Economic Evaluation of Hepatitis C Treatment Extension to Acute Infection and Early-Stage Fibrosis Among Patients Who Inject Drugs in Developing Countries: A Case of China
Abstract
1. Introduction
2. Materials and Methods
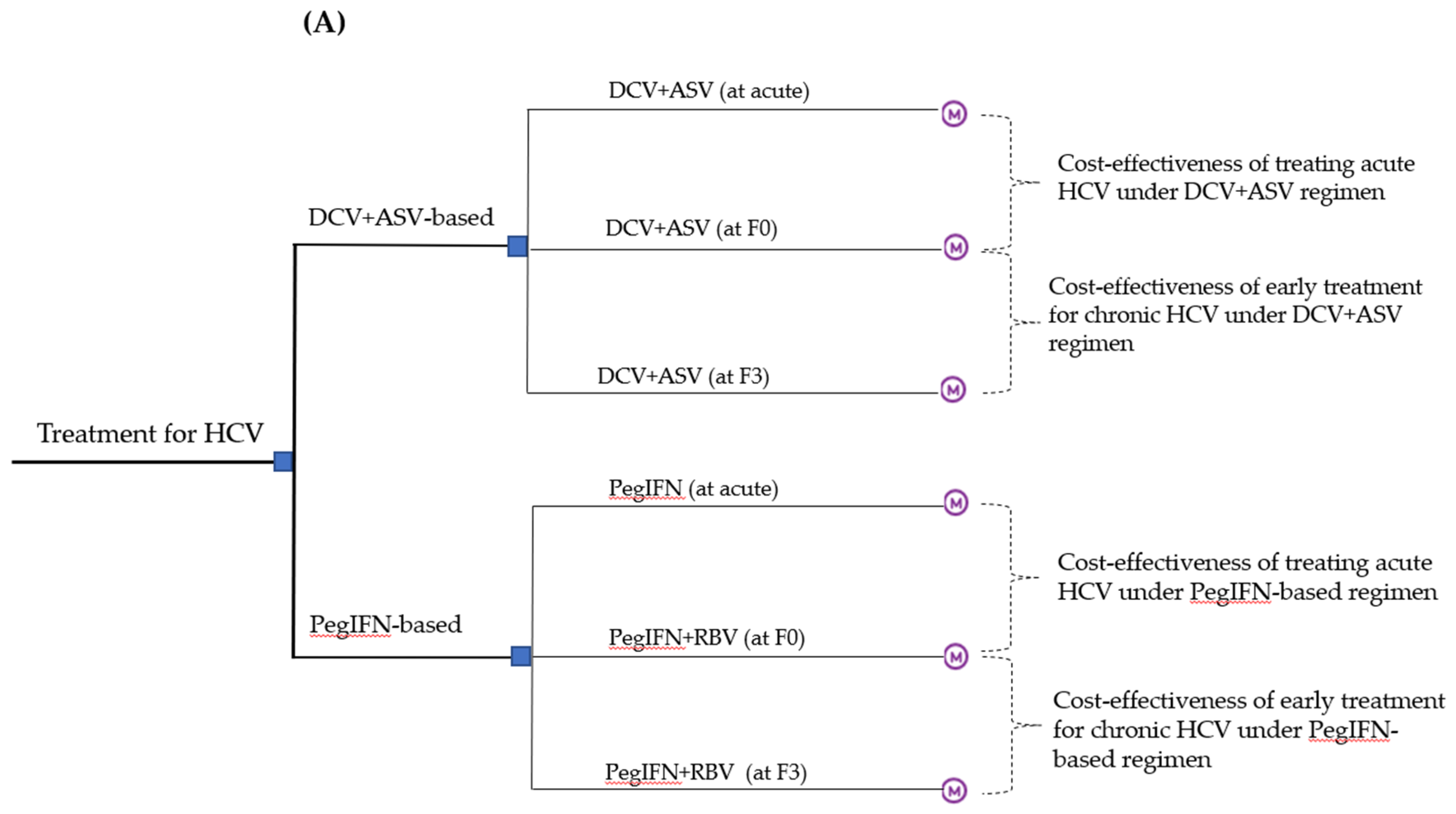
2.1. Model Overview
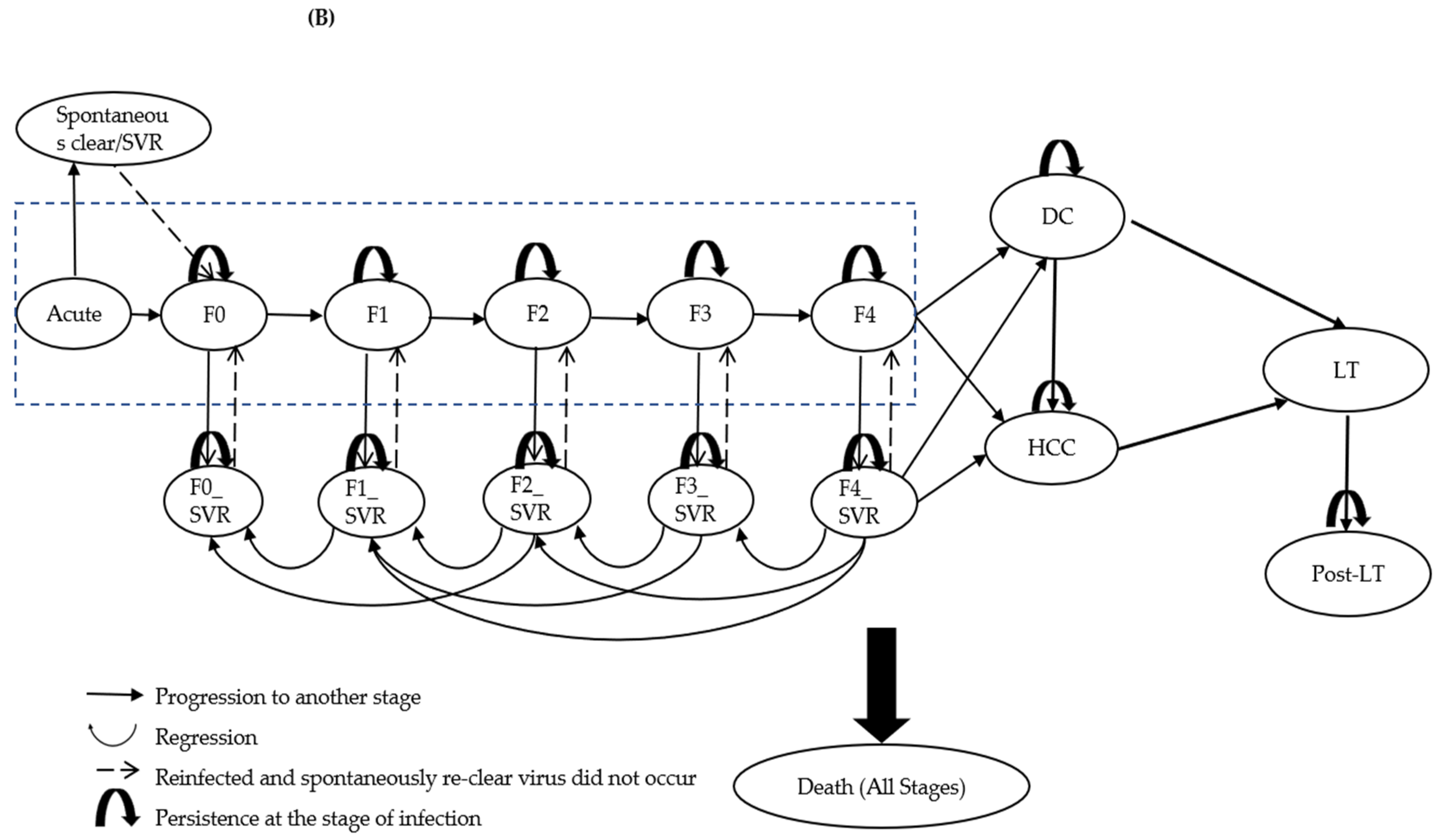
