The Impact of Non-optimum Ambient Temperature on Years of Life Lost: A Multi-county Observational Study in Hunan, China
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sites
2.2. Death Data Collection
2.3. Meteorological Interpolation Method
2.4. YLL Calculation
2.5. Statistical Analysis
Stage-1: Quantify the general effect of daily ambient temperature
Stage-2: Estimated overall cumulative exposure-response association
2.6. Sensitivity Analysis
3. Results
3.1. Characteristics for YLL and Meteorological Variables
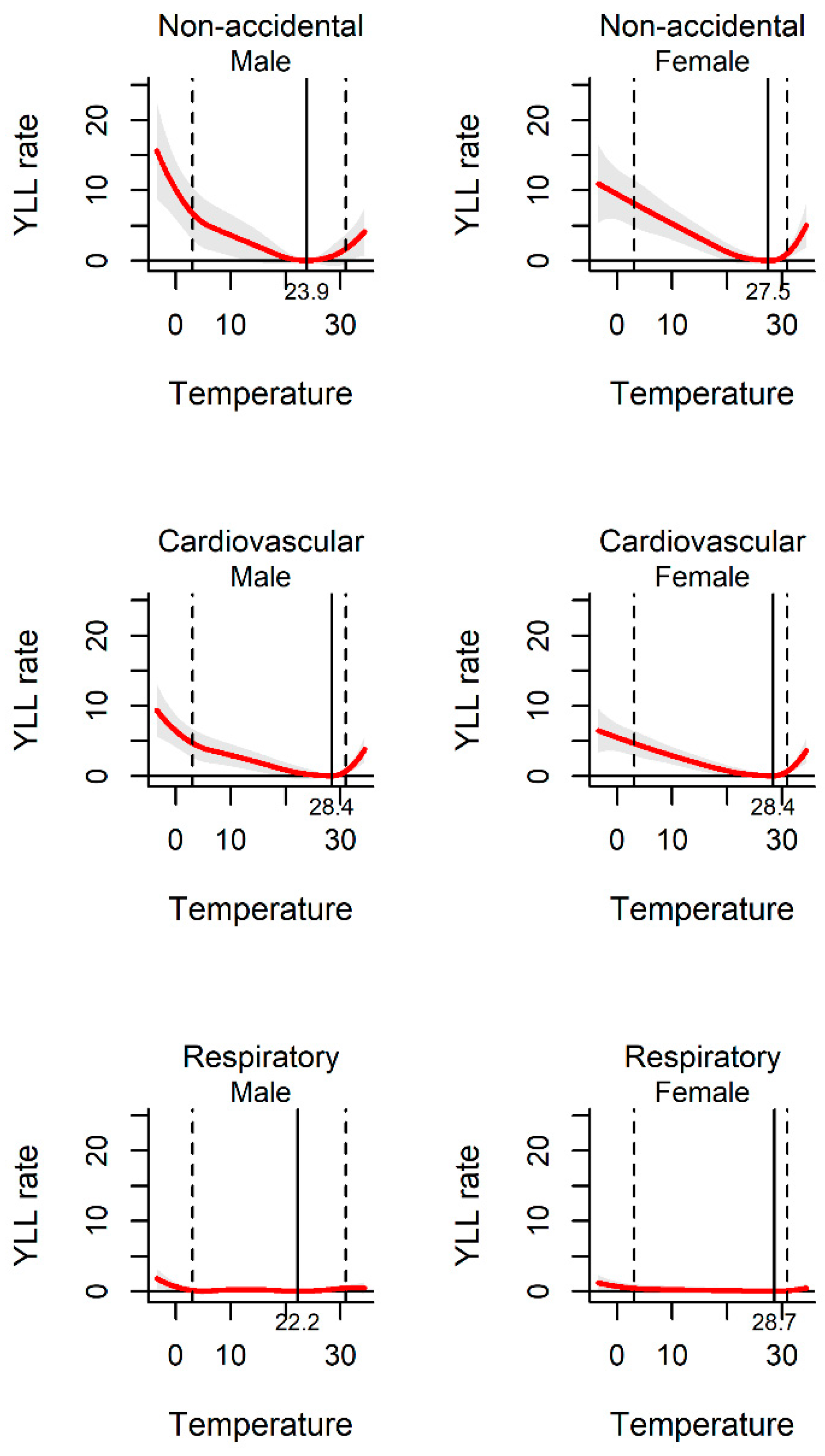
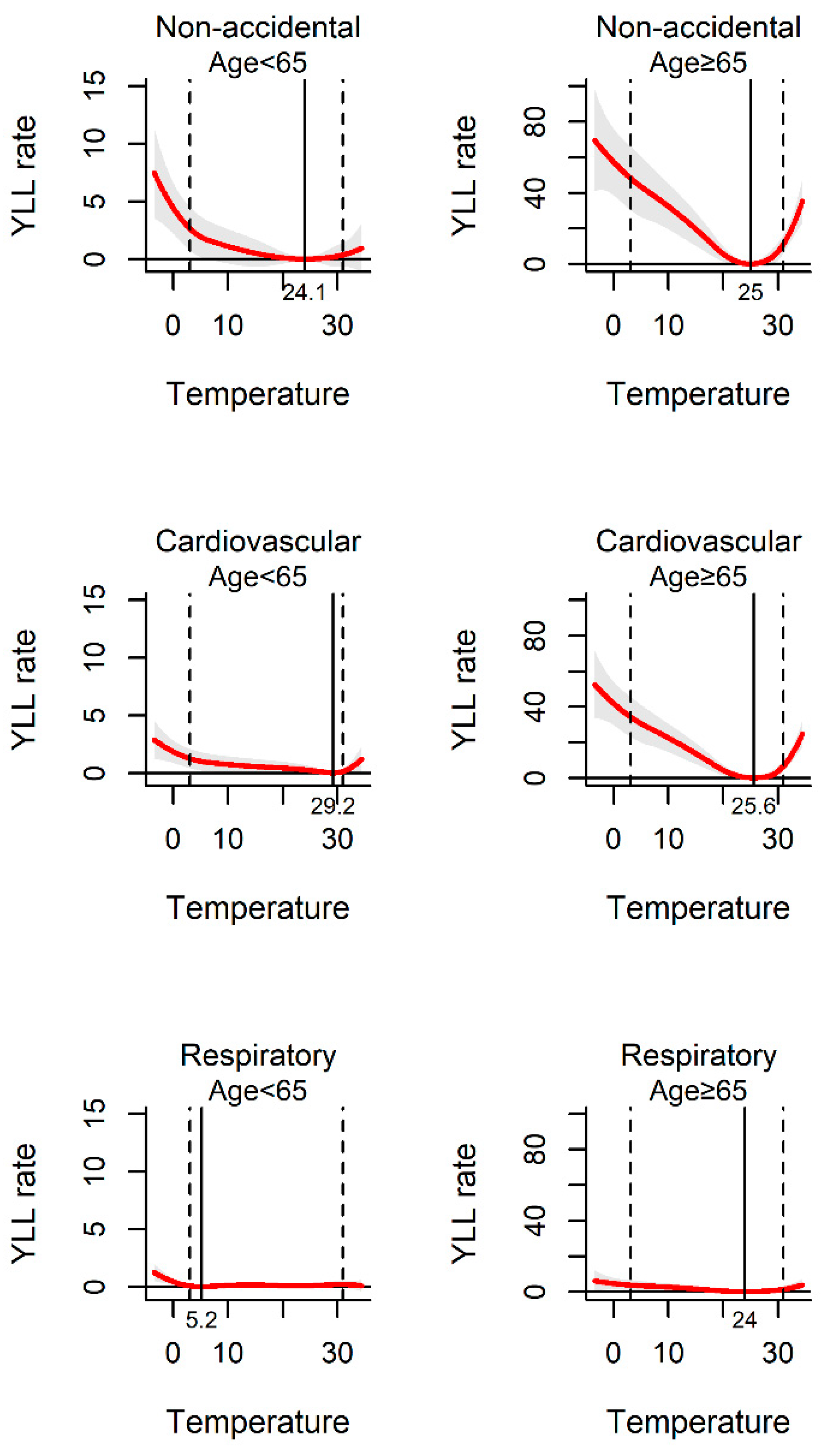
3.2. Association of Temperature and YLL
3.3. The Attributable Risk of Ambient Temperature on YLL
3.4. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| Df | Degree of freedom |
| AIC | Akaike’s Information Criterion |
References
- Pachauri, R.K.; Allen, M.R.; Barros, V.R.; Broome, J.; Cramer, W.; Christ, R.; Church, J.A.; Clarke, L.; Dahe, Q.; Dasgupta, P.; et al. Climate Change 2014: Synthesis Report. Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; IPCC World Meteorological Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Song, X.; Wang, S.; Hu, Y.; Yue, M.; Zhang, T.; Liu, Y.; Tian, J.; Shang, K. Impact of ambient temperature on morbidity and mortality: An overview of reviews. Sci. Total Env. 2017, 586, 241–254. [Google Scholar] [CrossRef] [PubMed]
- Mills, D.; Schwartz, J.; Lee, M.; Sarofim, M.; Jones, R.; Lawson, M.; Duckworth, M.; Deck, L. Climate change impacts on extreme temperature mortality in select metropolitan areas in the United States. Clim. Change. 2015, 131, 83–95. [Google Scholar] [CrossRef]
- Luan, G.; Yin, P.; Wang, L.; Zhou, M. The temperature-mortality relationship: An analysis from 31 Chinese provincial capital cities. Int. J. Environ. Health Res. 2018, 28, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Shafiei Shiva, J.; Chandler, D.G.; Kunkel, K.E. Localized Changes in Heat Wave Properties Across the United States. Earths Future 2019, 7, 300–319. [Google Scholar] [CrossRef]
- Curtis, S.; Fair, A.; Wistow, J.; Val, D.V.; Oven, K. Impact of extreme weather events and climate change for health and social care systems. Environ. Health 2017, 16, 128. [Google Scholar] [CrossRef]
