Abstract
Thyroid hormones are regulated by the pituitary thyroid stimulating hormone (TSH), whose secretion presents a circadian rhythmicity. Indeed, it is conceivable that shift- and night shift-work, affecting sleep-wake rhythms, may impact thyroid functionality. Therefore, the aim of the present review was to provide an overview on the association between shift- and night shift-work and thyroid hormonal changes and disease development. A systematic review of studies available in PubMed, Scopus, and ISI Web of Science databases was performed. A positive association between night shift-work and increased TSH concentrations was reported by most of the reviewed investigations. Inconclusive evidence was available on thyroid diseases. However, the limited number of studies, the noticeable heterogeneity in the shift-work scheduling, in terms of amount, duration, type of shift- or night shift-work, prevents easily integrating findings and extrapolating definite conclusions. Further investigation seems necessary to better define the relationship between shift schedules and different thyroid outcomes, and possible long-term implications of early functional changes. Overall, this may support the adoption of advanced risk assessment and management strategies aimed to achieve a safer workplace organization and a timely, responsible realization of all the benefits of a 24-h economy.
1. Introduction
The thyroid gland produces hormones, triiodothyronine (T3) and thyroxine (T4), that are essential for body’s metabolism, heat production, suitable development and differentiation of cells, and growth [1]. The hypothalamic-pituitary-thyroid (HPT) axis controls the thyroid function, as the T3 and T4 hormones are secreted in response to the pituitary thyroid stimulating hormone (TSH) [2]. Thyroid stimulating hormone secretion exhibits a clear daily rhythmicity, related to the sleep-wake cycle and sleep structure, and the HPT axis is under the control of the central circadian pacemaker in the suprachiasmatic nucleus of the anterior hypothalamus [3]. Under normal sleeping conditions, plasma TSH levels begin to increase in the late afternoon or early evening before sleep, and reach a maximal concentration during the early part of the night [4]. Following the nocturnal peak, plasma TSH levels reduce during the rest of the sleep period, up to reach the low diurnal levels. Sleep has been demonstrated to exert an inhibitory influence on TSH production, as confirmed by the increase in hormonal secretion caused by sleep withdrawal [5]. In fact, TSH secretion, which is normally inhibited during sleep, continues to occur during nocturnal sleep deprivation determining higher morning plasma levels of the hormone compared to those found in subjects with a normal night sleep [1]. Additionally, recovery sleep, following withdrawal, suppresses TSH levels to larger extent than normal sleep [6].
Many individuals, particularly night shift workers, frequently undergo circadian misalignment by desynchronizing their sleep/wake cycle from the biological timing system. Thus, it is conceivable that shift-work intended by the International Labour Organization as a “a method of organization of working time in which workers succeed one another at the workplace” [7], and night-work defined by the European Union as “working at least 3 h of the daily shift or a certain proportion of the yearly working time in a period of 7 h defined by national law and including the time from midnight to 05:00” [8] may have a significant impact on thyroid function, in relation to circadian disruption, sleep deprivation, poor sleep efficiency, as well as sudden reversal of sleep/wake habits.
Shift-work, in particular night-work, in fact, has been recognized as stressors for the human body, as alterations of the sleep/wake cycle can affect human biological functions, physical–psychological conditions, quality of life, as well as working efficiency [9,10]. Overall, it has been demonstrated that shift-work is able to induce a huge spectrum of adverse health outcomes, ranging from sleep disturbances to the development of, e.g., cardiovascular, gastrointestinal, and neuropsychic diseases, and possible risk of cancers [11,12,13]. Less defined evidence is currently available on the relationship between circadian misalignment and adverse effects on metabolic and hormonal factors, particularly on the HPT axis. This seems an intriguing public and occupational health issue, considering the worldwide prevalence of shift-workers, as among one fifth of the workforce is involved into such kind of working schedule, and the 750 million people worldwide that the World Health Organization estimated to be affected by thyroid diseases, including cancer, hypothyroidism, hyperthyroidism and thyroiditis [14,15]. Therefore, the aim of the present study was to gain deep insight into the possible relationship between shift- and night-work and alterations in the function of the HPT axis, as well as the development of thyroid diseases. From an occupational risk assessment and management perspective, this may be useful to define early endocrine effects potentially induced by specific work schedules and particular conditions of hyper-susceptibility that should require peculiar preventive measures to protect the health of exposed workers.
2. Materials and Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement (PRISMA) criteria were followed to perform a systematic literature search [16]. Studies addressing possible implications of “shift work” or “night work” on thyroid function or clinical outcomes, published until 20 January 2020, were identified by research on three principal scientific databases: PubMed, Scopus, and ISI Web of Science. The terms “shift work or night work” to assess the context of exposure and “thyroid” as the outcome of the investigation, combined with the Boolean operator “AND”, were employed for the research.
