The Being Taken Seriously Questionnaire—Development and Psychometric Evaluation of a PREM Measure for Person-Centeredness in a High-Tech Hospital Environment
Abstract
1. Introduction
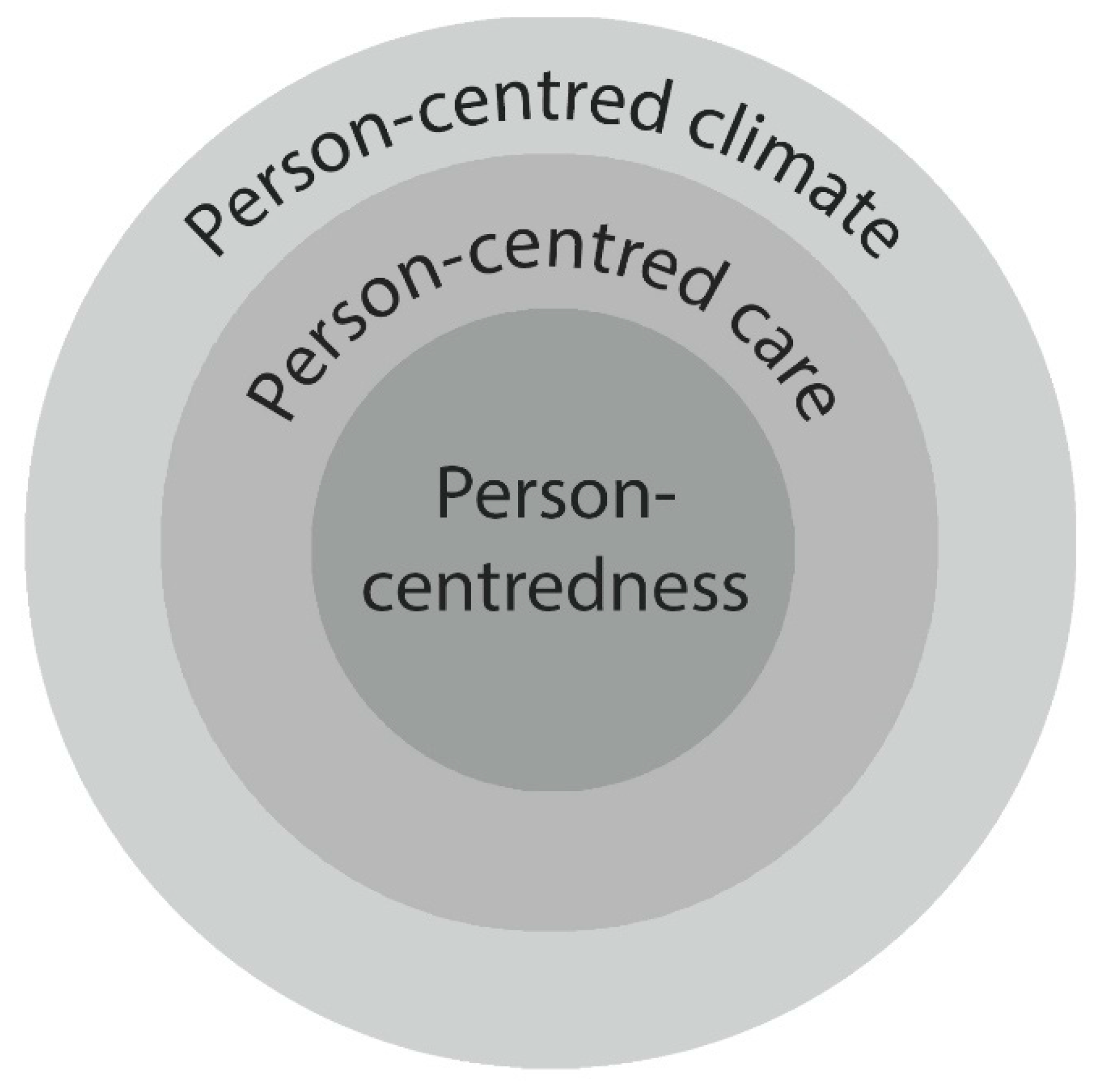
Framework
- Prerequisites: The professionals must adopt characteristics such as professional conduct and interpersonal interaction skills. They must be engaged and aware of their own behavior.
- The care environment: The context where the care takes place should involve a structure that supports shared power and decision making between the patient and the professionals. Different competencies are valued and there is an innovative atmosphere that encourages the testing of new strategies.