2.2. Natural History of HCV Infection
2.3. Patient Cohort
2.4. Progression, Regression and Reinfection after SVR
2.5. Mortality
2.6. Treatment Strategies
2.7. Costs and Health State Utility Values
2.8. Model Outcomes and Statistical Analysis
3. Results
3.1. Base-Case Results
3.1.1. Cost-Effectiveness of Treating Acute HCV among PWID
3.1.2. Cost-Effectiveness of Early Treatment at F0 Stage for Chronic HCV among PWID
3.2. One-Way Sensitivity Analysis
3.2.1. Cost-Effectiveness of Treating Acute HCV among PWID
3.2.2. Cost-Effectiveness of Early Treatment at F0 Stage for Chronic HCV among PWID
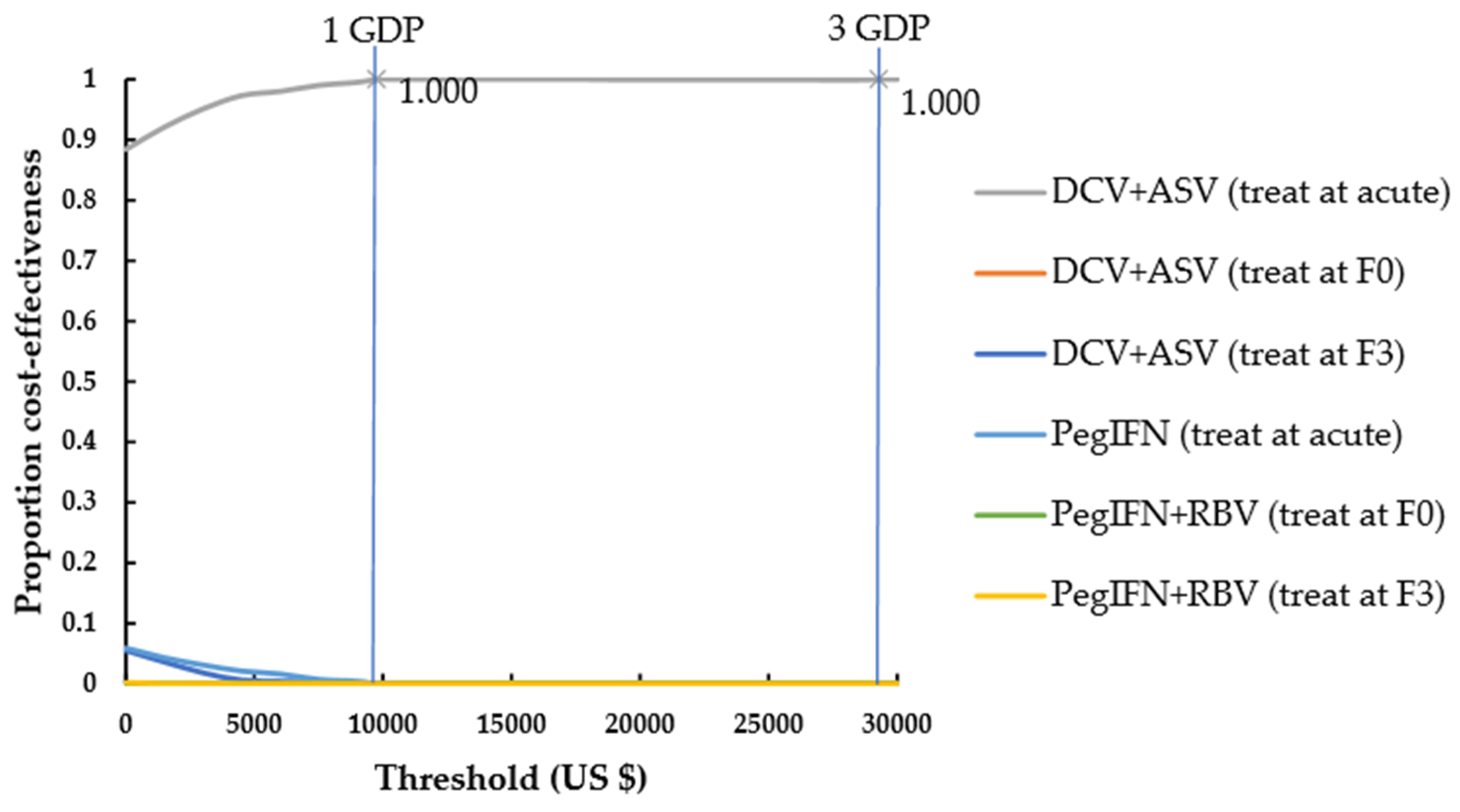
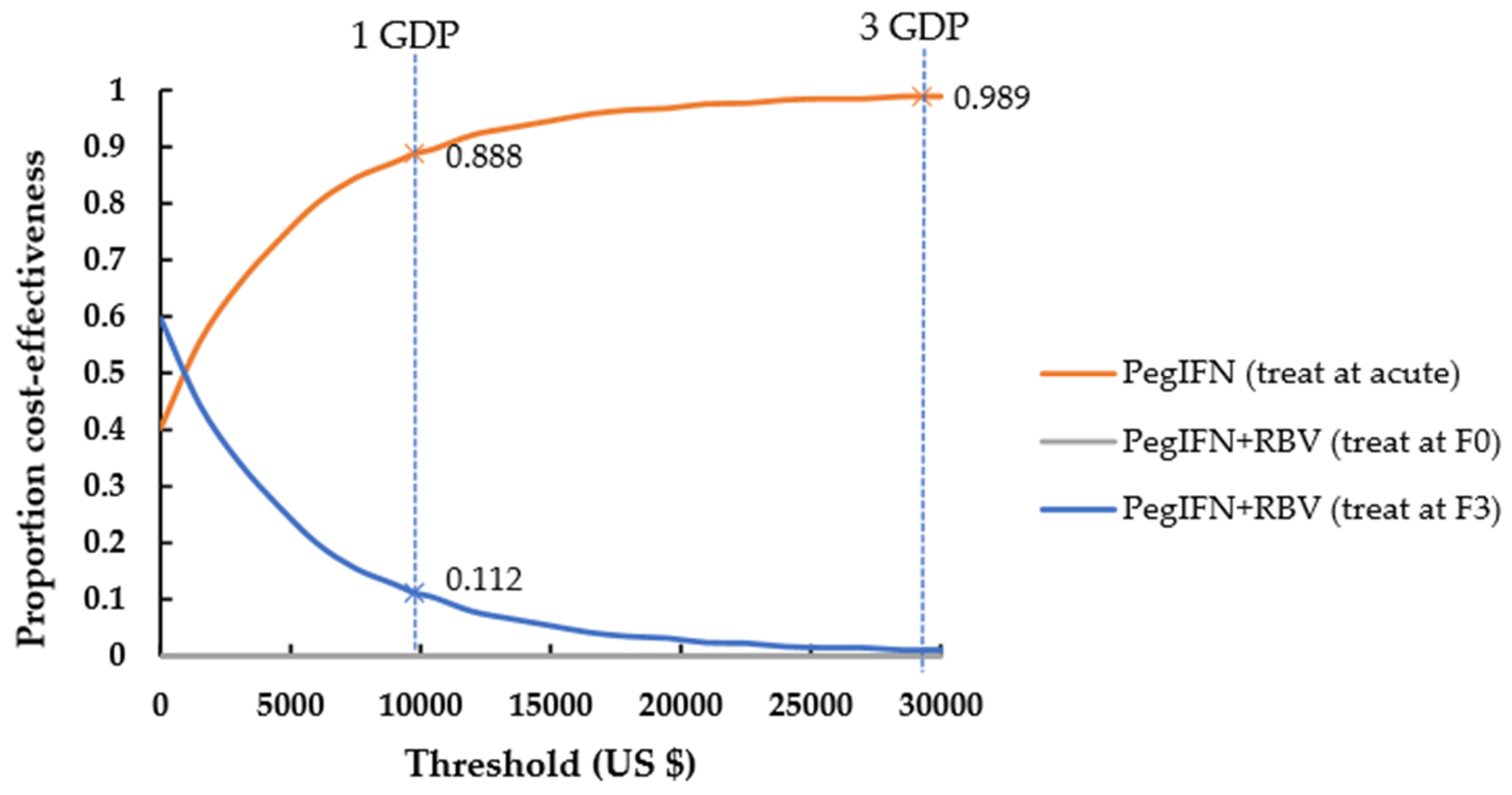
3.3. Probabilistic Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Global Hepatitis Report. 2017. Available online: https://www.who.int/hepatitis/publications/global-hepatitis-report2017/en/ (accessed on 21 April 2019).