All the titles and abstracts retrieved through the computerized search were independently reviewed by three of the authors who selected papers suitable for the review purposes according to the inclusion criteria. These included all types of human peer-reviewed research articles (i.e., descriptive epidemiological-occupational surveys, medical reports, case series, cohort and case-control studies) published in English, and reporting possible implications of “shift work or night work” on various thyroid outcomes in workers. Exclusion criteria regarded reviews, case reports, conference papers, experimental studies on cellular and animal models, publications that did not focus on thyroid function of shift workers or those that, although exploring thyroid outcomes, did not provide information on shift schedules, as well as all the papers published in languages other than English.
The quality of the included studies was assessed separately by two investigators. Each eligible study was subjected to methodological critical appraisal through the Newcastle Ottawa Scale (NOS) adapted to perform a quality assessment of cross-sectional studies for systematic review [17,18,19]. The adapted NOS assesses the risk of bias in three domains: selection of participants (maximum 5 points); comparability of study groups (maximum two points); and outcome assessment (maximum 3 points). Quality rating of the studies was assessed as follows: very good (9, 10 points); good (7, 8 points); satisfactory (5, 6 points), unsatisfactory (0–4 points) (Table 1).
3. Results
The preliminary search retrieved a total of 71 articles: 15, 30 and 26 in PubMed, Scopus, and Isi Web of Knowledge databases, respectively. From the total number of papers, 28 duplicates were removed. Among the remaining 43 articles, those (n. 35) that did not meet the inclusion criteria were excluded. Among those, 30 were considered out of the topic from the title and abstract analysis, 3 studies were excluded for the language other than English and 2 because were review articles. A total of 8 papers remained suitable for review. The full texts of all these articles were obtained and subjected to a critical evaluation. The citation pool of relevant publications was enlarged through the analysis of the reference list accompanying the selected articles identified with the previously detailed literature search. Another 5 eligible papers could be added. Overall, our search retrieved a total of 13 articles suitable for review (Figure 1). Most of the reviewed studies assessed the association between shift-work and night-work and thyroid hormonal changes in different occupational settings [20,21,22,23,24,25,26,27,28,29] (Table 1). Only a few publications focused on possible clinical adverse outcomes [26,30,31,32]. Some thyroid function alterations were demonstrated in relation to the shift-working organization and interesting issues could be pointed out as detailed in the following paragraphs.
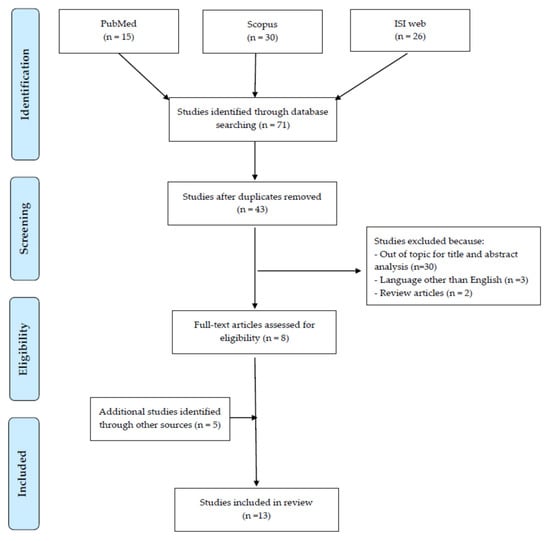
Figure 1.
Flow diagram of literature search.

Table 1.
Studies assessing the relationship between shift work and thyroid alterations.
3.1. Night Shift-Work and Thyroid Hormonal Changes
3.1.1. Healthcare Sector
Several studies investigated changes in TSH levels in relation to night shift-work in the healthcare sector and found a positive correlation between such working schedule and increased hormonal concentrations [21,26,27]. Chang et al. [21] in a cohort of nurses enrolled in the largest psychiatric center in southern Taiwan, demonstrated that TSH levels were significantly higher in those who had sleep restriction for two consecutive night shifts compared to those who had been free of duty for at least 3 days before entering the study day. Comparably, in a retrospective study carried out on employees of a University hospital in Korea, Moon et al. [26] demonstrated that night shift workers had significantly 0.303 mIU/L higher TSH levels, over a 5 year study period (2011–2015), compared to non-night shift workers after adjusting for age and employment department. In line with these results, a study on Indian healthcare professionals, including doctors, nurses, technicians and support staff, demonstrated that mean TSH values were significantly higher in night shift (3.11 ± 1.81 mIU/L) than day-shift workers (2.04 ± 0.8 mIU/L) [27].
