Evidence of the Importance of Dietary Habits Regarding Depressive Symptoms and Depression
Abstract
1. Introduction
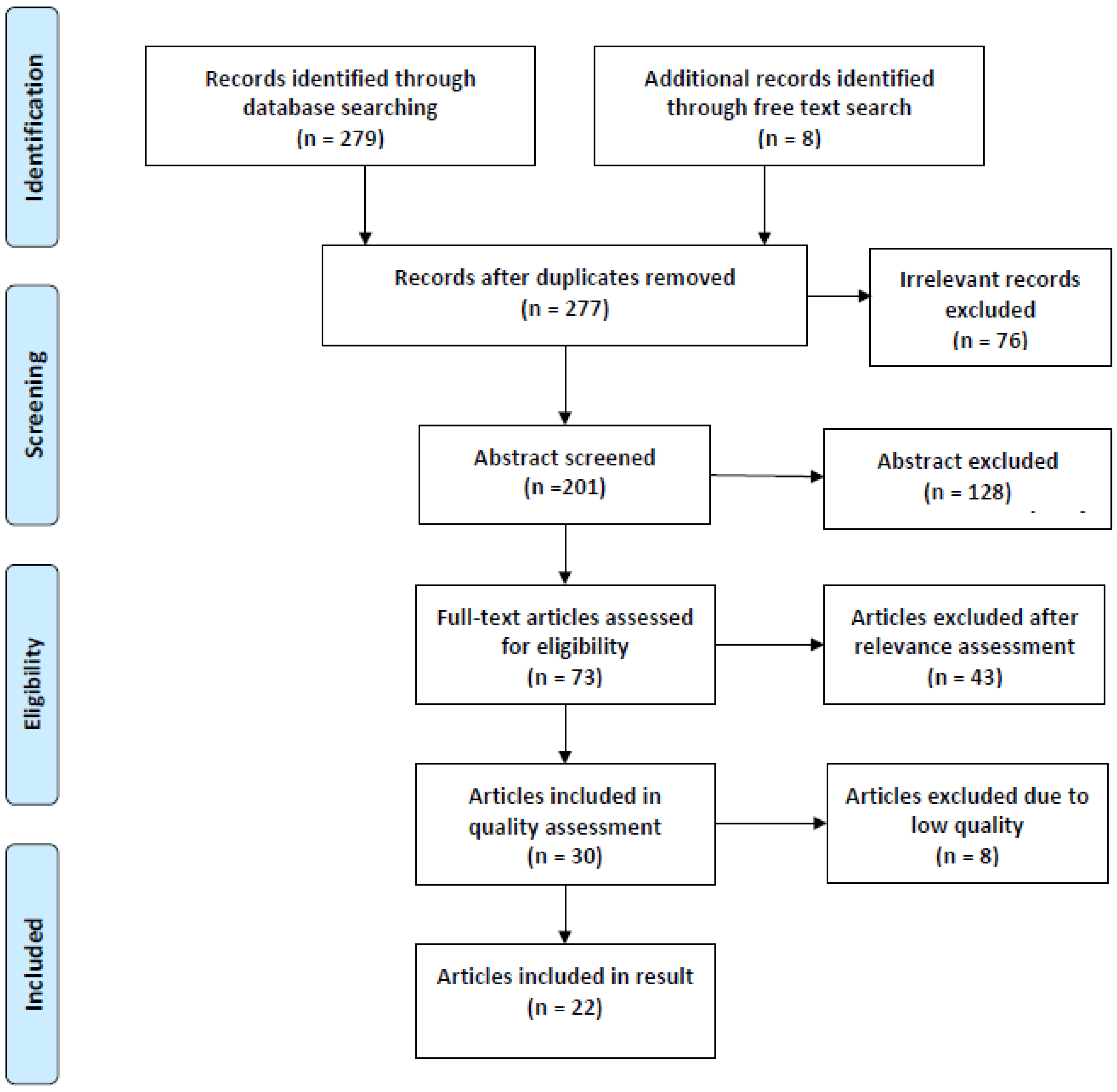
2. Materials and Methods
3. Results
3.1. Subsection
- Adherence to dietary recommendations and risk of depression;
- Pro-inflammatory diet and depression;
- Dietary intake of folic acid, magnesium, and fatty acids linked to depression;
- Dietary choices and risk of depression;
- Causal link between diet and depression.