- Su, J.; Brook, R.A.; Kleinman, N.L.; Corey-Lisle, P. The impact of hepatitis c virus infection on work absence, productivity, and healthcare benefit costs. Hepatology 2010, 52, 436–442. [Google Scholar] [CrossRef]
- Jakovljevic, M.; Jakab, M.; Gerdtham, U.; McDaid, D.; Ogura, S.; Varavikova, E.; Merrick, J.; Adany, R.; Okunade, A.; Getzen, T. Comparative financing analysis and political economy of noncommunicable diseases. J. Med. Econ. 2019, 22, 722–727. [Google Scholar] [CrossRef] [PubMed]
- Fitzmaurice, C.; Allen, C.; Barber, R.M.; Barregard, L.; Bhutta, Z.A.; Brenner, H.; Dicker, D.J.; Chimed-Orchir, O.; Dandona, R.; Dandona, L.; et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: A systematic analysis for the global burden of disease study. JAMA Oncol. 2017, 3, 524–548. [Google Scholar] [PubMed]
- Bethea, E.D.; Chen, Q.; Hur, C.; Chung, R.T.; Chhatwal, J. Should we treat acute hepatitis c? A decision and cost-effectiveness analysis. Hepatology 2018, 67, 837–846. [Google Scholar] [CrossRef] [PubMed]
- Micallef, J.M.; Kaldor, J.M.; Dore, G.J. Spontaneous viral clearance following acute hepatitis c infection: A systematic review of longitudinal studies. J. Viral Hepat. 2006, 13, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Degenhardt, L.; Peacock, A.; Colledge, S.; Leung, J.; Grebely, J.; Vickerman, P.; Stone, J.; Cunningham, E.B.; Trickey, A.; Dumchev, K.; et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of hiv, hbv, and hcv in people who inject drugs: A multistage systematic review. Lancet Glob. Health 2017, 5, e1192–e1207. [Google Scholar] [CrossRef]
- Grebely, J.; Knight, E.; Ngai, T.; Genoway, K.A.; Raffa, J.D.; Storms, M.; Gallagher, L.; Krajden, M.; Dore, G.J.; Duncan, F.; et al. Reinfection with hepatitis c virus following sustained virological response in injection drug users. J. Gastroenterol. Hepatol. 2010, 25, 1281–1284. [Google Scholar] [CrossRef]
- Degenhardt, L.; Bucello, C.; Mathers, B.; Briegleb, C.; Ali, H.; Hickman, M.; McLaren, J. Mortality among regular or dependent users of heroin and other opioids: A systematic review and meta-analysis of cohort studies. Addiction 2011, 106, 32–51. [Google Scholar] [CrossRef]
- World Health Organization. Global Health Sector Strategy on Viral Hepatitis, 2016–2021; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Pradat, P.; Virlogeux, V.; Trepo, E. Epidemiology and elimination of hcv-related liver disease. Viruses 2018, 10, 545. [Google Scholar] [CrossRef]
- Ruan, Y.; Qin, G.; Yin, L.; Chen, K.; Qian, H.Z.; Hao, C.; Liang, S.; Zhu, J.; Xing, H.; Hong, K.; et al. Incidence of hiv, hepatitis c and hepatitis b viruses among injection drug users in southwestern china: A 3-year follow-up study. AIDS 2007, 21 (Suppl. 8), S39–S46. [Google Scholar] [CrossRef]
- Jackson, J.B.; Wei, L.; Liping, F.; Aramrattana, A.; Celentano, D.D.; Walshe, L.; Xing, Y.; Richardson, P.; Jun, M.; Beauchamp, G.; et al. Prevalence and seroincidence of hepatitis b and hepatitis c infection in high risk people who inject drugs in china and thailand. Hepat. Res. Treat. 2014, 2014, 296958. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.; Hou, J.L. The guideline of prevention and treatment for hepatitis c: A 2015 update. Chin. J. Hepatol. 2015, 23, 906–923. [Google Scholar]
- China FDA Approves the Listing of Daclatasvir and Asunaprevir. Available online: http://www.nmpa.gov.cn/WS04/CL2168/329397.html (accessed on 21 April 2019).