The effects of an irregular rotating working system, including night shifts, was also assessed in intensive care unit Greek nurses with respect to daily workers [23]. Thyroid stimulating hormone concentrations significantly decreased from the beginning to the end of a morning shift in rotating workers, while no significant effects were detected in the morning group. Conversely, T4 values significantly increased in rotating workers, but not in daily employees. When the overall mean changes in the hormonal levels were compared in the two groups, only T4 alterations resulted significantly different in rotating and daily workers. Concerning the possibility that irregular shifts may have effects on the circadian rhythm of serum hormone levels, and, consequently, on possible variables which are thought to modify an individual’s response to shift-work, such as personality, psychological health and social and domestic disruption, the authors found a significant positive correlation between TSH change in the rotating shift and the general health questionnaire score, indicating that greater changes in TSH are accompanied by poorer psychological health. Interestingly, when the TSH hormonal profile was assessed during a usual day sleep time for night- (7:00–15:00 h) and day-active workers (22:00–6:00 h), some differences could be pointed out [25]. In fact, TSH plateaued during night sleep in day-employees, while progressively declined during day sleep in night workers. Conversely, during working time, an ascending TSH trend was observed in night workers (22:00–6:00 h) in comparison to the lower levels seen in daytime ones (9:00–17:00 h). However, the mechanisms responsible for such changes as well as the physiological consequences of these hormonal profile modifications, still remain to be elucidated.
Hormonal changes have not been confirmed in a more recent study in healthcare workers, involved in rotating night shifts (principally nurses), and daily workers (primarily technicians) from an Italian teaching hospital, that showed comparable levels of TSH, FT3 and FT4 [32].
3.1.2. Industrial Sector
Thyroid hormonal alterations were also investigated in shift-workers engaged in different industrial sectors, although with conflicting results. Among male workers employed in a rubber and ceramics Egyptian industry, who have been performing fixed morning-, afternoon- or night shifts for at least 2 years, those who were employed in night shifts had significantly higher levels of TSH than those who were employed in other schedules [28]. Night shift resulted as an independent predictor of TSH hormonal changes. These results are not in line with those obtained by a previous study carried out on female workers, employed in the packaging units of a pharmaceutical factory in Iran, that failed to demonstrate significant differences in TSH levels between night- and non-night shift workers [20].
3.2. Night on-Call-Work and Thyroid Hormonal Changes
When the effects of a night or 24-h on-call duty were investigated on the TSH levels, conflicting results were reported [22,24,25]. A significant increase in TSH levels was demonstrated by Harbeck et al. [22] in German internal medicine physicians the morning after a 24-h on-call-duty, compared to the TSH levels determined before a normal working day. Sleep deprivation with disturbed sleep patterns, natural biological rhythm desynchronization and stress conditions experienced in night-call-duties may stimulate nervous, immune and endocrine physiological responses, possibly leading to hormonal increase. Concerning the impact that such changes may have on physician neurocognitive functions and performance, no impairment was observed, while focused attention tended to be better after a 24-h shift, as a possible effect of long-term gating of attentional properties. This may support physician ability to adapt to the workload and stressful events during a 24-h on-call-shift, and TSH alterations may function as a first indicator of such an effect as other biochemical stress parameters, e.g., cortisol, epinephrine, norepinephrine, insulin and glucagon, did not show significant changes. An increasing trend in hormonal values was determined also in the study by Kuetting et al. [24] that observed significantly higher levels of TSH, FT3 and FT4 in German radiology residents following 24-h shift and work-related short-term partial sleep deprivation, compared to the values detected before the shift, while no significant changes were observed before and after a regular day of work and regular sleep.
When the effects of a night call-duty was assessed in Swedish physicians involved in different specialties, a significant 28% and 26% decrease in TSH levels were determined 1 day after the night call compared to those found in an ordinary day of work in anesthesiologists and pediatricians/ear-nose-throat surgeons, respectively [25]. In contrast to the anesthesiologists, the plasma levels of pediatricians/ear-nose-throat surgeons returned to baseline levels when measured 3 days after the night-call duty. Concerning FT4, a reduction of 3% was detected the third day after night call, compared with the plasma levels measured on the ordinary workday and 1 day after the night-call duty. However, the levels were within the normal range and the overall results did not imply serious metabolic changes with only minor differences between specialist groups.
3.3. Shift Work and Other Thyroid Effects
Limited evidence is currently available regarding thyroid diseases in shift- compared to non-shift workers [26,30,31,32]. Burdelack et al. [30] investigated the frequency of different diseases in a cohort of 725 nurses and midwives employed on rotating night shifts or in daily fixed shifts. They observed an overall prevalence of thyroid diseases of 21.2%, without significant percentage differences in rotating night shift workers (22.6%) and daily workers (20%). Interestingly, when the risk of thyroid disease was assessed according to the duration of night shift work, a twofold increased risk was detected in those workers employed for ≥15 years on night shifts in comparison to employees engaged in night shifts for a shorter, less than 15 years period of time. In the analysis of the relative risk of occurrence of thyroid diseases according to the frequency of night duties per month, no increase could be detected in workers with an average of more than 4 nights shifts per month with respect to those with less frequent night schedules. Unfortunately, this study failed to provide data on which diseases were considered in the analysis, therefore limiting the interpretation of the results. In the above-mentioned study by Moon et al. [26], the age-adjusted TSH levels ≥4.5 mIU/L among night shift healthcare workers were associated with a 1.4-fold higher risk of subclinical hypothyroidism compared to non-night shift workers. Comparably, a study carried out on 642 workers employed in a large teaching Italian hospital showed a significantly higher risk of subclinical autoimmune hypothyroidism in shift workers compared to the daytime workers, that remained significant also when possible confounding factors, such as age, gender, smoking habits, alcohol intake, familial history of autoimmune thyroid diseases, and exposure to radiations were included in the analysis [31]. Concerning anti-TPO antibodies prevalence, a significant difference was found between shift-workers, with a prevalence of 13.6%, compared to 8.6% of day-time workers. The prevalence of hypothyroidism unrelated to altered anti-TPO antibodies was significantly higher in shift workers (5.45%) than daytime workers (2.10%), while no differences could be detected for the prevalence of hyperthyroidism in absence of altered anti-TPO antibodies between the two investigated groups [31]. In a more recent study of the same research group [32], rotating night shift workers employed in the same hospital, showed a higher risk of thyroid nodules compared to diurnal workers. However, the lack of data on the characterization of such lesions and their possible malignancy, and information on potential co-exposures to other risk factors for thyroid diseases, such as ionizing radiation, do not allow to extrapolate definite conclusions.