- Person-centered processes: The caring actions stem from patients’ values and engagement. The professionals are close to the patients, not only satisfying basic needs, but working with shared decision making.
- Outcomes: These include satisfaction with the care, participation, sense of well-being and the aim of creating a safe environment involving hospitality. In order to enable these outcomes, professional characteristics must be evident along with a context that supports person-centeredness.
2. Materials and Methods
2.1. Setting
2.2. Participants and Procedures
2.3. The Instruments
2.3.1. The Being Taken Seriously Questionnaire—Patient Version (BTSQ-P)
- The staff listened to me,
- I received help to understand what has happened,
- I received help to understand what is about to happen,
- My concerns have been taken seriously,
- My symptoms have been taken seriously,
- I have been taken seriously as a person,
- The staff made me feel good in the present moment, and
- The staff made me feel safe.
2.3.2. The Person-Centered Climate Questionnaire—Patient Version (PCQ-P)
2.4. Data Analysis
- A principal component analysis,
- A parallel analysis based on minimum rank factor analysis [18],
- An exploratory factor analysis,
- Exploring relationships between the BTSQ-P and PCQ-P by means of Spearman’s correlation,
- Standard multiple regression.
2.5. Ethical Considerations
3. Results
3.1. Construct Validity and Reliability
3.2. Descriptive Statistics and Correlations
3.3. Possible Explanatory Factors
4. Discussion
4.1. Discussions of the Findings
4.2. Methodological Considerations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ekman, I.; Swedberg, K.; Taft, C.; Lindseth, A.; Norberg, A.; Brink, E.; Carlsson, J.; Dahlin-Ivanoff, S.; Johansson, I.L.; Kjellgren, K.; et al. Person-centered care—Ready for prime time. Eur. J. Cardiovasc. Nurs. 2011, 10, 248–251. [Google Scholar] [CrossRef] [PubMed]
- DiLollo, A.; Favreau, C. Person-centered care and speech and language therapy. Semin. Speech Lang. 2010, 31, 90–97. [Google Scholar] [CrossRef] [PubMed]
- McCormack, B.; McCance, T. Person-Centered Nursing. Theory and Practice; Wiley-Blackwell: Oxford, UK, 2010. [Google Scholar]
- McCormack, B.; McCance, T.V. Development of a framework for person-centred nursing. J. Adv. Nurs. 2006, 56, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Edvardsson, D.; Sandman, P.O.; Rasmussen, B. Swedish language Person-centred Climate Questionnaire—Patient version: Construction and psychometric evaluation. J. Adv. Nurs. 2008, 63, 302–309. [Google Scholar] [CrossRef]
- Kristensson Uggla, B. Personfilosofi-Filosofiska Utgångspunkter för Personcentrering Inom Hälso-Och Sjukvård [Personal Philosophy-Filosophical Starting Points for Person-Centeredness in Health Care]. In Person-Centeredness in Health Care. From Philosophy to Practice [Personcentrering inom Hälso-Och Sjukvård. Från Filosofi Till Praktik; Ekman, I., Ed.; Liber: Stockholm, Sweden, 2014. [Google Scholar]
- Lützén, K. We may know? What’person-centred care in nursing is and? Why’, but what about the? how to’? Nord. J. Nur. Res. 2015, 35, 131. [Google Scholar] [CrossRef]
- Brooker, D.; Latham, I. Person-Centred Dementia Care: Making Services Better with the VIPS Framework; Jessica Kingsley Publishers, Ltd.: London, UK, 2015. [Google Scholar]
- Edvardsson, J.D.; Sandman, P.O.; Rasmussen, B.H. Sensing an atmosphere of ease: A tentative theory of supportive care settings. Scand. J. Caring Sci. 2005, 19, 344–353. [Google Scholar] [CrossRef]
- Rantala, A.; Forsberg, A.; Ekwall, A. Person-centred climate and psychometrical exploration of person-centredness and among patients not conveyed by the Ambulance Care Service. Scand. J. Caring Sci. 2018, 32, 852–860. [Google Scholar] [CrossRef]
- McCormack, B.; Karlsson, B.; Dewing, J.; Lerdal, A. Exploring person-centredness: A qualitative meta-synthesis of four studies. Scand. J. Caring Sci. 2010, 24, 620–634. [Google Scholar] [CrossRef]
- Rantala, A.; Ekwall, A.; Forsberg, A. Significant others’ perceptions of being taken seriously by the Swedish Ambulance Service when the patient is assessed as nonurgent. Scand. J. Caring Sci. 2019. [Google Scholar] [CrossRef]
