Assess the Performance and Cost-Effectiveness of LACE and HOSPITAL Re-Admission Prediction Models as a Risk Management Tool for Home Care Patients: An Evaluation Study of a Medical Center Affiliated Home Care Unit in Taiwan
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting, Data Source, and Ethical Concerns
2.2. Study Cohort, Enrolled Hospitalizations, and 30-Day Readmissions
2.3. The LACE Index and HOSPITAL Score Models for Prediction of Readmission
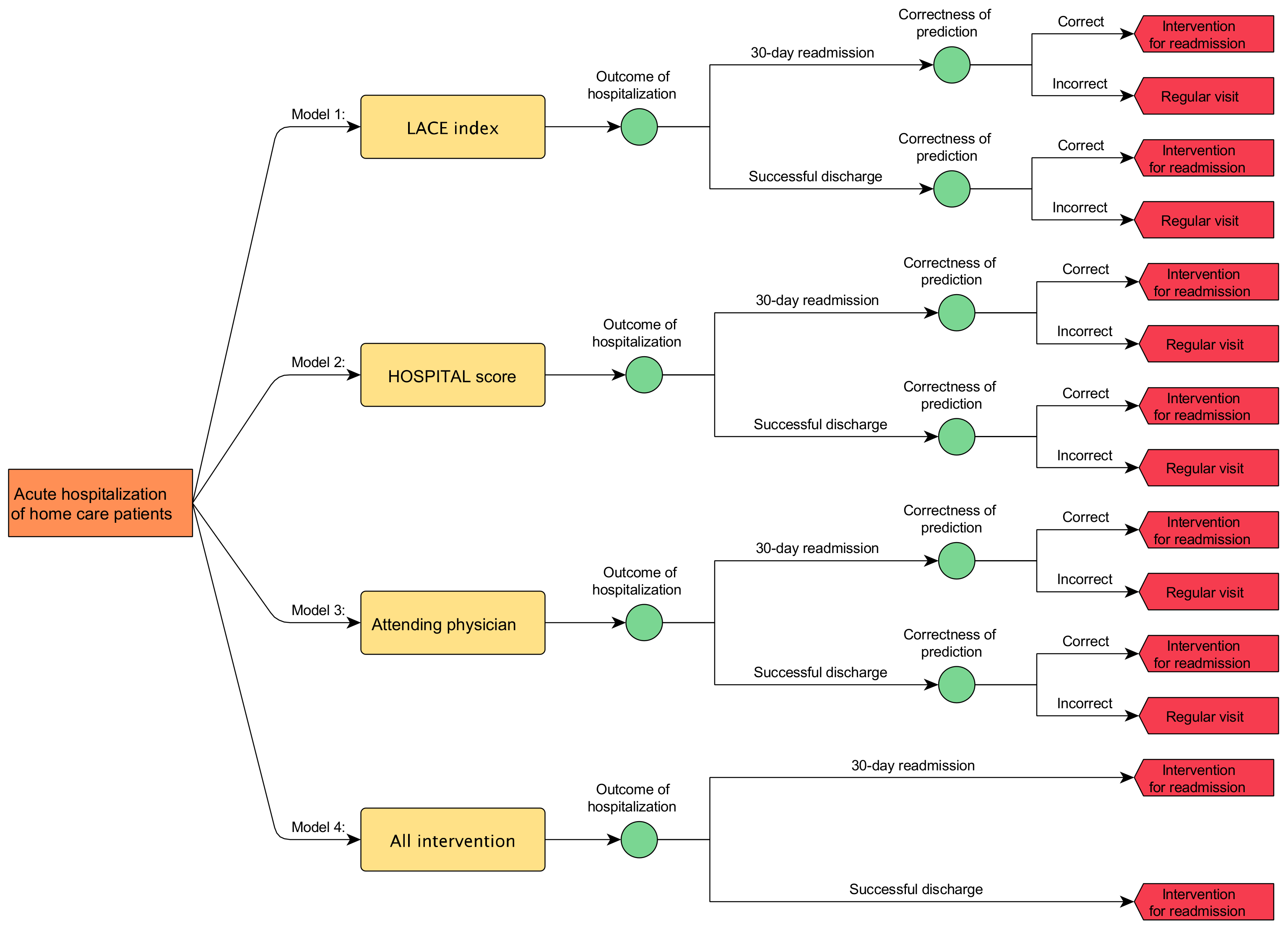
2.4. Microsimulation Model
2.5. Error Analysis and Statistical Analysis
2.6. Experimentation of Microsimulation Model
3. Results
3.1. Study Population and 30-Day Readmission Rates
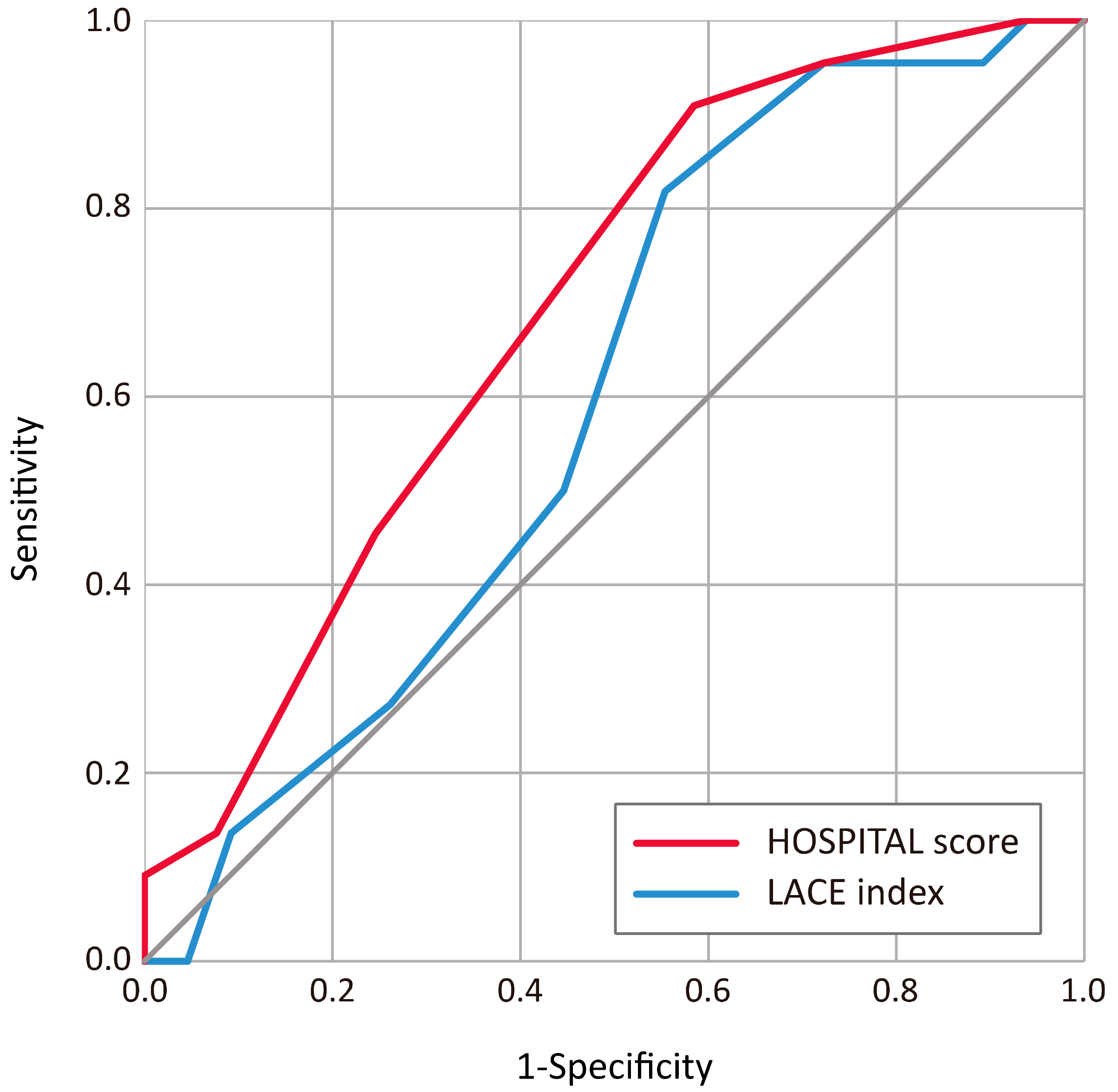
3.2. Discrimination and Calibration of the LACE and HOSPITAL Models
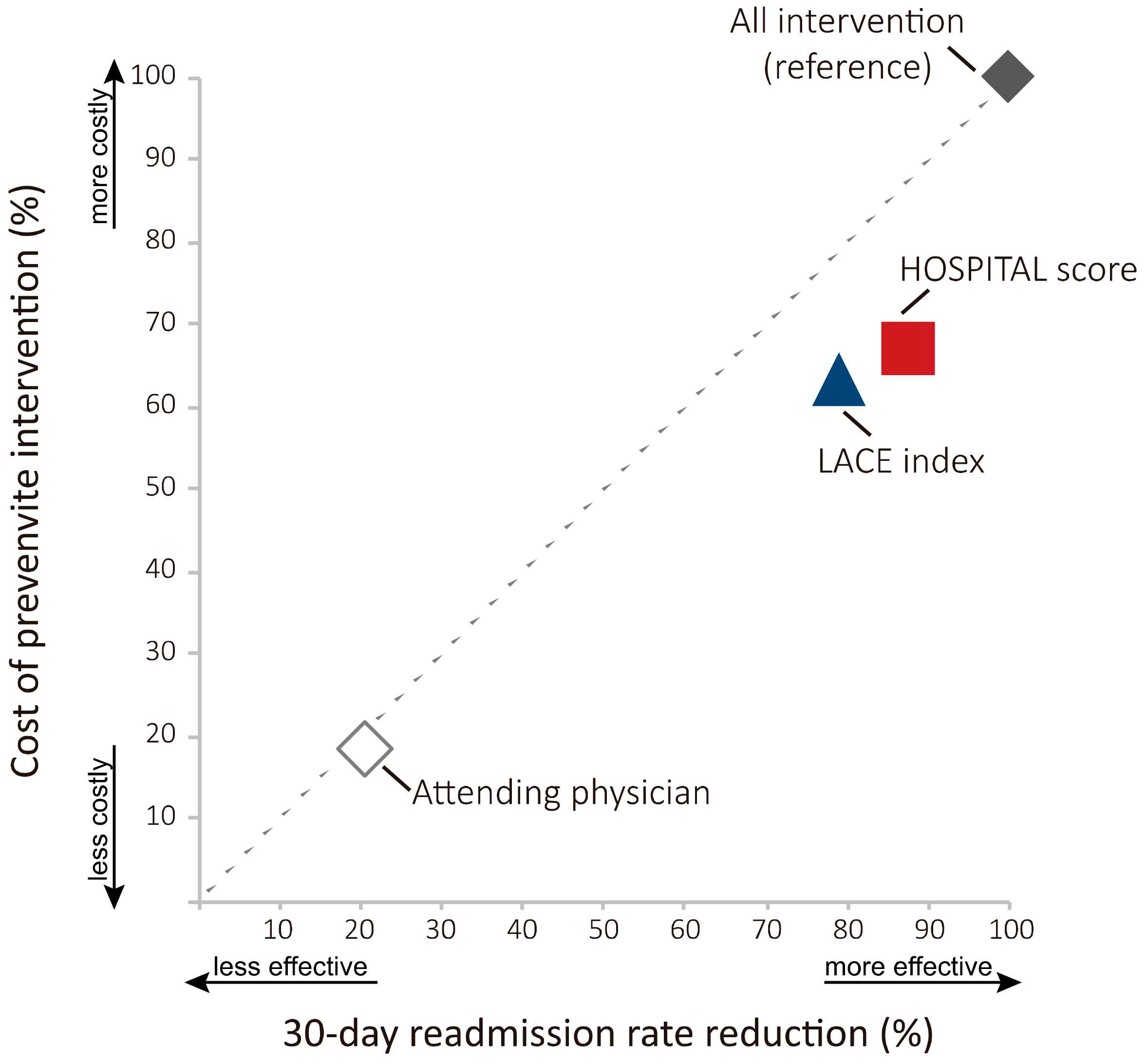
3.3. Cost of Intervention and Readmission Rate Reduction of the LACE Index and HOSPITAL Score Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| 30-Day Readmission Prediction Models | Sensitivity (%) | (95% CI) | Specificity | (95% CI) |
|---|---|---|---|---|
| LACE index | 81.8 | (59.7–94.8) | 44.6 | (32.3–57.5) |
| HOSPITAL score | 90.9 | (70.8–98.9) | 41.5 | (29.4–54.4) |
| Attending physician 1 | 23 | (13–37) | 84 | (75–90) |
| Variables | Type, Value | Lower Limit | Mode | Upper Limit |
|---|---|---|---|---|
| Readmission rate | Constant = 0.25 | - | - | - |
| Successful rate of preventive intervention | Constant = 0.5 | - | - | - |
| LACE index—Sensitivity | Triangular distribution | 0.597 | 0.818 | 0.948 |
| HOSPITAL score—Sensitivity | Triangular distribution | 0.708 | 0.909 | 0.989 |
| Attending physician—Sensitivity | Triangular distribution | 0.13 | 0.23 | 0.37 |
| LACE index—Specificity | Triangular distribution | 0.323 | 0.446 | 0.575 |
| HOSPITAL score—Specificity | Triangular distribution | 0.294 | 0.415 | 0.544 |
| Attending physician—Specificity | Triangular distribution | 0.75 | 0.84 | 0.90 |
Appendix B
| No. | Studies Used LACE Index | Population (n) | Area under Curve (AUC) | (95% CI) 1 | Discrimination Power 2 |
|---|---|---|---|---|---|
| 1. | Cotter et al., (2012) [12] | UK population, n = 507 | 0.57 | NA | Poor |
| 2. | Van Walraven et al., (2012) [44] 3 | Medical records, n = 500,000 | 0.771 | (0.767–0.775) | Clearly useful |
| 3. | Wang et al., (2014) [45] | Heart failure patients, n = 253 | 0.664 | (0.575–0.752) | Possibly helpful |
| 4. | Low et al., (2015) [46] | Singapore population, n = 5862 | 0.628 | (0.602–0.653) | Possibly helpful |
| 5. | Yazdan-Ashoori et al., (2016) [47] | Heart failure patients, n = 378 | 0.58 | (0.57–0.61) | Poor |
| 6. | Damery et al., (2017) [48] | Inpatient health records, n = 7107 | 0.773 | (0.768–0.779) | Clearly useful |
| 7. | Low et al., (2017) [49] | Singapore, elder inpatients, n = 17,006 | 0.595 | (0.581–0.608) | Poor |
| 8. | Robinson et al., (2017) [13] | Inpatient health records, n = 432 | 0.58 | (0.48–0.68) | Poor |
| 9. | Baig et al., (2018) [50] | New Zealand population, n = 213,440 | 0.752 | NA | Clearly useful |
| 10. | Hakim et al., (2018) [51] | COPD 4 patients, n = 2662 | 0.63 | (0.62–0.65) | Possibly helpful |
