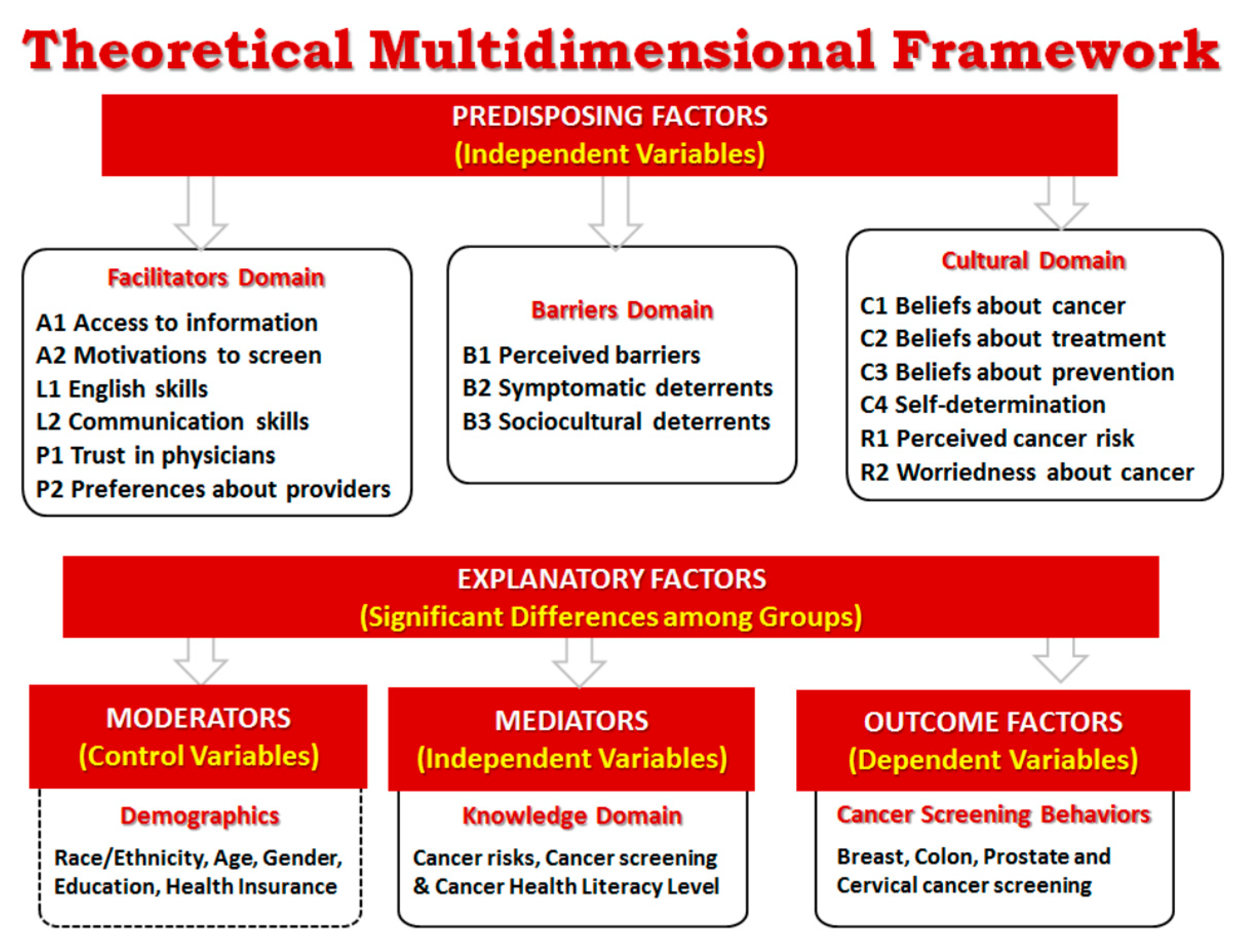
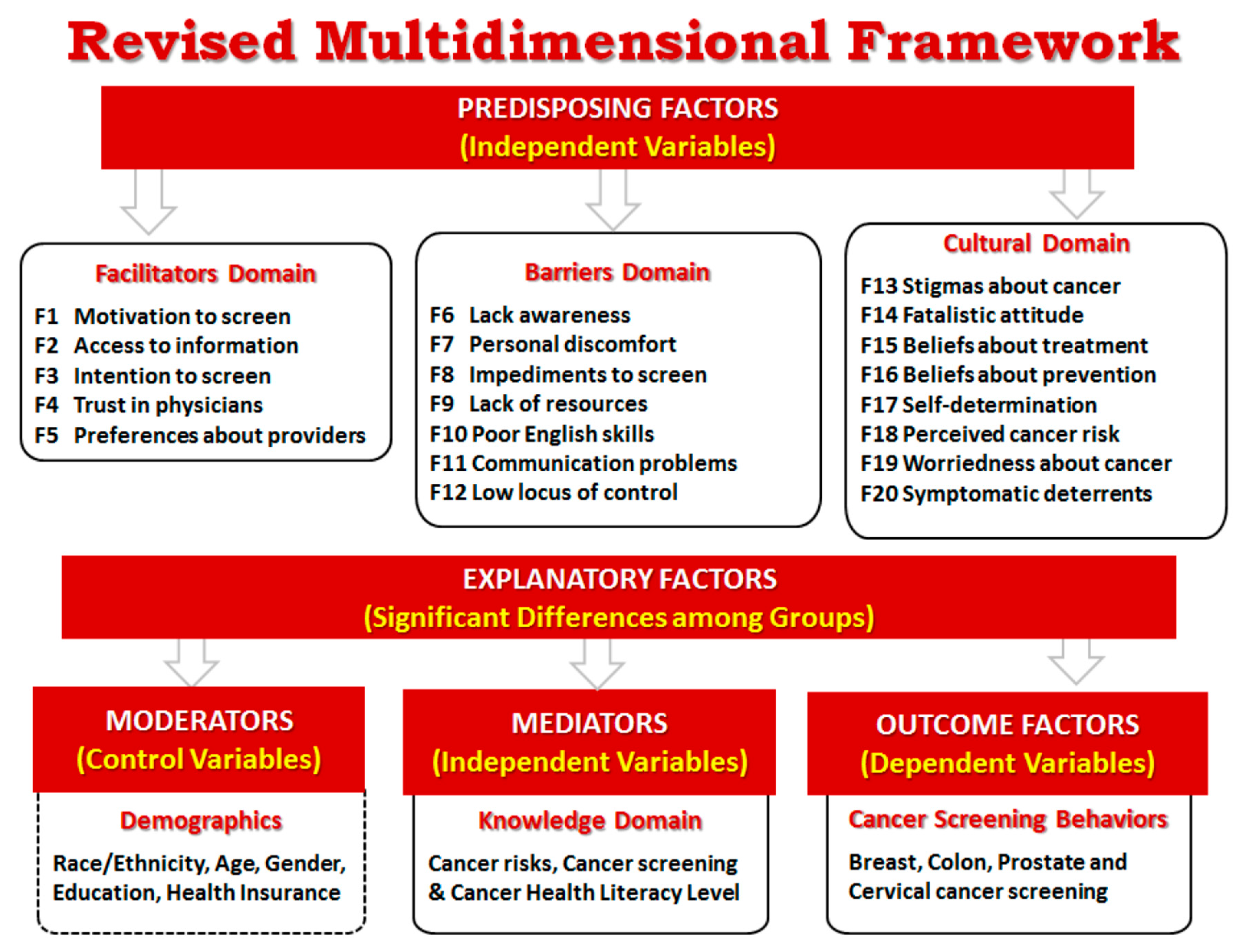
2.1. Development of Multidimensional Cancer Literacy Framework (MCLF)
2.2. Development of Multidimensional Cancer Literacy Questionnaire (MCLQ)
2.3. Participants and Data Collection Procedure for Field Test
2.4. Statistical Analysis to Refine the MCLQ
3. Results
3.1. Multidimensional Framework Exploration
3.2. Facilitators Domain
3.3. Barriers Domain
3.4. Cultural Domain
3.5. Secondary Analysis of Preliminary Validity of the Constructs
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Disclaimer
References
- Mantwill, S.; Monestel-Umaña, S.; Schulz, P.J. The relationship between health literacy and health disparities: A systematic review. PLoS ONE 2015, 10, e0145455. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Viera, A.; Crotty, K.; Holland, A.; Brasure, M.; Viswanathan, M. Health Literacy Interventions and Outcomes: An Updated Systematic Review; Evidence Report/Technology Assessment No. 199, AHRQ Publication Number 11-E006; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2011.
- Dewalt, D.A.; Berkman, N.D.; Sheridan, S.; Lohr, K.N.; Pignone, M.P. Literacy and health outcomes: A systematic review of the literature. J. Gen. Int. Med. 2004, 19, 1228–1239. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Rhee, T.G.; Kim, N.K.; Ahluwalia, J.S. Health literacy as a social determinant of health in Asian American immigrants: Findings from a population-based survey in California. J. Gen. Int. Med. 2015, 30, 1118. [Google Scholar] [CrossRef] [PubMed]