4. Discussion
This review represents the first attempt to provide an overview on the possible alterations exerted by the circadian rhythm disruption induced by shift- and night shift-work in the function of the HPT axis and in the development of thyroid diseases. The determination of serum TSH concentrations has been employed as a specific and sensitive measure for the early detection of endocrine disorders. Different investigations performed on healthcare employees demonstrated that night shift-work could be related to higher levels of TSH serum levels in involved workers, although concentrations were included in a physiological range [21,22,24,26,27,28]. Interestingly, this effect was evident for any type of shift-working schedule considered, such as to have been involved in two consecutive night shifts before entry the study day [21], to have been performing more than 3 nights a week, for at least 1 year [27], as well as to have been engaged in night-, or 24-h on-call-duties [22,24].
Although the reason for such effects are not fully understood, it may be primarily conceived that night shift-induced changes in sleep schedule, timing, and quality may alter the body’s normal circadian rhythm and lead to an abnormal TSH circadian secretion. Changes in the TSH daily rhythmicity induced by sleep deprivation after night shifts may promote a hormonal increase [33,34]. It has also argued that night shift work can affect the immune system function, increasing the risk of autoimmune disease [35], as suggested by the results obtained by Moon et al. [26] and Magrini et al. [31] who determined a higher risk for subclinical autoimmune hypothyroidism in night shift workers compared to those not involved in such schedule. Additionally, several hormonal alterations, including those related to TSH secretion, may be dependent on the irregular eating habits and nocturnal eating frequent in night shift workers [36].
Although an increase in TSH serum concentrations was reported, the limited number of available studies and the noticeable heterogeneity in the enrolled populations, and shift-work scheduling, in terms of amount and type of shift- or night shift-work, does not allow to extrapolate definite conclusions, also, on possible underlining mechanisms of action. In this regard, it should be important to assess the role of personal features, including ethnicity, body mass index, calorie intake during work-shift, exercise status (including fitness level, sport activity performed before/after work or before going to bed), smoking and drinking habits, as well as therapies taken for comorbidities in possibly influencing TSH results. Particular attention in this regard should be focused at the worldwide aging of the workforce and the possible diverse age-dependent response that the endocrine system may have with respect to the circadian disruption induced by night shift-work. This seems important considering also the not definite evidence reporting an age-dependent increase in the median and upper reference limits of TSH [37,38,39,40], and an earlier shift of the beginning of the nocturnal rise of the serum TSH rhythm with aging [41]. Additionally, the impact of different work-related confounding factors, e.g., duration of employment, type of shift rotation, and sleep quality on hormonal response, should be also deeply evaluated. In contrast to classic rotating shift-work, in fact, physicians’ night call schedules are more irregular, with longer working hours (sometimes more than 16 h), reduced sleep and physiological and psychological stress, which may all function as specific factors influencing TSH alterations. On-call-duty was reported to induce disruption in the rhythm of TSH secretion even after a single night [22]. In this perspective, TSH may be the earliest and most sensitive parameter indicating even mild stress, whereas other biochemical stress indicators were less influenced by an on-call-shift, as also demonstrated by the lack of significant alterations in the concentrations of other circadian related hormones [22].
