Effects of HIV-Related Discrimination on Psychosocial Syndemics and Sexual Risk Behavior among People Living with HIV
Abstract
1. Introduction
1.1. Syndemic Theory
1.2. HIV and Discrimination in Hong Kong
1.3. The Present Study
2. Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Data Analysis
3. Results
3.1. HIV-Related Discrimination and Psychosocial Syndemics
3.2. Condom Use with Steady and Casual Partners
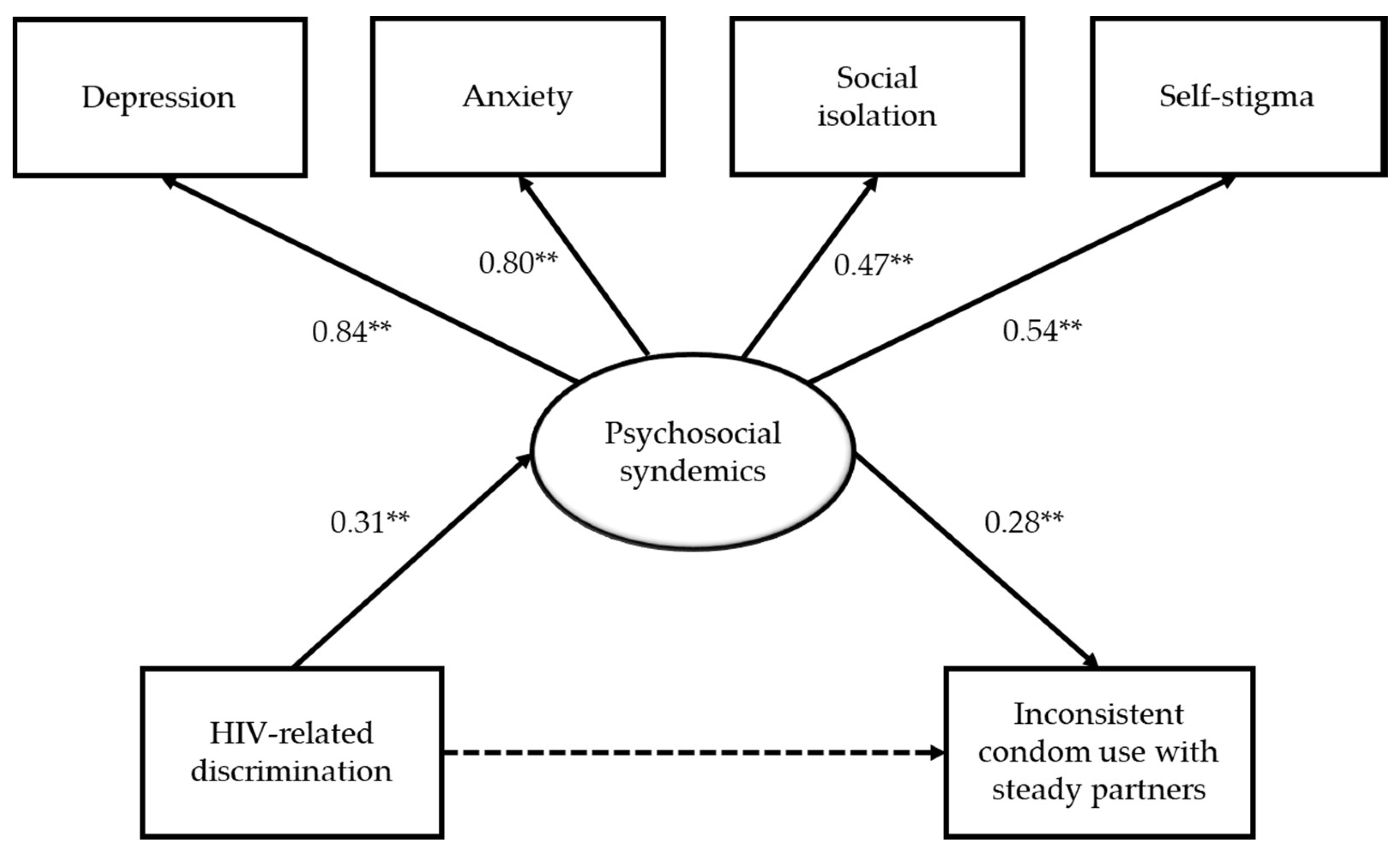
3.3. A Mediation Model of HIV-Related Discrimination on Sexual Risk Behavior
4. Discussion
4.1. Relevance to Local Context
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dos Santos, M.M.; Kruger, P.; Mellors, S.E.; Wolvaardt, G.; Van Der Ryst, E. An exploratory survey measuring stigma and discrimination experienced by people living with HIV/AIDS in South Africa: The People Living with HIV Stigma Index. BMC Public Health 2014, 14, 80. [Google Scholar] [CrossRef] [PubMed]
- Simbayi, L.C.; Kalichman, S.; Strebel, A.; Cloete, A.; Henda, N.; Mqeketo, A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc. Sci. Med. 2007, 64, 1823–1831. [Google Scholar] [CrossRef] [PubMed]
- Paxton, S.; Gonzales, G.; Uppakaew, K.; Abraham, K.; Okta, S.; Green, C.; Nair, K.; Parwati Merati, T.; Thephthien, B.; Marin, M. AIDS-related discrimination in Asia. AIDS Care 2005, 17, 413–424. [Google Scholar] [CrossRef] [PubMed]
- Nachega, J.B.; Morroni, C.; Zuniga, J.M.; Sherer, R.; Beyrer, C.; Solomon, S.; Schechter, M.; Rockstroh, J. HIV-related stigma, isolation, discrimination, and serostatus disclosure: A global survey of 2035 HIV-infected adults. J. Int. Assoc. Physicians AIDS Care 2012, 11, 172–178. [Google Scholar] [CrossRef]
- Wingood, G.M.; DiClemente, R.J.; Mikhail, I.; McCree, D.H.; Davies, S.L.; Hardin, J.W.; Peterson, S.H.; Hook, E.W.; Saag, M. HIV discrimination and the health of women living with HIV. Women Health 2007, 46, 99–112. [Google Scholar] [CrossRef]
- Stutterheim, S.E.; Pryor, J.B.; Bos, A.E.; Hoogendijk, R.; Muris, P.; Schaalma, H.P. HIV-related stigma and psychological distress: The harmful effects of specific stigma manifestations in various social settings. AIDS 2009, 23, 2353–2357. [Google Scholar] [CrossRef]
- Elford, J.; Ibrahim, F.; Bukutu, C.; Anderson, J. HIV-related discrimination reported by people living with HIV in London, UK. AIDS Behav. 2008, 12, 255–264. [Google Scholar] [CrossRef]