- Rantala, A.; Ekwall, A.; Forsberg, A. The meaning of being triaged to non-emergency ambulance care as experienced by patients. Int. Emerg. Nurs. 2016, 25, 65–70. [Google Scholar] [CrossRef]
- Wijk, H. Personcentrerad Utformning av Vårdmiljön. In Vårdmiljöns Betydelse; Wijk, H., Ed.; Studentlitteratur: Lund, Sweden, 2014. [Google Scholar]
- Almerud, S.; Alapack, R.J.; Fridlund, B.; Ekebergh, M. Of vigilance and invisibility—Being a patient in technologically intense environments. Nurs. Crit. Care 2007, 12, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Suhr, D.D. Exploratory or Confirmatory Factor Analysis; SAS Institute Inc.: Cary, CN, USA, 2006. [Google Scholar]
- Barrett, P.T.; Kline, P. The observation to variable ratio in factor analysis. Personal. Study Group Behav. 1981, 1, 23–33. [Google Scholar]
- Timmerman, M.E.; Lorenzo-Seva, U. Dimensionality assessment of ordered polytomous items with parallel analysis. Psychol. Methods 2011, 16, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Streiner, D.L.; Norman, G.R.; Cairney, J. Health Measurement Scales: A practical Guide to Their Development and Use; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Gadermann, A.M.; Guhn, M.; Zumbo, B.D. Estimating ordinal reliability for Likert-type and ordinal item response data: A conceptual, empirical, and practical guide. Pract. Assess. Res. Eval. 2012, 17, 3. [Google Scholar]
- Nunnally, J.; Bernstein, I. Psychometric Theory, 3rd ed.; McGraw-Hill Inc.: New York, NY, USA, 1994. [Google Scholar]
- World Medical, A. World Medical Association Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Mardia, K.V. Measures of multivariate skewness and kurtosis with applications. Biometrika 1970, 57, 519–530. [Google Scholar] [CrossRef]
- Nilsson, E.; Kristenson, M. Att fråga patienten hur hen mår—Ett sätt att lära och leda vårdens insatser mot hälsa [To ask the patient about his or her wellbeing-a way to learn and lead the interventions towards health]. Socialmedicinsk Tidskrift 2017, 94, 237–244. [Google Scholar]
- Chen, J.; Ou, L.; Hollis, S.J. A systematic review of the impact of routine collection of patient reported outcome measures on patients, providers and health organisations in an oncologic setting. BMC Health Serv. Res. 2013, 13, 211. [Google Scholar] [CrossRef]
- Lungu, D.A.; Pennucci, F.; De Rosis, S.; Romano, G.; Melfi, F. Implementing successful systematic Patient Reported Outcome and Experience Measures (PROMs and PREMs) in robotic oncological surgery—The role of physicians. Int. J. Health Plan. Manag. 2019. [Google Scholar] [CrossRef]
- Murante, A.M.; Vainieri, M.; Rojas, D.; Nuti, S. Does feedback influence patient-professional communication? Empirical evidence from Italy. Health Policy 2014, 116, 273–280. [Google Scholar] [CrossRef]
- Nilsson, E.; Wenemark, M.; Bendtsen, P.; Kristenson, M. Respondent satisfaction regarding SF-36 and EQ-5D, and patients’ perspectives concerning health outcome assessment within routine health care. Qual. Life Res. 2007, 16, 1647–1654. [Google Scholar] [CrossRef]
- Aaronson, N.; Alonso, J.; Burnam, A.; Lohr, K.N.; Patrick, D.L.; Perrin, E.; Stein, R.E. Assessing health status and quality-of-life instruments: Attributes and review criteria. Qual. Life Res. 2002, 11, 193–205. [Google Scholar] [CrossRef]
- Andresen, E.M. Criteria for assessing the tools of disability outcomes research. Arch. Phys. Med. Rehabil. 2000, 81, S15–S20. [Google Scholar] [CrossRef]
- Fitzpatrick, P. Evaluating patient-based outcome measures for use in clinical trials. Health Technol. Assess. 1998, 2, 1–74. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef]
| Step | Task * | Performance |
|---|---|---|
| 1 | Specificying measurment goals | The BTSQ-P was developed for adult persons undergoing health care. They should be able to read and write Swedish or any other language into which the instrument is translated. The primary purpose of the instrument is to be discriminative and evaluative, serving as a generic patient-reported experience measures (PREMs). The instrument is supposed to be self-administered, but is also suitable for telephone interviews. |
| 2 | Item generation | The item pool was chosen from open-ended, in-depth interviews (as described by Rantala, Ekwall and Forsberg [13]), review of the specific literature on person-centered care and discussions with health care professionals. |