- Perkins, S.E.; Alexander, L.V. On the measurement of heat waves. J. Clim. 2013, 26, 4500–4517. [Google Scholar] [CrossRef]
- Meehl, G.A.; Tebaldi, C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science 2004, 305, 994–997. [Google Scholar] [CrossRef]
- Chen, R.; Yin, P.; Wang, L.; Liu, C.; Niu, Y. Association between ambient temperature and mortality risk and burden: Time series study in 272 main Chinese cities. BMJ 2018, 363, 1–37. [Google Scholar] [CrossRef]
- Vardoulakis, S.; Dear, K.; Hajat, S.; Heaviside, C.; Eggen, B.; McMichael, A.J. Comparative assessment of the effects of climate change on heat-and cold-related mortality in the United Kingdom and Australia. Environ. Health Perspect. 2014, 122, 1285–1292. [Google Scholar] [CrossRef]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobias, A.; Tong, S.; Rocklöv, J.; Forsberg, B.; et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Fu, S.H.; Antonio, G.; Rodriguez, P.S.; Prabhat, J.; Madeleine, T. Mortality attributable to hot and cold ambient temperatures in India: A nationally representative case-crossover study. PLoS Med. 2018, 15, 1–35. [Google Scholar] [CrossRef] [PubMed]
- Joacim, R.V.; Bertil, F.; Kristie, E.; Tom, B. Susceptibility to mortality related to temperature and heat and cold wave duration in the population of Stockholm County, Sweden. Glob. Health Action 2014, 7, 1–11. [Google Scholar] [CrossRef]
- Li, Y.; Li, G.; Zeng, Q.; Liang, F.; Pan, X. Projecting temperature-related years of life lost under different climate change scenarios in one temperate megacity, China. Environ. Pollut. 2018, 233, 1068–1075. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Horton, R.M.; Bader, D.A.; Lesk, C.; Jiang, L.; Jones, B.; Zhou, L.; Chen, X.; Bi, J.; Kinney, P.L. Impact of climate change on heat-related mortality in Jiangsu Province, China. Environ. Pollut. 2017, 224, 317–325. [Google Scholar] [CrossRef]
- Odhiambo Sewe, M.; Bunker, A.; Ingole, V.; Egondi, T.; Oudin Åström, D.; Hondula, D.M.; Rocklöv, J.; Schumann, B. Estimated effect of temperature on years of life lost: A retrospective time-series study of low-, middle-, and high-income regions. Environ. Health Perspect. 2018, 126, 017004. [Google Scholar] [CrossRef]