- Peterson, P.N.; Shetterly, S.M.; Clarke, C.L.; Bekelman, D.B.; Chan, P.S.; Allen, L.A.; Masuidi, F.A. Health literacy and outcomes among patients with heart failure. JAMA 2011, 305, 1695–1701. [Google Scholar] [CrossRef]
- Simmons, R.A.; Cosgrove, S.C.; Romney, M.C.; Plumb, J.D.; Brawer, R.O.; Gonzalez, E.T.; Fleisher, L.G.; Moore, B.S. Health literacy: Cancer prevention strategies for early adults. Am. J. Prev. Med. 2017, 53 (Suppl. 1), S73–S77. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services. Healthy People 2020: Health Literacy. Available online: https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/health-literacy (accessed on 27 February 2020).
- U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. National Action Plan to Improve Health Literacy; U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion: Washington, DC, USA, 2010.
- Easton, P.; Entwistle, V.A.; Williams, B. Health in the ’hidden population’ of people with low literacy. A systematic review of the literature. BMC Public Health 2010, 10, 459. [Google Scholar] [CrossRef]
- Eastman, P. The link between health literacy & cancer communication. Oncol. Times 2019, 41, 5–6. [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2020. Health Communication and Health Information Technology: Objectives. Available online: https://www.healthypeople.gov/2020/topics-objectives/topic/health-communication-and-health-information-technology/objectives (accessed on 27 February 2020).