3.1.1. Adherence to Dietary Recommendations and Risk of Depression
3.1.2. Pro-Inflammatory Diet and Depression
3.1.3. Dietary Intake of Micronutrients Linked to Depression
3.1.4. Dietary Choice and Risk of Depression
3.1.5. Causal Link between Diet and Depression
4. Discussion
5. Conclusions
- -
- Advice should be given to people regarding health-promoting diets such as increasing the intake of vegetables, fruits, fish, nuts, legumes, olive oil and excluding or severely restricting the intake of processed foods such as sausages, juices, soft drinks, and sweets to promote and prevent depression (strong evidence value).
- -
- The diet’s content of micronutrients such as magnesium, folic acid, and various B vitamins is of importance for depression (moderately strong evidence value).
- -
- The public health professionals may advantageously use MI as an approach and strategy in the guiding work to motivate and support dietary changes in depression (limited evidence value). Resources should be used to help people maintain a healthy diet for preventive purposes for depression (strong evidence value).
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Depression; World Health Organization: Geneva, Switzerland, 2018; Available online: https://www.who.int/news-room/fact-sheets/detail/depression (accessed on 12 January 2020).
- WHO. Preventing depression in the WHO European Region; World Helth Organization: Geneva, Switzerland, 2016; Available online: http://www.euro.who.int/en/health-topics/noncommunicable-diseases/mental-health/publications/2016/preventing-depression-in-the-who-european-region-2016 (accessed on 12 January 2020).
- Berk, M.; Sarris, J.; Coulson, C.E.; Jacka, F.N. Lifestyle management of unipolar depression. Acta Psychiatr. Scandinavica. Suppl. 2013, 127, 38–54. [Google Scholar] [CrossRef]
- Assosciation, U.N. Agenda 2030. Available online: https://www.un.org/sustainabledevelopment/sustainable-development-goals/ (accessed on 12 January 2020).
- Hopewell, S.; Loudon, K.; Clarke, M.J.; Oxman, A.D.; Dickersin, K. Publication bias in clinical trials due to statistical significance or direction of trial results. Cochrane Database Syst. Rev. 2009, Mr000006. [Google Scholar] [CrossRef]
- Haynes, R.B.; Devereaux, P.J.; Guyatt, G.H. Physicians’ and patients’ choices in evidence based practice. BMJ (Clin. Res. Ed.) 2002, 324, 1350. [Google Scholar] [CrossRef] [PubMed]
- Golder, S.; Loke, Y.K.; Bland, M. Meta-analyses of adverse effects data derived from randomised controlled trials as compared to observational studies: Methodological overview. Plos Med. 2011, 8, e1001026. [Google Scholar] [CrossRef] [PubMed]
- Atkins, D.; Best, D.; Briss, P.A.; Eccles, M.; Falck-Ytter, Y.; Flottorp, S.; Guyatt, G.H.; Harbour, R.T.; Haugh, M.C.; Henry, D.; et al. Grading quality of evidence and strength of recommendations. BMJ (Clin. Res. Ed.) 2004, 328, 1490. [Google Scholar]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Boudin, F.; Nie, J.Y.; Bartlett, J.C.; Grad, R.; Pluye, P.; Dawes, M. Combining classifiers for robust PICO element detection. BMC Med. Inform. Decis. Mak. 2010, 10, 29. [Google Scholar] [CrossRef] [PubMed]
- Rosen, M. The aprotinin saga and the risks of conducting meta-analyses on small randomised controlled trials—A critique of a Cochrane review. BMC Health Serv. Res. 2009, 9, 34. [Google Scholar] [CrossRef]
- Moher, D.; Tetzlaff, J.; Tricco, A.C.; Sampson, M.; Altman, D.G. Epidemiology and reporting characteristics of systematic reviews. Plos Med. 2007, 4, e78. [Google Scholar] [CrossRef]
- Shea, B.J.; Grimshaw, J.M.; Wells, G.A.; Boers, M.; Andersson, N.; Hamel, C.; Porter, A.C.; Tugwell, P.; Moher, D.; Bouter, L.M. Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Med. Res. Methodol. 2007, 7, 10. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Plos Med. 2007, 4, e296. [Google Scholar] [CrossRef] [PubMed]