| 3 | Item reduction | No item reduction was performed. The original eight items were retained. |
| 4 | Questionnaire formatting | Words were used that apply to the widest range of cultures and geographic areas in order to facilitate translation and widespread use. Each response relates to the perceived importance of the BTSQ-P construct on a 6-point Likert-type scale ranging from complete disagreement (1) to complete agreement (6). |
| 5 | Pretesting | A small pretest (as part of the face validity assessment) was performed involving five thoracic patients. |
| 6 | Reliability | Scale reliability was estimated using the ordinal alpha as well as Cronbach’s alpha. Reliability will be further tested in future research. |
| 7 | Validity | The content validity was assessed in two ways: comparison with the literature on person-centeredness and consultation with an expert group comprising two senior nurse researchers (with experience of scale development) and two clinical specialist nurses with specific interest in and knowledge of PCC. They were asked to assess the relevance, clarity and readability of the items. The experts considered the content validity good and that the items reflect what the literature describes as central aspects of person-centeredness. In addition, a content validity index was evaluated by eight patients and found satisfactory, in terms of the relevance, clarity and readability of the items. Construct validity was determined by the confirmatory multi-trait analysis program and by explorative principal component analysis (with oblique, varimax rotation) as well as by examining the relation between the BTSQ-P and the generic Person-Centered Climate Questionnaire (PCQ-P) instrument. |
| 8 | Interpretability | We use the so-called anchor-based approach, where the changes in BTSQ-P measures are compared or anchored to other clinically meaningful outcomes. This will be tested further. |
| Min. Score | Max. Score | |
|---|---|---|
| PCQ-P, the whole instrument | 17 | 102 |
| A climate of safety (items 1–10) | 10 | 60 |
| A climate of everydayness (items 11–14) | 4 | 24 |
| A climate of hospitality (items 15–17) | 3 | 18 |
| Items | Factor Loadings PCA | Factor Loadings EFA |
|---|---|---|
| The staff listened to me | 0.697 | 0.802 |
| I received help to understand what has happened | 0.684 | 0.806 |
| I received help to understand what is about to happen | 0.718 | 0.821 |
| My concerns have been taken seriously | 0.731 | 0.863 |
| My symptoms have been taken seriously | 0.801 | 0.908 |
| I have been taken seriously as a person | 0.806 | 0.875 |
| The staff made me feel good in the present moment | 0.759 | 0.870 |
| The staff made me feel safe | 0.636 | 0.759 |
| Independent Variable | B | Beta | t | p |
|---|---|---|---|---|
| Climate of safety | 0.383 | 0.554 | 4.793 | ≤0.001 |
| Climate of everydayness | 0.252 | 0.242 | 1.986 | 0.051 |
| Climate of hospitality | −0.085 | 0.048 | −0.354 | 0.724 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Forsberg, A.; Rantala, A. The Being Taken Seriously Questionnaire—Development and Psychometric Evaluation of a PREM Measure for Person-Centeredness in a High-Tech Hospital Environment. Int. J. Environ. Res. Public Health 2020, 17, 2660. https://doi.org/10.3390/ijerph17082660
Forsberg A, Rantala A. The Being Taken Seriously Questionnaire—Development and Psychometric Evaluation of a PREM Measure for Person-Centeredness in a High-Tech Hospital Environment. International Journal of Environmental Research and Public Health. 2020; 17(8):2660. https://doi.org/10.3390/ijerph17082660
Chicago/Turabian StyleForsberg, Anna, and Andreas Rantala. 2020. "The Being Taken Seriously Questionnaire—Development and Psychometric Evaluation of a PREM Measure for Person-Centeredness in a High-Tech Hospital Environment" International Journal of Environmental Research and Public Health 17, no. 8: 2660. https://doi.org/10.3390/ijerph17082660
APA StyleForsberg, A., & Rantala, A. (2020). The Being Taken Seriously Questionnaire—Development and Psychometric Evaluation of a PREM Measure for Person-Centeredness in a High-Tech Hospital Environment. International Journal of Environmental Research and Public Health, 17(8), 2660. https://doi.org/10.3390/ijerph17082660





