An Innovative Treatment Approach Using Digital Workflow and CAD-CAM Part 2: The Restoration of Molar Incisor Hypomineralization in Children
Abstract
1. Introduction
2. Methods
2.1. Compliance with Ethical Standards
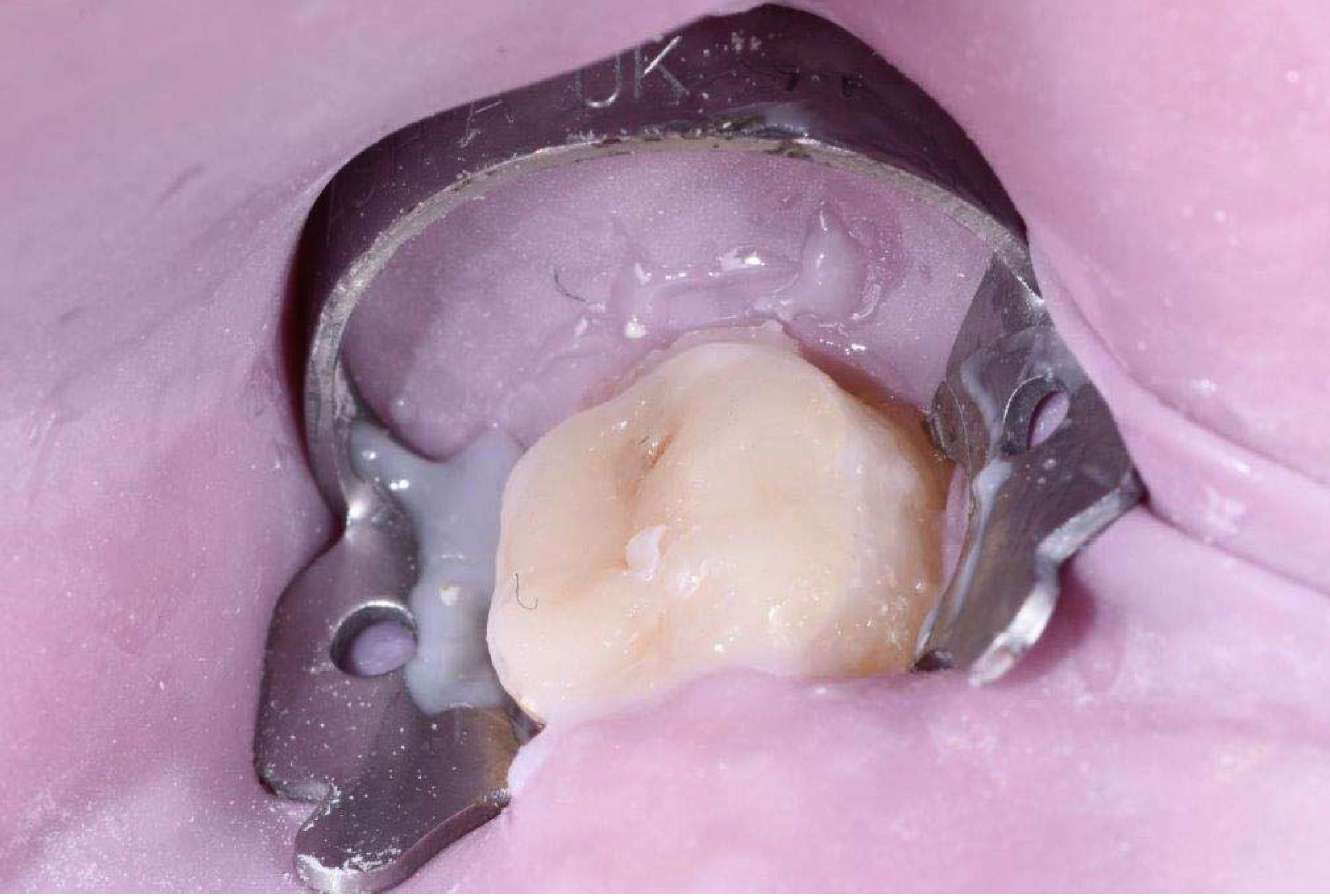
2.2. Clinical Case
3. Discussion
3.1. Treatment Options
3.1.1. Adhesive Restorations—RC and Glass Ionomer Cements
3.1.2. Adhesive Restorations—Glass Ionomer Cements
3.1.3. Full Coronal Coverage Restorations—Stainless-Steel Crowns
3.1.4. Porcelain Veneers and Overlays
- The child’s cooperation;
- The child’s immediate and long-term needs;
- Financial costs;
- The dentist’s skills and the materials available.