- Duan, Z.; Jia, J.-D.; Hou, J.-L.; Lou, L.; Tobias, H.; Yuan, X.; Wei, L.; Zhuang, H.; Pan, C. Current challenges and the management of chronic hepatitis c in mainland china. J. Clin. Gastroenterol. 2014, 48, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Hullegie, S.J.; Arends, J.E.; Rijnders, B.J.; Irving, W.L.; Salmon, D.; Prins, M.; Wensing, A.M.; Klenerman, P.; Leblebicioglu, H.; Boesecke, C.; et al. Current knowledge and future perspectives on acute hepatitis c infection. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2015, 21, 797–799. [Google Scholar] [CrossRef] [PubMed]
- Cipriano, L.E.; Goldhaber-Fiebert, J.D. Population health and cost-effectiveness implications of a “treat all” recommendation for hcv: A review of the model-based evidence. MDM Policy Pract. 2018, 3. [Google Scholar] [CrossRef] [PubMed]
- Scott, N.; Iser, D.M.; Thompson, A.J.; Doyle, J.S.; Hellard, M.E. Cost-effectiveness of treating chronic hepatitis c virus with direct-acting antivirals in people who inject drugs in australia. J. Gastroenterol. Hepatol. 2016, 31, 872–882. [Google Scholar] [CrossRef]
- Visconti, A.J.; Doyle, J.S.; Weir, A.; Shiell, A.M.; Hellard, M.E. Assessing the cost-effectiveness of treating chronic hepatitis c virus in people who inject drugs in australia. J. Gastroenterol. Hepatol. 2013, 28, 707–716. [Google Scholar] [CrossRef]
- Scott, N.; McBryde, E.S.; Thompson, A.; Doyle, J.S.; Hellard, M.E. Treatment scale-up to achieve global hcv incidence and mortality elimination targets: A cost-effectiveness model. Gut 2017, 66, 1507–1515. [Google Scholar] [CrossRef]
- van Santen, D.K.; de Vos, A.S.; Matser, A.; Willemse, S.B.; Lindenburg, K.; Kretzschmar, M.E.; Prins, M.; de Wit, G.A. Cost-effectiveness of hepatitis c treatment for people who inject drugs and the impact of the type of epidemic; extrapolating from amsterdam, the netherlands. PLoS ONE 2016, 11, e0163488. [Google Scholar] [CrossRef]
- Martin, N.K.; Vickerman, P.; Dore, G.J.; Grebely, J.; Miners, A.; Cairns, J.; Foster, G.R.; Hutchinson, S.J.; Goldberg, D.J.; Martin, T.C.S.; et al. Prioritization of hcv treatment in the direct-acting antiviral era: An economic evaluation. J. Hepatol. 2016, 65, 17–25. [Google Scholar] [CrossRef]
- Bennett, H.; Gordon, J.; Jones, B.; Ward, T.; Webster, S.; Kalsekar, A.; Yuan, Y.; Brenner, M.; McEwan, P. Hepatitis c disease transmission and treatment uptake: Impact on the cost-effectiveness of new direct-acting antiviral therapies. Eur. J. Health Econ. HEPAC Health Econ. Prev. Care 2017, 18, 1001–1011. [Google Scholar] [CrossRef] [PubMed]
- Martin, N.K.; Vickerman, P.; Brew, I.F.; Williamson, J.; Miners, A.; Irving, W.L.; Saksena, S.; Hutchinson, S.J.; Mandal, S.; O’Moore, E.; et al. Is increased hepatitis c virus case-finding combined with current or 8-week to 12-week direct-acting antiviral therapy cost-effective in uk prisons? A prevention benefit analysis. Hepatology 2016, 63, 1796–1808. [Google Scholar] [CrossRef] [PubMed]
