Sex Differences in Cardiovascular Disease Risk by Socioeconomic Status (SES) of Workers Using National Health Information Database
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
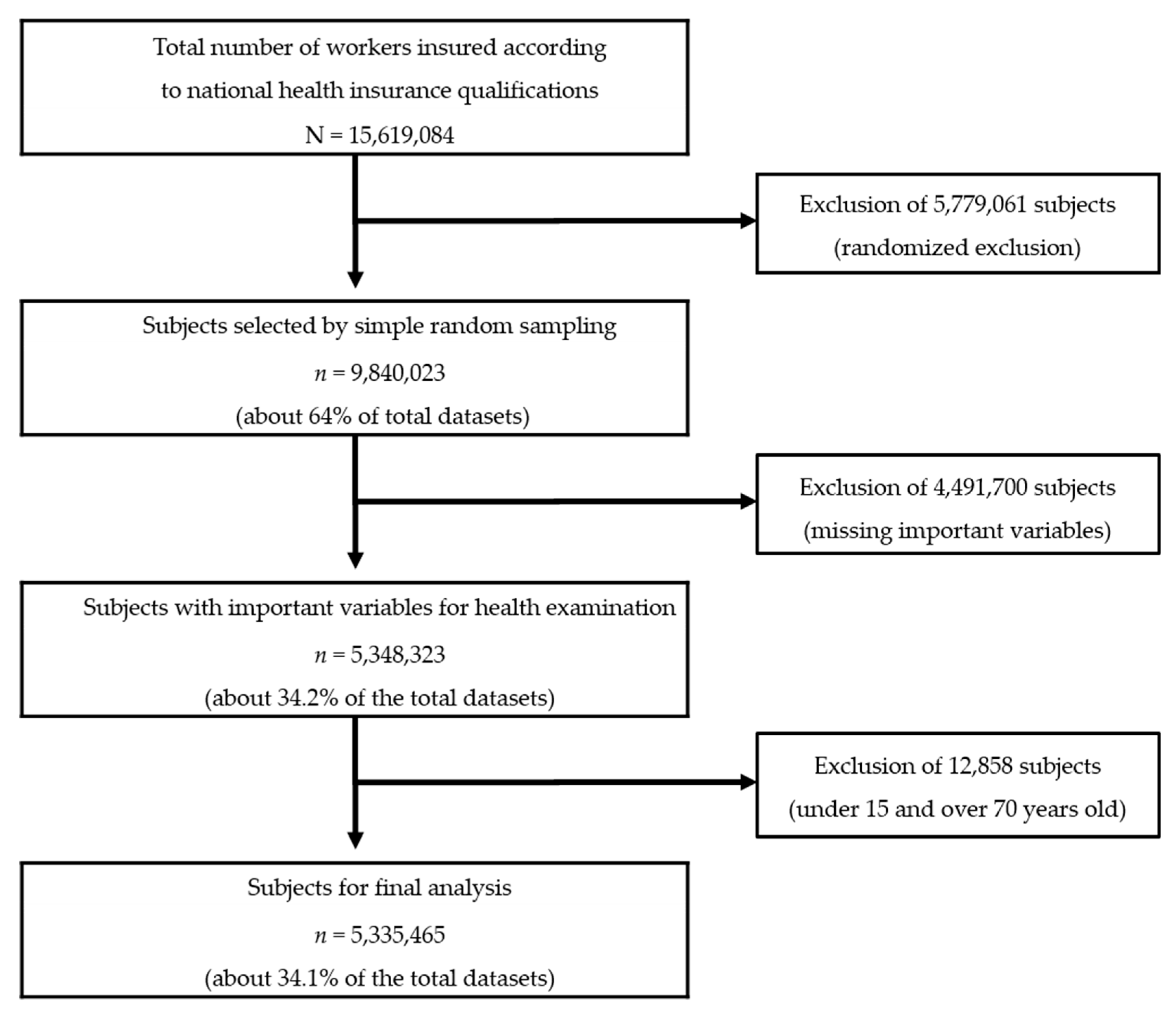
2.2. Study Population and Design
2.3. General Characteristics and Socioeconomic Status
2.4. Health Behaviors
2.5. CVD-Related Health Status
2.6. Statistical Analysis
3. Results
3.1. Socioeconomic Status by Gender
3.2. Health Behavior by Age, Income, and Residential Area
3.3. CVD-Related Health Status by Age, Income, and Residential Area
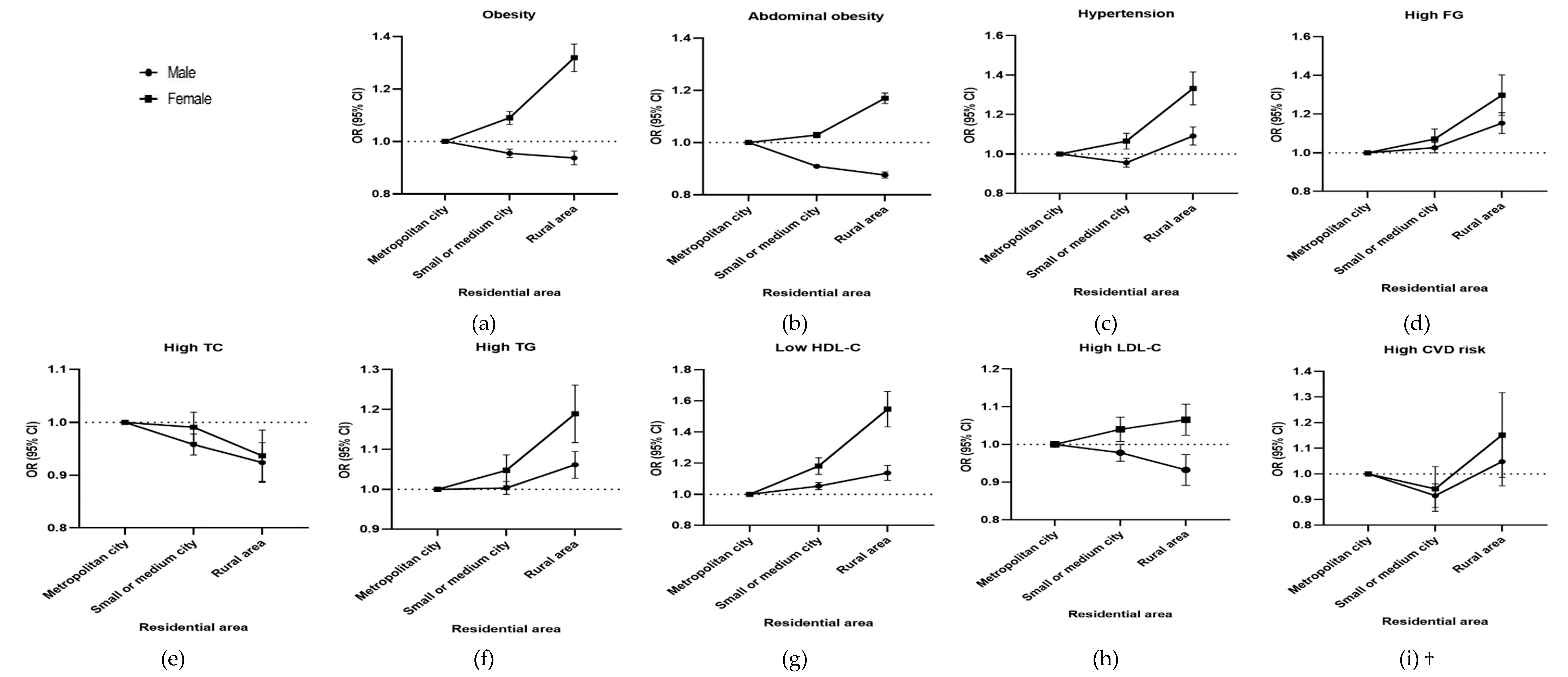
3.4. Odds Ratio of CVD-Related Health Status by Income and Residential Area
3.5. Factors Influencing CVD Risk
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Statistics Korea. December 2018 Employment Trends; Statistics Korea: Daejeon, Korea, 2019. [Google Scholar]
- National Health Insurance Service. National Health and Nutritional Survey Data; National Health Insurance Service: Wonju, Korea, 2016.
- Tabák, A.G.; Herder, C.; Rathmann, W.; Brunner, E.J.; Kivimäki, M. Prediabetes: A high-risk state for diabetes development. Lancet 2012, 379, 2279–2290. [Google Scholar] [CrossRef]
- World Health Organization. Available online: http://www.who.int/news-room/fact-sheets/ detail/the-top-10-causes-of-death (accessed on 19 September 2019).
- Ministry of Employment and Labor. Analysis of Industrial Accident Status 2018; Ministry of Employment and Labor: Sejong, Korea, 2019; p. 556.
- Konradi, A.O.; Rotar, O.P.; Korostovtseva, L.S.; Ivanenko, V.V.; Solntcev, V.N.; Anokhin, S.B.; Bart, A.V.; Shlyakhto, E.V. Prevalence of metabolic syndrome components in a population of bank employees from St. Petersburg, Russia. Metab. Syndr. Relat. Disord. 2011, 9, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.C.; Song, Y.H.; Rhee, S.Y.; Woo, J.T. Framingham risk scores by occupational group: Based on the 3rd Korean National Health and Nutrition Examination Survey. Korean J. Occup. Environ. Med. 2009, 21, 63–75. [Google Scholar] [CrossRef]