- Bogart, L.M.; Wagner, G.J.; Galvan, F.H.; Landrine, H.; Klein, D.J.; Sticklor, L.A. Perceived discrimination and mental health symptoms among Black men with HIV. Cult. Divers. Ethn. Minor. Psychol. 2011, 17, 295–302. [Google Scholar] [CrossRef]
- Préau, M.; Bouhnik, A.D.; Peretti-Watel, P.; Obadia, Y.; Spire, B.; Group, A.E.V. Suicide attempts among people living with HIV in France. AIDS Care 2008, 20, 917–924. [Google Scholar] [CrossRef]
- Mak, W.W.; Cheung, R.Y. Self-stigma among concealable minorities in Hong Kong: Conceptualization and unified measurement. Am. J. Orthopsychiatry 2010, 80, 267–281. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Watson, A.C. The paradox of self-stigma and mental illness. Clin. Psychol. Sci. Pract. 2002, 9, 35–53. [Google Scholar] [CrossRef]
- Mak, W.W.; Cheung, R.Y.; Law, R.W.; Woo, J.; Li, P.C.; Chung, R.W. Examining attribution model of self-stigma on social support and psychological well-being among people with HIV+/AIDS. Soc. Sci. Med. 2007, 64, 1549–1559. [Google Scholar] [CrossRef] [PubMed]
- Peretti-Watel, P.; Spire, B.; Obadia, Y.; Moatti, J.P.; Group, V. Discrimination against HIV-infected people and the spread of HIV: Some evidence from France. PLoS ONE 2007, 2, 411. [Google Scholar] [CrossRef] [PubMed]
- Paz-Bailey, G.; Fernandez, V.I.; Miranda, S.M.; Jacobson, J.O.; Mendoza, S.; Paredes, M.A.; Danaval, D.C.; Mabey, D.; Monterroso, E. Unsafe sexual behaviors among HIV-positive men and women in Honduras: The role of discrimination, condom access, and gender. Sex. Transm. Dis. 2012, 39, 35–41. [Google Scholar] [CrossRef]
- Singer, M.; Clair, S. Syndemics and public health: Reconceptualizing disease in bio-social context. Med. Anthropol. Q. 2003, 17, 423–441. [Google Scholar] [CrossRef]
- Singer, M. AIDS and the health crisis of the US urban poor; the perspective of critical medical anthropology. Soc. Sci. Med. 1994, 39, 931–948. [Google Scholar] [CrossRef]
- Mustanski, B.; Garofalo, R.; Herrick, A.; Donenberg, G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: Preliminary evidence of a syndemic in need of attention. Ann. Behav. Med. 2007, 34, 37–45. [Google Scholar] [CrossRef]
- Tsai, A.C.; Burns, B.F. Syndemics of psychosocial problems and HIV risk: A systematic review of empirical tests of the disease interaction concept. Soc. Sci. Med. 2015, 139, 26–35. [Google Scholar] [CrossRef]
- Batchelder, A.W.; Lounsbury, D.W.; Palma, A.; Carrico, A.; Pachankis, J.; Schoenbaum, E.; Gonzalez, J.S. Importance of substance use and violence in psychosocial syndemics among women with and at-risk for HIV. AIDS Care 2016, 28, 1316–1320. [Google Scholar] [CrossRef]