Overall, the different characteristics of the work-shifts may explain the not homogeneous results obtained on TSH levels. In fact, Rizza et al. [32] in healthcare professionals, and Attarchi et al. [20] in a pharmaceutical factory night shift workers failed to detect significant hormonal changes, while Korompeli et al. [23] and Marlberg et al. [25] determined a decreasing trend in TSH serum values in rotating shift nurses or in night-call-duty physicians, respectively. This latter result may be potentially related to a direct acute stress effect, or to the recovery sleep (following a period of sleep deprivation) characterized by a large fraction of deep sleep known to inhibit the hormone secretion [42]. It cannot be also excluded that the lack of TSH alterations could be explained by an “healthy worker” effect, meaning that those who could not face the workload had left the employment. Moreover, it is possible that participants had considerable experience on working on call and were probably confident in being able to handle emergency situations. These conditions may limit the stress experienced on such schedule organization, therefore preventing hormonal effects. However, deep details on work schedule, job tasks, duration of engagement in such kind of occupational organization, as well as population characteristics, in terms of physiological or pathological features, were not always provided by the authors, therefore preventing to clearly understand the relationship between thyroid functional changes and possible influencing occupational factors. These considerations may provide stimulus to future search aimed to deeply explore mechanisms responsible for specific hormonal changes also in relation to the characteristics of the work activities. In this regard, the possible effects of co-exposures to other risk factors on the thyroid function in the workplaces, e.g., chemical, biological and physical factors, should be considered. Although taking into consideration the different conditions of exposures and the remarkable inter-subject variability, the thyroid is very sensitive to the action of chemical disruptors [43]. Therefore, it cannot be ruled out that physicians, e.g., anesthesiologists and surgeons, employees in rubber and ceramic industry, as well as those involved in the packaging units of a pharmaceutical industry, may be exposed to chemicals, e.g., anesthetics, metals and plasticizers that may mediate hormonal alterations as reported in occupational, epidemiological and experimental settings [44,45,46,47,48,49].
Additionally, some other limitations of the studies should be carefully considered to have a suitable interpretation of the results. Several of the reviewed investigations focused on total female [20,21,26] or male [24] occupational populations. This limits the investigation of gender-based differences in sensitivity to night shift work-related hormonal changes in comparable workplace settings. Blood samples were obtained at different times, as workers have been evaluated during night or day shift depending on their duty schedules, therefore preventing achieving results representing specific changes in circadian rhythm well [26,28]. In some studies, differences between the beginning and the end of night shifts, or of the daytime shifts following the nights on duty, were assessed, therefore representing additional quite different outcomes for a correct interpretation of the endocrine effects. Moreover, all but one [21] of the reviewed studies did not collect blood samples on days off-duty, therefore preventing to achieve a complete picture of hormone profile on rest days. Moreover, in many cases, only TSH values were determined and this may limit a more comprehensive understanding of the effects that night shifts may have on thyroid functionality.
Concerning the role that such preclinical alterations may have in the possible development of thyroid diseases and the periods of time in which hormone alterations could be resolved, only one study confirmed that TSH levels, affected by short term sleep deprivation, returned quickly to control values following recovery sleep [25]. Interestingly, this hormonal trend was demonstrated only in particular groups of workers, e.g., pediatricians and ear-nose-throat surgeons compared to anesthesiologists, maybe in relation to their different job task features. In anesthesiologists, in fact, there may be an overlapping between the endocrine “insult” exerted by the circadian disruption induced by night shifts and strongly stressful events determined by taking care of life-threatening conditions for most of their working time, therefore providing an extra stress exposure. This may differently impact the thyroid function. The quick normalization of hormone values, on the one side, may suggest that such changes may most likely be without clinical significance. However, the findings of a higher prevalence of thyroid diseases [30], subclinical autoimmune hypothyroidism [26,31] and thyroid nodules [32] in night shift workers may suggest the need to deeply verify the long-term implications of early changes in hormonal pathways on endocrine diseases development. Additionally, it may be interesting to assess the relationship between night shifts, mental well-being, neurocognitive functions and performance of workers during different types of schedules, and thyroid hormonal changes. It should be verified whether determined hormone alterations may function as possible biomarkers of worker ability or “disability” to adapt to the workload and stressful events during night shifts or on-call-duties.
Although this review fills a gap in the literature, some limitations need to be considered when drawing conclusions from reported results. First of all, the cross-sectional nature of the studies inherently limits the definition of a suitable relationship between shift- or night-work and thyroid effects. The different conditions of exposure, as well as the variable outcomes investigated do not allow to easily integrate findings and extrapolate definite conclusions. According to the NOS checklist adapted for cross-sectional studies, about half of the reviewed papers were of satisfactory or good quality, while the others could be classified as unsatisfactory rating. Greater deficiencies regarded the representativeness of the exposed cohort, as enrolled subjects were generally selected groups of users and not sufficiently representative of the average target populations, as well as the inadequate degree of control for relevant confounding factors. Overall, although these aspects may question the reliability of the reviewed investigations, the relevance that this topic may have for the general 24-h workplace organization, as well as for the health of exposed workers, makes it important to explore the current, although still incomplete, knowledge on the topic with the aim to provide guidance for deeper future research.