- Ali, M.K.; Bhaskarapillai, B.; Shivashankar, R.; Mohan, D.; Fatmi, Z.A.; Pradeepa, R.; Kadir, M.M.; Mohan, V.; Tandon, N.; Narayan, K.M.V.; et al. Socioeconomic status and cardiovascular risk in urban South Asia: The CARRS Study. Eur. J. Prev. Cardiol. 2016, 23, 408–419. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Xu, H.; Song, F.; Xu, W.; Pallard-Borg, S.; Qi, X. Relation of socioeconomic status to overweight and obesity: A large population-based study of Chinese adults. Ann. Hum. Biol. 2017, 44, 495–501. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, A.; Wellenius, G. Rural–urban disparities in the prevalence of diabetes and coronary heart disease. Public Health 2012, 126, 813–820. [Google Scholar] [CrossRef]
- Gamlath, L.; Nandasena, S.; Hennadige Padmal de Silva, S.; Linhart, C.; Ngo, A.; Morrell, S.; Nathan, S.; Sharpe, A.; Taylor, R. Differentials in cardiovascular risk factors and diabetes by socioeconomic status and sex in Kalutara, Sri Lanka. Asia Pac. J. Public Health 2017, 29, 401–410. [Google Scholar] [CrossRef]
- Kim, B.Y.; Lee, E.S. Relationship between Alcohol Drinking Patterns and Obesity and Abdominal Obesity in Korean Adult Men. J. Korean Public Health Nurs. 2017, 31, 478–491. [Google Scholar] [CrossRef]
- Jeong, H.S. Korea’s National Health Insurance—lessons from the past three decades. Health Aff. 2011, 30, 136–144. [Google Scholar] [CrossRef]
- National Health Insurance Service and Health Insurance Reviw & Assessmet Service. 2017 National Health Insurance Statistical Yearbook National Health Insurance Service; Health Insurance Review & Assessment Service: Seoul, Korea, 2018. [Google Scholar]
- Lee, Y.H.; Han, K.; Ko, S.H.; Ko, K.S.; Lee, K.U. Data analytic process of a nationwide population-based study using national health information database established by National Health Insurance Service. Diabetes Metab. J. 2016, 40, 79–82. [Google Scholar] [CrossRef]
- National Health Insurance Sharing Service. Available online: http://Nhiss.nhis.or.kr/ bd/ay/bdaya001iv.do (accessed on 28 September 2019).
- Park, H.H.; Chun, I.A.; Ryu, S.Y.; Park, J.; Han, M.A.; Chio, S.W.; Shin, J.H. Social Disparities in Utilization of Preventive Health Services among Korean Women Aged 40–64. J. Health Inf. Stat. 2016, 41, 369–378. [Google Scholar] [CrossRef]
- National Health Insurance Service. Available online: http://www.nhis.or.kr (accessed on 28 September 2019).