| 11. | Miller et al., (2018) [37] | Inpatients, n = 359 | 0.620 | (0.521–0.718) | Possibly helpful |
| 12. | Saluk et al., (2018) [52] | Radical cystectomy patients, n = 3470 | 0.581 | (0.556-0.606) | Poor |
| 13. | Caplan et al., (2019) [53] 3 | Brain tumor population, n = 352 | 0.58 | NA | Poor |
| 14. | Caplan et al., (2019) [54] 3 | Craniotomy patients, n = 238 | 0.69 | NA | Possibly helpful |
| 15. | Ibrahim et al., (2019) [55] | Heart failure patients, n = 730 | 0.551 | (0.503–0.598) | Poor |
| 16. | Robinson et al., (2019) [56] | Inpatients, n = 1916 | 0.598 | (0.58–0.64) | Poor |
| 17. | Shaffer et al., (2019) [57] | Surgical patients, n = 192,670 | 0.82 | NA | Possibly helpful |
| No. | Studies Used HOSPITAL Score | Population (n) | Area under Curve (AUC) | (95% CI) 1 | Discrimination Power 2 |
|---|---|---|---|---|---|
| 1. | Aubert et al., (2016) [10] | Switzerland, inpatients, n = 346 | 0.70 | (0.62–0.79) | Possibly helpful |
| 2. | Donze et al., (2016) [58] | Inpatients, n = 117,065 | 0.72 | (0.72–0.72) | Possibly helpful |
| 3. | Kim et al., (2016) [59] | Inpatients, n = 4208 | 0.65 | NA | Possibly helpful |
| 4. | Robinson (2016) [60] | Inpatients, n = 998 | 0.77 | (0.73–0.81) | Clearly useful |
| 5. | Aubert et al., (2017) [61] | Inpatients, n = 117,065 | 0.69 | (0.68–0.69) | Possibly helpful |
| 6. | Burke et al., (2017) [8] | Inpatients, n = 9181 | 0.68 | (0.67–0.71) | Possibly helpful |
| 7. | Robinson et al., (2017) [13] | Inpatient health records, n = 432 | 0.75 | (0.67–0.83) | Possibly helpful |
| 8. | Ibrahim et al., (2019) [55] | Heart failure inpatients, n = 730 | 0.595 | (0.549–0.641) | Poor |
| 9. | Robinson et al., (2019) [56] | Inpatients, n = 1916 | 0.675 | (0.65–0.70) | Possibly helpful |
References
- Wadhera, R.K.; Joynt Maddox, K.E.; Wasfy, J.H.; Haneuse, S.; Shen, C.; Yeh, R.W. Association of the Hospital Readmissions Reduction Program with Mortality Among Medicare Beneficiaries Hospitalized for Heart Failure, Acute Myocardial Infarction, and Pneumonia. JAMA 2018, 320, 2542–2552. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liebel, D.V.; Yu, F.; Caprio, T.V.; Shang, J. Inverse Dose-Response Relationship Between Home Health Care Services and Rehospitalization in Older Adults. J. Am. Med. Dir. Assoc. 2019, 20, 736–742. [Google Scholar] [CrossRef] [PubMed]
- Meadow, A.; Sangl, J. Hospital Readmissions in Medicare Home Healthcare: What Are the Leading Risk Indicators? Home Health. Now. 2019, 37, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, M.K.; Nielsen, G.L.; Uhrenfeldt, L.; Lundbye-Christensen, S. Risk Assessment of Acute, All-Cause 30-Day Readmission in Patients Aged 65+: A Nationwide, Register-Based Cohort Study. J. Gen. Intern. Med. 2019, 34, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Mehta, H.B.; Sieloff, E.; Veeranki, S.P.; Sura, S.D.; Riall, T.S.; Senagore, A.J.; Goodwin, J.S. Risk Prediction Models for Hospital Readmission in Surgery: A Systematic Review. J. Am. Coll. Surg. 2017, 225, e113. [Google Scholar] [CrossRef]
- Brooke, B.S.; Goodney, P.P.; Kraiss, L.W.; Gottlieb, D.J.; Samore, M.H.; Finlayson, S.R. Readmission destination and risk of mortality after major surgery: An observational cohort study. Lancet 2015, 386, 884–895. [Google Scholar] [CrossRef]