- JBI Critical Appraisal Tools. Available online: https://joannabriggs.org/ebp/critical_appraisal_tools (accessed on 21 December 2019).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Plos Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Adjibade, M.; Lemogne, C.; Touvier, M.; Hercberg, S.; Galan, P.; Assmann, K.E.; Julia, C.; Kesse-Guyot, E. The Inflammatory Potential of the Diet is Directly Associated with Incident Depressive Symptoms Among French Adults. J. Nutr. 2019, 149, 1198–1207. [Google Scholar] [CrossRef] [PubMed]
- Adjibade, M.; Julia, C.; Alles, B.; Touvier, M.; Lemogne, C.; Srour, B.; Hercberg, S.; Galan, P.; Assmann, K.E.; Kesse-Guyot, E. Prospective association between ultra-processed food consumption and incident depressive symptoms in the French NutriNet-Sante cohort. BMC Med. 2019, 17, 78. [Google Scholar] [CrossRef]
- Adjibade, M.; Lemogne, C.; Julia, C.; Hercberg, S.; Galan, P.; Assmann, K.E.; Kesse-Guyot, E. Prospective association between adherence to dietary recommendations and incident depressive symptoms in the French NutriNet-Sante cohort. Br. J. Nutr. 2018, 120, 290–300. [Google Scholar] [CrossRef]
- Adjibade, M.; Andreeva, V.A.; Lemogne, C.; Touvier, M.; Shivappa, N.; Hebert, J.R.; Wirth, M.D.; Hercberg, S.; Galan, P.; Julia, C.; et al. The Inflammatory Potential of the Diet Is Associated with Depressive Symptoms in Different Subgroups of the General Population. J. Nutr. 2017, 147, 879–887. [Google Scholar] [CrossRef]
- Akbaraly, T.N.; Sabia, S.; Shipley, M.J.; Batty, G.D.; Kivimaki, M. Adherence to healthy dietary guidelines and future depressive symptoms: Evidence for sex differentials in the Whitehall II study. Am. J. Clin. Nutr. 2013, 97, 419–427. [Google Scholar] [CrossRef]
- Bergmans, R.S.; Malecki, K.M. The association of dietary inflammatory potential with depression and mental well-being among U.S. adults. Prev. Med. 2017, 99, 313–319. [Google Scholar] [CrossRef]
- Chang, S.C.; Cassidy, A.; Willett, W.C.; Rimm, E.B.; O’Reilly, E.J.; Okereke, O.I. Dietary flavonoid intake and risk of incident depression in midlife and older women. Am. J. Clin. Nutr. 2016, 104, 704–714. [Google Scholar] [CrossRef]
- Collin, C.; Assmann, K.E.; Andreeva, V.A.; Lemogne, C.; Hercberg, S.; Galan, P.; Kesse-Guyot, E. Adherence to dietary guidelines as a protective factor against chronic or recurrent depressive symptoms in the French SU.VI.MAX cohort. Prev. Med. 2016, 91, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Elstgeest, L.E.M.; Winkens, L.H.H.; Penninx, B.; Brouwer, I.A.; Visser, M. Associations of depressive symptoms and history with three a priori diet quality indices in middle-aged and older adults. J. Affect. Disord. 2019, 249, 394–403. [Google Scholar] [CrossRef] [PubMed]
- Emerson, S.D.; Carbert, N.S. An apple a day: Protective associations between nutrition and the mental health of immigrants in Canada. Soc. Psychiatry Psychiatr. Epidemiol. 2019, 54, 567–578. [Google Scholar] [CrossRef] [PubMed]
- Gangwisch, J.E.; Hale, L.; Garcia, L.; Malaspina, D.; Opler, M.G.; Payne, M.E.; Rossom, R.C.; Lane, D. High glycemic index diet as a risk factor for depression: Analyses from the Women’s Health Initiative. Am. J. Clin. Nutr. 2015, 102, 454–463. [Google Scholar] [CrossRef] [PubMed]
- Godos, J.; Castellano, S.; Ray, S.; Grosso, G.; Galvano, F. Dietary Polyphenol Intake and Depression: Results from the Mediterranean Healthy Eating, Lifestyle and Aging (MEAL) Study. Molecules 2018, 23, 999. [Google Scholar] [CrossRef] [PubMed]
- Gougeon, L.; Payette, H.; Morais, J.A.; Gaudreau, P.; Shatenstein, B.; Gray-Donald, K. Intakes of folate, vitamin B6 and B12 and risk of depression in community-dwelling older adults: The Quebec Longitudinal Study on Nutrition and Aging. Eur. J. Clin. Nutr. 2016, 70, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Huddy, R.L.; Torres, S.J.; Milte, C.M.; McNaughton, S.A.; Teychenne, M.; Campbell, K.J. Higher Adherence to the Australian Dietary Guidelines Is Associated with Better Mental Health Status among Australian Adult First-Time Mothers. J. Acad. Nutr. Diet. 2016, 116, 1406–1412. [Google Scholar] [CrossRef] [PubMed]