- Waskiewicz, A.; Sygnowska, E. Alcohol intake and cardiovascular risk factor profile in men participating in the WOBASZ study. Kardiol. Pol. 2013, 71, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Ryu, H.; Moon, J.; Jung, J. Influence of health behaviors and occupational stress on prediabetic state among male office workers. Int. J. Environ. Res. Public Health 2018, 15, 1264. [Google Scholar] [CrossRef] [PubMed]
- World Halth Organization. The Asia-Pacific Perspective: Redefining Obesity and its Treatment; Health Communications Australia: Sydney, Australia, 2000; pp. 17–20. [Google Scholar]
- Choi, C.J.; Seo, M.; Choi, W.S.; Kim, K.S.; Youn, S.A.; Lindsey, T.; Choi, Y.J.; Kim, C.M. Relationship between serum 25-hydroxyvitamin D and lung function among Korean adults in Korea National Health and Nutrition Examination Survey (KNHANES), 2008–2010. J. Clin. Endocrinol. Metab. 2013, 98, 1703–1710. [Google Scholar] [CrossRef]
- Lee, S.; Park, H.S.; Kim, S.M.; Kwon, H.S.; Kim, D.Y.; Kim, D.J.; Cho, G.J.; Han, J.H.; Kim, S.R.; Park, C.Y.; et al. Cut-off points of waist circumference for defining abdominal obesity in the Korean population. Korean J. Obes. 2006, 15, 1–9. [Google Scholar]
- Lee, H.Y. New definition for hypertension. J. Korean Med. Assoc. 2018, 61, 485–492. [Google Scholar] [CrossRef]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014, 33, S81–S90. [Google Scholar] [CrossRef]
- National Cholesterol Education Program. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Im, E.; Kim, G.S. Relationship between sleep duration and Framingham cardiovascular risk score and prevalence of cardiovascular disease in Koreans. Medicine 2017, 96, e7744. [Google Scholar] [CrossRef]
- Hu, G.; Tuomilehto, J.; Borodulin, K.; Jousilahti, P. The joint associations of occupational, commuting, and leisure-time physical activity, and the Framingham risk score on the 10-year risk of coronary heart disease. Eur. Heart J. 2007, 28, 492–498. [Google Scholar] [CrossRef]
- Korean Diabetes Association. Diabetes Fact Sheet in Korea 2018; Korean Diabetes Association: Seoul, Korea, 2018. [Google Scholar]
- Korea Centers for Disease Control and Prevention. Trends in the proportions of hypertensive, prehypertensive and normotensive Korean adults aged 30 and over, 2007–2016. In Public Health Weekly Report; Korea Centers for Disease Control and Prevention: Cheongju, Korea, 2018; Volume 11, p. 645. [Google Scholar]
- Lee, S.; Jeon, Y. The effects of high health risky activities including smoking and drinking habits. Korean Public Health Res. 2015, 41, 21–35. [Google Scholar]
- Honjo, K.; Iso, H.; Tsugane, S.; Tamakoshi, A.; Satoh, H.; Tajima, K.; Suzui, T.; Sobue, T. The effects of smoking and smoking cessation on mortality from cardiovascular disease among Japanese: Pooled analysis of three large-scale cohort studies in Japan. Tob. Control 2010, 19, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.A.; Huxley, R.R.; Woodward, M. Smoking as a risk factor for stroke in women compared with men: A systematic review and meta-analysis of 81 cohorts, including 3,980,359 individuals and 42,401 strokes. Stroke 2013, 44, 2821–2828. [Google Scholar] [CrossRef] [PubMed]
- De Gaetano, G.; Costanzo, S. Alcohol and health: Praise of the J curves. J. Am. Coll. Cardiol. 2017, 70, 923–925. [Google Scholar] [CrossRef] [PubMed]
- Corrao, G.; Rubbiati, L.; Bagnardi, V.; Zambon, A.; Poikolainen, K. Alcohol and coronary heart disease: A meta-analysis. Addiction 2000, 95, 1505–1523. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.S.; Kang, H.J.; Oh, H.S.; Paek, Y.M.; Choue, R.W.; Park, Y.K.; Choi, T.I. Effects of worksite nutrition counseling for health promotion; Twelve-weeks of nutrition counseling has positive effect on metabolic syndrome risk factors in male workers. Korean J. Community Nutr. 2008, 13, 46–61. [Google Scholar]
- Nam, G.E.; Cho, K.H.; Park, Y.G.; Han, K.D.; Choi, Y.S.; Kim, S.M.; Lee, K.S.; Ko, B.J.; Kim, Y.H.; Han, B.D.; et al. Socioeconomic status and dyslipidemia in Korean adults: The 2008–2010 Korea national health and nutrition examination survey. Prev. Med. 2013, 57, 304–309. [Google Scholar] [CrossRef]