- Nehl, E.J.; Klein, H.; Sterk, C.E.; Elifson, K.W. Prediction of HIV sexual risk behaviors among disadvantaged African American adults using a syndemic conceptual framework. AIDS Behav. 2016, 20, 449–460. [Google Scholar] [CrossRef][Green Version]
- Kim, H.; He, Y.; Pham, R.; Ravelo, G.J.; Rojas, P.; Rodriguez, P.; Castro, G.; Barengo, N.C.; Acuña, J.M.; Cyrus, E. Analyzing the association between depression and high-risk sexual behavior among adult Latina immigrant farm workers in Miami-Dade County. Int. J. Environ. Res. Public Health 2019, 16, 1120. [Google Scholar] [CrossRef] [PubMed]
- Operario, D.; Yang, M.F.; Reisner, S.L.; Iwamoto, M.; Nemoto, T. Stigma and the syndemic of HIV-related health risk behaviors in a diverse sample of transgender women. J. Community Psychol. 2014, 42, 544–557. [Google Scholar] [CrossRef]
- Biello, K.B.; Colby, D.; Closson, E.; Mimiaga, M.J. The syndemic condition of psychosocial problems and HIV risk among male sex workers in Ho Chi Minh City, Vietnam. AIDS Behav. 2014, 18, 1264–1271. [Google Scholar] [CrossRef] [PubMed][Green Version]
- An, X.; Sun, Q.; Fang, F.; Rao, Z.; Li, X.; Lv, Y.; Li, T.; Lin, A. The prevalence of depression associated with the infection status and sexual behaviors among men who have sex with men in Shenzhen, China: A cross-sectional study. Int. J. Environ. Res. Public Health 2020, 17, 127. [Google Scholar] [CrossRef] [PubMed]
- Coulter, R.W.; Kinsky, S.M.; Herrick, A.L.; Stall, R.D.; Bauermeister, J.A. Evidence of syndemics and sexuality-related discrimination among young sexual-minority women. LGBT Health 2015, 2, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Herrick, A.; Stall, R.; Egan, J.; Schrager, S.; Kipke, M. Pathways towards risk: Syndemic conditions mediate the effect of adversity on HIV risk behaviors among young men who have sex with men (YMSM). J. Urban Health 2014, 91, 969–982. [Google Scholar] [CrossRef]
- van den Berg, J.J.; Fernández, M.I.; Fava, J.L.; Operario, D.; Rudy, B.J.; Wilson, P.A. Using syndemics theory to investigate risk and protective factors associated with condomless sex among youth living with HIV in 17 US cities. AIDS Behav. 2017, 21, 833–844. [Google Scholar] [CrossRef]
- Virtual AIDS Office of Hong Kong, Department of Health, The Government of the Hong Kong Special Administrative Region. HIV Surveillance and Epidemiology. Available online: http://www.info.gov.hk/aids/english/surveillance/latest_stat.htm (accessed on 20 May 2019).