- Jacka, F.N.; O’Neil, A.; Opie, R.; Itsiopoulos, C.; Cotton, S.; Mohebbi, M.; Castle, D.; Dash, S.; Mihalopoulos, C.; Chatterton, M.L.; et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med. 2017, 15, 23. [Google Scholar] [CrossRef]
- Lai, J.S.; Oldmeadow, C.; Hure, A.J.; McEvoy, M.; Hiles, S.A.; Boyle, M.; Attia, J. Inflammation mediates the association between fatty acid intake and depression in older men and women. Nutr. Res. (New York N.Y.) 2016, 36, 234–245. [Google Scholar] [CrossRef]
- Lucas, M.; Chocano-Bedoya, P.; Schulze, M.B.; Mirzaei, F.; O’Reilly, E.J.; Okereke, O.I.; Hu, F.B.; Willett, W.C.; Ascherio, A. Inflammatory dietary pattern and risk of depression among women. Brainbehaviorand Immun. 2014, 36, 46–53. [Google Scholar] [CrossRef]
- Matta, J.; Czernichow, S.; Kesse-Guyot, E.; Hoertel, N.; Limosin, F.; Goldberg, M.; Zins, M.; Lemogne, C. Depressive Symptoms and Vegetarian Diets: Results from the Constances Cohort. Nutrients 2018, 10, 1695. [Google Scholar] [CrossRef]
- Parletta, N.; Zarnowiecki, D.; Cho, J.; Wilson, A.; Bogomolova, S.; Villani, A.; Itsiopoulos, C.; Niyonsenga, T.; Blunden, S.; Meyer, B.; et al. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutr. Neurosci. 2019, 22, 474–487. [Google Scholar] [CrossRef] [PubMed]
- Ruusunen, A.; Lehto, S.M.; Mursu, J.; Tolmunen, T.; Tuomainen, T.P.; Kauhanen, J.; Voutilainen, S. Dietary patterns are associated with the prevalence of elevated depressive symptoms and the risk of getting a hospital discharge diagnosis of depression in middle-aged or older Finnish men. J. Affect. Disord. 2014, 159, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.J.; Sanderson, K.; McNaughton, S.A.; Gall, S.L.; Dwyer, T.; Venn, A.J. Longitudinal associations between fish consumption and depression in young adults. Am. J. Epidemiol. 2014, 179, 1228–1235. [Google Scholar] [CrossRef] [PubMed]
- Yary, T.; Lehto, S.M.; Tolmunen, T.; Tuomainen, T.P.; Kauhanen, J.; Voutilainen, S.; Ruusunen, A. Dietary magnesium intake and the incidence of depression: A 20-year follow-up study. J. Affect. Disord. 2016, 193, 94–98. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Kunz, R.; Vist, G.E.; Falck-Ytter, Y.; Schunemann, H.J. What is “quality of evidence” and why is it important to clinicians? BMJ (Clin. Res. Ed.) 2008, 336, 995–998. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Kunz, R.; Woodcock, J.; Brozek, J.; Helfand, M.; Alonso-Coello, P.; Glasziou, P.; Jaeschke, R.; Akl, E.A.; et al. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J. Clin. Epidemiol. 2011, 64, 1294–1302. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schunemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clin. Res. Ed.) 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Huang, Q.; Liu, H.; Suzuki, K.; Ma, S.; Liu, C. Linking What We Eat to Our Mood: A Review of Diet, Dietary Antioxidants, and Depression. Antioxidants 2019, 8, 376. [Google Scholar] [CrossRef]
- Lassale, C.; Batty, G.D.; Baghdadli, A.; Jacka, F.; Sanchez-Villegas, A.; Kivimaki, M.; Akbaraly, T. Healthy dietary indices and risk of depressive outcomes: A systematic review and meta-analysis of observational studies. Mol. Psychiatry 2019, 24, 965–986. [Google Scholar] [CrossRef]
- Nicolaou, M.; Colpo, M.; Vermeulen, E.; Elstgeest, L.E.M.; Cabout, M.; Gibson-Smith, D.; Knuppel, A.; Sini, G.; Schoenaker, D.; Mishra, G.D.; et al. Association of a priori dietary patterns with depressive symptoms: A harmonised meta-analysis of observational studies. Psychol. Med. 2019, 1–12. [Google Scholar] [CrossRef]