- Li, G.; Li, Y.; Tian, L.; Guo, Q.; Pan, X. Future temperature-related years of life lost projections for cardiovascular disease in Tianjin, China. Sci. Total Environ. 2018, 630, 943–950. [Google Scholar] [CrossRef]
- Huang, C.; Barnett, A.G.; Wang, X.; Tong, S. The impact of temperature on years of life lost in Brisbane, Australia. Nat. Clim. Change 2012, 2, 265–270. [Google Scholar] [CrossRef]
- Hutchinson, M.F.; Xu, T. ANUSPLIN Version 4.4 User Guide; Fenner School of Environment and Society at the Australian National University: Canberra, Australia, 2013. [Google Scholar]
- Wang, Q. Economic impact of air pollution. Ph.D. Thesis, KU Leuven University, Tsinghua, China, May 2019. [Google Scholar]
- Gasparrini, A. Distributed lag linear and non-linear models in R: The package dlnm. J. Stat. Softw. 2011, 43, 1. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B. Reducing and meta-analysing estimates from distributed lag non-linear models. BMC Med. Res. Methodol. 2013, 13, 1. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, C.; Peng, M.; Zhang, L. The burden of ambient temperature on years of life lost: A multi-community analysis in Hubei, China. Sci. Total Environ. 2018, 621, 1491–1498. [Google Scholar] [CrossRef]
- Liu, T.; Ren, Z.; Zhang, Y.; Feng, B.; Lin, H.; Xiao, J.; Zeng, W.; Li, X.; Li, Z.; Rutherford, S. Modification effects of population expansion, ageing, and adaptation on heat-related mortality risks under different climate change scenarios in Guangzhou, China. Int. J. Environ. Res. Public Health 2019, 16, 376. [Google Scholar] [CrossRef] [PubMed]
- Luan, G.; Yin, P.; Li, T.; Wang, L.; Zhou, M. The years of life lost on cardiovascular disease attributable to ambient temperature in China. Sci. Rep. 2017, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Yao, Y.; Duan, Y.; Liao, Y.; Yan, S.; Liu, X.; Zhao, Z.; Fu, Y.; Yin, P.; Cheng, J. Years of life lost and mortality risk attributable to non-optimum temperature in Shenzhen: A time-series study. J. Expo. Sci. Environ. Epidemiol. 2020, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Mercer, J.B.; Østerud, B.; Tveita, T. The effect of short-term cold exposure on risk factors for cardiovascular disease. Thromb. Res. 1999, 95, 93–104. [Google Scholar] [CrossRef]