- Kim, J.J.; Lee, E.J.; Lee, K.R. Study on Health Consciousness and Eating Habits of Workers at Deluxe Hotels in Seoul and Gyonggi-do regions. J. Korean Soc. Food Cult. 2016, 31, 587–596. [Google Scholar] [CrossRef]
- Sotos-Prieto, M.; Cash, S.B.; Christophi, C.A.; Folta, S.; Moffatt, S.; Muegge, C.; Korre, M.; Mozaffarian, D.; Kales, S.N. Rationale and design of feeding America’s bravest: Mediterranean diet-based intervention to change firefighters’ eating habits and improve cardiovascular risk profiles. Contemp. Clin. Trials 2017, 61, 101–107. [Google Scholar] [CrossRef]
- Egan, B.M.; Stevens-Fabry, S. Prehypertension—prevalence, health risks, and management strategies. Nat. Rev. Cardiol. 2015, 12, 289–300. [Google Scholar] [CrossRef] [PubMed]
- Nichols, G.A.; Hillier, T.A.; Brown, J.B. Progression from newly acquired impaired fasting glusose to type 2 diabetes. Diabetes Care 2007, 30, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Son, J.S.; Choi, S.; Kim, K.; Kim, S.M.; Choi, D.; Lee, G.; Jeong, S.M.; Park, S.Y.; Kim, Y.Y.; Yun, J.M.; et al. Association of blood pressure classification in Korean young adults according to the 2017 American College of Cardiology/American Heart Association guidelines with subsequent cardiovascular disease events. JAMA 2018, 320, 1783–1792. [Google Scholar] [CrossRef] [PubMed]
- Chun, B.Y.; Shin, J.Y. The scientific evidence for the management of prehypertensives and high risk group. J. Korean Med. Assoc. 2011, 54, 1013–1019. [Google Scholar] [CrossRef]
- Dosi, R.; Bhatt, N.; Shah, P.; Patell, R. Cardiovascular disease and menopause. J. Clin. Diagn. Res. 2014, 8, 62–64. [Google Scholar] [CrossRef]
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]

| Total Workers | Male Workers | Female Workers | p-Value | ||||
|---|---|---|---|---|---|---|---|
| (n = 5,335,465) | (n = 3,301,052) | (n = 2,034,413) | |||||
| n (%) | |||||||
| Age | |||||||
| Under 30 | 724,715 | (13.58) | 367,212 | (10.83) | 357,504 | (18.05) | <0.001 |
| 30s | 1,372,326 | (25.72) | 450,012 | (27.94) | 922,314 | (22.12) | |
| 40s | 1,550,794 | (29.07) | 575,332 | (29.55) | 975,461 | (28.28) | |
| 50s | 1,228,316 | (23.02) | 479,308 | (22.69) | 749,009 | (23.56) | |
| 60s | 459,313 | (8.61) | 162,550 | (8.99) | 296,765 | (7.99) | |
| Income level | |||||||
| 1 Q | 863,264 | (16.18) | 302,376 | (9.16) | 560,888 | (27.57) | <0.001 |
| 2 Q | 1,033,537 | (19.37) | 444,982 | (13.48) | 588,556 | (28.93) | |
| 3 Q | 1,111,566 | (20.83) | 698,172 | (21.15) | 413,393 | (20.32) | |
| 4 Q | 1,184,254 | (22.20) | 898,216 | (27.21) | 286,038 | (14.06) | |
| 5 Q | 1,142,845 | (21.42) | 957,305 | (29.00) | 185,538 | (9.12) | |
| Residential area | |||||||
| Metropolitan city | 3,720,540 | (69.73) | 2,272,444 | (68.84) | 1,448,095 | (71.18) | <0.001 |
| Small or medium city | 1,310,832 | (24.57) | 839,458 | (25.43) | 471,373 | (23.17) | |
| Rural area | 304,094 | (5.70) | 189,150 | (5.73) | 114,944 | (5.65) | |
| Male Workers | Female Workers | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Under 30 | 30s | 40s | 50s | 60s | p-Value | Under 30 | 30s | 40s | 50s | 60s | p-Value | |
| % | % | |||||||||||
| Smoking | ||||||||||||
| Non-smoker | 45.18 | 33.58 | 24.10 | 26.37 | 31.42 | <0.001 | 90.52 | 92.46 | 95.52 | 97.55 | 97.69 | <0.001 |
| Past smoker | 10.94 | 20.58 | 29.61 | 38.62 | 43.56 | 3.56 | 3.57 | 1.95 | 1.01 | 0.99 | ||
| Current smoker | 43.88 | 45.84 | 46.29 | 35.01 | 25.02 | 5.92 | 3.97 | 2.53 | 1.44 | 1.32 | ||
| Alcohol consumption | ||||||||||||
| Light drinker | 30.49 | 27.85 | 27.54 | 32.47 | 44.06 | <0.001 | 48.59 | 62.67 | 69.27 | 80.72 | 89.33 | <0.001 |
| Moderate drinker | 15.72 | 16.13 | 14.27 | 14.20 | 18.15 | 21.48 | 20.47 | 18.34 | 12.24 | 6.94 | ||
| Heavy drinker | 53.79 | 56.02 | 58.19 | 53.33 | 37.79 | 29.93 | 16.86 | 12.39 | 7.04 | 3.73 | ||
| Walking | ||||||||||||
| None | 16.46 | 16.82 | 18.52 | 20.57 | 21.18 | <0.001 | 14.47 | 19.79 | 21.34 | 23.46 | 26.67 | <0.001 |