- Kansagara, D.; Englander, H.; Salanitro, A.; Kagen, D.; Theobald, C.; Freeman, M.; Kripalani, S. Risk Prediction Models for Hospital Readmission A Systematic Review. JAMA-J. Am. Med. Assoc. 2011, 306, 1688–1698. [Google Scholar] [CrossRef]
- Burke, R.E.; Schnipper, J.L.; Williams, M.V.; Robinson, E.J.; Vasilevskis, E.E.; Kripalani, S.; Metlay, J.P.; Fletcher, G.S.; Auerbach, A.D.; Donze, J.D. The HOSPITAL Score Predicts Potentially PrevenTable 30-Day Readmissions in Conditions Targeted by the Hospital Readmissions Reduction Program. Med. Care 2017, 55, 285–290. [Google Scholar] [CrossRef]
- Zhou, H.; Della, P.R.; Roberts, P.; Goh, L.; Dhaliwal, S.S. Utility of models to predict 28-day or 30-day unplanned hospital readmissions: An updated systematic review. BMJ Open 2016, 6, e011060. [Google Scholar] [CrossRef]
- Aubert, C.E.; Folly, A.; Mancinetti, M.; Hayoz, D.; Donze, J.D. Prospective validation and adaptation of the HOSPITAL score to predict high risk of unplanned readmission of medical patients. Swiss Med. Wkly. 2016, 146. [Google Scholar] [CrossRef][Green Version]
- Cooksley, T.; Nanayakkara, P.W.B.; Nickel, C.H.; Subbe, C.P.; Kellett, J.; Kidney, R.; Merten, H.; Van Galen, L.; Henriksen, D.P.; Lassen, A.T.; et al. Readmissions of medical patients: An external validation of two existing prediction scores. QJM-Int. J. Med. 2016, 109, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Cotter, P.E.; Bhalla, V.K.; Wallis, S.J.; Biram, R.W.S. Predicting readmissions: Poor performance of the LACE index in an older UK population. Age Ageing 2012, 41, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Robinson, R.; Hudali, T. The HOSPITAL score and LACE index as predictors of 30 day readmission in a retrospective study at a university-affiliated community hospital. PeerJ 2017, 5. [Google Scholar] [CrossRef] [PubMed]
- Pesko, M.F.; Gerber, L.M.; Peng, T.R.; Press, M.J. Home Health Care: Nurse-Physician Communication, Patient Severity, and Hospital Readmission. Health Serv. Res. 2018, 53, 1008–1024. [Google Scholar] [CrossRef]
- Simpson, M.; Macias Tejada, J.; Driscoll, A.; Singh, M.; Klein, M.; Malone, M. The Bundled Hospital Elder Life Program-HELP and HELP in Home Care-and Its Association with Clinical Outcomes Among Older Adults Discharged to Home Healthcare. J. Am. Geriatr. Soc. 2019, 67, 1730–1736. [Google Scholar] [CrossRef] [PubMed]
- Van Walraven, C.; Dhalla, I.A.; Bell, C.; Etchells, E.; Stiell, I.G.; Zarnke, K.; Austin, P.C.; Forster, A.J. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. Can. Med. Assoc. J. 2010, 182, 551–557. [Google Scholar] [CrossRef]
- Donze, J.; Aujesky, D.; Williams, D.; Schnipper, J.L. Potentially Avoidable 30-Day Hospital Readmissions in Medical Patients Derivation and Validation of a Prediction Model. JAMA Intern. Med. 2013, 173, 632–638. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Vickers, A.J.; Cook, N.R.; Gerds, T.; Gonen, M.; Obuchowski, N.; Pencina, M.J.; Kattan, M.W. Assessing the performance of prediction models: A framework for traditional and novel measures. Epidemiology 2010, 21, 128–138. [Google Scholar] [CrossRef]