- Hong Kong Advisory Council on AIDS. Recommended HIV/AIDS Strategies for Hong Kong 2017–2021. 2017. Available online: http://www.aca.gov.hk/english/strategies/pdf/strategies17-21.pdf (accessed on 20 May 2019).
- Lau, J.; Kim, J.; Lau, M.; Tsui, H. HIV related behaviours and attitudes among Chinese men who have sex with men in Hong Kong: A population based study. Sex. Transm. Infect. 2004, 80, 459–465. [Google Scholar] [CrossRef]
- Chan, W. AIDS and the Law: The Hong Kong Experience; Hong Kong Advisory Council on AIDS, the Government of the Hong Kong Special Administrative Region: Hong Kong, China, 1997.
- Mak, W.W.; Mo, P.K.; Cheung, R.Y.; Woo, J.; Cheung, F.M.; Lee, D. Comparative stigma of HIV/AIDS, SARS, and tuberculosis in Hong Kong. Soc. Sci. Med. 2006, 63, 1912–1922. [Google Scholar] [CrossRef]
- Lau, J.; Tsui, H.; Li, C.; Chung, R.; Chan, M.; Molassiotis, A. Needs assessment and social environment of people living with HIV/AIDS in Hong Kong. AIDS Care 2003, 15, 699–706. [Google Scholar] [CrossRef]
- Equal Opportunities Commission. Baseline Survey on Public Attitudes towards Persons with a Disability. 2010. Available online: http://www.eoc.org.hk/EOC/Upload/UserFiles/File/ResearchReport/201109/DisabilityReport(eng).pdf (accessed on 20 May 2019).
- Zhou, Y.R. “If you get AIDS You have to endure it alone”: Understanding the social constructions of HIV/AIDS in China. Soc. Sci. Med. 2007, 65, 284–295. [Google Scholar] [CrossRef] [PubMed]
- Au, A.; Chan, I.; Li, P.; Chung, R.; Po, L.M.; Yu, P. Stress and health–related quality of life among HIV-infected persons in Hong Kong. AIDS Behav. 2004, 8, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Szymanski, D.M. Does internalized heterosexism moderate the link between heterosexist events and lesbians’ psychological distress? Sex Roles 2006, 54, 227–234. [Google Scholar] [CrossRef]
- Veit, C.T.; Ware, J.E. The structure of psychological distress and well-being in general populations. J. Consult. Clin. Psychol. 1983, 51, 730–742. [Google Scholar] [CrossRef] [PubMed]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The multidimensional scale of perceived social support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Kuhns, L.M.; Hotton, A.L.; Garofalo, R.; Muldoon, A.L.; Jaffe, K.; Bouris, A.; Voisin, D.; Schneider, J. An index of multiple psychosocial, syndemic conditions is associated with antiretroviral medication adherence among HIV-positive youth. AIDS Patient Care STDs 2016, 30, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, Y.; Purcell, D.W.; Knowlton, A.R.; Wilkinson, J.D.; Gourevitch, M.N.; Knight, K.R. Syndemic vulnerability, sexual and injection risk behaviors, and HIV continuum of care outcomes in HIV-positive injection drug users. AIDS Behav. 2015, 19, 684–693. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Social Sciences, 2nd ed.; Erlbaum: New York, NY, USA, 1988. [Google Scholar]
- Flora, D.B.; Curran, P.J. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychol. Methods 2004, 9, 466–491. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Yu, C.Y. Evaluating Cut off Criteria of Model Fit Indices for Latent Variable Models with Binary and Continuous Outcomes. Ph.D. Thesis, University of California, Los Angeles, CA, USA, 2002. [Google Scholar]
- George, D.; Mallery, M. SPSS for Windows Step by Step: A Simple Guide and Reference, 10th ed.; Pearson: Boston, MA, USA, 2010. [Google Scholar]