- Hong, Y.; Kim, H.; Oh, S.; Lim, Y.; Kim, S.; Yoon, H.; Park, M. Association of cold ambient temperature and cardiovascular markers. Sci. Total Environ. 2012, 435, 74–79. [Google Scholar] [CrossRef]
- Basu, R.; Samet, J.M. Relation between elevated ambient temperature and mortality: A review of the epidemiologic evidence. Epidemiol. Rev. 2002, 24, 190–202. [Google Scholar] [CrossRef]
- Wang, M.; Jiang, A.; Gong, L.; Luo, L.; Guo, W.; Li, C.; Zheng, J.; Li, C.; Yang, B.; Zeng, J.; et al. Temperature significant change COVID-19 Transmission in 429 cities. medRxiv 2020. medRxiv 2020.02.22.20025791. Available online: https://www.medrxiv.org/content/10.1101/2020.02.22.20025791v1 (accessed on 22 February 2020).
- Qiu, H.; Sun, S.; Tang, R.; Chan, K.P.; Tian, L. Pneumonia Hospitalization Risk in the Elderly Attributable to Cold and Hot Temperatures in Hong Kong, China. Am. J. Epidemiol. 2016, 8. [Google Scholar] [CrossRef]
- Chindapol, S.; Blair, J.; Osmond, P.; Prasad, D. A Suitable Thermal Stress Index for the Elderly in Summer Tropical Climates. Procedia Eng. 2017, 180, 932–943. [Google Scholar] [CrossRef]
- Yu, W.; Vaneckova, P.; Mengersen, K.; Pan, X.; Tong, S. Is the association between temperature and mortality modified by age, gender and socio-economic status? Sci. Total Environ. 2010, 408, 3513–3518. [Google Scholar] [CrossRef]


| Characteristics | Min | P2.5 | Median | Mean | P97.5 | Max | SD |
|---|---|---|---|---|---|---|---|
| Meteorological | |||||||
| Temperature (°C) | −3.52 | 10.41 | 18.55 | 17.74 | 24.74 | 34.49 | 8.30 |
| Relative humidity (%) | 30.72 | 70.51 | 78.88 | 77.80 | 86.11 | 100 | 10.99 |
| Non-accidental | 0 | 13.51 | 20.64 | 22.62 | 29.29 | 343.63 | 13.41 |
| Gender | |||||||
| Male | 0 | 13.91 | 23.41 | 26.44 | 35.33 | 405.63 | 18.18 |
| Female | 0 | 8.14 | 15.77 | 18.61 | 25.64 | 297.33 | 14.78 |
| Age | |||||||
| <65 | 0 | 4.89 | 10.29 | 12.24 | 17.39 | 257.57 | 10.51 |
| ≥65 | 0 | 66.05 | 102.40 | 113.55 | 147.15 | 2428.45 | 72.20 |
| Cardiovascular | 0 | 5.00 | 8.82 | 10.14 | 13.65 | 225.50 | 7.48 |
| Gender | |||||||
| Male | 0 | 4.19 | 9.35 | 11.41 | 16.12 | 255.20 | 10.21 |
| Female | 0 | 2.72 | 6.92 | 8.80 | 12.63 | 194.19 | 8.52 |
| Age | |||||||
| <65 | 0 | 0 | 2.66 | 4.05 | 6.49 | 122.79 | 5.34 |
| ≥65 | 0 | 31.09 | 54.96 | 63.63 | 85.63 | 1760.64 | 48.90 |