- Alba, A.C.; Agoritsas, T.; Walsh, M.; Hanna, S.; Iorio, A.; Devereaux, P.J.; McGinn, T.; Guyatt, G. Discrimination and Calibration of Clinical Prediction Models Users’ Guides to the Medical Literature. JAMA-J. Am. Med. Assoc. 2017, 318, 1377–1384. [Google Scholar] [CrossRef]
- Kerr, K.F.; Wang, Z.; Janes, H.; McClelland, R.L.; Psaty, B.M.; Pepe, M.S. Net reclassification indices for evaluating risk prediction instruments: A critical review. Epidemiology 2014, 25, 114–121. [Google Scholar] [CrossRef]
- Krijkamp, E.M.; Alarid-Escudero, F.; Enns, E.A.; Jalal, H.J.; Hunink, M.G.M.; Pechlivanoglou, P. Microsimulation Modeling for Health Decision Sciences Using R: A Tutorial. Med. Decis. Making 2018, 38, 400–422. [Google Scholar] [CrossRef] [PubMed]
- Pencina, K.M.; D’Agostino, R.B.; Vasan, R.S.; Pencina, M.J. Microsimulation model to predict incremental value of biomarkers added to prognostic models. J. Am. Med. Inf. Assoc. 2018, 25, 1382–1385. [Google Scholar] [CrossRef] [PubMed]
- Allaudeen, N.; Schnipper, J.L.; Orav, E.J.; Wachter, R.M.; Vidyarthi, A.R. Inability of providers to predict unplanned readmissions. J. Gen. Intern. Med. 2011, 26, 771–776. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, A.; Do, J.M.; Sales, V.L.; Ly, S.; Joseph, J. Impact of patient-centred home telehealth programme on outcomes in heart failure. J. Telemed. Telecare 2019, 25, 425–430. [Google Scholar] [CrossRef]
- Bhatt, S.P.; Patel, S.B.; Anderson, E.M.; Baugh, D.; Givens, T.; Schumann, C.; Sanders, J.G.; Windham, S.T.; Cutter, G.R.; Dransfield, M.T. Video Telehealth Pulmonary Rehabilitation Intervention in Chronic Obstructive Pulmonary Disease Reduces 30-Day Readmissions. Am. J. Respir. Crit. Care Med. 2019, 200, 511–513. [Google Scholar] [CrossRef]
- Cunha Ferre, M.F.; Gallo Acosta, C.M.; Dawidowski, A.R.; Senillosa, M.B.; Scozzafava, S.M.; Saimovici, J.M. 72-hour hospital readmission of older people after hospital discharge with home care services. Home Health Care Serv. 2019, 38, 153–161. [Google Scholar] [CrossRef]
- Dowding, D.W.; Russell, D.; Onorato, N.; Merrill, J.A. Technology Solutions to Support Care Continuity in Home Care: A Focus Group Study. J. Healthc. Qual. 2018, 40, 236–246. [Google Scholar] [CrossRef]
- Parry, C.; Min, S.J.; Chugh, A.; Chalmers, S.; Coleman, E.A. Further application of the care transitions intervention: Results of a randomized controlled trial conducted in a fee-for-service setting. Home Health Care Serv. 2009, 28, 84–99. [Google Scholar] [CrossRef]
- Coleman, E.A.; Parry, C.; Chalmers, S.; Min, S.J. The care transitions intervention: Results of a randomized controlled trial. Arch. Intern. Med. 2006, 166, 1822–1828. [Google Scholar] [CrossRef]
- Ballester, N.; Parikh, P.J.; Donlin, M.; May, E.K.; Simon, S.R. An early warning tool for predicting at admission the discharge disposition of a hospitalized patient. Am. J. Manag. Care 2018, 24, e325–e331. [Google Scholar]