5. Conclusions
These preliminary data on possible effects of shift-work, and particularly night-work, on the thyroid function of exposed workers need to be confirmed in future investigations designed to better define the relationship between shift schedules, in terms of, for example, night shifts per month, duration of employment in such organization, specific gender sensitivity, as well as possible confounding occupational factors and different endocrine outcomes, from early hormonal changes to confirmed clinical diseases. From an occupational health point of view, these findings may open innovative scenarios concerning workplace risk assessment and suitable measures to protect the health of night shift workers. Once confirmed, in fact, awareness concerning possible thyroid effects derived from the circadian disruption in night shift workers should require efforts for advanced approaches to risk assessment and management in workplace settings. Health surveillance programs should also include the evaluation of early thyroid alterations and specific attention to all subjects with possible hyper-susceptibility conditions. Considering also that about 10% of people worldwide are affected by thyroid diseases during their lifetime, with a definite need for therapy [50], the possible impact of shift-work on endocrine outcomes and the clinical history of the diseases appear extremely important to define fitness for work for affected workers. Overall this review provides stimulus to overcome knowledge gaps in the incompletely understood impact of shift-work organization on thyroid functionality of exposed workers. This will support the adoption and implementation of specific preventive strategies that may support a safer workplace organization and the timely, responsible realization of all the benefits of a 24-h economy.
Author Contributions
Conceptualization, V.L., I.I.; Methodology, V.L., I.V., A.S., R.R., Writing – Original Draft Preparation, V.L., I.V., A.S., R.R., Writing – Review & Editing, V.L. and I.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ikegami, K.; Refetoff, S.; Van Cauter, E.; Yoshimura, T. Interconnection between circadian clocks and thyroid function. Nat. Rev. Endocrinol. 2019, 15, 590–600. [Google Scholar] [CrossRef] [PubMed]
- Ortiga-Carvalho, T.M.; Chiamolera, M.I.; Pazos-Moura, C.C.; Wondisford, F.E. Hypothalamus-pituitary-thyroid axis. Compr. Physiol. 2016, 6, 1387–1428. [Google Scholar] [CrossRef] [PubMed]
- Kalsbeek, A.; Fliers, E. Daily regulation of hormone profile. Handb. Exp. Pharmacol. 2013, 217, 185–226. [Google Scholar] [CrossRef]
- Morris, C.J.; Aeschbach, D.; Scheer, F.A. Circadian system, sleep and endocrinology. Mol. Cell. Endocrinol. 2012, 349, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, K.; Leproult, R.; Van Cauter, E. Impact of sleep debt on metabolic and endocrine function. Lancet 1999, 354, 1435–1439. [Google Scholar] [CrossRef]
- Brabant, G.; Prank, K.; Ranft, U.; Schuermeyer, T.; Wagner, T.O.F.; Hauser, H.; Kummer, B.; Feistner, H.; Hesch, R.D.; von sur Mühlen, A. Physiological regulation of circadian and pulsatile thyrotropin secretion in normal man and Woman. J. Clin. Endocr. Metab. 1990, 70, 403–409. [Google Scholar] [CrossRef]
- International Labour Office (ILO). Shift Work. Conditions of Work and Employment Programme. Information Sheet No. WT-8 2004. Available online: https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---travail/documents/publication/wcms_170713.pdf (accessed on 8 January 2020).
- Your Europe—European Union. Working Hours. Available online: https://europa.eu/youreurope/business/human-resources/working-hours-holiday-leave/working-hours/index_en.htm#shortcut-5 (accessed on 8 January 2020).
- Fischer, F.M.; Silva-Costa, A.; Griep, R.H.; Smolensky, M.H.; Bohle, P.; Rotenberg, L. Working Time Society consensus statements: Psychosocial stressors relevant to the health and wellbeing of night and shift workers. Ind. Health 2019, 57, 175–183. [Google Scholar] [CrossRef]
- Matheson, A.; O’Brien, L.; Reid, J.A. The impact of shiftwork on health: A literature review. J. Clin. Nurs. 2014, 23, 3309–3320. [Google Scholar] [CrossRef]
- IARC Monographs Vol 124 Group. Carcinogenicity of night shift work. Lancet Oncol. 2019, 20, 1058–1059. [Google Scholar] [CrossRef]
- Proper, K.I.; van de Langenberg, D.; Rodenburg, W.; Vermeulen, R.C.H.; van der Beek, A.J.; van Steeg, H.; van Kerkhof, L.W.M. The Relationship between Shift Work and Metabolic Risk Factors: A Systematic Review of Longitudinal Studies. J. Prev. Med. 2016, 50, e147–e157. [Google Scholar] [CrossRef]
- Kecklund, G.; Axelsson, J. Health consequences of shift work and insufficient sleep. BMJ 2016, 355, i5210. [Google Scholar] [CrossRef] [PubMed]
- American Thyroid Association. World Thyroid Day Aims to Raise Awareness of Disease. 2014. Available online: http://www.thyroid.org (accessed on 26 January 2020).
- Global Wellness Institute. Night Shift Work Is on Rise Globally—And It’s a New Wellness Problem. 2018. Available online: https://globalwellnessinstitute.org/global-wellness-institute-blog/2018/06/19/night-shift-work-is-on-the-rise-globally-and-its-a-new-wellness-problem/ (accessed on 28 January 2020).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analysis. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 28 January 2020).