| Subtypes | |||||||
| Hypertension | 0 | 0 | 1.89 | 2.93 | 4.43 | 100.22 | 3.57 |
| Cerebrovascular | 0 | 0 | 2.58 | 3.67 | 5.44 | 113.41 | 4.16 |
| Hemorrhagic stroke | 0 | 0 | 0 | 1.61 | 2.37 | 56.53 | 2.81 |
| Ischemic heart stroke | 0 | 0 | 0 | 0.83 | 1.10 | 100.16 | 1.72 |
| Respiratory | 0 | 0 | 1.35 | 2.33 | 3.38 | 65.45 | 3.23 |
| Gender | |||||||
| Male | 0 | 0 | 0 | 2.80 | 4.12 | 105.64 | 4.67 |
| Female | 0 | 0 | 0 | 1.84 | 2.57 | 104.59 | 3.82 |
| Age | |||||||
| <65 | 0 | 0 | 0 | 0.76 | 0 | 58.36 | 2.47 |
| ≥65 | 0 | 0 | 9.49 | 15.75 | 24.40 | 488.11 | 20.80 |
| Subtype | |||||||
| COPD | 0 | 0 | 0 | 0.58 | 0 | 24.15 | 1.39 |
| Disease Death | Total (%) | Cold (%) | Heat (%) | Extreme Cold (%) | Moderate Cold (%) | Moderate Heat (%) | Extreme Heat (%) |
|---|---|---|---|---|---|---|---|
| Non-accidental | 10.73 (4.36–17.09) | 10.27 (4.52–16.03) | 0.45 (−0.16–1.06) | 1.02 (0.64–1.39) | 9.26 (3.87–14.64) | 0.22 (−0.23–0.68) | 0.23 (0.08–0.38) |
| Gender | |||||||
| Male | 7.64 (0.71–14.57) | 6.99 (1.21–12.76) | 0.65 (−0.50–1.81) | 0.83 (0.45–1.21) | 6.16 (0.76–11.55) | 0.44 (−0.50–1.38) | 0.22 (0–0.43) |
| Female | 14.99 (6.77–23.21) | 14.59 (6.75–22.43) | 0.39 (0.01–0.77) | 1.20 (0.73–1.68) | 13.39 (6.03–20.76) | 0.14 (−0.09–0.36) | 0.26 (0.10–0.41) |
| Age | |||||||
| <65 | 5.23 (−2.47–12.92) | 4.93 (−1.53–11.39) | 0.30 (−0.94–1.54) | 0.77 (0.34–1.19) | 4.16 (−1.87–10.19) | 0.20 (−0.79–1.18) | 0.10 (−0.15–0.35) |
| ≥65 | 14.92 (8.16–21.68) | 14.06 (7.95–20.17) | 0.86 (0.21–1.52) | 1.19 (0.78–1.60) | 12.87 (7.17–18.57) | 0.50 (−0.03–1.02) | 0.37 (0.24–0.50) |
| Cardiovascular | 16.44 (9.09–23.79) | 15.94 (8.82–23.05) | 0.50 (0.26–0.73) | 1.39 (0.99–1.79) | 14.55 (7.83–21.27) | 0.15 (0.05–0.26) | 0.35 (0.22–0.48) |
| Gender | |||||||
| Male | 14.41 (4.59–24.23) | 13.97 (4.44–23.5) | 0.44 (0.15–0.73) | 1.26 (0.78–1.75) | 12.71 (3.67–21.76) | 0.14 (0–0.27) | 0.30 (0.15–0.45) |
| Female | 17.90 (7.92–27.88) | 17.35 (7.67–27.04) | 0.54 (0.25–0.84) | 1.47 (0.92–2.01) | 15.89 (6.75–25.03) | 0.17 (0.05–0.29) | 0.37 (0.20–0.55) |
| Age | |||||||
| <65 | 12.45 (−0.63–25.52) | 12.16 (−0.56–24.89) | 0.28 (−0.07–0.63) | 1.00 (0.42–1.58) | 11.16 (−0.99–23.31) | 0.06 (−0.05–0.16) | 0.23 (−0.02–0.48) |