| 1–2 times a week | 20.10 | 26.41 | 28.54 | 26.28 | 18.87 | 23.29 | 28.08 | 30.39 | 21.15 | 15.96 | ||
| 3–4 times a week | 19.16 | 20.76 | 22.94 | 24.25 | 24.25 | 22.03 | 20.82 | 21.95 | 22.55 | 19.68 | ||
| 5–7 times a week | 44.28 | 36.01 | 30.00 | 28.90 | 35.70 | 40.21 | 31.31 | 26.32 | 32.85 | 37.69 | ||
| Moderate exercise | ||||||||||||
| None | 37.57 | 39.03 | 38.17 | 38.69 | 43.51 | <0.001 | 47.56 | 50.64 | 47.08 | 50.24 | 59.09 | <0.001 |
| 1–2 times a week | 35.27 | 38.92 | 37.74 | 33.63 | 25.10 | 33.90 | 32.42 | 29.95 | 24.39 | 17.00 | ||
| 3–4 times a week | 16.94 | 14.72 | 16.32 | 18.12 | 18.67 | 13.52 | 12.12 | 15.40 | 16.04 | 12.90 | ||
| 5–7 times a week | 10.22 | 7.33 | 7.77 | 9.56 | 12.72 | 5.02 | 4.82 | 7.57 | 9.33 | 11.01 | ||
| Vigorous exercise | ||||||||||||
| None | 40.12 | 44.18 | 42.75 | 41.91 | 47.95 | <0.001 | 58.35 | 62.43 | 57.25 | 59.16 | 68.31 | <0.001 |
| 1–2 times a week | 36.16 | 37.69 | 36.64 | 34.71 | 26.36 | 28.65 | 26.2 | 26.1 | 22.82 | 15.38 | ||
| 3–4 times a week | 15.64 | 12.78 | 14.55 | 15.86 | 15.83 | 9.92 | 8.57 | 11.61 | 11.97 | 9.42 | ||
| 5–7 times a week | 8.08 | 5.35 | 6.06 | 7.52 | 9.86 | 3.08 | 2.80 | 5.04 | 6.05 | 6.89 | ||
| Male Workers | Female Workers | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1Q | 2Q | 3Q | 4Q | 5Q | p-Value | 1Q | 2Q | 3Q | 4Q | 5Q | p-Value | |
| % | % | |||||||||||
| Smoking | ||||||||||||
| Non-smoker | 31.01 | 32.81 | 29.64 | 28.29 | 30.30 | <0.001 | 94.65 | 93.85 | 93.88 | 95.45 | 96.94 | <0.001 |
| Past smoker | 27.17 | 24.74 | 23.76 | 27.95 | 35.82 | 2.21 | 2.36 | 2.59 | 2.29 | 1.77 | ||
| Current smoker | 41.82 | 42.45 | 46.61 | 43.76 | 33.87 | 3.14 | 3.79 | 3.53 | 2.25 | 1.29 | ||
| Alcohol consumption | ||||||||||||
| Light drinker | 40.11 | 37.73 | 32.03 | 27.27 | 26.02 | <0.001 | 74.21 | 67.09 | 63.37 | 64.6 | 71.15 | <0.001 |
| Moderate drinker | 14.04 | 15.01 | 14.75 | 15.23 | 16.11 | 13.94 | 16.86 | 19.23 | 20.23 | 17.30 | ||
| Heavy drinker | 45.85 | 47.26 | 53.22 | 57.49 | 57.87 | 11.86 | 16.05 | 17.40 | 15.17 | 11.55 | ||
| Walking | ||||||||||||
| None | 25.10 | 21.92 | 20.36 | 18.00 | 15.03 | <0.001 | 22.69 | 20.90 | 19.50 | 18.83 | 19.60 | <0.001 |
| 1–2 times a week | 22.71 | 20.57 | 24.01 | 27.56 | 28.79 | 20.53 | 22.52 | 25.67 | 28.72 | 29.29 | ||
| 3–4 times a week | 19.81 | 20.46 | 20.20 | 22.14 | 25.22 | 20.74 | 21.63 | 21.91 | 23.37 | 22.57 | ||
| 5–7 times a week | 32.38 | 37.05 | 35.43 | 32.30 | 30.96 | 36.04 | 34.95 | 32.92 | 30.08 | 28.54 | ||
| Moderate exercise | ||||||||||||
| None | 49.00 | 45.69 | 42.66 | 38.44 | 32.90 | <0.001 | 52.96 | 49.95 | 48.00 | 47.08 | 46.97 | <0.001 |
| 1–2 times a week | 27.87 | 29.65 | 34.22 | 38.22 | 39.68 | 23.93 | 27.62 | 31.76 | 34.01 | 33.18 | ||
| 3–4 times a week | 13.92 | 15.26 | 14.73 | 15.66 | 18.79 | 14.00 | 14.75 | 14.18 | 13.85 | 14.22 | ||
| 5–7 times a week | 9.21 | 9.40 | 8.39 | 7.68 | 8.63 | 9.11 | 7.68 | 6.06 | 5.06 | 5.63 | ||
| Vigorous exercise | ||||||||||||
| None | 52.95 | 49.66 | 46.55 | 42.52 | 38.32 | <0.001 | 62.96 | 59.40 | 58.34 | 58.56 | 58.76 | <0.001 |
| 1–2 times a week | 28.16 | 30.32 | 34.58 | 37.88 | 38.60 | 21.12 | 24.68 | 27.34 | 28.1 | 27.12 | ||
| 3–4 times a week | 11.74 | 12.97 | 12.59 | 13.77 | 16.56 | 10.20 | 11.00 | 10.46 | 10.14 | 10.54 | ||
| 5–7 times a week | 7.15 | 7.05 | 6.28 | 5.83 | 6.52 | 5.72 | 4.92 | 3.86 | 3.20 | 3.59 | ||
| Male Workers | Female Workers | |||||||
|---|---|---|---|---|---|---|---|---|
| Metropolitan City | Small or Medium City | Rural Area | p-Value | Metropolitan City | Small or Medium City | Rural Area | p-Value | |
| % | % | |||||||
| Smoking | ||||||||
| Non-smoker | 29.97 | 30.20 | 33.14 | <0.001 | 93.96 | 96.09 | 96.44 | <0.001 |
| Past smoker | 29.19 | 28.17 | 24.46 | 2.60 | 1.63 | 1.34 | ||
| Current smoker | 40.84 | 41.64 | 42.40 | 3.44 | 2.28 | 2.22 | ||
| Alcohol consumption | ||||||||
| Light drinker | 30.45 | 30.18 | 33.36 | <0.001 | 67.51 | 69.84 | 73.33 | <0.001 |
| Moderate drinker | 15.77 | 14.24 | 13.96 | 17.69 | 15.81 | 13.73 | ||
| Heavy drinker | 53.78 | 55.58 | 52.68 | 14.81 | 14.34 | 12.94 | ||