- Lau, J.T.; Tsui, H.; Ho, S.P.; Wong, E.; Yang, X. Prevalence of psychological problems and relationships with condom use and HIV prevention behaviors among Chinese female sex workers in Hong Kong. AIDS Care 2010, 22, 659–668. [Google Scholar] [CrossRef]
- Starks, T.J.; Millar, B.M.; Parsons, J.T. Predictors of condom use with main and casual partners among HIV-positive men over 50. Health Psychol. 2015, 34, 1116–1122. [Google Scholar] [CrossRef] [PubMed]
- Bauermeister, J.A.; Hickok, A.M.; Meadowbrooke, C.; Veinot, T.; Loveluck, J. Self-efficacy among young men who have sex with men: An exploratory analysis of HIV/AIDS risk behaviors across partner types. AIDS Behav. 2014, 18, 69–77. [Google Scholar] [CrossRef] [PubMed]
- van Kesteren, N.M.; Hospers, H.J.; van Empelen, P.; Van Breukelen, G.; Kok, G. Sexual decision-making in HIV-positive men who have sex with men: How moral concerns and sexual motives guide intended condom use with steady and casual sex partners. Arch. Sex. Behav. 2007, 36, 437–449. [Google Scholar] [CrossRef] [PubMed]
- Auerbach, J.D. Principles of positive prevention. J. Acquir. Immune Defic. Syndr. 2004, 37, 122–125. [Google Scholar] [CrossRef]
- Yeo, T.E.D.; Chu, T.H. Social-cultural factors of HIV-related stigma among the Chinese general population in Hong Kong. AIDS Care 2017, 29, 1255–1259. [Google Scholar] [CrossRef]
- Kan, R.; Au, K.; Chan, W.; Cheung, L.; Lam, C.; Liu, H.; Ng, L.; Wong, M.; Wong, W. Homophobia in medical students of the University of Hong Kong. Sex Educ. 2009, 9, 65–80. [Google Scholar] [CrossRef]
- Yip, B.H.K.; Sheng, X.T.; Chan, V.W.Y.; Wong, L.H.L.; Lee, S.W.Y.; Abraham, A.A. ‘Let’s talk about sex’—A knowledge, attitudes and practice study among paediatric nurses about teen sexual health in Hong Kong. J. Clin. Nurs. 2015, 24, 2591–2600. [Google Scholar] [CrossRef]
- Hong Kong Advisory Council on AIDS. Recommended HIV/AIDS Strategies for Hong Kong 2012–2016. 2012. Available online: http://www.chp.gov.hk/files/pdf/spp_g253.pdf (accessed on 20 May 2019).
- Hankivsky, O.; Grace, D.; Hunting, G.; Giesbrecht, M.; Fridkin, A.; Rudrum, S.; Ferlatte, O.; Clark, N. An intersectionality-based policy analysis framework: Critical reflections on a methodology for advancing equity. Int. J. Equity Health 2014, 13, 119. [Google Scholar] [CrossRef]
- Chan, R.C.H.; Mak, W.W.S. Cognitive, regulatory, and interpersonal mechanisms of HIV stigma on the mental and social health of men who have sex with men living with HIV. Am. J. Men’s Health 2019, 13. [Google Scholar] [CrossRef]
- Ferlatte, O.; Salway, T.; Trussler, T.; Oliffe, J.L.; Gilbert, M. Combining intersectionality and syndemic theory to advance understandings of health inequities among Canadian gay, bisexual and other men who have sex with men. Crit. Public Health 2018, 28, 509–521. [Google Scholar] [CrossRef]
- Watkins-Hayes, C. Intersectionality and the sociology of HIV/AIDS: Past, present, and future research directions. Annu. Rev. Sociol. 2014, 40, 431–457. [Google Scholar] [CrossRef]
- Mustanski, B.; Phillips, G.; Ryan, D.T.; Swann, G.; Kuhns, L.; Garofalo, R. Prospective effects of a syndemic on HIV and STI incidence and risk behaviors in a cohort of young men who have sex with men. AIDS Behav. 2017, 21, 845–857. [Google Scholar] [CrossRef]