- Salari-Moghaddam, A.; Keshteli, A.H.; Afshar, H.; Esmaillzadeh, A.; Adibi, P. Association between dietary inflammatory index and psychological profile in adults. Clin. Nutr. (Edinb. Scotl.) 2019, 38, 2360–2368. [Google Scholar] [CrossRef] [PubMed]
- Shivappa, N.; Hebert, J.R.; Rashidkhani, B. Association between Inflammatory Potential of Diet and Stress Levels in Adolescent Women in Iran. Arch. Iran. Med. 2017, 20, 108–112. [Google Scholar] [PubMed]
- Peirce, J.M.; Alvina, K. The role of inflammation and the gut microbiome in depression and anxiety. J. Neurosci. Res. 2019, 97, 1223–1241. [Google Scholar] [CrossRef]
- Petridou, E.T.; Kousoulis, A.A.; Michelakos, T.; Papathoma, P.; Dessypris, N.; Papadopoulos, F.C.; Stefanadis, C. Folate and B12 serum levels in association with depression in the aged: A systematic review and meta-analysis. Aging Ment. Health 2016, 20, 965–973. [Google Scholar] [CrossRef] [PubMed]
- Skarupski, K.A.; Tangney, C.; Li, H.; Ouyang, B.; Evans, D.A.; Morris, M.C. Longitudinal association of vitamin B-6, folate, and vitamin B-12 with depressive symptoms among older adults over time. Am. J. Clin. Nutr. 2010, 92, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Tarleton, E.K.; Littenberg, B. Magnesium intake and depression in adults. J. Am. Board Fam. Med. Jabfm 2015, 28, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Wang, R.; Li, Z.; Zhang, D. Dietary magnesium intake and risk of depression. J. Affect. Disord. 2019, 246, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Bender, A.; Hagan, K.E.; Kingston, N. The association of folate and depression: A meta-analysis. J. Psychiatr. Res. 2017, 95, 9–18. [Google Scholar] [CrossRef]
- McEligot, A.J.; Cruz, S.S.; Gonzalez, S.; Pogoda, J.M. The Association between Total Folate Intakes and Depression amongst Three Racial/Ethnic Groups. Calif. J. Health Promot. 2018, 16, 6–15. [Google Scholar] [CrossRef]
- Li, Y.; Lv, M.R.; Wei, Y.J.; Sun, L.; Zhang, J.X.; Zhang, H.G.; Li, B. Dietary patterns and depression risk: A meta-analysis. Psychiatry Res. 2017, 253, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.J.; Yang, T.F.; Wang, G.S.; Zhao, Y.Y.; Yang, L.J.; Bi, B.N. Association between dietary patterns and depressive symptoms among middle-aged adults in China in 2016-2017. Psychiatry Res. 2018, 260, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Hu, D.; Cheng, L.; Jiang, W. Sugar-sweetened beverages consumption and the risk of depression: A meta-analysis of observational studies. J. Affect. Disord. 2019, 245, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Kim, Y.; Je, Y. Fish consumption and risk of depression: Epidemiological evidence from prospective studies. Asia-Pac. Psychiatry Off. J. Pac. Rim Coll. Psychiatr. 2018, 10, e12335. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Liu, X.; Zhang, D. Fish consumption and risk of depression: A meta-analysis. J. Epidemiol. Community Health 2016, 70, 299–304. [Google Scholar] [CrossRef]
- Matsuoka, Y.J.; Sawada, N.; Mimura, M.; Shikimoto, R.; Nozaki, S.; Hamazaki, K.; Uchitomi, Y.; Tsugane, S. Dietary fish, n-3 polyunsaturated fatty acid consumption, and depression risk in Japan: A population-based prospective cohort study. Transl. Psychiatry 2017, 7, e1242. [Google Scholar] [CrossRef]
- Roca, M.; Kohls, E.; Gili, M.; Watkins, E.; Owens, M.; Hegerl, U.; van Grootheest, G.; Bot, M.; Cabout, M.; Brouwer, I.A.; et al. Prevention of depression through nutritional strategies in high-risk persons: Rationale and design of the MooDFOOD prevention trial. BMC Psychiatry 2016, 16, 192. [Google Scholar] [CrossRef]
- Lehman, S.L. J NNT for Statins vs. the Mediterranean Diet In ACA News Articles. 2015. Available online: https://www.acatoday.org/News-Publications/ACA-News-Archive/ArtMID/5721/ArticleID/106/NNT-for-Statins-vs-the-Mediterranean-Diet (accessed on 12 January 2020).
