Keeping People with Dementia or Mild Cognitive Impairment in Employment: A Literature Review on Its Determinants
Abstract
1. Introduction
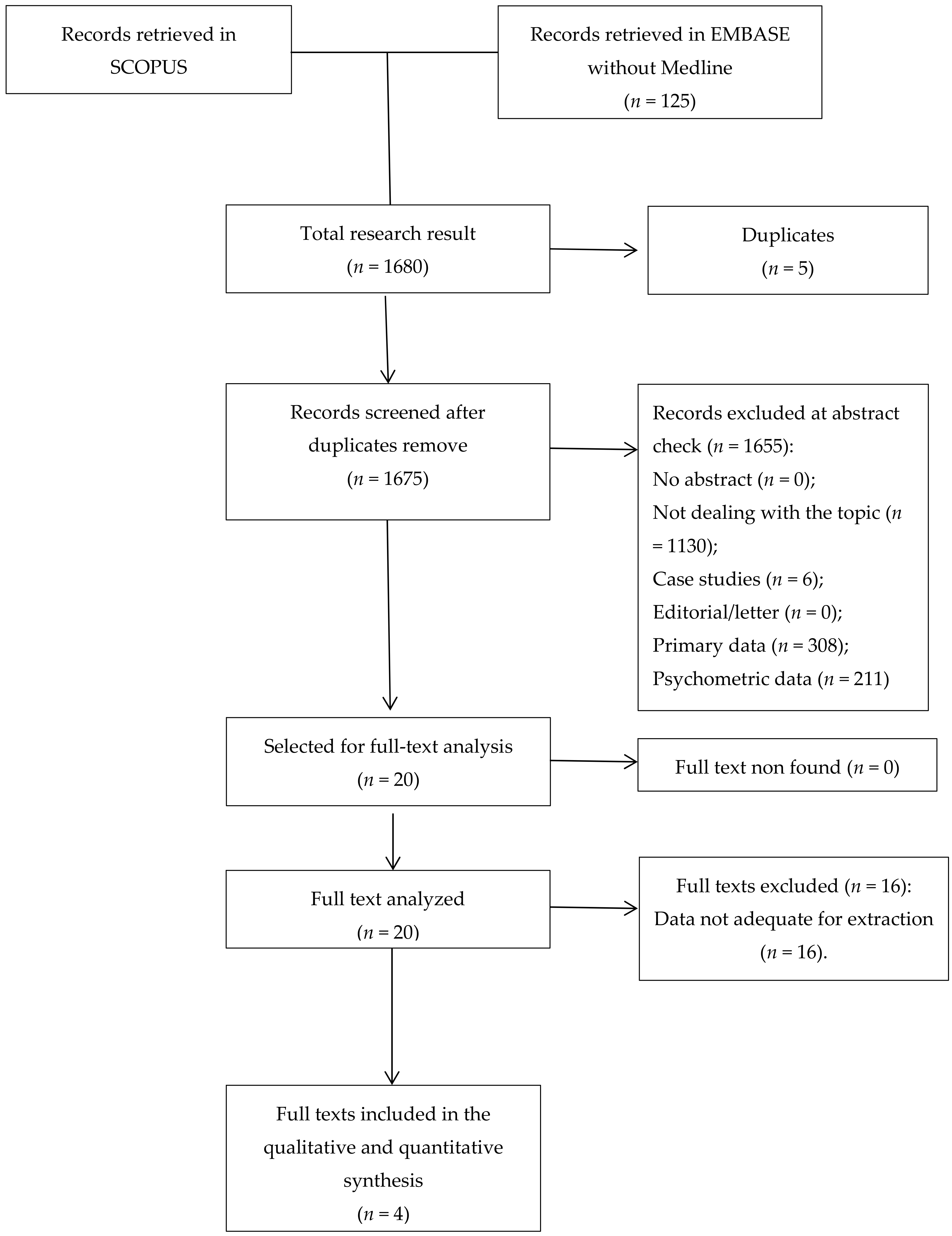
2. Materials and Methods
2.1. Search Strategy
2.2. Articles’ Inclusion and Exclusion Criteria
2.3. Paper Selection and Data Extraction
3. Results
3.1. Management of Dementia in the Workplace
3.2. The Impact of Symptoms on Working Status
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Cunningham, E.L.; McGuinness, B.; Herron, B.; Passmore, A.P. Dementia. Ulster Med. J. 2015, 84, 79–87. [Google Scholar] [PubMed]
- Thakur, T.K.; Albanese, E.; Giannakopoulos, P.; Jette, N.; Linde, M.; Prince, M.J.; Steiner, T.J.; Dua, T. Neurological disorders. Mental, Neurological, and Substance Use Disorders: Disease Control Priorities, 3rd ed.; Patel, V., Chisholm, D., Dua, T., Laxminarayan, R., Medina, M., Eds.; The International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA, 2016. [Google Scholar]
- Garre-Olmo, J.; Genís Batlle, D.; del Mar, F.M.; Marquez, D.F.; de Eugenio Huélamo, R.; Casadevall, T.; Turbau Recio, J.; Turon Estrada, A.; López-Pousa, S. Incidence and subtypes of early-onset dementia in a geographically defined general population. Neurology 2010, 75, 1249–1255. [Google Scholar] [CrossRef] [PubMed]
- Ratanavalli, E.; Brayne, C.; Dawson, K.; Hodges, J.R. The prevalence of frontotemporal dementia. Neurology 2002, 58, 1615–1621. [Google Scholar] [CrossRef] [PubMed]
- Harvey, R.J.; Skelton-Robinson, M.; Rossor, M.N. The prevalence and causes of dementia in people under the age of 65 years. J. Neurol. Neurosurg. Psychiatry 2003, 74, 1206–1209. [Google Scholar] [CrossRef] [PubMed]
- Rosso, S.M.; Kaat, L.D.; Baks, T.; Joosse, M.; Koning, I.; Pijnenburg, Y.; Jong, D.; Dooijes, D.; Kamphorst, W.; Ravid, R.; et al. Frontotemporal dementia in The Netherlands: Patient characteristics and prevalence estimates from a population-based study. Brain 2003, 126, 2016–2022. [Google Scholar] [CrossRef] [PubMed]
- Sanford, A.M. Mild Cognitive Impairment. Clin. Geriatr. Med 2017, 33, 325–337. [Google Scholar] [CrossRef]
- World Health Organisation (WHO). Dementia: A Public Health Priority, The World Health Organization; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Evans, D. An exploration of the impact of younger-onset dementia on employment. Dementia 2016, 8, 262–281. [Google Scholar] [CrossRef]
- Chaplin, R.; Davidson, I. What are the experiences of people with dementia in employment? Dementia 2016, 15, 147–161. [Google Scholar] [CrossRef]