- Ruggeri, M.; Coretti, S.; Romano, F.; Kondili, L.A.; Vella, S.; Cicchetti, A. Economic evaluation of the hepatitis c virus treatment extension to early-stage fibrosis patients: Evidence from the piter real-world cohort. Value Health J. Int. Soc. Pharm. Outcomes Res. 2018, 21, 783–791. [Google Scholar] [CrossRef] [PubMed]
- Obach, D.; Deuffic-Burban, S.; Esmat, G.; Anwar, W.A.; Dewedar, S.; Canva, V.; Cousien, A.; Doss, W.; Mostafa, A.; Pol, S.; et al. Effectiveness and cost-effectiveness of immediate versus delayed treatment of hepatitis c virus–infected patients in a country with limited resources: The case of egypt. Clin. Infect. Dis. 2014, 58, 1064–1071. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Wang, Z.; Xie, Q. Cost-effectiveness of novel regimens for chinese patients with chronic hepatitis c. Curr. Med. Res. Opin. 2019, 35, 847–857. [Google Scholar] [CrossRef] [PubMed]
- Chahal, H.S.; Marseille, E.A.; Tice, J.A.; Pearson, S.D.; Ollendorf, D.A.; Fox, R.K.; Kahn, J.G. Cost-effectiveness of early treatment of hepatitis c virus genotype 1 by stage of liver fibrosis in a us treatment-naive population. JAMA Intern. Med 2016, 176, 65–73. [Google Scholar] [CrossRef]
- Smith, D.J.; Combellick, J.; Jordan, A.E.; Hagan, H. Hepatitis c virus (hcv) disease progression in people who inject drugs (pwid): A systematic review and meta-analysis. Int. J. Drug Policy 2015, 26, 911–921. [Google Scholar] [CrossRef]
- van der Meer, A.J.; Veldt, B.J.; Feld, J.J.; Wedemeyer, H.; Dufour, J.F.; Lammert, F.; Duarte-Rojo, A.; Heathcote, E.J.; Manns, M.P.; Kuske, L.; et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis c and advanced hepatic fibrosis. JAMA 2012, 308, 2584–2593. [Google Scholar] [CrossRef]
- Morgan, R.L.; Baack, B.; Smith, B.D.; Yartel, A.; Pitasi, M.; Falck-Ytter, Y. Eradication of hepatitis c virus infection and the development of hepatocellular carcinoma: A meta-analysis of observational studies. Ann. Intern. Med. 2013, 158, 329–337. [Google Scholar] [CrossRef]
- Martinello, M.; Dore, G.J.; Matthews, G.V.; Grebely, J. Strategies to reduce hepatitis c virus reinfection in people who inject drugs. Infect. Dis. Clin. N. Am. 2018, 32, 371–393. [Google Scholar] [CrossRef]
- Sacks-Davis, R.; Grebely, J.; Dore, G.J.; Osburn, W.; Cox, A.L.; Rice, T.M.; Spelman, T.; Bruneau, J.; Prins, M.; Kim, A.Y.; et al. Hepatitis c virus reinfection and spontaneous clearance of reinfection--the inc3 study. J. Infect. Dis. 2015, 212, 1407–1419. [Google Scholar] [CrossRef] [PubMed]
- China Health Statistics Yearbook. 2018. Available online: http://www.stats.gov.cn/tjsj/ndsj/2018/indexeh.htm (accessed on 21 April 2019).
