The Effect of Ultraviolet B Irradiation Compared with Oral Vitamin D Supplementation on the Well-being of Nursing Home Residents with Dementia: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
3. Results
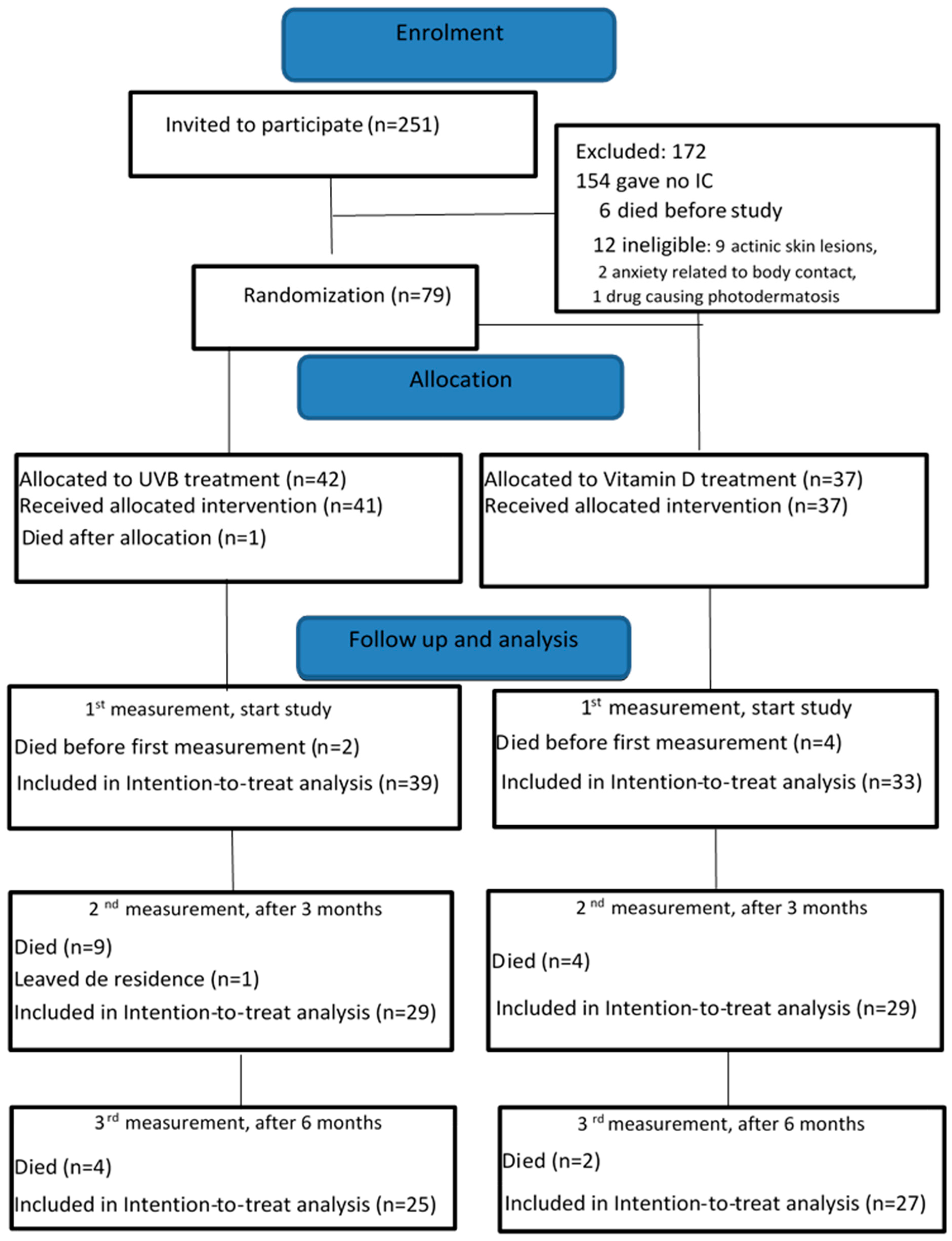
3.1. Participants
3.2. Adherence of Nursing Home Residents to the Intervention
3.3. Effect of UVB on the Outcome Variables
3.3.1. Effect of UVB Treatment on Well-Being
3.3.2. Effect of UVB Treatment on Secondary Outcomes
3.3.3. Harmful or Adverse Events
3.4. Additional (Sensitivity) Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| 3 Months (n = 58) | 6 Months (n = 52) | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimated Mean | Adjusted MD | p-Value | Estimated Mean | Adjusted MD | p-Value | Pg | Pt | Pgt | |
| Score (95% CI) | (95% CI) | Score (95% CI) | (95% CI) | ||||||
| CMAI total score | 0.847 | 0.175 | 0.155 | ||||||
| UVB | 49.3 (43.9, 54.7) | 3.3 (−3.6, 10.2) | 0.343 | 49.2 (43.5–54.8) | −2.2 (−9.4, 5.0) | 0.554 | |||
| VD | 46.0 (41.7, 50.3) | 51.3 (46.7–55.8) | |||||||
| Cornell scale for depression | 0.483 | 0.032 | 0.260 | ||||||
| UVB | 8.5 (6.4, 10.7) | 2.1 (−1.9, 4.6) | 0.200 | 10.1 (8.0–12.2) | −0.5 (−2.7, 3.6) | 0.775 | |||
| VD | 7.1 (5.0, 9.1) | 11.0 (8.8, 12.9) | |||||||
| Care relationship (QUAL) | 0.575 | 0.617 | 0.285 | ||||||
| UVB | 6.0 (5.4, 6.7) | −0.5 (− 1.3, 1.3) | 0.259 | 6.2 (5.5, 6.8) | 0.3 (−0.5, 1.2) | 0.820 | |||
| VD | 6.5 (6.0, 7.0) | 6.1 (5.6, 6.7) | |||||||
| Positive affect (QUAL.) | 0.827 | 0.602 | 0.171 | ||||||
| UVB | 8.8 (7.8, 9.9) | 0.4 (−0.9, 1.6) | 0.561 | 8.5 (7.5, 9.6) | 0.0 (−1.3, 1.3) | 0.354 | |||
| VD | 8.5 (7.7, 9.3) | 9.1 (8.3, 9.9) | |||||||
| Negative affect (QUAL.) | 0.945 | 0.337 | 0.218 | ||||||
| UVB | 3.6 (3.2, 4.0) | 0.2 (−0.3, 0.7) | 0.452 | 3.3 (2.8,3.7) | −0.2 (−0.7, 0.3) | 0.406 | |||
| VD | 3.4 (3.1, 3.7) | 3.5 (3.2, 3.8) | |||||||
| Restless/Tense (QUAL.) | 0.969 | 0.462 | 0.012 | ||||||
| UVB | 4.8 (4.0, 5.6) | −0.6 (−1.7, 0.4,) | 0.207 | 5.7 (4.8, 6.5) | 1.2 (0.2, 2.3,) | 0.025 | |||
| VD | 5.4 (4.8, 6.0) | 4.5 (3.7, 5.1) | |||||||
| Social relations (QUAL.) | 0.939 | 0.857 | 0.324 | ||||||
| UVB | 5.9 (5.2, 6.7) | 0.3 (−0.6, 1.2) | 0.484 | 5.6 (4.9, 6.4) | −0.3 (−1.2, 0.7) | 0.573 | |||
| VD | 5.6 (5.1, 6.2) | 5.9 (5.3, 6.5) | |||||||
| Social isolation (QUAL.) | 0.292 | 0.557 | 0.546 | ||||||
| UVB | 6.0 (5.2, 6.8) | −0.6 (−1.6, 0.4) | 0.223 | 6.0 (5.2, 6.8) | −0.3 (−1.3, 0.7) | 0.596 | |||
| VD | 6.6 (6.0, 7.2) | 6.2 (5.6, 6.7) | |||||||
| 25(OH)D3 | 0.039 | 0.237 | 0.005 | ||||||