- Modesti, P.A.; Reboldi, G.; Cappuccio, F.P.; Agyemang, C.; Remuzzi, G.; Rapi, S.; Perruolo, E.; Parati, G.; ESH Working Group on CV Risk in Low Resource Settings. Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0147601. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, R.S.; Barker, A.R.; Wilkinson, K.M.; Abbott, R.A.; Williams, C.A. Is cardiac autonomic function associated with cardiorespiratory fitness and physical activity in children and adolescents? A systematic review of cross-sectional studies. Int. J. Cardio 2017, 236, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Attarchi, M.; Darkhi, H.; Khodarahmian, M.; Dolati, M.; Kashanian, M.; Ghaffari, M.; Mirzamohammadi, E.; Mohammadi, S. Characteristics of menstrual cycle in shift workers. Glob. J. Health Sci. 2013, 5, 163–172. [Google Scholar] [CrossRef]
- Chang, Y.S.; Chen, H.L.; Hsu, C.Y.; Su, S.F.; Liu, C.K.; Hsu, C. Nurses working on fast rotating shifts overestimate cognitive function and the capacity of maintaining wakefulness during the daytime after a rotating shift. SleepMed 2013, 14, 605–613. [Google Scholar] [CrossRef]
- Harbeck, B.; Suefke, S.; Haas, C.S.; Lehnert, H.; Kropp, P.; Moenig, H. No stress after 24-h on-call shifts? J. Occup. Health. 2015, 57, 438–447. [Google Scholar] [CrossRef]
- Korompeli, A.; Sourtzi, P.; Tzavara, C.; Velonakis, E. Rotating shift-related changes in hormone levels in intensive care unit nurses. J. Adv. Nurs. 2009, 65, 1274–1282. [Google Scholar] [CrossRef]
- Kuetting, D.L.R.; Feisst, A.; Sprinkart, A.M.; Homsi, R.; Luetkens, J.; Thomas, D.; Schild, H.H.; Dabir, D. Effects of a 24-hr-shift-related short-term sleep deprivation on cardiac function: A cardiac magnetic resonance-based study. J. Sleep Res. 2019, 28, e12665. [Google Scholar] [CrossRef]
- Malmberg, B.; Persson, R.; Jönsson, B.A.; Erfurth, E.M.; Flisberg, P.; Ranklev, E.; Orbaek, P. Physiological restitution after night-call duty in anaesthesiologists: Impact on metabolic factors. Acta Anaesthesiol. Scand. 2007, 51, 823–830. [Google Scholar] [CrossRef]
- Moon, S.H.; Lee, B.J.; Kim, S.J.; Kim, H.C. Relationship between thyroid stimulating hormone and night shift work. Ann. Occup. Environ. Med. 2016, 28, 53. [Google Scholar] [CrossRef] [PubMed]
- Sathyanarayana, S.M.; Gangadharaiah, S. Night shift working and its impact on sleep quality, calorie intake, and serum thyroid stimulating hormone level among health-care workers in a tertiary hospital, Bengaluru. Natl. J. Physiol. Pharm. Pharmacol. 2018, 8, 1330–1334. [Google Scholar] [CrossRef]
- Shaker, D.; Samir, A.; Zyada, F.; El-Sharkawy, M.; Ekladious, S.M. Impact of shift work on sleep problems, hormonal changes, and features of metabolic syndrome in a sample of Egyptian industrial workers: A cross-sectional study. Middle East Curr. Psychiatry 2018, 25, 91–97. [Google Scholar] [CrossRef]
- Weibel, L.; Brandenberger, G. Disturbances in hormonal profiles of night workers during their usual sleep and work times. J. Biol. Rhythms 1998, 13, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Burdelak, W.; Bukowska, A.; Krysicka, J.; Pepłońska, B. Night work and health status of nurses and midwives. Cross-sectional study. Med Pr. 2012, 63, 517–529. [Google Scholar]
- Magrini, A.; Pietroiusti, A.; Coppeta, L.; Babbucci, A.; Barnaba, E.; Papadia, C.; Iannaccone, U.; Boscolo, P.; Bergamaschi, E.; Bergamaschi, A. Shift work and autoimmune thyroid disorders. Int. J. Immunopathol. Pharmacol. 2006, 19 (Suppl. 4), 31–36. [Google Scholar]
- Rizza, S.; Neri, A.; Capanna, A.; Grecuccio, C.; Pietroiusti, A.; Magrini, A.; Federici, M.; Coppeta, L. Night Shift Working Is Associated with an Increased Risk of Thyroid Nodules. J. Occup. Environ. Med. 2020, 62, 1–3. [Google Scholar] [CrossRef]
- Parker, D.C.; Rossman, L.G.; Pekary, A.E.; Hershman, J.M. Effect of 64-h sleep deprivation on the circadian waveform of TSH: Further evidence of sleep related inhibition of TSH release. J. Clin. Endocrinol. Metab. 1987, 64, 157–161. [Google Scholar] [CrossRef]
- Allan, J.S.; Czeisler, C.A. Persistence of the circadian thyrotropin rhythm under constant conditions and after light-induced shifts of circadian phase. J. Clin. Endocrinol. Metab. 1994, 79, 508–512. [Google Scholar] [CrossRef]