- Mustanski, B.; Andrews, R.; Herrick, A.; Stall, R.; Schnarrs, P.W. A syndemic of psychosocial health disparities and associations with risk for attempting suicide among young sexual minority men. Am. J. Public Health 2014, 104, 287–294. [Google Scholar] [CrossRef]
- Chou, K.L. Assessing Chinese adolescents’ social support: The multidimensional scale of perceived social support. Personal. Individ. Differ. 2000, 28, 299–307. [Google Scholar] [CrossRef]
- Liang, J.; Wu, S.C.; Krause, N.M.; Chiang, T.L.; Wu, H.Y. The structure of the mental health inventory among Chinese in Taiwan. Med. Care 1992, 30, 659–676. [Google Scholar] [CrossRef] [PubMed]
- Rojas, P.; Huang, H.; Li, T.; Ravelo, G.J.; Sanchez, M.; Dawson, C.; Brook, J.; Kanamori, M.; De La Rosa, M. Sociocultural determinants of risky sexual behaviors among adult Latinas: A longitudinal study of a community-based sample. Int. J. Environ. Res. Public Health 2016, 13, 1164. [Google Scholar] [CrossRef] [PubMed]
- Crosby, R.A.; DiClemente, R.J.; Salazar, L.F.; Wingood, G.M.; McDermott-Sales, J.; Young, A.M.; Rose, E. Predictors of consistent condom use among young African American women. AIDS Behav. 2013, 17, 865–871. [Google Scholar] [CrossRef] [PubMed]
- Cohen, M.S.; Chen, Y.Q.; McCauley, M.; Gamble, T.; Hosseinipour, M.C.; Kumarasamy, N.; Hakim, J.G.; Kumwenda, J.; Grinsztejn, B.; Pilotto, J.H. Antiretroviral therapy for the prevention of HIV-1 transmission. N. Engl. J. Med. 2016, 375, 830–839. [Google Scholar] [CrossRef] [PubMed]
| Demographic Characteristics | n (%)/M (SD) |
|---|---|
| Gender | |
| Male | 277 (95.8%) |
| Female | 12 (4.2%) |
| Age | 41.8 years (11.1 years) |
| Ethnicity | |
| Chinese | 271 (94.8%) |
| South Asian | 6 (2.1%) |
| Caucasian | 6 (2.1%) |
| Others | 3 (1.0%) |
| Education | |
| Secondary education or less | 138 (48.3%) |
| Tertiary education | 133 (46.5%) |
| Employment status | |
| Full-time employment | 183 (63.3%) |
| Part-time or irregular employment | 46 (15.9%) |
| Unemployed | 36 (12.5%) |
| Others | 24 (8.3%) |
| Marital status | |
| Single | 194 (67.4%) |
| Cohabiting/Married | 76 (26.4%) |
| Separated/Divorced/Widowed | 20 (6.9%) |
| Sexual orientation | |
| Heterosexual | 68 (23.7%) |
| Gay | 141 (49.1%) |
| Bisexual | 70 (24.4%) |
| Questioning | 8 (2.8%) |
| Length of being diagnosed with HIV infection | 5.25 years (4.70 years) |
| Use of antiretroviral therapy | |
| Yes | 254 (90.1%) |
| No | 28 (9.9%) |
| Number of psychosocial syndemic problem(s) | |
| 0 | 86 (29.6%) |
| 1 | 126 (43.3%) |
| 2 | 54 (18.6%) |
| 3 | 21 (7.2%) |
| 4 | 4 (1.4%) |
| Condom use with steady partners | |
| Consistent condom use | 28 (25.9%) |
| Inconsistent condom use | 80 (74.1%) |
| Condom use with casual partners | |
| Consistent condom use | 20 (18.7%) |
| Inconsistent condom use | 87 (81.3%) |
| Variable | All Participants (N = 291) | Had HIV-Related Discrimination (n = 94) | Did not Have HIV-Related Discrimination (n = 197) | Independent Samples t-Test | Pearson Correlation Coefficients | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Skewness | Kurtosis | Mean (SD) | Mean (SD) | t-Value | Cohen’s d | 1 | 2 | 3 | 4 | |
| 1. Depression (1–6) | 2.41 | 0.90 | 0.79 | 1.34 | 2.70 (0.95) | 2.28 (0.84) | 3.81 ** | 0.47 | - | |||
| 2. Anxiety (1–6) | 2.57 | 0.87 | 0.37 | −0.06 | 2.76 (0.82) | 2.49 (0.88) | 2.50 * | 0.32 | 0.78 ** | - | ||