| UVB | 67.6 (59.1, 76.0) | −5.1 (−15.8, 5.6) | 0.344 | 64.1 (54.9, 73.3) | −16.8 (−28.0, −5.5) | 0.004 | |||
| VD | 72.7 (66.5, 78.9) | 80.7 (74.5, 87.1) | |||||||
References
- Lindqvist, P.G.; Epstein, E.; Nielsen, K.; Landin-Olsson, M.; Ingvar, C.; Olsson, H. Avoidance of sun exposure as a risk factor for major causes of death: A competing risk analysis of the Melanoma in Southern Sweden cohort. J. Intern. Med. 2016, 280, 375–387. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Vitamin D for health and in chronic kidney disease. Semin. Dial. 2005, 18, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Edstrom, D.W.; Linder, J.; Wennersten, G.; Brismar, K.; Ros, A.M. Phototherapy with ultraviolet radiation: A study of hormone parameters and psychological effects. J. Eur. Acad. Dermatol. Venereol. 2010, 24, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Pudikov, I.V.; Dorokhov, V.B. The special physiological importance of the UV-A spectrum for successful phototherapy. Hum. Physiol. 2012, 38, 634–639. [Google Scholar] [CrossRef]
- Taylor, S.L.; Kaur, M.; LoSicco, K.; Willard, J.; Camacho, F.; O’Rourke, K.S.; Feldman, S.R. Pilot study of the effect of ultraviolet light on pain and mood in fibromyalgia syndrome. J. Altern. Complement. Med. 2009, 15, 15–23. [Google Scholar] [CrossRef]
- Gambichler, T.; Bader, A.; Vojvodic, M.; Avermaete, A.; Schenk, M.; Altmeyer, P.; Hoffmann, K. Plasma levels of opioid peptides after sunbed exposures. Br. J. Dermatol. 2002, 147, 1207–1211. [Google Scholar] [CrossRef]
- Knippenberg, S.; Damoiseaux, J.; Bol, Y.; Hupperts, R.; Taylor, B.V.; Ponsonby, A.L.; Dwyer, T.; Simpson, S.; van der Mei, I.A. Higher levels of reported sun exposure, and not vitamin D status, are associated with less depressive symptoms and fatigue in multiple sclerosis. Acta Neurol. Scand. 2014, 129, 123–131. [Google Scholar] [CrossRef]
- Meffert, H.; Scherf, H.-P.; Piazena, H. Systemic effects of infrared and ultraviolet irradiations—A prospective, placebo-controlled intra-individual comparison. German Systemische wirkungen infraroter und ultravioletter strahlen: Ein prospektiver, plazebokontrollierter, intraindividueller vergleich. Aktuelle Dermatol. 2006, 32, 249–255. [Google Scholar]
- Veleva, B.I.; van Bezooijen, R.L.; Chel, V.G.M.; Numans, M.E.; Caljouw, M.A.A. Effect of ultraviolet light on mood, depressive disorders and well-being. Photodermatol. Photoimmunol. Photomed. 2018, 34, 288–297. [Google Scholar] [CrossRef]
- Holick, M.F. Biological Effects of Sunlight, Ultraviolet Radiation, Visible Light, Infrared Radiation and Vitamin D for Health. Anticancer Res. 2016, 36, 1345–1356. [Google Scholar]