| Walking | ||||||||
| None | 17.20 | 20.80 | 24.39 | <0.001 | 18.54 | 25.06 | 29.66 | <0.001 |
| 1–2 times a week | 25.06 | 27.31 | 25.41 | 23.36 | 26.22 | 25.06 | ||
| 3–4 times a week | 22.42 | 22.41 | 20.93 | 21.84 | 21.54 | 20.07 | ||
| 5–7 times a week | 35.32 | 29.48 | 29.27 | 36.26 | 27.18 | 25.21 | ||
| Moderate exercise | ||||||||
| None | 38.76 | 38.74 | 42.08 | <0.001 | 48.85 | 50.76 | 55.25 | <0.001 |
| 1–2 times a week | 36.05 | 35.61 | 32.50 | 29.51 | 27.78 | 25.11 | ||
| 3–4 times a week | 16.52 | 16.74 | 16.23 | 14.42 | 14.23 | 12.84 | ||
| 5–7 times a week | 8.67 | 8.91 | 9.19 | 7.22 | 7.23 | 6.80 | ||
| Vigorous exercise | ||||||||
| None | 43.31 | 42.35 | 44.64 | <0.001 | 59.62 | 59.98 | 63.56 | <0.001 |
| 1–2 times a week | 35.76 | 35.53 | 32.54 | 25.39 | 24.32 | 22.10 | ||
| 3–4 times a week | 14.38 | 15.01 | 15.14 | 10.53 | 10.77 | 9.76 | ||
| 5–7 times a week | 6.55 | 7.11 | 7.68 | 4.46 | 4.93 | 4.58 | ||
| Male Workers | Female Workers | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Under 30 | 30s | 40s | 50s | 60s | p-Value | Under 30 | 30s | 40s | 50s | 60s | p-Value | |
| Mean ± SD or % | Mean ± SD or % | |||||||||||
| BMI (kg/m2) | 24.33 ± 3.80 | 25.11 ± 3.58 | 24.91 ± 3.20 | 24.54 ± 2.88 | 24.28 ± 2.81 | 21.45 ± 3.58 | 22.09 ± 3.69 | 22.98 ± 3.39 | 23.57 ± 3.11 | 24.15 ± 3.07 | ||
| Obesity | 37.05 | 47.58 | 46.60 | 42.40 | 39.26 | <0.001 | 12.99 | 17.13 | 23.28 | 28.72 | 36.37 | <0.001 |
| WC (cm) | 82.08 ± 9.52 | 84.96 ± 9.14 | 84.83 ± 8.24 | 84.81 ± 7.60 | 82.55 ± 7.77 | 71.37 ± 8.70 | 75.05 ± 8.09 | 75.82 ± 8.08 | 76.91 ± 8.38 | 79.74 ± 8.27 | ||
| Abdominal obesity | 19.12 | 27.18 | 25.75 | 24.97 | 23.58 | <0.001 | 7.05 | 10.76 | 12.28 | 16.52 | 26.18 | <0.001 |
| BP (SBP/DBP, mmHg) | 120.68 ± 11.68/ 74.61 ± 8.50 | 122.86 ± 12.40/ 77.17 ± 9.33 | 123.69 ± 13.15/ 78.64 ± 9.77 | 125.04 ± 13.63/ 78.96 ± 9.51 | 127.00 ± 13.87/ 78.08 ± 9.21 | 110.95 ± 10.97/ 69.26 ± 8.30 | 111.71 ± 11.91/ 70.29 ± 8.92 | 116.04 ± 13.45/ 73.00 ± 9.59 | 120.20 ± 14.15/ 74.94 ± 9.54 | 124.19 ± 14.30/ 75.65 ± 9.25 | ||
| Borderline | 51.65 | 54.56 | 53.8 | 55.06 | 56.55 | <0.001 | 23.66 | 25.67 | 36.08 | 45.35 | 51.71 | <0.001 |
| Hypertension | 4.88 | 9.03 | 13.05 | 15.31 | 18.37 | 1.22 | 2.34 | 5.79 | 9.67 | 14.61 | ||
| FG (mg/dL) | 91.90 ± 14.20 | 96.37 ± 19.35 | 101.73 ± 25.01 | 106.46 ± 9.51 | 108.19 ± 29.27 | 88.66 ± 11.93 | 90.66 ± 14.49 | 94.10 ± 17.18 | 97.62 ± 19.83 | 100.52 ± 21.85 | ||
| Pre-diabetes | 17.39 | 26.43 | 34.14 | 38.52 | 38.91 | <0.001 | 9.11 | 12.97 | 20.09 | 26.83 | 31.05 | <0.001 |
| High FG | 1.06 | 3.01 | 7.37 | 12.52 | 15.37 | 0.56 | 1.20 | 2.67 | 5.08 | 7.81 | ||
| TG (mg/dL) | 116.77 ± 27.25 | 155.52 ± 38.49 | 167.02 ± 39.33 | 154.84 ± 34.21 | 137.68 ± 32.88 | 75.23 ± 16.76 | 86.53 ± 11.11 | 95.84 ± 14.00 | 112.10 ± 20.45 | 119.86 ± 22.19 | ||
| High TG | 10.80 | 21.69 | 25.62 | 21.64 | 15.96 | <0.001 | 2.01 | 3.99 | 5.22 | 8.56 | 10.10 | <0.001 |
| HDL-C (mg/dL) | 55.13 ± 13.99 | 52.54 ± 14.23 | 52.17 ± 14.84 | 52.32 ± 14.56 | 52.58 ± 15.05 | 66.93 ± 15.60 | 64.66 ± 16.23 | 62.68 ± 17.38 | 61.24 ± 16.78 | 58.73 ± 15.41 | ||
| Low HDL-C | 9.10 | 13.49 | 14.68 | 14.98 | 15.12 | <0.001 | 1.63 | 2.62 | 3.53 | 4.55 | 6.32 | <0.001 |
| CVD risk† | ||||||||||||
| Low | 99.86 | 98.62 | 95.72 | 91.36 | <0.001 | 99.97 | 99.67 | 98.27 | 94.71 | <0.001 | ||
| Moderate | 0.14 | 1.35 | 3.53 | 5.86 | 0.03 | 0.33 | 1.65 | 4.51 | ||||
| High | 0.00 | 0.03 | 0.75 | 2.78 | 0.00 | 0.00 | 0.09 | 0.78 | ||||
| Male Workers | Female Workers | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1Q | 2Q | 3Q | 4Q | 5Q | p-Value | 1Q | 2Q | 3Q | 4Q | 5Q | p-Value | |
| Mean ± SD or % | Mean ± SD or % | |||||||||||
| BMI (kg/m2) | 24.59 ± 3.46 | 24.46 ± 3.53 | 24.71 ± 3.54 | 24.87 ± 3.30 | 24.86 ± 2.94 | 23.36 ± 3.54 | 22.92 ± 3.55 | 22.39 ± 3.54 | 21.97 ± 3.32 | 22.25 ± 3.18 | ||
| Obesity | 40.32 | 42.79 | 43.09 | 45.52 | 45.64 | <0.001 | 28.00 | 24.10 | 19.56 | 15.68 | 16.91 | <0.001 |
| WC (cm) | 84.74 ± 9.11 | 83.87 ± 9.18 | 84.23 ± 8.97 | 84.77 ± 8.39 | 85.20 ± 7.66 | 76.39 ± 13.67 | 75.08 ± 19.88 | 74.44 ± 32.77 | 74.28 ± 39.61 | 74.36 ± 3.85 | ||