- Kim, K.; Han, H.R. Potential links between health literacy and cervical cancer screening behaviors: A systematic review. Psycho Oncol. 2016, 25, 122–130. [Google Scholar] [CrossRef]
- Flores, B.E.; Acton, G.; Arevalo-Flechas, L.; Gill, S.; Mackert, M. Health literacy and cervical cancer screening among mexican-American women. HLRP Health Lit. Res. Pract. 2019, 3, e1–e8. [Google Scholar] [CrossRef]
- Karadag, A.S.; Bakan, A.B.; Aslan, G. Distribution of cervical and breast cancer risk factors in women and their screening behaviours. Eur. J. Cancer Care 2019, 28, e12960. [Google Scholar] [CrossRef]
- Oldach, B.R.; Katz, M.L. Health literacy and cancer screening: A systematic review. Patient Educ. Couns. 2014, 94, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Lofters, A.K.; Shuler, A.; Slater, M.; Baxter, N.N.; Persaud, N.; Kiran, T. Using self-reported data on the social determinants of health in primary care to identify cancer screening disparities: Opportunities and challenges. BMC Fam. Pract. 2017, 18, 31. [Google Scholar] [CrossRef] [PubMed]
- Diaz, J.A.; Roberts, M.B.; Clarke, J.G.; Simmons, E.M.; Goldman, R.E.; Rakowski, W. Colorectal Cancer Screening: Language is a Greater Barrier for Latino Men than Latino Women. J. Immigr. Minority Health 2013, 15, 472–475. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fridman, D.; Dominick, G.M. African American men’s understanding and perceptions about prostate cancer: Why multiple dimensions of health literacy are important in cancer communication. J. Community Health 2009, 34, 449–460. [Google Scholar] [CrossRef]
- Berkman, N.D.; Davis, T.C.; McCormack, L. Health literacy: What is it? J. Health Commun. Int. Perspect. 2010, 15 (Suppl. 2), 9–19. [Google Scholar] [CrossRef]
- Gazmararian, J.A.; Williams, M.V.; Peel, J.; Baker, D.W. Health literacy and knowledge of chronic disease. Patient Educ. Couns. 2003, 51, 267–275. [Google Scholar] [CrossRef]
- Heijmans, M.; Waverijn, G.; Rademakers, J.; Van der Vaart, R.; Rijken, M. Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management. Patient Educ. Couns. 2015, 98, 41–48. [Google Scholar] [CrossRef]
- Shaw, S.J.; Armin, J.; Torres, C.H.; Orzech, K.M.; Vivian, J. Chronic disease self-management and health literacy in four ethnic groups. J. Health Commun. 2012, 17 (Suppl. 3), 67–81. [Google Scholar] [CrossRef]
- Dumenci, L.; Matsuyama, R.K.; Kuhn, L.; Perera, R.A.; Siminoff, L.A. On the validity of the shortened Rapid Estimate of Adult Literacy in Medicine (REALM) scale as a measure of health literacy. Commun. Methods Meas. 2013, 7, 134–143. [Google Scholar] [CrossRef]
- Housten, A.J.; Lowenstein, L.M.; Hoover, D.S.; Leal, V.B.; Kamath, G.R.; Volk, R.J. Limitations of the S-TOFHLA in measuring poor numeracy: A cross-sectional study. BMC Public Health 2018, 18, 405. [Google Scholar] [CrossRef]
- Sharma, S.; Oremus, M. PRISMA and AMSTAR show systematic reviews on health literacy and cancer screening are of good quality. J. Clin. Epidemiol. 2018, 99, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Zarcadoolas, C.; Pleasant, A.; Greer, D.S. Advancing Health Literacy: A Framework for Understanding and Action; Jossey-Bass: San Francisco, CA, USA, 2006. [Google Scholar]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, F.; Brand, H. Heath literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, V.H.; Armes, J.; Ream, E. Perceptions of prostate cancer in Black African and Black Caribbean men: A systematic review of the literature. Pscho Oncol. 2012, 21, 457–468. [Google Scholar] [CrossRef] [PubMed]
- Neuhauser, L. Integrating participatory design and health literacy to improve research and interventions. Inf. Serv. Use 2017, 37, 153–176. [Google Scholar] [CrossRef]
- Strecher, V.J.; Rosenstock, I.M.; Glanz, K.; Lewis, F.M.; Rimer, B.K. Health Behavior and Health Education: Theory, Research and Practice, 2nd ed.; Jossey-Bass Publisher: San Francisco, CA, USA, 1997. [Google Scholar]
- Betancourt, H.; Flynn, P.M.; Riggs, M.; Garberoglio, C. A cultural research approach to instrument development: The case of breast and cervical cancer screening among Latino and Anglo women. Health Educ. Res. 2010, 25, 991–1007. [Google Scholar] [CrossRef] [PubMed]
- Buki, L.; Yee, B. Culture and Cancer Literacy: Health Literacy Measure. 2010; (unpublished). (Confidential copy received from author on 5 May 2014). [Google Scholar]
- Gansler, T.; Henley, S.J.; Stein, K.; Slaughter, E. Sociodemographic determinants of cancer treatment health literacy. Cancer 2005, 104, 653–660. [Google Scholar] [CrossRef]
- National Cancer Institute. Health Information National Trends Survey; HINTS 5 Cycle 3 Codebook; National Cancer Institute: Bethesda, MA, USA. Available online: https://hints.cancer.gov/docs/Instruments/HINTS5C3_Annotated_Instrument_English.pdf (accessed on 27 February 2020).
- Mayfield, J.B. Development and validation of the Cancer Literacy Measure for African Americans. Ph.D. Thesis, Doctor of Philosophy in Educational Psychology, Graduate College of the University of Illinois at Urbana-Champaign, Champaign, IL, USA, 2014. [Google Scholar]
- Morris, N.S.; Field, T.S.; Wagner, J.L.; Mazor, K.M. The association between health literacy and cancer-related attitudes, behaviors, and knowledge. J. Health Commun. Int. Perspect. 2014, 18 (Suppl. 1), 223–241. [Google Scholar] [CrossRef]
- Babbie, E. The Practice of Social Research, 12th ed.; Wadsworth Publishing Company: Belmont, CA, USA, 2009; p. 530. [Google Scholar]
- Thompson, B. Exploratory and Confirmatory Factor Analysis; American Psychological Association: Washington, DC, USA, 2004; Available online: https://epdf.pub/queue/exploratory-and-confirmatory-factor-analysis-understanding-concepts-and-applicat.html# (accessed on 24 April 2020).