- Tabak, Y.P.; Sun, X.W.; Nunez, C.M.; Gupta, V.; Johannes, R.S. Predicting Readmission at Early Hospitalization Using Electronic Clinical Data an Early Readmission Risk Score. Med. Care 2017, 55, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Pepe, M.S.; Fan, J.; Feng, Z.; Gerds, T.; Hilden, J. The Net Reclassification Index (NRI): A Misleading Measure of Prediction Improvement Even with Independent Test Data Sets. Stat. Biosci. 2015, 7, 282–295. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Zhao, H.; Qiu, J.; Zhu, W.; Lei, H.; Cai, Z.; Lin, W.H.; Huang, W.; Zhang, H.; Zhang, Y.T. The Different Effects of BMI and WC on Organ Damage in Patients from a Cardiac Rehabilitation Program after Acute Coronary Syndrome. Biomed. Res. Int. 2015, 2015, 942695. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Huang, X.; Ma, J.; Huang, J.; Fan, Y.; Li, H.; Qiu, J.; Zhang, H.; Huang, W. Value of three-dimensional strain parameters for predicting left ventricular remodeling after ST-elevation myocardial infarction. Int. J. Cardiovasc. Imaging 2017, 33, 663–673. [Google Scholar] [CrossRef] [PubMed]
- Flaks-Manov, N.; Topaz, M.; Hoshen, M.; Balicer, R.D.; Shadmi, E. Identifying patients at highest-risk: The best timing to apply a readmission predictive model. BMC Med. Inform. Decis. Mak. 2019, 19, 9. [Google Scholar] [CrossRef] [PubMed]
- Greenwood, K.L.; LaMori, J.C.; Smith, B.; Doshi, D.; Davis, C. Impact of Behavioral Health Screening on Proactive Identification of Patients at Risk for Hospital Readmission. Popul. Health Manag. 2019, 22, 196–204. [Google Scholar] [CrossRef]
- Miller, W.D.; Nguyen, K.; Vangala, S.; Dowling, E. Clinicians can independently predict 30-day hospital readmissions as well as the LACE index. BMC Health Serv. Res. 2018, 18, 32. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Uno, H.; Ioannidis, J.P.A.; van Calster, B.; Ukaegbu, C.; Dhingra, T.; Syngal, S.; Kastrinos, F. Poor performance of clinical prediction models: The harm of commonly applied methods. J. Clin. Epidemiol. 2018, 98, 133–143. [Google Scholar] [CrossRef]
- Eckert, C.; Nieves-Robbins, N.; Spieker, E.; Louwers, T.; Hazel, D.; Marquardt, J.; Solveson, K.; Zahidl, A.; Ahmadl, M.; Barnhill, R.; et al. Development and Prospective Validation of a Machine Learning-Based Risk of Readmission Model in a Large Military Hospital. Appl. Clin. Inform. 2019, 10, 316–325. [Google Scholar] [CrossRef]
- Morgan, D.J.; Bame, B.; Zimand, P.; Dooley, P.; Thom, K.A.; Harris, A.D.; Bentzen, S.; Ettinger, W.; Garrett-Ray, S.D.; Tracy, J.K.; et al. Assessment of Machine Learning vs Standard Prediction Rules for Predicting Hospital Readmissions. JAMA Netw. Open 2019, 2, e190348. [Google Scholar] [CrossRef]
- Min, X.; Yu, B.; Wang, F. Predictive Modeling of the Hospital Readmission Risk from Patients’ Claims Data Using Machine Learning: A Case Study on COPD. Sci. Rep. 2019, 9, 2362. [Google Scholar] [CrossRef] [PubMed]
- Walsh, C.G.; Sharma, K.; Hripcsak, G. Beyond discrimination: A comparison of calibration methods and clinical usefulness of predictive models of readmission risk. J. Biomed. Inform. 2017, 76, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Lieder, F.; Griffiths, T.L.; M Huys, Q.J.; Goodman, N.D. The anchoring bias reflects rational use of cognitive resources. Psychon. Bull. Rev. 2018, 25, 322–349. [Google Scholar] [CrossRef] [PubMed]