- Boscolo, P.; Youinou, P.; Theoharides, T.C.; Cerulli, G.; Conti, P. Environmental and occupational stress and autoimmunity. Autoimmun. Rev. 2008, 7, 340–343. [Google Scholar] [CrossRef]
- Holmbäck, U.; Forslund, A.; Lowden, A.; Forslund, J.; Akerstedt, T.; Lennernäs, M.; Hambraeus, L.; Stridsberg, M. Endocrine responses to nocturnal eating–possible implications for night work. Eur J Nutr. 2003, 42, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Hollowell, J.G.; Staehling, N.W.; Flanders, W.D.; Hannon, W.H.; Gunter, E.W.; Spencer, C.A.; Braverman, L.E. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J. Clin. Endocrinol. Metab. 2002, 87, 489–499. [Google Scholar] [CrossRef] [PubMed]
- Boucai, L.; Hollowell, J.G.; Surks, M.I. An approach for development of age-, gender-, and ethnicity-specific thyrotropin reference limits. Thyroid 2011, 21, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Surks, M.I.; Hollowell, J.G. Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population: Implications for the prevalence of subclinical hypothyroidism. J. Clin. Endocrinol. Metab. 2007, 92, 4575–4582. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Kim, H.I.; Oh, H.K.; Kim, T.H.; Jang, H.W.; Chung, J.H.; Shin, M.H.; Kim, S.W. Age- and gender-specific reference intervals of TSH and free T4 in an iodine-replete area: Data from Korean National Health and Nutrition Examination Survey IV (2013–2015). PLoS ONE 2018, 13, e0190738. [Google Scholar] [CrossRef] [PubMed]
- Roelfsema, F.; Pijl, H.; Kok, P.; Endert, E.; Fliers, E.; Biermasz, N.R.; Pereira, A.M.; Veldhuis, J.D. Thyrotropin secretion in healthy subjects is robust and independent of age and gender, and only weakly dependent on body mass index. J. Clin. Endocrinol. Metab. 2014, 99, 570–578. [Google Scholar] [CrossRef]
- Goichot, B.; Weibel, L.; Chapotot, F.; Gronfier, C.; Piquard, F.; Brandenberger, G. Effect of the shift of the sleep-wake cycle on three robust endocrine markers of the circadian clock. Am. J. Physiol. 1998, 275 Pt 1, E243–E248. [Google Scholar] [CrossRef]
- Yilmaz, B.; Terekeci, H.; Sandal, S.; Kelestimur, F. Endocrine disrupting chemicals: Exposure, effects on human health, mechanism of action, models for testing and strategies for prevention. Rev. Endocr. Metab. Disord. 2019, in press. [Google Scholar] [CrossRef]
- Özütürk, B.; Ersoy, A.; Altan, A.; Uygur, L.M. Comparison of the Effects of Remifentanil and Dexmedetomidine Infusions on Hemodynamic Parameters and Thyroid Hormones. Turk. J. Anaesthesiol. Reanim. 2013, 41, 206–210. [Google Scholar] [CrossRef]
- Şentürk, B.; Umuroğlu, T.; Saraçoğlu, A.; Eti, Z.; Göğüş, F.Y. The Effects of Desflurane and Propofol on the Release of Thyroid Hormones in Euthyroid Patients Undergoing Elective Lumbar Discectomy. Turk. J. Anaesthesiol. Reanim. 2015, 43, 68–72. [Google Scholar] [CrossRef]
- Calsolaro, V.; Pasqualetti, G.; Niccolai, F.; Caraccio, N.; Monzani, F. Thyroid Disrupting Chemicals. Int. J. Mol. Sci. 2017, 18, 2583. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.; Kim, S.S.; Chung, E.; Dietrich, K.N. Thyroid hormones in relation to lead, mercury, and cadmium exposure in the National Health and Nutrition Examination Survey, 2007–2008. Environ. Health Perspect. 2013, 121, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Iavicoli, I.; Fontana, L.; Bergamaschi, A. The effects of metals as endocrine disruptors. J. Toxicol. Environ. Health B Crit. Rev. 2009, 12, 206–223. [Google Scholar] [CrossRef] [PubMed]
- Uzma, N.; Salar, B.M.; Kumar, B.S.; Aziz, N.; David, M.A.; Reddy, V.D. Impact of organic solvents and environmental pollutants on the physiological function in petrol filling workers. Int. J. Environ. Res. Public Health 2008, 5, 139–146. [Google Scholar] [CrossRef]
- Chen, T.Y.; Hsu, C.C.; Feng, I.J.; Wang, J.J.; Su, S.B.; Guo, H.R.; Huang, C.C.; Lin, H.J. Higher risk for thyroid diseases in physicians than in the general population: A Taiwan nationwide population-based secondary analysis study. QJM 2017, 110, 163–168. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).