- Yong, A.D.; Pearce, S. A Beginner’s guide to factor analysis: Focusing on exploratory factor analysis. Tutor. Quant. Methods Psychol. 2013, 9, 79–94. [Google Scholar] [CrossRef]
- Nunnally, J.C. Psychometric Theory, 2nd ed.; McGraw-Hill: New York, NY, USA, 1978. [Google Scholar]
- Anderson, J.C.; Gerbing, D.W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Echeverri, M.; Anderson, D.; Napoles, A.M.; Haas, J.M.; Johnson, M.E.; Serrano, S.A. Cancer health literacy and willingness to participate in cancer research and donate bio-specimens. Int. J. Environ. Res. Public Health 2018, 15, 2091. [Google Scholar] [CrossRef]
- Rogers, C.R.; Goodson, P. Male role norms, knowledge, attitudes, and perceptions of colorectal cancer screening among young adult African American Men. Front. Public Health 2014, 2, 252. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Education. Adult Literacy in the United States; National Center for Education Statistics (NCES) report 2019-179; U.S. Department of Education: Washington, DC, USA, 2019. Available online: https://nces.ed.gov/pubs2019/2019179.pdf (accessed on 24 April 2020).
- American College Testing. The Condition of College & Career Readiness 2019; ACT, Inc.: Washington, DC, USA, 2019; Available online: www.act.org/condition2019 (accessed on 24 April 2020).
- Klein, W.M.P.; Stefanek, M.E. Cancer risk elicitation and communication: Lessons from the psychology of risk perception. CA Cancer J. Clin. 2007, 57, 147–167. [Google Scholar] [CrossRef] [PubMed]
- Lipkus, I.M.; Kuchibhatla, M.; McBride, C.M.; Bosworth, H.B.; Pollak, K.I.; Siegler, L.C.; Rime, B.K. Relationships among breast cancer perceived absolute risk, comparative risk, and worries. Cancer Epidemiol. Biomark. Prev. 2000, 9, 973–975. [Google Scholar]
| Domains and Factors | Item Content | Sources of Items or Item Themes |
|---|---|---|
| Facilitators Domain | ||
| E1. Motivations to screen (9 items) 1 | I have had regular cancer screening because a-I asked my doctor to order the test; b-An interpreter was available during the exam; c-The doctor/nurse recommended it; d-A family member or friend recommended it; e-I got a reminder card in the mail; f-I had a symptom that made me worry; g-I did not have to pay for it; h-I had the money to pay for the exam; i-I had somebody to go with me to the appointment | a–h Adapted from Buki [32]; i-added by participants in the pilot-test |
| E2. Access to information (8 items) 2 | How much information about cancer have you received from a-Doctors or other health professionals; b-Family or friends; c-Newspapers or magazines; d-The radio or television; e-The Internet; f-Religious organizations and leaders; g-Government health agencies; h-Community health fairs | Adapted from HINTS [34]; Buki [32] |
| L1. English skills (3 items) 3 | How well do you a-speak English; b-read English; c-write English | Adapted from HINTS [34] |
| L2. Communication skills (3 items) 1 | a-It is difficult for me to fill out medical forms; b-I have a hard time understanding when health professionals speak to me quickly; c-I have had difficulties understanding doctors who come from other regions and have a different English accent | a-Adapted from Buki [32]; b-Adapted Morris [36]; c-Recommended by Latino participants in pilot-test |
| P1. Trust in Physicians (4 items) 4 | a-How much do you trust your doctor’s decisions about which medical screenings are best for you; b-How much do you trust doctors of a different race/ethnicity from you; c-How much do you trust doctors of same cultural background; d-How effective are doctors at curing illness | all-Adapted from Mayfield [35]; Buki [32] |
| P2. Preferences about Providers (4 items) 1 | a-I prefer my doctor to be of my same gender; b-I prefer my doctor to be of my same racial/ethnic and cultural background; c-I prefer a doctor who speaks my language; d-I prefer my doctor to be of my same religion | Added by participants in pilot-test and adapted by authors’ experience with previous research |
| Barriers Domain | ||
| B1. Perceived barriers to screening (7 items) 1 | The following would be barriers or obstacles for me to have regular cancer screenings a-The doctor does not order the tests; b-Being unsure if there is a need for testing; c-Lack of trust on these cancer tests; d-Being afraid the test will cause harm if it is not well done; e-Being afraid the test will cause cancer; f-Dislike having exams in those parts of the body; g-Do not want to know if cancer is present | a–g Adapted from Buki [32] |