| Abdominal obesity | 23.82 | 24.20 | 24.81 | 25.75 | 26.08 | <0.001 | 17.17 | 13.63 | 11.06 | 9.12 | 10.03 | <0.001 |
| BP (SBP/DBP, mmHg) | 124.74 ± 13.85/ 77.89 ± 9.77 | 124.37 ± 13.64/ 77.53 ± 0.64 | 124.05 ± 13.29/ 77.87 ± 9.59 | 123.92 ± 12.82/ 78.06 ± 9.48 | 123.01 ± 12.74/ 77.78 ± 9.42 | 118.57 ± 14.20/ 73.85 ± 9.57 | 116.72 ± 13.63/ 73.04 ± 0.42 | 114.36 ± 12.98/ 71.76 ± 9.21 | 112.38 ± 12.40/ 70.30 ± 9.05 | 113.07 ± 13.13/ 70.60 ± 9.48 | ||
| Borderline | 53.94 | 53.57 | 54.34 | 55.27 | 53.71 | <0.001 | 41.04 | 37.50 | 31.81 | 26.63 | 28.64 | <0.001 |
| Hypertension | 15.09 | 13.73 | 12.51 | 11.76 | 10.85 | 8.61 | 6.28 | 4.29 | 2.93 | 3.87 | ||
| FG (mg/dL) | 104.73 ± 31.23 | 101.12 ± 26.09 | 100.01 ± 24.55 | 100.00 ± 23.35 | 101.23 ± 22.75 | 96.11 ± 19.77 | 94.13 ± 17.63 | 92 ± 15.86 | 91.15 ± 14.28 | 92.19 ± 14.81 | ||
| Pre-diabetes | 32.83 | 30.84 | 30.32 | 31.04 | 33.37 | <0.001 | 23.31 | 20.02 | 16.48 | 14.04 | 15.93 | <0.001 |
| High FG | 11.58 | 8.23 | 6.73 | 6.41 | 7.37 | 4.42 | 3.13 | 2.14 | 1.54 | 1.89 | ||
| TG (mg/dL) | 153.91 ± 32.57 | 144.14 ± 28.33 | 153.00 ± 28.34 | 158.04 ± 25.75 | 154.50 ± 20.74 | 104.07 ± 28.75 | 97.15 ± 16.92 | 90.63 ± 16.88 | 86.73 ± 15.28 | 92.08 ± 16.74 | ||
| High TG | 21.68 | 18.40 | 21.01 | 22.62 | 21.67 | <0.001 | 7.15 | 5.83 | 4.64 | 3.84 | 4.38 | <0.001 |
| HDL-C (mg/dL) | 52.18 ± 14.87 | 53.46 ± 15.18 | 53.23 ± 15.72 | 52.58 ± 14.16 | 51.90 ± 13.24 | 61.53 ± 16.89 | 63.21 ± 17.15 | 64.37 ± 16.60 | 64.68 ± 15.68 | 63.78 ± 15.96 | ||
| Low HDL-C | 15.69 | 13.25 | 13.22 | 13.66 | 14.67 | <0.001 | 4.51 | 3.45 | 2.78 | 2.58 | 3.01 | <0.001 |
| CVD risk † | ||||||||||||
| Low | 94.58 | 96.1 | 97.97 | 98.35 | 97.84 | <0.001 | 98.01 | 98.84 | 99.36 | 99.62 | 99.51 | <0.001 |
| Moderate | 3.88 | 2.87 | 1.63 | 1.40 | 1.90 | 1.79 | 1.07 | 0.60 | 0.36 | 0.47 | ||
| High | 1.54 | 1.03 | 0.40 | 0.25 | 0.26 | 0.21 | 0.10 | 0.04 | 0.02 | 0.02 | ||
| Male Workers | Female Workers | |||||||
|---|---|---|---|---|---|---|---|---|
| Metropolitan City | Small or Medium City | Rural Area | p-Value | Metropolitan City | Small or Medium City | Rural Area | p-Value | |
| Mean ± SD or % | Mean ± SD or % | |||||||
| BMI (kg/m2) | 24.77 ± 3.29 | 24.73 ± 3.29 | 24.76 ± 3.34 | 22.66 ± 3.51 | 22.86 ± 3.48 | 23.22 ± 3.57 | ||
| Obesity | 44.29 | 43.96 | 44.63 | <0.001 | 21.75 | 23.19 | 27.12 | <0.001 |
| WC (cm) | 84.77 ± 8.51 | 84.28 ± 8.46 | 84.04 ± 8.71 | 75.10 ± 7.35 | 75.04 ± 74 | 75.92 ± 797 | ||
| Abdominal obesity | 26.01 | 23.18 | 23.74 | <0.001 | 12.85 | 13.27 | 15.64 | <0.001 |
| BP (SBP/DBP, mmHg) | 124.76 ± 13.14/ 77.81 ± 9.59 | 123.64 ± 12.87/ 77.81 ± 9.29 | 123.89 ± 13.06/ 77.92 ± 9.30 | 115.6 ± 13.65/ 72.17 ± 9.50 | 116.37 ± 13.46/ 72.81 ± 9.31 | 117.61 ± 13.89/ 73.49 ± 9.43 | ||
| Borderline | 53.77 | 55.70 | 54.68 | <0.001 | 33.82 | 37.42 | 39.32 | <0.001 |
| Hypertension | 12.30 | 11.24 | 12.32 | 5.68 | 5.84 | 7.58 | ||
| FG (mg/dL) | 100.86 ± 14.31 | 100.63 ± 14.65 | 101.24 ± 16.11 | 93.50 ± 10.09 | 93.96 ± 10.53 | 95.17 ± 10.32 | ||
| Pre-diabetes | 31.72 | 31.31 | 31.37 | <0.001 | 18.56 | 19.68 | 21.62 | <0.001 |
| High FG | 7.34 | 7.24 | 7.99 | 2.83 | 3.06 | 3.99 | ||
| TG (mg/dL) | 152.83 ± 30.20 | 153.19 ± 30.41 | 153.53 ± 30`69 | 95.10 ± 10.57 | 96.63 ± 10.41 | 101.40 ± 10.87 | ||
| High TG | 21.07 | 21.29 | 21.40 | <0.001 | 5.39 | 5.73 | 6.82 | <0.001 |
| HDL-C (mg/dL) | 52.71 ± 8.02 | 52.62 ± 8.09 | 52.34 ± 7.79 | 63.54 ± 8.50 | 62.81 ± 8.05 | 61.06 ± 8.77 | ||
| Low HDL-C | 13.72 | 14.03 | 14.72 | <0.001 | 3.23 | 3.75 | 4.92 | <0.001 |
| CVD risk† | ||||||||
| Low | 97.47 | 97.8 | 97.28 | <0.001 | 98.88 | 98.93 | 98.41 | <0.001 |
| Moderate | 2.04 | 1.77 | 2.15 | 1.02 | 0.97 | 1.42 | ||
| High | 0.49 | 0.43 | 0.57 | 0.10 | 0.10 | 0.17 | ||
| Variables | Male Workers | Female Workers | ||
|---|---|---|---|---|
| OR | 95% CI Wald F | OR | 95% CI Wald F | |
| Age | ||||
| 30s | reference | reference | ||
| 40s | 9.217 | 8.702–9.762 | 10.552 | 8.846–12.588 |