- Van Walraven, C.; Wong, J.; Forster, A.J. LACE+ index: Extension of a validated index to predict early death or urgent readmission after hospital discharge using administrative data. Open Med 2012, 6, e80–e90. [Google Scholar]
- Wang, H.; Robinson, R.D.; Johnson, C.; Zenarosa, N.R.; Jayswal, R.D.; Keithley, J.; Delaney, K.A. Using the LACE index to predict hospital readmissions in congestive heart failure patients. BMC Cardiovasc. Disord. 2014, 14, 97. [Google Scholar] [CrossRef]
- Low, L.L.; Lee, K.H.; Hock Ong, M.E.; Wang, S.; Tan, S.Y.; Thumboo, J.; Liu, N. Predicting 30-Day Readmissions: Performance of the LACE Index Compared with a Regression Model among General Medicine Patients in Singapore. Biomed. Res. Int. 2015, 2015, 169870. [Google Scholar] [CrossRef]
- Yazdan-Ashoori, P.; Lee, S.F.; Ibrahim, Q.; Van Spall, H.G. Utility of the LACE index at the bedside in predicting 30-day readmission or death in patients hospitalized with heart failure. Am. Heart J. 2016, 179, 51–58. [Google Scholar] [CrossRef]
- Damery, S.; Combes, G. Evaluating the predictive strength of the LACE index in identifying patients at high risk of hospital readmission following an inpatient episode: A retrospective cohort study. BMJ Open 2017, 7, e016921. [Google Scholar] [CrossRef]
- Low, L.L.; Liu, N.; Ong, M.E.H.; Ng, E.Y.; Ho, A.F.W.; Thumboo, J.; Lee, K.H. Performance of the LACE index to identify elderly patients at high risk for hospital readmission in Singapore. Medicine (Baltimore) 2017, 96, e6728. [Google Scholar] [CrossRef]
- Baig, M.; Zhang, E.; Robinson, R.; Ullah, E.; Whitakker, R. Evaluation of Patients at Risk of Hospital Readmission (PARR) and LACE Risk Score for New Zealand Context. Stud. Health Technol. Inform. 2018, 252, 21–26. [Google Scholar]
- Hakim, M.A.; Garden, F.L.; Jennings, M.D.; Dobler, C.C. Performance of the LACE index to predict 30-day hospital readmissions in patients with chronic obstructive pulmonary disease. Clin. Epidemiol. 2018, 10, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Saluk, J.L.; Blackwell, R.H.; Gange, W.S.; Zapf, M.A.C.; Kothari, A.N.; Kuo, P.C.; Quek, M.L.; Flanigan, R.C.; Gupta, G.N. The LACE Score as a Tool to Identify Radical Cystectomy Patients at Increased Risk of 90-Day Readmission and Mortality. Curr. Urol. 2018, 12, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Caplan, I.F.; Sullivan, P.Z.; Kung, D.; O’Rourke, D.M.; Choudhri, O.; Glauser, G.; Osiemo, B.; Goodrich, S.; McClintock, S.D.; Malhotra, N.R. LACE+ Index as Predictor of 30-Day Readmission in Brain Tumor Population. World Neurosurg. 2019, 127, e443. [Google Scholar] [CrossRef] [PubMed]
- Caplan, I.F.; Zadnik Sullivan, P.; Glauser, G.; Choudhri, O.; Kung, D.; O’Rourke, D.M.; Osiemo, B.; Goodrich, S.; McClintock, S.D.; Malhotra, N.R. The LACE+ index fails to predict 30–90 day readmission for supratentorial craniotomy patients: A retrospective series of 238 surgical procedures. Clin. Neurol. Neurosurg. 2019, 182, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.M.; Koester, C.; Al-Akchar, M.; Tandan, N.; Regmi, M.; Bhattarai, M.; Al-Bast, B.; Kulkarni, A.; Robinson, R. HOSPITAL Score, LACE Index and LACE+ Index as predictors of 30-day readmission in patients with heart failure. BMJ Evid. Based Med. 2019. [Google Scholar] [CrossRef]