| B2. Symptomatic deterrents (4 items) 1 | There is no need to have cancer screenings when a-Feeling healthy; b-Having several normal screening test results; c-Not feeling anything abnormal (symptoms); d-Being too young or too old | a–c Adapted from Betancourt [31]; d-added by participants in the pilot-test |
| B3. Sociocultural deterrents (13 items) 5 | I have had the following problems to get the cancer screening exams a-Do not know where to go for the exam; b-Have forgotten to make the appointment; c-Have had problems making the appointment; d-Do not know if it is time to have the exams; e-Have not received a reminder postcard; f-Waiting too long for an appointment; g-Not able to get time off work; h-Lack of transportation to go to the appointment; i-Need somebody to take care of my children or family; j-Lack of health insurance; k-Lack of money to pay for the exam; l-Need an interpreter during the appointment; m-Need a friend/family to go with me to the appointment | a,c,e,g–k Adapted from Betancourt [31]; b,d,f, Adapted Buki [32]; l–m Added by Latino participants |
| Cultural Domain | ||
| C1. Beliefs about cancer as a disease (7 items) 1 | a-It seems like almost everything causes cancer; b-Cancer is due to bad luck; c-Cancer is a punishment from God; d-Cancer is the worst thing that can happen to a person; e-Cancer is a deadly disease; f-When I think of cancer, I automatically think of death; g-Everybody has cancer but only some develop the disease | a-Adapted from Morris [36]; HINTS [34]; b-Adapted Buki [32]; c-Adapted Buki [32]; d-e Adapted Betancourt [31]; f-HINTS [34]; g-added by participants in pilot-test |
| C2. Beliefs about cancer treatment (5 items) 1 | a-All you need to beat cancer is a positive attitude, no treatment; b-Treating cancer with surgery can cause it to spread throughout the body; c-Cancer can be only cured if it is God’s will; d-There is a cure for cancer but it is only available to the rich and privileged; e-There is nothing I can do to change my fate if I find out I have cancer. | a-b Adapted from Gansler [33]; c-Added by participants in pilot-test; d-Recommended by participants in pilot-test; e-Adapted HINTS [34] |
| C3. Beliefs about screening as a preventive measure (10 items) 1 | a-It is not necessary to have cancer screening regularly because it is in God’s hands anyway; b-It is not necessary to have cancer screening regularly because everyone will eventually die of something anyway; c-It is not necessary to have cancer screening regularly because if you are meant to get cancer you will get it no matter what you do; d-There are so many recommendations about preventing cancer; it’s hard to know which ones to follow; e-There is not much people can do to lower their chances of getting cancer; f-Cancer screenings help to save lives; g-Other people my age have cancer screenings regularly; h-All people should have regular cancer screenings; i-Routine cancer screening is a way to show that people care for their health and their families; j-It is possible for me to get cancer during my lifetime | a–b Adapted from Betancourt [31]; Morris [36], HINTS [34]; Buki [32] |
| C4. Self-Determination (8 items) 1 | a-I feel comfortable checking my own body for signs of health problems; b-If I noticed a symptom, I would go to the doctor to get it checked immediately; c-If I found out I have cancer, I would seek a second opinion about my condition and treatment options; d-I would offend my doctor if I were to make my own decision(s) about my health; e-I don’t know enough to make my own medical decisions; f-I’d rather be given many choices about what’s best for my health than have the doctor make the decision for me; g-Sometimes, there are good reasons not to follow the advice of a doctor; h-I feel that some doctors treat me differently because of my different racial background | a–h Adapted from Buki [32] |
| R1. Perceived cancer risk (7 items) 6 | Compared to other people my age and my same gender, I think that my risk of getting the following cancers are a-Breast cancer; b-Cervical cancer; c-Colon cancer; d-Stomach cancer; e-Liver cancer; f-Skin cancer; g-Prostate cancer | Adapted from HINTS [34] |
| R2. Worriedness about cancer (7 items) 7 | How often do you worry about getting one of the following cancer types in your lifetime a-Breast cancer; b-Cervical cancer; c-Colon cancer; d-Stomach cancer; e-Liver cancer; f-Skin cancer; g-Prostate cancer | Adapted from HINTS [34] |
| African Americans 2 | Latinos 3 | Whites 4 | Total | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | N | % | |
| Total Participants | 500 | 33.3 | 500 | 33.3 | 500 | 33.33 | 1500 | 100.0 |
| Gender | ||||||||
| Male | 250 | 50.0 | 250 | 50.0 | 250 | 50.0 | 750 | 50.0 |
| Female | 250 | 50.0 | 250 | 50.0 | 250 | 50.0 | 750 | 50.0 |