- Estruch, R.; Ros, E.; Salas-Salvado, J.; Covas, M.I.; Corella, D.; Aros, F.; Gomez-Gracia, E.; Ruiz-Gutierrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef]
| Search Number (#) | Search Terms | Hits | Reviewed Abstracts | Selection 1 Relevance Assessment | Selection 2 Quality Assessment | Selection 3 Included Studies |
|---|---|---|---|---|---|---|
| #1 | Eating [MeSH] OR Diet [MeSH] | 324,299 | - | - | - | - |
| #2 | Causality [MeSH] | 796,445 | - | - | - | - |
| #3 | Depression [MeSH] OR Anxiety [MeSH] OR Mental health [MeSH] | 288,337 | - | - | - | - |
| #4 | #1 AND #2 AND #3 | 175 | 127 | 47 | 20 | 14 |
| Author/ Year/ Country | Study Design/ Number of Participants | Population/ Selection | Aim | Results | Conclusion | Study Quality According to GRADE |
|---|---|---|---|---|---|---|
| Adjibade et al. (2019a) [17] France | Prospective cohort n = 26,730 | Participants from Nutrinet-Santé Adults 18–86 years | Relationship between inflammatory diet and depressive symptoms. | The result indicates that a pro-inflammatory diet may be associated with an increased risk of depression symptoms, especially in obese and obese participants (Hazard Ratio (HR) 1.29). | Maintaining normal weight and avoiding pro-inflammatory foods can be interesting targets for prevention strategies to prevent depression and depressive symptoms. | Strong |
| Adjibade et al. (2019b) [18] France | Prospective cohort n = 26,730 | Participants from Nutrinet-Santé Adults 18–86 years | Relationship between processed food and risk of depression. | An increased risk of depressive symptoms was observed in a high proportion of processed foods in the diet (HR 1.21). | Avoiding processed foods can be important in preventing mental illness. | Strong |
| Adjibade et al. (2018) [19] France | Prospective cohort n = 26,225 | Participants from Nutrinet-Santé Adults 18–86 years | Examine the prospective relationship between adherence to dietary advice and the incidence of depression. | High adherence to dietary advice was associated with lower risk of depressive symptoms. | Adherence to dietary advice can have a preventive effect on depression. | Strong |
| Adjibade et al. (2017) [20] France | Prospective cohort study mean follow-up 12.6 years n = 3523 35–60 years | Participants from SU.VI. MAX cohort that initially did not have depressive symptoms Adults | Investigate prospective relationship between diet’s potential inflammatory effects and risk of developing depressive symptoms. | Significance was found in the subgroups of men, smokers, and physically inactive that a diet with a higher proportion of pro-inflammatory foods could increase the risk of depressive symptoms (Odds Ratio (OR) 2.32 / 2.21 / 2.07, respectively). | Promoting a healthy diet consisting of anti-inflammatory foods can help prevent depressive symptoms. | Strong |
| Akbaraly et al. (2013) [21] United Kingdom | Prospective cohort n = 4215 | Data from Whitehall II Adults 35–55 years | Investigating whether adherence to a healthy diet was associated with depressive symptoms. | A healthy dietary index was associated with protective effects against depression in women. | For women, a healthy diet can prevent depression. | Moderately strong |
| Bergmans and Malecki (2017) [22] USA | Cross-sectional study n = 11,592 | Data from NHANES Adults aged 20 years and older | Investigate whether the diet’s inflammatory index is associated with depression and other mental illness. | A high intake of inflammatory foods was associated with significantly increased risk of depression (OR 2.26), and for frequent anxiety (OR 1.81). | A pro-inflammatory diet has the potential to increase inflammation, which in turn can increase the risk of depression. | Limited |
| Chang et al. 2016 [23] USA | Prospective cohorts with 10 y of follow-up Associations n = 82,643 | Data from Nurse health study Women 36–80 years | Greater intakes of dietary flavonoids were significantly associated with a modest reduction in depression risk, particularly among the older women. | Higher intakes of all flavonoid subclasses except for flavan-3-ols were associated with significantly lower depression risk; the strongest associations (HR for both: 0.83) was found for flavones and pro-anthocyanin showed. | Higher flavonoid intakes may be associated with lower depression risk, particularly among older women. | Strong |