- Chel, V.G.; Ooms, M.E.; Pavel, S.; de Gruijl, F.; Brand, A.; Lips, P. Prevention and treatment of vitamin D deficiency in Dutch psychogeriatric nursing home residents by weekly half-body UVB exposure after showering: A pilot study. Age Ageing 2011, 40, 211–214. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Broe, K.E.; Chen, T.C.; Weinberg, J.; Bischoff-Ferrari, H.A.; Holick, M.F.; Kiel, D.P. A higher dose of vitamin d reduces the risk of falls in nursing home residents: A randomized, multiple-dose study. J. Am. Geriatr. Soc. 2007, 55, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Juzeniene, A.; Moan, J. Beneficial effects of UV radiation other than via vitamin D production. Dermatoendocrinol 2012, 4, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Chenoweth, L.; King, M.T.; Jeon, Y.H.; Brodaty, H.; Stein-Parbury, J.; Norman, R.; Haas, M.; Luscombe, G. Caring for Aged Dementia Care Resident Study (CADRES) of person-centred care, dementia-care mapping, and usual care in dementia: A cluster-randomised trial. Lancet Neurol. 2009, 8, 317–325. [Google Scholar] [CrossRef]
- Morley, J.E.; Vellas, B.; van Kan, G.A.; Anker, S.D.; Bauer, J.M.; Bernabei, R.; Cesari, M.; Chumlea, W.C.; Doehner, W.; Evans, J.; et al. Frailty consensus: A call to action. J. Am. Med. Dir. Assoc. 2013, 14, 392–397. [Google Scholar] [CrossRef]
- Klapwijk, M.S.; Caljouw, M.A.; Pieper, M.J.; van der Steen, J.T.; Achterberg, W.P. Characteristics Associated with Quality of Life in Long-Term Care Residents with Dementia: A Cross-Sectional Study. Dement. Geriatr. Cogn. Disord. 2016, 42, 186–197. [Google Scholar] [CrossRef]
- Steptoe, A.; Deaton, A.; Stone, A.A. Subjective wellbeing, health, and ageing. Lancet 2015, 385, 640–648. [Google Scholar] [CrossRef]
- Hendriks, S.A.; Smalbrugge, M.; Galindo-Garre, F.; Hertogh, C.M.; van der Steen, J.T. From admission to death: Prevalence and course of pain, agitation, and shortness of breath, and treatment of these symptoms in nursing home residents with dementia. J. Am. Med. Dir. Assoc. 2015, 16, 475–481. [Google Scholar] [CrossRef]
- He, S.Y.; McCulloch, C.E.; Boscardin, W.J.; Chren, M.M.; Linos, E.; Arron, S.T. Self-reported pigmentary phenotypes and race are significant but incomplete predictors of Fitzpatrick skin phototype in an ethnically diverse population. J. Am. Acad. Dermatol. 2014, 71, 731–737. [Google Scholar] [CrossRef]
- Evaluation of Dietary Reference Values for Vitamin D; Health Council of the Netherlands: The Hague, The Netherlands, 2012.