| Age | ||||||||
| 25–40 | 135 | 27.0 | 211 | 42.2 | 181 | 36.2 | 527 | 35.1 |
| 41–55 | 169 | 33.8 | 150 | 30.0 | 143 | 28.6 | 462 | 30.8 |
| 56+ | 196 | 39.2 | 139 | 27.8 | 176 | 35.2 | 511 | 34.1 |
| Education | ||||||||
| Primary school or lower | 11 | 2.2 | 112 | 22.4 | 3 | 0.6 | 126 | 8.4 |
| Some High School | 76 | 15.2 | 74 | 14.8 | 29 | 5.8 | 179 | 11.9 |
| High School Diploma | 187 | 37.4 | 111 | 22.2 | 132 | 26.4 | 430 | 28.7 |
| Some college or vocational diploma | 152 | 30.4 | 133 | 26.6 | 175 | 35.0 | 460 | 30.7 |
| Bachelor or advanced degree | 74 | 14.8 | 70 | 14.0 | 161 | 32.2 | 305 | 20.3 |
| Domains and Factors | % of Variance | N | Mean 1 | SD | Cronbach’s Alpha | Number of Items |
|---|---|---|---|---|---|---|
| Facilitators Domain | 21.04 | 28 | ||||
| F1 Motivation to screen 2 | 4.237 | 1104 | 2.71 | 1.094 | 0.813 | 7 |
| F2 Access to information | 6.126 | 1500 | 2.49 | 1.064 | 0.910 | 8 |
| F3 Intention to screen | 3.956 | 1500 | 3.92 | 0.995 | 0.821 | 5 |
| F4 Trust in physicians | 3.494 | 1500 | 3.87 | 0.837 | 0.845 | 4 |
| F5 Preferences about providers | 3.230 | 1500 | 2.54 | 1.154 | 0.822 | 4 |
| Barriers Domain | 22.41 | 26 | ||||
| F6 Lack awareness | 1.970 | 1500 | 2.89 | 1.378 | 0.757 | 2 |
| F7 Personal discomfort | 3.961 | 1500 | 2.20 | 1.096 | 0.833 | 5 |
| F8 Impediments to screen | 4.881 | 1500 | 1.97 | 1.047 | .866 | 6 |
| F9 Lack of resources | 3.530 | 1500 | 1.78 | 1.022 | 0.836 | 5 |
| F10 Poor English skills | 4.209 | 1500 | 3.83 | 1.527 | 0.978 | 3 |
| F11 Communication problems | 2.127 | 1500 | 2.46 | 1.214 | 0.670 | 3 |
| F12 Low locus of control | 1.731 | 1500 | 2.92 | 1.256 | 0.480 | 2 |
| Cultural Domain | 23.49 | 28 | ||||
| F13 Stigmas about cancer | 1.999 | 1500 | 1.48 | 0.918 | 0.755 | 2 |
| F14 Fatalistic attitude | 2.586 | 1500 | 3.16 | 1.259 | 0.750 | 3 |
| F15 Beliefs about treatment | 1.829 | 1500 | 2.70 | 1.262 | 0.517 | 2 |
| F16 Beliefs about prevention | 3.561 | 1500 | 1.98 | 0.934 | 0.776 | 5 |
| F17 Self-determination | 2.225 | 1500 | 3.56 | 0.914 | 0.569 | 4 |
| F18 Perceived cancer risk | 3.870 | 1500 | 2.77 | 0.868 | 0.900 | 4 |
| F19 Worriedness about cancer | 3.976 | 1500 | 1.96 | 1.086 | 0.922 | 4 |
| F20 Symptomatic deterrents | 3.448 | 1500 | 2.52 | 1.292 | 0.856 | 4 |
| Total Scale | 66.95 | 1104 | 0.888 | 82 |
| Factors and Items | Item Description | Factor Load | Mean 1 | SD | CITC | h2 |
|---|---|---|---|---|---|---|
| F1 Motivation to screen (7 items) | ||||||
| F1e_GotRemainder | Received a reminder (mail/call) | 0.730 | 2.69 | 1.386 | 0.620 | 0.579 |
| F1g_WasFree | Free service | 0.697 | 2.64 | 1.377 | 0.574 | 0.524 |
| F1f_HadSymptom | Had a symptom | 0.691 | 2.70 | 1.392 | 0.574 | 0.530 |
| F1i_GotCompany | Had company to go to the appointment | 0.671 | 2.45 | 1.347 | 0.550 | 0.544 |
| F1c_DoctorOrdered | The doctor/nurse recommended it | 0.659 | 3.33 | 1.392 | 0.520 | 0.528 |
| F1d_FriendRecommended | A family/friend recommended it | 0.657 | 2.55 | 1.309 | 0.545 | 0.497 |
| F1h_HadMoney | Had the money to pay for the exam/copayment | 0.600 | 2.64 | 1.359 | 0.471 | 0.412 |
| F2 Access to information (8 items) | ||||||
| F2d_InfoFromRadioTV | From the radio or television | 0.819 | 2.71 | 1.292 | 0.756 | 0.699 |
| F2g_InfoAgenciasGno | From government health agencies | 0.814 | 2.20 | 1.350 | 0.750 | 0.697 |
| F2c_InfoFromNewspaper | From newspapers, bulletins, magazines | 0.811 | 2.62 | 1.311 | 0.745 | 0.706 |
| F2h_InfoFromHealthFairs | From community health fairs | 0.796 | 2.27 | 1.392 | 0.716 | 0.693 |
| F2f_InfoFromNGOs | From religious and community organizations | 0.783 | 2.06 | 1.345 | 0.700 | 0.728 |
| F2e_InfoFromInternet | From the Internet | 0.769 | 2.70 | 1.413 | 0.691 | 0.668 |
| F2b_InfoFromFriends | From family or friends | 0.728 | 2.70 | 1.357 | 0.680 | 0.610 |
| F2a_InfoFromDoctor | From doctors or other health professionals | 0.673 | 2.62 | 1.404 | 0.639 | 0.588 |
| F3 Intention to screen (5 items) | ||||||
| C3i_ScreenRegularCare | Routine cancer screening shows that people care for their health and their families | 0.845 | 4.14 | 1.253 | 0.748 | 0.773 |
| C3h_ScreenRegularAll | All people should have regular cancer screenings | 0.827 | 4.08 | 1.273 | 0.718 | 0.751 |
| C3f_ScreenSaveLifes | Cancer screenings help to save lives | 0.778 | 4.20 | 1.273 | 0.653 | 0.646 |
| C3j_PossibleHaveCancerLife | It is possible to get cancer during lifetime | 0.628 | 3.88 | 1.370 | 0.493 | 0.562 |
| C3g_ScreenRegularAge | Friends of my age have cancer screenings regularly | 0.618 | 3.30 | 1.348 | .481 | 0.479 |
| F4 Trust in physicians (4 items) | ||||||
| P1c_TrustSameCulture | Trust doctors of same cultural background | 0.861 | 3.97 | 1.011 | 0.767 | 0.786 |