| Collin et al. (2016) [24] France | Prospective cohort n = 3328 | Data from SU.VI.MAX study Adults 35–60 years | Investigate whether there is a relationship between adherence to dietary recommendations and depression in middle-aged women and men. | Adherence to French dietary advice was associated with lower incidence of chronic and recurrent depressive symptoms (p > 0.001). | Adherence to dietary recommendations may be relevant to avoiding depression symptoms. | Strong |
| Elstgeest et al. (2019) [25] The Netherlands | Longitudinal cohort study n = 1439 | Data from the LASA Nutrition and Food-related behaviour Adults 55–85 years | Investigate the relationship between depression and diet quality. | Current and past depressive symptoms were associated with poorer dietary quality based on dietary index, especially in men. | Men with depression symptoms can feel better by eating high quality diets. | Limited |
| Emerson and Carbert 2019 [26] Canada | Prospective cohort cross-section measurement n = 37,071 | Data from the Canadian Community Health Survey From 12 years. | Investigate the relationship between nutrition and depression of immigrants in Canada. | Fruits and vegetables showed significant protective effects against depressive symptoms such as mood and anxiety disorders. | A healthy diet should be considered to prevent mental illness for immigrants in Canada. | Limited |
| Gangwisch et al. (2015) [27] USA | Prospective cohort n = 87,618 | Data from Women’s Health Initiative Observational study Women 50–79 years. | Investigate the association between high GI and depression in women post menopause. | Dietary glycemic index (GI) was associated with a significantly increased risk of depression in postmenopausal women (OR 1.22). A higher intake of added sugar was associated with a significantly increased risk of depression (OR 1.23) and high consumption of fruits (OR 0.88) vegetables (OR 0.88), and fibre (OR 0.86) was associated with a significantly reduced risk of depression. | High GI diets may be a risk factor for depression in postmenopausal women. | Strong |
| Godos et al. 2018 [28] Italy | Observational study n = 1572 | Data from the MEAL study Adults 18–92 years. | To assess the relation between estimated dietary intakes of total polyphenols, their classes, subclasses and compounds, and depressive symptoms. | Total polyphenol intake was not associated with depressive symptoms. However, for certain polyphenol classes intake was significant inverse associated with depressive symptoms, comparing intake from the highest with the lowest quartile. Phenolic acid (OR 0.64), flavanones (OR 0.54), and anthocyanins (OR 0.61). | Greater dietary intake of flavonoids may be inversely associated with depressive symptoms. | Moderately strong |
| Gougeon et al. 2016 [29] Canada | Longitudinal observational study n = 1793 | Data from a randomized medical database in Quebec Adults 67–84 years. | Relationship between intake of B vitamins and depression. | In women, those with the highest intake of B6 had a reduced risk (OR 0.57) and among men, the ones with the highest intake of B12 had a reduced risk (OR 0.42). | Intake of vitamin B can affect the risk of depression. | Strong |
| Huddy et al. (2016) [30] Australia | Cross-sectional study n = 437 | Data from the Melbourne Infant Feeding, Activity, and Nutrition Trial Women 19–45 years | Examine the relationship between intake of fruits, vegetables, fish, and depression in first time mothers. | Healthy diet was associated with less depressive symptoms. | Adherence to a healthy diet can reduce the risk of depressive symptoms in first time mothers. | Limited |
| Jacka et al. (2017) [31] Australia | RCT n = 56 | Single blind RCT Adults from 18 years | The aim was to investigate the effectiveness of diet improvement programs to treat depression. | Both groups had a significantly better condition after three months. The group receiving treatment with dietary intervention had more than 30% improved condition, compared to those receiving social support 8%. | Treatment with dietary interventions in the form of individual counselling according to MI can help people with depression to improve mental health. | Strong |