- Cohen-Mansfield, J.; Marx, M.S.; Rosenthal, A.S. A description of agitation in a nursing home. J. Gerontol. 1989, 44, M77–M84. [Google Scholar] [CrossRef]
- Miller, R.J.; Snowdon, J.; Vaughan, R. The use of the Cohen-Mansfield Agitation Inventory in the assessment of behavioral disorders in nursing homes. J. Am. Geriatr. Soc. 1995, 43, 546–549. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, G.S.; Abrams, R.C.; Young, R.C.; Shamoian, C.A. Cornell Scale for Depression in Dementia. Biol. Psychiatry 1988, 23, 271–284. [Google Scholar] [CrossRef]
- Ettema, T.P.; Droes, R.M.; de Lange, J.; Mellenbergh, G.J.; Ribbe, M.W. QUALIDEM: Development and evaluation of a dementia specific quality of life instrument. Scalability, reliability and internal structure. Int. J. Geriatr. Psychiatry 2007, 22, 549–556. [Google Scholar] [CrossRef] [PubMed]
- West, B.T. Analyzing longitudinal data with the linear mixed models procedure in SPSS. Eval. Health Prof. 2009, 32, 207–228. [Google Scholar] [CrossRef] [PubMed]
- Gambichler, T.; Bader, A.; Vojvodic, M.; Bechara, F.G.; Sauermann, K.; Altmeyer, P.; Hoffmann, K. Impact of UVA exposure on psychological parameters and circulating serotonin and melatonin. BMC Dermatol. 2002, 2, 6. [Google Scholar] [CrossRef][Green Version]
- Mjorud, M.; Rosvik, J.; Rokstad, A.M.; Kirkevold, M.; Engedal, K. Variables associated with change in quality of life among persons with dementia in nursing homes: A 10 months follow-up study. PLoS ONE 2014, 9, e115248. [Google Scholar] [CrossRef]
- Alpert, J.S. Sunshine: Clinical friend or foe? Am. J. Med. 2010, 123, 291–292. [Google Scholar] [CrossRef]
- Cui, X.; Gooch, H.; Petty, A.; McGrath, J.J.; Eyles, D. Vitamin D and the brain: Genomic and non-genomic actions. Mol. Cell. Endocrinol. 2017, 453, 131–143. [Google Scholar] [CrossRef]
- Slominski, A.; Wortsman, J. Neuroendocrinology of the skin. Endocr. Rev. 2000, 21, 457–487. [Google Scholar] [CrossRef]
- Slominski, A.; Wortsman, J.; Tobin, D.J. The cutaneous serotoninergic/melatoninergic system: Securing a place under the sun. FASEB J. 2005, 19, 176–194. [Google Scholar] [CrossRef]
- Skobowiat, C.; Postlethwaite, A.E.; Slominski, A.T. Skin Exposure to Ultraviolet B Rapidly Activates Systemic Neuroendocrine and Immunosuppressive Responses. Photochem. Photobiol. 2017, 93, 1008–1015. [Google Scholar] [CrossRef] [PubMed]
- Slominski, A.T.; Zmijewski, M.A.; Plonka, P.M.; Szaflarski, J.P.; Paus, R. How UV Light Touches the Brain and Endocrine System Through Skin, and Why. Endocrinology 2018, 159, 1992–2007. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M.; Endocrine, S. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Ultraviolet B Radiation: The Vitamin D Connection. Adv. Exp. Med. Biol. 2017, 996, 137–154. [Google Scholar] [PubMed]