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| IOS | intraoral scanners |
| MIH | molar incisor hypomineralization |
| 3D | three-dimensional |
| RC | resin composites |
References
- Weerheijm, K.L.; Jalevik, B.; Alaluusua, S. Molar-incisor hypomineralization. Caries Res. 2001, 35, 390–391. [Google Scholar] [CrossRef]
- Elfrink, M.E.; Ghanim, A.; Manton, D.J.; Weerheijm, K.L. Standardised studies on Molar Incisor Hypomineralisation (MIH) and Hypomineralised Second Primary Molars (HSPM): A need. Eur. Arch. Paediatr. Dent. 2015, 16, 247–255. [Google Scholar] [CrossRef]
- Weerheijm, K.L.; Groen, H.J.; Beentjes, V.E.; Poorterman, J.H. Prevalence of cheese molars in 11-year-old Dutch children. J. Dent. Child. 2001, 68, 259–262. [Google Scholar]
- Holtta, P.; Kiviranta, H.; Leppaniemi, A.; Vartiainen, T.; Lukinmaa, P.L.; Alaluusua, S. Developmental dental defects in children who reside by a river polluted by dioxins and furans. Arch. Environ. Health 2001, 56, 522–528. [Google Scholar] [CrossRef] [PubMed]
- Leppaniemi, A.; Lukinmaa, P.L.; Alaluusua, S. Nonfluoride hypomineralizations in the permanent first molars and their impact on the treatment need. Caries Res. 2001, 35, 36–40. [Google Scholar] [PubMed]
- William, V.; Messer, L.B.; Burrow, M.F. Molar incisor hypomineralization: Review and recommendations for clinical management. Pediatr Dent. 2006, 28, 224–232. [Google Scholar] [PubMed]
- Fearne, J.; Anderson, P.; Davis, G.R. 3D X-ray microscopic study of the extent of variations in enamel density in first permanent molars with idiopathic enamel hypomineralization. Br. Dent. J. 2004, 196, 634–638. [Google Scholar] [CrossRef]
- Wright, J.T.; Hall, K.; Yamauchi, M. The protein com-position of normal and developmentally defective enamel. Ciba Found. Symp. 1997, 205, 85–99, 106 (in discussion). [Google Scholar] [PubMed]
- Seow, W.K. Enamel hypoplasia in the primary dentition: A review. J. Dent. Child. 1991, 58, 441–452. [Google Scholar]
- Martinez, A.; Cubillos, P.; Jimenez, M.; Brethauer, U.; Catalan, P.; Gonzalez, U. Prevalence of developmental enamel defects in mentally retarded children. J. Dent. Child. 2002, 69, 151–155. [Google Scholar]
- Mangano, F.; Gandolfi, A.; Luongo, G.; Logozzo, S. Intraoral scanners in dentistry: A review of the current literature. BMC Oral Health 2017, 17, 149. [Google Scholar] [CrossRef] [PubMed]
- Sonmez, N.; Gultekin, P.; Turp, V.; Akgungor, G.; Sen, D.; Mijiritsky, E. Evaluation of five CAD/CAM materials by microstructural characterization and mechanical tests: A comparative in vitro study. BMC Oral Health 2018, 18, 5. [Google Scholar] [CrossRef] [PubMed]
- Ting-Shu, S.; Jian, S. Intraoral digital impression technique: A review. J. Prosthodont. 2015, 24, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.; Mehl, A.; Mormann, W.H.; Reich, S. Intraoral scanning systems—A current overview. Int. J. Comput. Dent. 2015, 18, 101–129. [Google Scholar]
- Koch, M.J.; Garcia-Godoy, F. The clinical performance of laboratory-fabricated crowns placed on first permanent molars with developmental defects. J. Am. Dent. Assoc. 2000, 131, 1285–1290. [Google Scholar] [CrossRef]
- Means, C.R.; Flenniken, I.E. Gagging—A problem in prosthetic dentistry. J. Prosthet. Dent. 1970, 23, 614–620. [Google Scholar] [CrossRef]
- Almeida, E.; Silva, J.S.; Erdelt, K.; Edelhoff, D.; Araújo, É.; Stimmelmayr, M.; Vieira, L.C.; Güth, J.F. Marginal and internal fit of four-unit zirconia fixed dental prostheses based on digital and conventional impression techniques. Clin. Oral Investig. 2014, 18, 515–523. [Google Scholar] [CrossRef]
- Tsirogiannis, P.; Reissmann, D.R.; Heydecke, G. Evaluation of the marginal fit of single-unit, complete-coverage ceramic restorations fabricated after digital and conventional impressions: A systematic review and meta-analysis. J. Prosthet. Dent. 2016, 116, 328–335. [Google Scholar] [CrossRef]
- Fayle, S.A. Molar incisor hypomineralization: Restorative management. Eur. J. Paediatr. Dent. 2003, 4, 121–126. [Google Scholar]
- Mahoney, E.K. The treatment of localized hypoplastic and hypomineralized defects in first permanent molars. N. Z. Dent. J. 2001, 97, 101–105. [Google Scholar]