| P1b_TrustDifferentRace | Trust doctors of a different race/ethnicity | 0.845 | 3.82 | 1.085 | 0.737 | 0.766 |
| P1a_TrustMedicalAdvise | Trust doctor’s decisions about medical screenings | 0.775 | 3.95 | .915 | 0.653 | 0.658 |
| P1d_TrustCureDiseases | Trust doctors effectiveness to curing diseases | 0.706 | 3.74 | 1.035 | 0.581 | 0.588 |
| F5 Preferences about providers (4 items) | ||||||
| P2b_SameRace | Preference for a doctor of same race/culture | 0.840 | 2.47 | 1.403 | 0.762 | 0.791 |
| P2a_SameGender | Preference for a doctor of same gender | 0.787 | 2.63 | 1.430 | 0.615 | 0.683 |
| P2c_SameLanguage | Preference for a doctor who speaks same language | 0.718 | 2.82 | 1.512 | 0.638 | 0.692 |
| P2d_SameReligion | Preference for a doctor of same religion | 0.698 | 2.24 | 1.370 | 0.571 | 0.635 |
| Factors and Items | Item Description | Factor Loads | Mean 1 | SD | CITC | h2 |
|---|---|---|---|---|---|---|
| F6 Lack awareness (2 items) | ||||||
| B1a_TestNoOrdered | Doctor does not order the screening tests | 0.809 | 2.85 | 1.588 | 0.610 | 0.749 |
| B1b_UnsureNeedTest | Being unsure if there is a need for screening | 0.801 | 2.93 | 1.485 | 0.610 | 0.778 |
| F7 Personal discomfort (5 items) | ||||||
| B1d_AfraidTestHarm | Being afraid the test will cause harm if it is not well done | 0.799 | 2.24 | 1.411 | 0.704 | 0.716 |
| B1e_AfraidTestCancer | Being afraid the test will cause cancer | 0.758 | 1.91 | 1.291 | 0.647 | 0.667 |
| B1f_DislikeTestTouching | Dislike having exams in private parts of the body | 0.690 | 2.38 | 1.469 | 0.634 | 0.596 |
| B1c_LackTrustResults | Lack of trust on cancer screening tests | 0.682 | 2.19 | 1.371 | 0.606 | 0.594 |
| B1g_DontWantKnow | Do not want to know if cancer is present | 0.658 | 2.26 | 1.524 | 0.580 | 0.547 |
| F8 Impediments to screen (6 items) | ||||||
| B3b_ForgotMakeAppt | Forgot to make the appointment | 0.780 | 1.87 | 1.276 | 0.692 | 0.689 |
| B3c_ProblemMakeAppt | Had problems making the appointment | 0.750 | 1.74 | 1.218 | 0.708 | 0.689 |
| B3d_DonotKnowWhen | Do not know if it is time to have the exams | 0.749 | 2.16 | 1.426 | 0.686 | 0.659 |
| B3e_NoReminder | Have not received a reminder (mail, call, etc.) | 0.698 | 2.10 | 1.448 | 0.666 | 0.616 |
| B3f_WaitTimeAppt | Waiting too long for an appointment | 0.670 | 1.92 | 1.279 | 0.635 | 0.606 |
| B3a_DontKnowWhere | Do not know where to go for the exam | 0.600 | 2.02 | 1.457 | 0.598 | 0.567 |
| F9 Lack of resources (5 items) | ||||||
| B3k_NoMoney | Lack of money to pay for the exam/copayment | 0.774 | 2.13 | 1.529 | 0.699 | 0.734 |
| B3j_NoInsurance | Lack of health insurance | 0.762 | 2.00 | 1.517 | 0.691 | 0.730 |
| B3i_NoChildCare | Need child/family care services | 0.634 | 1.48 | 1.053 | 0.580 | 0.578 |
| B3h_NoTransportation | Lack of transportation to go to the appointment | 0.631 | 1.60 | 1.153 | 0.643 | 0.621 |
| B3m_NeedCompany | Need company to go to the appointment | 0.566 | 1.68 | 1.257 | 0.608 | 0.585 |
| F10 Poor English skills (3 items) | ||||||
| L1b_ReadEnglish | How well do you read English | −0.915 | 3.83 | 1.546 | 0.961 | 0.930 |
| L1c_WriteEnglish | How well do you write English | −0.908 | 3.76 | 1.618 | 0.951 | 0.916 |
| L1a_SpeakEnglish | How well do you speak English | −0.908 | 3.88 | 1.518 | 0.943 | 0.913 |
| F11 Communication problems (3 items) | ||||||
| L2b_DifficultUnderFast | Hard time understanding doctors who speak quickly | 0.763 | 2.46 | 1.571 | 0.652 | 0.777 |
| L2c_DifficultAccent | Difficulties understanding doctors who have heavy accent | 0.713 | 2.74 | 1.614 | 0.276 | 0.616 |
| L2a_DifficultFillForms | Difficulty to fill out medical forms | 0.666 | 2.19 | 1.506 | 0.561 | 0.734 |
| F12 Low locus of control (2 items) | ||||||
| C4e_DontKnowDecision | Lack knowledge to make own decisions | 0.789 | 3.21 | 1.580 | 0.316 | 0.683 |
| C4d_OffendDoctor | Afraid of offending doctor when making own decisions | 0.681 | 2.63 | 1.517 | 0.316 | 0.595 |
| Factors and Items | Item Description | Factor Loads | Mean 1 | SD | CITC | h2 |
|---|---|---|---|---|---|---|
| F13 Stigmas about cancer (2 items) | ||||||
| C1b_CancerBadLuck | Cancer is due to bad luck | 0.803 | 1.55 | 1.055 | 0.608 | 0.765 |
| C1c_CancerPunishment | Cancer is a punishment from God | 0.799 | 1.41 | 0.992 | 0.608 | 0.767 |
| F14 Fatalistic attitude (3 items) | ||||||
| C1e_CancerEqualDeath | Cancer is a deadly disease | 0.829 | 3.53 | 1.519 | 0.591 | 0.722 |
| C1f_CancerThinkDeath | When thinking of cancer, automatically think of death | 0.798 | 3.11 | 1.512 | 0.614 | 0.705 |
| C1d_CancerWorstThing | Cancer is the worst thing that can happen to a person | 0.730 | 2.84 | 1.596 | 0.528 | 0.629 |