- Durvasula, S.; Gies, P.; Mason, R.S.; Chen, J.S.; Henderson, S.; Seibel, M.J.; Sambrook, P.N.; March, L.M.; Lord, S.R.; Kok, C.; et al. Vitamin D response of older people in residential aged care to sunlight-derived ultraviolet radiation. Arch. Osteoporos. 2014, 9, 197. [Google Scholar] [CrossRef]
| Variable | UVB | Vitamin D | p-Value |
|---|---|---|---|
| Gender %,(n) | 0.20 a | ||
| male | 24 (10) | 38 (14) | |
| Female | 76 (31) | 62 (23) | |
| Age in years, mean (SD) | 84.2 (79.5–87.5) | 83.6 (77.5–88.5) | 0.74 b |
| Fitzpatrick skin scale %,(n) | 0.90 c | ||
| 1. always burns easily, never tans | 0 | 3 (1) | |
| 2. always burns easily, tans slightly | 66 (27) | 62 (23) | |
| 3. burns moderately, tans gradually | 30 (12) | 32 (12) | |
| 4. burns minimally, tans moderately | 0 | 0 | |
| 5. rarely burns, tans profusely | 5 (2) | 0 | |
| 6. never burns, tans profusely | 0 | 3 (1) | |
| Dementia severity, mean BANS-S (SD) | 15.1 (4.3) | 16.6 (5.7) | 0.20 b |
| Agitation (median CMAI, IQR) | 40.0 (30.3–62.5) | 41.0 (30.5–61.0) | 0.82 d |
| Cornell Scale For Depression (Median, IQR) | 9.5 (4.9–13.0) | 9.5 (5.0–12.0) | 0.88 d |
| QUALIDEM (Median, IQR) | |||
| A. Care relationship | 6.0 (4.0–8.0) | 7.0 (5.0–8.5) | 0.28 d |
| B. Positive affect | 10.0 (7.5–12.0) | 9.0 (8.0–11.5) | 0.63 |
| C. Negative affect | 3.0 (3.0–4.0) | 4.0 (3.0–4.0) | 0.98 |
| D. Restless/tense behavior | 6.0 (2.5–8.0) | 6.0 (3.0–8.0) | 0.91 |
| E. Social relations | 6.0 (4.5–8.0) | 6.0 (4.0–7.0) | 0.45 |
| G. Social isolation | 6.5 (4.0–9.0) | 8.0 (5.0–9.0) | 0.52 |
| Blood tests (Median, IQR)) # | |||
| Creatinine (µmol/L) | 73.0 (61.0–982.0) | 72.5 (56.0–988.2) | 0.82 d |
| Calcium (mmol/L) | 2.3 (2.3–92.5) | 2.3 (2.3–92.4) | 0.81 |
| Phosphate (mmol/L) | 1.1 (1.0–91.1) | 1.1 (0.9–91.3) | 0.60 |
| Alkaline phosphatase (U/I) | 86.4 (65.3–9116.6) | 82.4 (70.0–997.9) | 0.96 |
| 25(OH)D3 (nmo/L) | 66.4 (53.6–978.7) | 86.4 (65.1–999.7) | 0.04 |
| Parathyroid hormone (pmol/L) | 5.7 (3.0–97.6) | 3.5 (2.7–96.5) | 0.24 |
| 3 Months (n = 58) | 6 Months (n = 52) | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimated Mean | Adjusted MD | p-Value | Estimated Mean | Adjusted MD | p-Value | Pg | Pt | Pgt | |
| Score (95% CI) | (95% CI) | Score (95% CI) | (95% CI) | ||||||
| CMAI total score | 0.431 | 0.076 | 0.258 | ||||||
| UVB | 49.4 (44.7, 54.0) | 4.4 (−2.3, 11.2) | 0.194 | 50.6 (45.7, 55.5) | −0.2 (−6.8, 7.2) | 0.953 | |||
| VD | 45.0 (41.0, 49.8.2) | 50.4 (45.4, 55.5) | |||||||
| Cornell scale for depression | 0.982 | 0.014 | 0.246 | ||||||
| UVB | 8.5 (6.4, 10.7) | 1.3 (−1.9, 4.6) | 0.412 | 10.1 (8.0, 12.2) | −1.3 (−4.5, 1.9,) | 0.427 | |||
| VD | 7.2 (4.8, 9.7) | 11.4 (9.0, 13.8) | |||||||
| Care relationship (QUAL) | 0.776 | 0.421 | 0.307 | ||||||
| UVB | 6.2 (5.8, 7.0) | −0.2 (−1.0, 0.6) | 0.684 | 6.3 (5.7, 6.7) | 0.3 (−0.5, 1.2) | 0.402 | |||