- Lygidakis, N.A.; Chaliasou, A.; Siounas, G. Evaluation of composite restorations in hypomineralized permanent molars: A four-year clinical study. Eur. J. Paediatr. Dent. 2003, 4, 143–148. [Google Scholar] [PubMed]
- Lygidakis, N.A.; Wong, F.; Jälevik, B.; Vierrou, A.M.; Alaluusua, S.; Espelid, I. Best Clinical Practice Guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH): An EAPD Policy Document. Eur. Arch. Paediatr. Dent. 2010, 11, 75–81. [Google Scholar] [CrossRef]
- Lygidakis, N.A. Treatment modalities in children with teeth affected by molar-incisor enamel hypomineralisation (MIH): A systematic review. Eur. Arch. Paediatr. Dent. 2010, 11, 65–74. [Google Scholar] [CrossRef] [PubMed]
- William, V.; Burrow, M.; Palamara, J.E.; Messer, L.B. Microshear Bond Strength of Resin Composite to Teeth Affected by Molar Hypomineralization Using 2 Adhesive Systems. Pediatr. Dent. 2006, 28, 233–241. [Google Scholar]
- Croll, T.P. Restorative options for malformed permanent molars in children. Compend. Contin. Educ. Dent. 2000, 21, 676–678, 680, 682. [Google Scholar] [PubMed]
- Berg, J.H. Glass ionomer cements. Pediatr. Dent. 2002, 24, 430–438. [Google Scholar] [PubMed]
- Croll, T.P.; Nicholson, J.W. Glass ionomer cements in pediatric dentistry: A review of the literature. Pediatr Dent. 2002, 24, 423–429. [Google Scholar]
- Radcliffe, R.M.; Cullen, C.L. Preservation of future options: Restorative procedures on first permanent molars in children. J. Dent. Child. 1991, 58, 104–108. [Google Scholar]
- Zagdwon, A.M.; Fayle, S.A.; Pollard, M.A. A prospective clinical trial comparing preformed metal crowns and cast restorations for defective first permanent molars. Eur. J. Oral Sci. 2003, 3, 138–142. [Google Scholar]
- Randall, R.C. Preformed metal crowns for primary and permanent molar teeth: Review of the literature. Pediatr. Dent. 2002, 24, 489–500. [Google Scholar]
- Harley, K.E.; Ibbetson, R.J. Dental anomalies: Are adhesive castings the solution? Br. Dent. J. 1993, 174, 15–22. [Google Scholar] [CrossRef] [PubMed]




| Restorative Considerations | Composite Restoration | Glass Ionomer Restoration | Full Coverage Stainless-Steel Crown | CAD/CAMCeramic Overlays |
|---|---|---|---|---|
| Effectiveness of restorative approach | ++ | ++ | +++ | +++ |
| Tooth sensitivity reduction | ++ | ++ | +++ | +++ |
| Tooth preparation | +++ | +++ | + | ++ |
| Restoration strength (shear & bond) | ++ | + | +++ | +++ |
| Occlusal contact stability | ++ | + | +++ | +++ |
| Interproximal contact stability | ++ | + | +++ | +++ |
| Pulpal trauma | + | ++ | +++ | +++ |
| Esthetics | ++ | ++ | - | +++ |
| Technique sensitivity | ++ | ++ | +++ | ++ |
| Cost | ++ | ++ | ++ | + |
| Predictability | + | + | +++ | +++ |
| Definitive restoration | +++ | +++ | - | +++ |
| Restoration longevity | ++ | + | +++ | +++ |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Davidovich, E.; Dagon, S.; Tamari, I.; Etinger, M.; Mijiritsky, E. An Innovative Treatment Approach Using Digital Workflow and CAD-CAM Part 2: The Restoration of Molar Incisor Hypomineralization in Children. Int. J. Environ. Res. Public Health 2020, 17, 1499. https://doi.org/10.3390/ijerph17051499
Davidovich E, Dagon S, Tamari I, Etinger M, Mijiritsky E. An Innovative Treatment Approach Using Digital Workflow and CAD-CAM Part 2: The Restoration of Molar Incisor Hypomineralization in Children. International Journal of Environmental Research and Public Health. 2020; 17(5):1499. https://doi.org/10.3390/ijerph17051499
Chicago/Turabian StyleDavidovich, Esti, Shlomi Dagon, Israel Tamari, Michael Etinger, and Eitan Mijiritsky. 2020. "An Innovative Treatment Approach Using Digital Workflow and CAD-CAM Part 2: The Restoration of Molar Incisor Hypomineralization in Children" International Journal of Environmental Research and Public Health 17, no. 5: 1499. https://doi.org/10.3390/ijerph17051499
APA StyleDavidovich, E., Dagon, S., Tamari, I., Etinger, M., & Mijiritsky, E. (2020). An Innovative Treatment Approach Using Digital Workflow and CAD-CAM Part 2: The Restoration of Molar Incisor Hypomineralization in Children. International Journal of Environmental Research and Public Health, 17(5), 1499. https://doi.org/10.3390/ijerph17051499