| F15 Beliefs about treatment (2 items) | ||||||
| C2c_CureGodWill | Cancer can be cured only if it is God’s will | 0.736 | 2.78 | 1.665 | 0.354 | 0.654 |
| C2b_TreatSurgerySpread | Treating cancer with surgery can cause it to spread throughout the body | 0.661 | 2.63 | 1.395 | 0.354 | 0.579 |
| F16 Beliefs about prevention (5 items) | ||||||
| C3b_NoScreenAllDie | No need of cancer screening because everyone dies anyway | 0.798 | 1.64 | 1.192 | 0.651 | 0.728 |
| C3c_NoScreenNothingToDo | No need of cancer screening because you will get it no matter what you do | 0.774 | 1.65 | 1.182 | 0.670 | 0.713 |
| C3a_NoScreenGodHands | No need of cancer screening because it is in God’s hands anyway | 0.714 | 1.70 | 1.262 | 0.584 | 0.614 |
| C3e_NothingToDo | There is no so much people can do to lower chances of getting cancer | 0.571 | 2.23 | 1.356 | 0.468 | 0.446 |
| C3d_NoClearWhatToDo | Too many recommendations about preventing cancer make difficult to choose | 0.531 | 2.66 | 1.422 | 0.415 | 0.486 |
| F17 Self-determination (4 items) | ||||||
| C4f_PreferKnowOptions | Prefer having choices instead of doctor making decisions for me | 0.717 | 3.49 | 1.502 | 0.436 | 0.585 |
| C4g_OkNoFollowAdvice | There are good reasons not to follow the advice of a doctor | 0.665 | 2.75 | 1.418 | 0.289 | 0.550 |
| C4a_OkSelfExamination | Being comfortable checking own body for signs of health problems | 0.573 | 3.67 | 1.472 | 0.323 | 0.465 |
| C4c_SecondOpinion | Prefer a second opinion about health conditions and treatment options | 0.524 | 4.33 | 1.107 | 0.382 | 0.532 |
| F18 Perceived cancer risk (4 items) | ||||||
| R1d_RiskStomach | Perceive risk of stomach cancer | 0.895 | 2.75 | 0.967 | 0.833 | 0.842 |
| R1e_RiskLiver | Perceive risk of liver cancer | 0.891 | 2.72 | 0.990 | 0.828 | 0.834 |
| R1c_RiskColon | Perceive risk of colon cancer | 0.856 | 2.83 | 1.006 | 0.774 | 0.770 |
| R1f_RiskSkin | Perceive risk of skin cancer | 0.780 | 2.77 | 0.997 | 0.679 | 0.658 |
| F19 Worriedness about cancer (4 items) | ||||||
| R2d_WorryStomach | Being worried about having stomach cancer | 0.884 | 1.91 | 1.197 | 0.855 | 0.857 |
| R2e_WorryLiver | Being worried about having liver cancer | 0.882 | 1.87 | 1.188 | 0.858 | 0.854 |
| R2c_WorryColon | Being worried about having colon cancer | 0.853 | 2.07 | 1.235 | 0.810 | 0.800 |
| R2f_WorrySkin | Being worried about having skin cancer | 0.838 | 2.01 | 1.207 | 0.755 | 0.760 |
| F20 Symptomatic deterrents (4 items) | ||||||
| B2c_NoNeedNoSymptoms | No need to have cancer screenings if there are not symptoms | 0.836 | 2.68 | 1.594 | 0.807 | 0.827 |
| B2b_NoNeedNormalResults | No need to have cancer screenings after having several normal screening test results | 0.784 | 2.82 | 1.573 | 0.673 | 0.687 |
| B2a_NoNeedFeelHealthy | No need to have cancer screenings when feeling healthy | 0.773 | 2.45 | 1.592 | 0.740 | 0.743 |
| B2d_NoNeedAge | No need to have cancer screenings when being too young or too old | 0.697 | 2.13 | 1.421 | 0.581 | 0.631 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Echeverri, M.; Anderson, D.; Haas, J.M.; Johnson, M.E.; Serrano, F.S.A.; Nápoles, A.M. Testing the Preliminary Validity of a Multidimensional Framework for Studying the Effects of Cancer Health Literacy on Cancer Screening Behaviors among Diverse Populations. Int. J. Environ. Res. Public Health 2020, 17, 2987. https://doi.org/10.3390/ijerph17092987
Echeverri M, Anderson D, Haas JM, Johnson ME, Serrano FSA, Nápoles AM. Testing the Preliminary Validity of a Multidimensional Framework for Studying the Effects of Cancer Health Literacy on Cancer Screening Behaviors among Diverse Populations. International Journal of Environmental Research and Public Health. 2020; 17(9):2987. https://doi.org/10.3390/ijerph17092987
Chicago/Turabian StyleEcheverri, Margarita, David Anderson, Jacqueline M. Haas, Marc E. Johnson, Friar Sergio A. Serrano, and Anna María Nápoles. 2020. "Testing the Preliminary Validity of a Multidimensional Framework for Studying the Effects of Cancer Health Literacy on Cancer Screening Behaviors among Diverse Populations" International Journal of Environmental Research and Public Health 17, no. 9: 2987. https://doi.org/10.3390/ijerph17092987
APA StyleEcheverri, M., Anderson, D., Haas, J. M., Johnson, M. E., Serrano, F. S. A., & Nápoles, A. M. (2020). Testing the Preliminary Validity of a Multidimensional Framework for Studying the Effects of Cancer Health Literacy on Cancer Screening Behaviors among Diverse Populations. International Journal of Environmental Research and Public Health, 17(9), 2987. https://doi.org/10.3390/ijerph17092987