| 50s | 23.648 | 22.352–25.019 | 50.033 | 42.107–59.450 |
| 60s | 36.951 | 34.877–39.149 | 125.506 | 105.526–149.269 |
| SES | ||||
| Income | ||||
| 1Q | 1.523 | 1.482–1.565 | 1.924 | 1.787–2.071 |
| 2Q | 1.265 | 1.231–1.300 | 1.576 | 1.462–1.700 |
| 3Q | 1.105 | 1.076–1.135 | 1.412 | 1.298–1.535 |
| 4Q | 1.094 | 1.067–1.121 | 1.317 | 1.194–1.454 |
| 5Q | reference | reference | ||
| Residential Area | ||||
| Metropolitan city | reference | reference | ||
| Small or medium city | 0.915 | 0.897–0.934 | 0.941 | 0.907–0.977 |
| Rural area | 1.048 | 1.010–1.086 | 1.151 | 1.086–1.219 |
| Health behavior | ||||
| Smoking | ||||
| Non-smoker | reference | reference | ||
| Past smoker | 0.811 | 0.792–0.830 | 1.352 | 1.188–1.538 |
| Current smoker | 1.273 | 1.247–1.300 | 1.369 | 1.226–1.528 |
| Alcohol consumption | ||||
| Light drinker | reference | reference | ||
| Moderate drinker | 0.828 | 0.805–0.852 | 0.668 | 0.630–0.708 |
| Heavy drinker | 1.298 | 1.273–1.323 | 0.914 | 0.857–0.975 |
| Walking | reference | reference | ||
| None | 1.722 | 1.583–1.899 | 2.003 | 1.865–1.211 |
| 1–2 times a week | 1.100 | 1.086–1.125 | 1.183 | 1.137–1.206 |
| 3–4 times a week | 1.036 | 1.010–1.062 | 1.056 | 1.029–1.083 |
| 5–7 times a week | reference | reference | ||
| Moderate exercise | ||||
| None | 1.051 | 1.023–1.078 | 1.044 | 1.028–1.075 |
| 1–2 times a week | 1.021 | 1.005–1.038 | 1.015 | 1.004–1.036 |
| 3–4 times a week | 0.939 | 0.901–0.979 | 0.970 | 0.901–1.045 |
| 5–7 times a week | reference | reference | ||
| Vigorous exercise | ||||
| None | 1.118 | 1.073–1.166 | 1.125 | 1.041–1.216 |
| 1–2 times a week | 1.009 | 0.966–1.054 | 0.974 | 0.894–1.062 |
| 3–4 times a week | 1.005 | 0.960–1.052 | 0.972 | 0.886–1.066 |
| 5–7 times a week | reference | reference | ||
| CVD-related health status | ||||
| BMI | ||||
| Normal | reference | reference | ||
| Overweight | 1.803 | 1.762–1.844 | 1.181 | 1.160–1.203 |
| Obesity | 2.649 | 2.598–2.701 | 1.546 | 1.501–1.592 |
| WC | ||||
| Normal | reference | reference | ||
| Abdominal obesity | 1.471 | 1.440–1.503 | 1.257 | 1.203– 1.313 |
| BP | ||||
| Normal | reference | reference | ||
| Borderline | 1.060 | 1.036–1.085 | 1.044 | 1.019–1.070 |
| Hypertension | 1.305 | 1.277–1.334 | 1.541 | 1.465–.620 |
| FG | ||||
| Normal | reference | reference | ||
| Pre-diabetes | 1.481 | 1.166–1.497 | 1.491 | 1.468–.515 |
| High FG | 1.851 | 1.847– 1.897 | 1.979 | 1.953–.806 |
| TC | ||||
| Normal | reference | reference | ||
| Hypercholesterolemia | 1.030 | 1.008–1.052 | 1.019 | 0.988–1.051 |
| TG | ||||
| Normal | reference | reference | ||
| Hypertriglyceridemia | 1.091 | 1.073–1.110 | 1.011 | 0.961–1.150 |
| HDL-C | ||||
| Normal | reference | reference | ||
| Low HDL-C | 1.041 | 1.023–1.061 | 1.103 | 1.070–1.144 |
| LDL-C | ||||
| Normal | reference | reference | ||
| High LDL-C | 1.052 | 1.035–1.071 | 1.038 | 1.010–1.066 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ryu, H.; Moon, J.; Jung, J. Sex Differences in Cardiovascular Disease Risk by Socioeconomic Status (SES) of Workers Using National Health Information Database. Int. J. Environ. Res. Public Health 2020, 17, 2047. https://doi.org/10.3390/ijerph17062047
Ryu H, Moon J, Jung J. Sex Differences in Cardiovascular Disease Risk by Socioeconomic Status (SES) of Workers Using National Health Information Database. International Journal of Environmental Research and Public Health. 2020; 17(6):2047. https://doi.org/10.3390/ijerph17062047
Chicago/Turabian StyleRyu, Hosihn, Jihyun Moon, and Jiyeon Jung. 2020. "Sex Differences in Cardiovascular Disease Risk by Socioeconomic Status (SES) of Workers Using National Health Information Database" International Journal of Environmental Research and Public Health 17, no. 6: 2047. https://doi.org/10.3390/ijerph17062047
APA StyleRyu, H., Moon, J., & Jung, J. (2020). Sex Differences in Cardiovascular Disease Risk by Socioeconomic Status (SES) of Workers Using National Health Information Database. International Journal of Environmental Research and Public Health, 17(6), 2047. https://doi.org/10.3390/ijerph17062047