- Robinson, R.; Bhattarai, M.; Hudali, T.; Vogler, C. Predictors of 30-day hospital readmission: The direct comparison of number of discharge medications to the HOSPITAL score and LACE index. Future Healthc. J. 2019, 6, 209–214. [Google Scholar] [CrossRef]
- Shaffer, B.K.; Cui, Y.; Wanderer, J.P. Validation of the LACE readmission and mortality prediction model in a large surgical cohort: Comparison of performance at preoperative assessment and discharge time points. J. Clin. Anesth 2019, 58, 22–26. [Google Scholar] [CrossRef]
- Donze, J.D.; Williams, M.V.; Robinson, E.J.; Zimlichman, E.; Aujesky, D.; Vasilevskis, E.E.; Kripalani, S.; Metlay, J.P.; Wallington, T.; Fletcher, G.S.; et al. International Validity of the HOSPITAL Score to Predict 30-Day Potentially Avoidable Hospital Readmissions. JAMA Intern. Med. 2016, 176, 496–502. [Google Scholar] [CrossRef]
- Kim, L.D.; Kou, L.; Messinger-Rapport, B.J.; Rothberg, M.B. Validation of the HOSPITAL Score for 30-Day All-Cause Readmissions of Patients Discharged to Skilled Nursing Facilities. J. Am. Med. Dir. Assoc. 2016, 17. [Google Scholar] [CrossRef]
- Robinson, R. The HOSPITAL score as a predictor of 30 day readmission in a retrospective study at a university affiliated community hospital. PeerJ 2016, 4. [Google Scholar] [CrossRef][Green Version]
- Aubert, C.E.; Schnipper, J.L.; Williams, M.V.; Robinson, E.J.; Zimlichman, E.; Vasilevskis, E.E.; Kripalani, S.; Metlay, J.P.; Wallington, T.; Fletcher, G.S.; et al. Simplification of the HOSPITAL score for predicting 30-day readmissions. BMJ Qual. Saf. 2017, 26, 799–805. [Google Scholar] [CrossRef]

| Demographics and Parameters | All Acute Hospitalizations (n = 87) | Acute Hospitalization Followed by 30-Day Readmission (n = 22) | Acute Hospitalization with Successful Discharge (n = 65) | - | - | |||
|---|---|---|---|---|---|---|---|---|
| Mean | (SD 1) | Mean | (SD 1) | Mean | (SD 1) | p-Value | Sig. 2 | |
| Personal demographics | ||||||||
| Gender | - | - | - | - | - | - | 0.055 | - |
| Female, no. (%) | 40 | (46.0) | 14 | (63.6) | 26 | (40.0) | - | - |
| Male, no. (%) | 47 | (54.0) | 8 | (36.4) | 39 | (60.0) | - | - |
| Age | 87.4 | (12.4) | 89.0 | (8.1) | 86.9 | (13.6) | 0.482 | - |
| LACE prediction model | ||||||||
| Length of stay (L) | 5.6 | (0.7) | 5.6 | (0.6) | 2.6 | (0.6) | 0.654 | - |
| Acuity of admission (A) | 2.7 | (0.9) | 2.9 | (0.6) | 2.6 | (0.6) | 0.21 | - |
| Comorbidities (C) | 1.7 | (0.9) | 1.6 | (0.9) | 1.7 | (0.9) | 0.864 | - |
| Emergency department visits (E) | 1.9 | (1.3) | 2.5 | (1.1) | 1.7 | (1.1) | 0.017 | * |
| LACE index | 11.8 | (2.6) | 12.5 | (1.8) | 11.5 | (1.8) | 0.053 | - |
| HOSPITAL prediction model 3 | ||||||||
| Hemoglobin level (H) | 0.7 | (0.5) | 0.9 | (0.4) | 0.6 | (0.5) | 0.009 | ** |
| Sodium level (S) | 0.3 | (0.4) | 0.1 | (0.3) | 0.3 | (0.5) | 0.009 | ** |
| Procedure during the index admission (P) | 0.3 | (0.5) | 0.3 | (0.5) | 0.3 | (0.5) | 0.967 | - |