- Braudy Harris, P. The perspectives of younger people with dementia: Still an overlooked population. Soc. Work Ment. Health 2004, 2, 17–36. [Google Scholar] [CrossRef]
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2017 Revision Volume II: Demographic Profiles; United Unions: New York, NY, USA, 2012. [Google Scholar]
- Mutlu, U.; Colijn, J.M.; Ikram, M.A.; Bonnemaijer, P.W.M.; Licher, S.; Wolters, F.J.; Tiemeier, H.; Koudstaal, P.J.; Klaver, C.C.W.; Ikram, M.K. Association of Retinal Neurodegeneration on Optical Coherence Tomography With Dementia: A Population-Based Study. JAMA Neurol. 2018, 75, 1256–1263. [Google Scholar] [CrossRef]
- Moreland, J.; Urhemaa, T.; van Gils, M.; Lötjönen, J.; Wolber, J.; Buckley, C.J. Validation of prognostic biomarker scores for predicting progression of dementia in patients with amnestic mild cognitive impairment. Nucl. Med. Commun. 2018, 39, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Donadio, V.; Incensi, A.; Rizzo, G.; Capellari, S.; Pantieri, R.; Stanzani Maserati, M.; Devigili, G.; Eleopra, R.; Defazio, G.; Montini, F.; et al. A new potential biomarker for dementia with Lewy bodies: Skin nerve α-synuclein deposits. Neurology 2017, 89, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Conway, E. Relating career stage to attitudes towards HR practices and commitment: Evidence of interaction effects? Eur. J. Work Organ. Psychol. 2004, 13, 417–446. [Google Scholar] [CrossRef]
- Guella, I.; Evans, D.M.; Szu-Tu, C.; Nosova, E.; Bortnick, S.F.; Goldman, J.G.; Dalrymple-Alford, J.C.; Geurtsen, G.J.; Litvan, I.; Ross, O.A.; et al. α-synuclein genetic variability: A biomarker for dementia in Parkinson disease. Ann. Neurol. 2016, 79, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Danaei, G.; Finucane, M.; Lu, Y.; Singh, G.M.; Cowan, M.J.; Paciorek, C.J.; Lin, J.K.; Farzadfar, F.; Khang, Y.H.; Stevens, G.A.; et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011, 378, 31–40. [Google Scholar] [CrossRef]
- Ohara, T.; Doi, Y.; Ninomiya, T. Glucose tolerance status and risk of dementia in the community: The Hisayama study. Neurology 2011, 77, 1126–1134. [Google Scholar] [CrossRef] [PubMed]
- Toossi, M. Labor force projections to 2014: Retiring boomers. Monthly Labor Rev. 2005, 128, 25–44. [Google Scholar]
- The National Audit Office London. Sustainable employment: supporting people to stay in work and advance; London. 2007. Available online: https://www.nao.org.uk/wp-content/uploads/2007/11/070832.pdf (accessed on 14 November 2018).