| 3. Social isolation (1–7) | 3.27 | 1.08 | 0.52 | 0.36 | 3.57 (1.14) | 3.12 (1.02) | 3.39 ** | 0.42 | 0.31 ** | 0.32 ** | - | |
| 4. Self-stigma (1–6) | 3.82 | 1.16 | −0.34 | −0.53 | 4.00 (1.19) | 3.74 (1.14) | 1.80 | 0.22 | 0.36 ** | 0.35 ** | 0.31 ** | - |
| Variable | Psychosocial Syndemics (N = 291) | Inconsistent Condom Use with Steady Partners (n = 108) | Inconsistent Condom Use with Casual Partners (n = 107) | |||
|---|---|---|---|---|---|---|
| IRR | (95% CI) | AOR | (95% CI) | AOR | (95% CI) | |
| HIV-related discrimination | ||||||
| Yes | 1.47 ** | (1.14, 1.89) | 5.40 * | (1.09, 26.70) | 3.24 | (0.70, 15.00) |
| No (reference category) | 1.00 | 1.00 | 1.00 | |||
| Psychosocial syndemics | - | - | 3.09 * | (1.22, 7.82) | 0.95 | (0.48, 1.90) |
| Gender | ||||||
| Male | 1.73 | (0.79, 3.78) | 14.54 | (0.40, 524.99) | - | - |
| Female (reference category) | 1.00 | 1.00 | - | - | ||
| Age | 1.00 | (0.99, 1.01) | 0.98 | (0.89, 1.07) | 1.05 | (0.97, 1.13) |
| Ethnicity | ||||||
| Chinese | 1.05 | (0.58, 1.89) | 0.32 | (0.02, 4.74) | - | - |
| Ethnic minority (reference category) | 1.00 | 1.00 | - | - | ||
| Education | ||||||
| Secondary education or less (reference category) | 1.00 | 1.00 | 1.00 | |||
| Tertiary education | 0.76 | (0.58, 1.00) | 2.62 | (0.52, 13.20) | 0.99 | (0.23, 4.36) |
| Employment status | ||||||
| Full-/part-time employment | 0.94 | (0.69, 1.27) | 0.30 | (0.05, 1.91) | 1.90 | (0.37, 9.68) |
| Not in employment | 1.00 | 1.00 | 1.00 | |||
| Marital status | ||||||
| Single (reference category) | 1.00 | 1.00 | 1.00 | |||
| Cohabiting/Married | 0.88 | (0.64, 1.22) | 0.11 * | (0.02, 0.58) | 0.24 * | (0.06, 0.99) |
| Separated/Divorced/Widowed | 0.98 | (0.57, 1.69) | 0.09 | (0.01, 1.19) | - | - |
| Sexual orientation | ||||||
| Heterosexual | 1.06 | (0.76, 1.50) | 0.13 * | (0.02, 0.94) | 1.33 | (.13, 13.79) |
| Sexual minority (reference category) | 1.00 | 1.00 | 1.00 | |||
| Length of being diagnosed with HIV infection | 1.00 | (1.00, 1.00) | 1.00 | (0.99, 1.02) | 0.98 * | (0.97, 1.00) |
| Antiretroviral medication use | ||||||
| Yes | 1.37 | (0.85, 2.20) | 3.98 | (0.38, 41.80) | 1.61 | (0.14, 18.41) |
| No (reference category) | 1.00 | 1.00 | 1.00 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, R.C.H.; Operario, D.; Mak, W.W.S. Effects of HIV-Related Discrimination on Psychosocial Syndemics and Sexual Risk Behavior among People Living with HIV. Int. J. Environ. Res. Public Health 2020, 17, 1924. https://doi.org/10.3390/ijerph17061924
Chan RCH, Operario D, Mak WWS. Effects of HIV-Related Discrimination on Psychosocial Syndemics and Sexual Risk Behavior among People Living with HIV. International Journal of Environmental Research and Public Health. 2020; 17(6):1924. https://doi.org/10.3390/ijerph17061924
Chicago/Turabian StyleChan, Randolph C. H., Don Operario, and Winnie W. S. Mak. 2020. "Effects of HIV-Related Discrimination on Psychosocial Syndemics and Sexual Risk Behavior among People Living with HIV" International Journal of Environmental Research and Public Health 17, no. 6: 1924. https://doi.org/10.3390/ijerph17061924
APA StyleChan, R. C. H., Operario, D., & Mak, W. W. S. (2020). Effects of HIV-Related Discrimination on Psychosocial Syndemics and Sexual Risk Behavior among People Living with HIV. International Journal of Environmental Research and Public Health, 17(6), 1924. https://doi.org/10.3390/ijerph17061924