| Lai et al. (2016) [32] Australia | Prospective cohort n = 2035 | Data from the Hunter Community study. Adults 55–85 years | Inflammatory markers influence on antioxidant and fatty acid intake is there an association with depression. | Relationships were observed between the intake of various fatty acids, antioxidants, the influence of inflammatory markers, and the risk of depression. | There may be a link between fatty acid intake and depression, partly mediated by inflammatory markers. | Moderately strong |
| Lucas et al. (2014) [33] USA | Prospective cohort n = 43,685 | Data from the Nurses’ health study Women 55–77 years | The aim was to investigate the relationship between inflammatory diet and depression. | An inflammatory diet was significantly associated with an increased risk of depression (Reduced Rank Regression (RRR) 1.41 (p > 0.001). | Chronic inflammation may be an underlying link between diet and depression. | Moderately strong |
| Matta et al. (2018) [34] France | Prospective cohort Cross-sectional n = 90,380 | Data from Constances Cohort Adults 18–69 years | The study examined the cross-sectional relationship between depressive symptoms and vegetarian diet. | Regardless of diet, the risk of depression gradually increased with the number of excluded foods. | Depressive symptoms can be associated with food exclusion. | Limited |
| Parletta et al. (2019) [35] Australia | RCT n = 85 | Single blind RCT Adults 18–65 years | The purpose was to investigate whether the Mediterranean diet supplemented with fish oil could improve the mental health of people with depression. | The group that received the intervention with dietary advice and education according to the Mediterranean diet had significantly improved mental health after three months and the positive result remained after six months follow-up. | Healthy dietary changes are possible and have been shown to improve the mental health of people with depression. | Strong |
| Ruusunen et al. (2014) [36] Finland | Prospective cohort n = 1003 | Data from Kuopio Ischemic heart disease Risk Factor Men 46–65 years. | Assess diet’s relationship with depression. | Three different dietary patterns were identified. The group with the highest intake of a healthy diet had a protective effect against depression. | Adherence to a healthy diet can reduce the risk of depression. | Moderately strong |
| Smith et al. (2014) [37] Australia | Longitudinal study n = 1386 | Data from The Childhood Determinants of Adult Health Adults 26–36 years | Relationship between fish consumption and risk of depression. | Fish consumption significantly protected against depression in women, in men no relationship was seen. | Regular fish consumption can reduce the risk of depression in women. | Strong |
| Yary et al. (2015) [38] Finland | Prospective cohort study 20 years of follow-up n = 2320 | Data from The KIDH study Men 42–61 years | Relationship between magnesium intake in the diet and risk of depression. | Magnesium intake had a protective effect against depression (HR 0.53). | Magnesium intake may have an impact on the risk of developing depression in men. | Moderately strong |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ljungberg, T.; Bondza, E.; Lethin, C. Evidence of the Importance of Dietary Habits Regarding Depressive Symptoms and Depression. Int. J. Environ. Res. Public Health 2020, 17, 1616. https://doi.org/10.3390/ijerph17051616
Ljungberg T, Bondza E, Lethin C. Evidence of the Importance of Dietary Habits Regarding Depressive Symptoms and Depression. International Journal of Environmental Research and Public Health. 2020; 17(5):1616. https://doi.org/10.3390/ijerph17051616
Chicago/Turabian StyleLjungberg, Tina, Emma Bondza, and Connie Lethin. 2020. "Evidence of the Importance of Dietary Habits Regarding Depressive Symptoms and Depression" International Journal of Environmental Research and Public Health 17, no. 5: 1616. https://doi.org/10.3390/ijerph17051616
APA StyleLjungberg, T., Bondza, E., & Lethin, C. (2020). Evidence of the Importance of Dietary Habits Regarding Depressive Symptoms and Depression. International Journal of Environmental Research and Public Health, 17(5), 1616. https://doi.org/10.3390/ijerph17051616