- Fleishman, E.A.; Reilly, M.E. Handbook of Human Abilities: Definitions, Measurements and Job Task Requirements; Consulting Psychologists Press: Mountain View, CA, USA, 1995. [Google Scholar]
- Ilmarinen, J. Work ability—A comprehensive concept for occupational health research and prevention. Scand. J. Work Environ. Health 2008, 35, 1–5. [Google Scholar] [CrossRef]
- Ilmarinen, J. Towards a Longer Worklife; FIOH Bookstore: Helsinki, Finland, 2005. [Google Scholar]
- Peltomäki, P.; Husman, K. Occupational health services and maintenance of work ability. Arh. Hig. Rada. Toksikol. 2012, 53, 263–274. [Google Scholar]
- Finnish Institute of Occupational Health. Maintenance of Work Ability Research and Assessment: Summaries; Social Insurance Institution: Helsinki, Finland, 2002. [Google Scholar]
- Waddell, G.; Burton, K. Is Work Good for Your Health and Wellbeing? TSO. 2016. Available online: https://cardinal-management.co.uk/wp-content/uploads/2016/04/Burton-Waddell-is-work-good-for-you.pdf (accessed on 14 November 2018).
- Gabriel, Y.; Gray, D.E.; Goregaokar, H. Temporary derailment or the end of the line? Managers coping with unemployment at 50. Organ. Stud. 2010, 31, 1687–1712. [Google Scholar] [CrossRef]
- Pejrova, I. Changing the perception of younger workers towards older workers: Workers under the age of imagine themselves as older ones. Medicine 2014, 18, 152–160. [Google Scholar] [CrossRef]
- Dibben, P.; James, P.; Cunningham, I.; Smythe, D. Employers and employees with disabilities in the UK: An economically beneficial relationship? Int. J. Soc. Econ. 2002, 29, 453–467. [Google Scholar] [CrossRef]
- Christ, S.L.; Lee, D.J.; Fleming, L.E.; LeBlanc, W.G.; Arheart, K.L.; Chung-Bridges, K.; Caban, A.J.; McCollister, K.E. Employment and occupation effects on depressive symptoms in older Americans: Does working past age protect against depression? J. Gerontol. Psychol. Sci. Soc. Sci. 2007, 62B, S399–S403. [Google Scholar] [CrossRef] [PubMed]
- Taskila, T.; Shreeve, V.; Laghini, M.; Bevan, S. Living Long, Working Well: Supporting Older Workers with Health Conditions to Remain Active at Work. The Work Foundation. 2015. Available online: http://www.theworkfoundation.com/wp-content/uploads/2016/11/386_Living_long_working_well_Final.pdf (accessed on 17 February 2019).