| VD | 6.4 (5.4, 6.5) | 6.3 (5.7, 6.7) | |||||||
| Positive affect (QUAL.) | 0.698 | 0.363 | 0.646 | ||||||
| UVB | 8.8 (7.9, 9.7) | 0.4 (−0.9, 1.6) | 0.555 | 8.9 (8.0, 9.9) | 0.0 (−1.3, 1.3) | 0.947 | |||
| VD | 8.4 (7.5, 9.3) | 8.9 (8.0, 9.8) | |||||||
| Negative affect (QUAL.) | 0.303 | 0.507 | 0.866 | ||||||
| UVB | 3.4 (3.0, 3.7) | −0.2 (−0.7, 0.3) | 0.483 | 3.3 (3.0, 3.7) | −0.2 (−0.7, 0.3) | 0.377 | |||
| VD | 3.6 (3.2, 3.9) | 3.5 (3.1, 3.8) | |||||||
| Restless/Tense (QUAL.) | 0.937 | 0.520 | 0.003 | ||||||
| UVB | 4.6 (3.9, 5.1) | −1.1 (−2.1, −0.1,) | 0.025 | 5.5 (4.8, 6.2) | 1.1 (0.1, 2.1,) | 0.042 | |||
| VD | 5.7 (5.0, 6.4) | 4.4 (3.7, 5.1) | |||||||
| Social relations (QUAL.) | 0.960 | 0.920 | 0.763 | ||||||
| UVB | 5.7 (5.1, 6.3) | −0.1 (−1.0, 0.8) | 0.813 | 5.8 (5.1, 6.5) | 0.1 (−0.8, 1.0) | 0.879 | |||
| VD | 5.8 (5.1, 6.4) | 5.7 (5.1, 6.4) | |||||||
| Social isolation (QUAL.) | 0.329 | 0.441 | 0.158 | ||||||
| UVB | 5.9 (5.3, 6.6) | −0.8 (−1.7, 0.2) | 0.104 | 6.2 (5.5,6.8) | 0.0 (−1.0, 1.0) | 0.988 | |||
| VD | 6.7 (6.1, 7.4) | 6.2 (5.5, 6.8) | |||||||
| 25(OH)D3 | 0.003 | 0.141 | 0.001 | ||||||
| UVB | 66.3 (59.1, 73.5) | −9.3 (−19.4, 1.0) | 0.073 | 62.7 (54.9, 70.5) | −21.9 (−32.6, −11.2) | 0.000 | |||
| VD | 75.6 (69.0, 82.1) | 84.6 (77.9, 91.3) | |||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veleva, B.I.; Caljouw, M.A.A.; van der Steen, J.T.; Mertens, B.J.A.; Chel, V.G.M.; Numans, M.E. The Effect of Ultraviolet B Irradiation Compared with Oral Vitamin D Supplementation on the Well-being of Nursing Home Residents with Dementia: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 1684. https://doi.org/10.3390/ijerph17051684
Veleva BI, Caljouw MAA, van der Steen JT, Mertens BJA, Chel VGM, Numans ME. The Effect of Ultraviolet B Irradiation Compared with Oral Vitamin D Supplementation on the Well-being of Nursing Home Residents with Dementia: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2020; 17(5):1684. https://doi.org/10.3390/ijerph17051684
Chicago/Turabian StyleVeleva, Bistra I., Monique A. A. Caljouw, Jenny T. van der Steen, Bart J. A. Mertens, Victor G. M. Chel, and Mattijs E. Numans. 2020. "The Effect of Ultraviolet B Irradiation Compared with Oral Vitamin D Supplementation on the Well-being of Nursing Home Residents with Dementia: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 17, no. 5: 1684. https://doi.org/10.3390/ijerph17051684
APA StyleVeleva, B. I., Caljouw, M. A. A., van der Steen, J. T., Mertens, B. J. A., Chel, V. G. M., & Numans, M. E. (2020). The Effect of Ultraviolet B Irradiation Compared with Oral Vitamin D Supplementation on the Well-being of Nursing Home Residents with Dementia: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 17(5), 1684. https://doi.org/10.3390/ijerph17051684