| Index type of admission (IT) | 0.9 | (0.3) | 0.9 | (0.3) | 0.8 | (0.4) | 0.465 | - |
| Number of admissions (A) | 1.7 | (1.2) | 2.3 | (1.2) | 1.5 | (1.2) | 0.007 | ** |
| Length of stay (L) | 1.9 | (0.4) | 2.0 | (0.0) | 1.9 | (0.4) | 0.083 | - |
| HOSPITAL score | 5.8 | (1.6) | 6.6 | (1.4) | 5.5 | (1.6) | 0.003 | ** |
| 30-Day Readmission Prediction Models | Area under Curve (AUC) | (95% C.I.) | p-Value | Sig. 1 | - |
| LACE index | 0.598 | (0.474–0.722) | 0.170 | - | - |
| HOSPITAL score | 0.691 | (0.573–0.808) | 0.008 | ** | - |
| 30-Day Readmission Prediction Models | Accuracy (%) | Sensitivity (%) | (95% CI) | Specificity (%) | (95% CI) |
| LACE index | 54.5 | 81.8 | (59.7–94.8) | 44.6 | (32.3–57.5) |
| HOSPITAL score | 54.0 | 90.9 | (70.8–98.9) | 41.5 | (29.4–54.4) |
| 30-Day Readmission Prediction Models 1 | 30-Day Readmission Rate Reduction (%) | (IQR 3) | Cost of Preventive Intervention (%) 4 | (IQR 2) |
|---|---|---|---|---|
| LACE index | 39.2 | (39.1–39.4) | 66.8 | (61.0–72.6) |
| HOSPITAL score | 43.4 | (43.3–43.5) | 72.0 | (63.1–79.4) |
| Attending physician | 10.1 | (9.8–10.3) | 18.6 | (17.2–19.9) |
| All intervention | 50.0 | (50.0–50.0) | 100 (reference) | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, M.-C.; Wang, Y.-J.; Chen, T.-J.; Chiu, S.-H.; Chang, H.-T.; Huang, M.-S.; Hu, L.-H.; Li, C.-C.; Yang, S.-J.; Wu, J.-C.; et al. Assess the Performance and Cost-Effectiveness of LACE and HOSPITAL Re-Admission Prediction Models as a Risk Management Tool for Home Care Patients: An Evaluation Study of a Medical Center Affiliated Home Care Unit in Taiwan. Int. J. Environ. Res. Public Health 2020, 17, 927. https://doi.org/10.3390/ijerph17030927
Su M-C, Wang Y-J, Chen T-J, Chiu S-H, Chang H-T, Huang M-S, Hu L-H, Li C-C, Yang S-J, Wu J-C, et al. Assess the Performance and Cost-Effectiveness of LACE and HOSPITAL Re-Admission Prediction Models as a Risk Management Tool for Home Care Patients: An Evaluation Study of a Medical Center Affiliated Home Care Unit in Taiwan. International Journal of Environmental Research and Public Health. 2020; 17(3):927. https://doi.org/10.3390/ijerph17030927
Chicago/Turabian StyleSu, Mei-Chin, Yi-Jen Wang, Tzeng-Ji Chen, Shiao-Hui Chiu, Hsiao-Ting Chang, Mei-Shu Huang, Li-Hui Hu, Chu-Chuan Li, Su-Ju Yang, Jau-Ching Wu, and et al. 2020. "Assess the Performance and Cost-Effectiveness of LACE and HOSPITAL Re-Admission Prediction Models as a Risk Management Tool for Home Care Patients: An Evaluation Study of a Medical Center Affiliated Home Care Unit in Taiwan" International Journal of Environmental Research and Public Health 17, no. 3: 927. https://doi.org/10.3390/ijerph17030927
APA StyleSu, M.-C., Wang, Y.-J., Chen, T.-J., Chiu, S.-H., Chang, H.-T., Huang, M.-S., Hu, L.-H., Li, C.-C., Yang, S.-J., Wu, J.-C., & Chen, Y.-C. (2020). Assess the Performance and Cost-Effectiveness of LACE and HOSPITAL Re-Admission Prediction Models as a Risk Management Tool for Home Care Patients: An Evaluation Study of a Medical Center Affiliated Home Care Unit in Taiwan. International Journal of Environmental Research and Public Health, 17(3), 927. https://doi.org/10.3390/ijerph17030927