- Ohman, O.; Nygard, L.; Borell, L. The vocational situation in cases of memory deficits or young onset dementia. Scand. J. Caring Sci. 2001, 15, 34–43. [Google Scholar] [CrossRef]
- Harris, P.B.; Keady, J. Selfhood in younger onset dementia: Transitions and testimonies. Aging Ment. Health 2009, 13, 437–444. [Google Scholar] [CrossRef]
- Luscombe, G.; Brodaty, H.; Freeth, S. Younger people with dementia: Diagnostic issues, effects on carers and use of services. Int. J. Geriatr. Psychiatry 1998, 13, 323–330. [Google Scholar] [CrossRef]
- Roach, P.; Keady, J. Younger people with dementia: Time for fair play. Br. J. Nurs. 2008, 17, 690. [Google Scholar] [CrossRef]
- Robertson, J.; Evans, D.; Horsnell, T. Side by Side: A workplace engagement program for people with younger onset dementia. Dementia 2013, 12, 666–674. [Google Scholar] [CrossRef]
- Sakata, N.; Okumura, Y. Job Loss After Diagnosis of Early-Onset Dementia: A Matched Cohort Study. J. Alzheimers Dis. 2017, 60, 1231–1235. [Google Scholar] [CrossRef]
- Jacobs, M.; Hart, E.P.; Roos, R.A.C. Cognitive Performance and Apathy Predict Unemployment in Huntington’s Disease Mutation Carriers. J. Neuropsychiatry Clin. Neurosci. 2018, 30, 188–193. [Google Scholar] [CrossRef]
- Watkins, K.; Purks, J.; Kumar, A.; Sokas, R.K.; Heller, H.; Anderson, K.E. Huntington’s Disease and Employment: The Relative Contributions of Cognitive and Motor Decline to the Decision to Leave Work. J. Huntingtons. Dis. 2018, 7, 367–377. [Google Scholar] [CrossRef]
- Erol, R.; Brooker, D.; Peel, E. Women and Dementia—A Global Research Review; Alzheimer’s Disease International: Worchester, UK, 2015. [Google Scholar]
- Rottenberg, Y.; Ratzon, N.Z.; Cohen, M.; Hubert, A.; Uziely, B.; de Boer, A.G.E.M. Unemployment risk at 2 and 4 years following colorectal cancer diagnosis: A population based study. Eur. J. Cancer 2016, 69, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Sherman, C.; Liu, C.S.; Herrmann, N.; Lanctôt, K.L. Prevalence, neurobiology, and treatments for apathy in prodromal dementia. Int. Psychogeriatr. 2018, 30, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Naarding, P.; Janzing, J.G.E.; Eling, P.; van der Werf, S.; Kremer, B. Apathy Is Not Depression in Huntington’s Disease. J. Neuropsychiatry Clin. Neurosci. 2009, 21. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, J.M.; Salmon, D.P.; Corey-Bloom, J.; Gamst, A.; Paulsen, J.S.; Jerkins, S.; Jacobson, M.W.; Peavy, G. Behavioural abnormalities contribute to functional decline in Huntington’s disease. J. Neurol. Neurosurg. Psychiatry 2003, 74, 120–122. [Google Scholar] [CrossRef] [PubMed]
- Clarke, D.E.; Ko, Y.J.; Kuhl, E.A.; van Reekum, R.; Salvador, R.; Marin, R.S. Are the available apathy measures reliable and valid? A review of the psychometric evidence. J. Psychosom. Res. 2011, 70, 73–97. [Google Scholar] [CrossRef]
- Zuelke, A.E.; Luck, T.; Schroeter, M.L.; Witte, A.V.; Hinz, A.; Engel, C.; Enzenbach, C.; Zachariae, S.; Loeffler, M.; Thiery, J.; et al. The association between unemployment and depression-Results from the population-based LIFE-adult-study. J. Affect. Disord. 2018, 235, 399–406. [Google Scholar] [CrossRef]
- Lerner, D.; Adler, D.A.; Chang, H.; Lapitsky, L.; Hood, M.Y.; Perissinotto, C.; Reed, J.; McLaughlin, T.J.; Berndt, E.R.; Rogers, W.H. Unemployment, job retention, and productivity loss among employees with depression. Psychiatr. Serv. 2004, 55, 1371–1378. [Google Scholar] [CrossRef]
- Klaus, P. Communication breakdown. Job J. 2010, 28, 1–9. [Google Scholar]
- John, J. Study on The Nature of Impact of Soft Skills Training Programme on The Soft Skills Development of Management Students. Pac. Bus. Rev. 2009. Available online: http://ssrn.com/abstract=1591331 (accessed on 14 May 2018).