| ≥65 | 18.54 (10.93–26.15) | 17.70 (10.73–24.67) | 0.84 (0.20–1.47) | 1.53 (1.06–2.00) | 16.17 (9.66–22.67) | 0.42 (−0.08–0.91) | 0.42 (0.28–0.56) |
| Respiratory | 5.47 (−2.65–13.60) | 4.31 (−1.75–10.37) | 1.16 (−0.91–3.22) | 0.56 (0.11–1.01) | 3.75 (−1.86–9.37) | 0.86 (−0.85–2.56) | 0.30 (−0.05–0.66) |
| Gender | |||||||
| Male | 5.41 (−4.20–15.01) | 3.28 (−3.43–10.00) | 2.12 (−0.76–5.01) | 0.40 (−0.11–0.90) | 2.88 (−3.33–9.10) | 1.72 (−0.72–4.16) | 0.40 (−0.04–0.85) |
| Female | 7.48 (−11.65–26.61) | 7.19 (−11.46–25.84) | 0.29 (−0.19–0.77) | 0.79 (−0.09–1.67) | 6.40 (−11.37–24.17) | 0.08 (−0.10–0.26) | 0.21 (−0.09–0.52) |
| Age | |||||||
| <65 | 15.40 (−7.68–38.48) | 1.12 (0.34–1.89) | 14.28 (−8.02–36.58) | 1.01 (0.36–1.65) | 0.11 (−0.02–0.24) | 13.69 (−7.49–34.87) | 0.59 (−0.53–1.72) |
| ≥65 | 8.77 (0.39–17.15) | 7.91 (1.16–14.65) | 0.86 (−0.77–2.50) | 0.68 (0.20–1.16) | 7.23 (0.97–13.49) | 0.55 (−0.76–1.87) | 0.31 (−0.01–0.63) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lv, L.-S.; Jin, D.-H.; Ma, W.-J.; Liu, T.; Xu, Y.-Q.; Zhang, X.-E.; Zhou, C.-L. The Impact of Non-optimum Ambient Temperature on Years of Life Lost: A Multi-county Observational Study in Hunan, China. Int. J. Environ. Res. Public Health 2020, 17, 2699. https://doi.org/10.3390/ijerph17082699
Lv L-S, Jin D-H, Ma W-J, Liu T, Xu Y-Q, Zhang X-E, Zhou C-L. The Impact of Non-optimum Ambient Temperature on Years of Life Lost: A Multi-county Observational Study in Hunan, China. International Journal of Environmental Research and Public Health. 2020; 17(8):2699. https://doi.org/10.3390/ijerph17082699
Chicago/Turabian StyleLv, Ling-Shuang, Dong-Hui Jin, Wen-Jun Ma, Tao Liu, Yi-Qing Xu, Xing-E Zhang, and Chun-Liang Zhou. 2020. "The Impact of Non-optimum Ambient Temperature on Years of Life Lost: A Multi-county Observational Study in Hunan, China" International Journal of Environmental Research and Public Health 17, no. 8: 2699. https://doi.org/10.3390/ijerph17082699
APA StyleLv, L.-S., Jin, D.-H., Ma, W.-J., Liu, T., Xu, Y.-Q., Zhang, X.-E., & Zhou, C.-L. (2020). The Impact of Non-optimum Ambient Temperature on Years of Life Lost: A Multi-county Observational Study in Hunan, China. International Journal of Environmental Research and Public Health, 17(8), 2699. https://doi.org/10.3390/ijerph17082699