- Fundarò, C.; Casale, R. Rehabilitation and dementia in the era of elderly workers. Giornale Italiano di Medicina del Lavoro ed Ergonomia 2012, 34, 197–201. [Google Scholar]
- Robles, M.M. Executive Perceptions of the Top 10 Soft Skills Needed in Today’s Workplace. Bus. Commun. Q. 2012, 74, 453–465. [Google Scholar] [CrossRef]
- Worach-Kardas, H.; Kostrzewski, S. Quality of Life and Health State of Long—Term Unemployed in Older Production Age. Appl. Res. Qual. Life 2014, 9, 335–353. [Google Scholar] [CrossRef] [PubMed]
- Marder, K.; Zhao, H.; Myers, R.H.; Cudkowicz, M.; Kayson, E.; Kieburtz, K.; Orme, C.; Paulsen, J.; Penney, J.B.; Siemers, E.; et al. Rate of functional decline in Huntington’s disease. Huntington Study Group. Neurology 2000, 54, 452–458. [Google Scholar] [CrossRef]
- Ross, C.A.; Pantelyat, A.; Kogan, J.; Brandt, J. Determinants of functional disability in Huntington’s disease: Role of cognitive and motor dysfunction. Mov. Disord 2014, 29, 1351–1358. [Google Scholar] [CrossRef]
- Ebbitt, B.; Burns, T.; Christensen, R. Work therapy: Intervention for community based Alzheimer’s patients. Am. J. Alzheimer ’s Care Related Disord. Res. 1989, 4, 7–15. [Google Scholar] [CrossRef]
- de Bruin, S.; Oosting, S.; van der Zijpp, A.; Enders-Slegers, M.J.; Schols, J. The concept of green care farms for older people with dementia: An integrative framework. Dementia 2010, 9, 79–128. [Google Scholar] [CrossRef]
- Kinney, J.M.; Kart, C.S.; Reddecliff, L. ‘That’s me, the Goother’: Evaluation of a program for individuals with early-onset dementia. Dementia 2011, 10, 361–377. [Google Scholar] [CrossRef]
- Roach, P.; Drummond, N. ′It’s nice to have something to do’: Early-onset dementia and maintaining purposeful activity. J. Psychiatr. Ment. Health Nurs. 2014, 21, 889–895. [Google Scholar] [CrossRef]
- Cantarero-Prieto, D.; Leon, P.L.; Blazquez-Fernandez, C.; Juan, P.S.; Cobo, C.S. The economic cost of dementia: A systematic review. Dementia 2019, 0, 1–21. [Google Scholar] [CrossRef]
| ID | Dementia Type | Sample Size | Age | Male Gender (%) | Employed (%) | Main Results |
|---|---|---|---|---|---|---|
| Robertson et al., 2013 [37] | EOD | 7 | 57.5 (50–65) b | 4 (57.1%) | 7 (100%) | Appropriate support povided in the workplace is associated with improvement of the work ability in patients with EOD. |
| Jacobs et al., 2018 [38] | HD | 220 | 46.6 (19–75) b | 96 (43.6%) | 114 (52%) | Apathy and cognitive impairments (information processing speed and cognitive flexibility) are determinants of unemployment in patients with HD. |
| Sakata et al., 2017 [39] | EOD | 143 | 53 (48–57) a | 19 (13%) | 143 (100%) | A total of 14% of patients with EOD left their jobs within one year after their diagnosis (7.3% among those without EOD). |
| Watkins et al., 2018 [40] | HD | 642 | 18–65 | 298 (46%) | 305 (44%) | Cognitive symptoms and motor symptoms have a significant influence on decline of work ability and on the decision to leave work in patients with HD |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silvaggi, F.; Leonardi, M.; Tiraboschi, P.; Muscio, C.; Toppo, C.; Raggi, A. Keeping People with Dementia or Mild Cognitive Impairment in Employment: A Literature Review on Its Determinants. Int. J. Environ. Res. Public Health 2020, 17, 842. https://doi.org/10.3390/ijerph17030842
Silvaggi F, Leonardi M, Tiraboschi P, Muscio C, Toppo C, Raggi A. Keeping People with Dementia or Mild Cognitive Impairment in Employment: A Literature Review on Its Determinants. International Journal of Environmental Research and Public Health. 2020; 17(3):842. https://doi.org/10.3390/ijerph17030842
Chicago/Turabian StyleSilvaggi, Fabiola, Matilde Leonardi, Pietro Tiraboschi, Cristina Muscio, Claudia Toppo, and Alberto Raggi. 2020. "Keeping People with Dementia or Mild Cognitive Impairment in Employment: A Literature Review on Its Determinants" International Journal of Environmental Research and Public Health 17, no. 3: 842. https://doi.org/10.3390/ijerph17030842
APA StyleSilvaggi, F., Leonardi, M., Tiraboschi, P., Muscio, C., Toppo, C., & Raggi, A. (2020). Keeping People with Dementia or Mild Cognitive Impairment in Employment: A Literature Review on Its Determinants. International Journal of Environmental Research and Public Health, 17(3), 842. https://doi.org/10.3390/ijerph17030842