- Heffernan, A.; Cooke, G.S.; Nayagam, S.; Thursz, M.; Hallett, T.B. Scaling up prevention and treatment towards the elimination of hepatitis c: A global mathematical model. Lancet 2019, 393, 1319–1329. [Google Scholar] [CrossRef]
- Fattovich, G.; Giustina, G.; Degos, F.; Tremolada, F.; Diodati, G.; Almasio, P.; Nevens, F.; Solinas, A.; Mura, D.; Brouwer, J.T.; et al. Morbidity and mortality in compensated cirrhosis type c: A retrospective follow-up study of 384 patients. Gastroenterology 1997, 112, 463–472. [Google Scholar] [CrossRef]
- He, T.; Li, K.; Roberts, M.S.; Spaulding, A.C.; Ayer, T.; Grefenstette, J.J.; Chhatwal, J. Prevention of hepatitis c by screening and treatment in U.S. Prisons. Ann. Intern. Med. 2016, 164, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Dimova, R.B.; Zeremski, M.; Jacobson, I.M.; Hagan, H.; Des Jarlais, D.C.; Talal, A.H. Determinants of hepatitis c virus treatment completion and efficacy in drug users assessed by meta-analysis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2013, 56, 806–816. [Google Scholar] [CrossRef] [PubMed]
- Boglione, L.; Mornese Pinna, S.; De Nicolo, A.; Cusato, J.; Cariti, G.; Di Perri, G.; D’Avolio, A. Treatment with direct-acting antiviral agents of hepatitis c virus infection in injecting drug users: A prospective study. J. Viral Hepat. 2017, 24, 850–857. [Google Scholar] [CrossRef]
- Grebely, J.; Dalgard, O.; Conway, B.; Cunningham, E.; Bruggmann, P.; Hajarizadeh, B.; Amin, J.; Marks, P.; Quiene, S.; Applegate, T.L.; et al. Efficacy and safety of sofosbuvir/velpatasvir in people with chronic hepatitis c virus infection and recent injecting drug use: The simplify study. J. Hepatol. 2017, 66, S513. [Google Scholar] [CrossRef]
- Lu, Y.; Jin, X.; Duan, C.A.; Chang, F. Cost-effectiveness of daclatasvir plus asunaprevir for chronic hepatitis c genotype 1b treatment-naive patients in china. Clin. Drug Investig. 2018, 13, e0195117. [Google Scholar] [CrossRef]
- People’s Republic of China 2018 National Economic and Social Development Statistical Bulletin. Available online: http://www.stats.gov.cn/tjsj/zxfb/201902/t20190228_1651265.html (accessed on 2 April 2019).
- Chen, G.F.; Wei, L.; Chen, J.; Duan, Z.P.; Dou, X.G.; Xie, Q.; Zhang, W.H.; Lu, L.G.; Fan, J.G.; Cheng, J.; et al. Will sofosbuvir/ledipasvir (harvoni) be cost-effective and affordable for chinese patients infected with hepatitis c virus? An economic analysis using real-world data. PLoS ONE 2016, 11, e0155934. [Google Scholar] [CrossRef]
- Wu, B.; Li, T.; Chen, H.; Shen, J. Cost-effectiveness of nucleoside analog therapy for hepatitis b in china: A markov analysis. Value Health J. Int. Soc. Pharm. Outcomes Res. 2010, 13, 592–600. [Google Scholar] [CrossRef]
- Liu, S.; Cipriano, L.E.; Holodniy, M.; Owens, D.K.; Goldhaber-Fiebert, J.D. New protease inhibitors for the treatment of chronic hepatitis c: A cost-effectiveness analysis. Ann. Intern. Med. 2012, 156, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Salomon, J.A.; Weinstein, M.C.; Hammitt, J.K.; Goldie, S.J. Cost-effectiveness of treatment for chronic hepatitis c infection in an evolving patient population. JAMA 2003, 290, 228–237. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Thein, H.H.; Krahn, M.; Kaldor, J.M.; Dore, G.J. Estimation of utilities for chronic hepatitis c from sf-36 scores. Am. J. Gastroenterol. 2005, 100, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Grebely, J.; Dore, G.J.; Morin, S.; Rockstroh, J.K.; Klein, M.B. Elimination of hcv as a public health concern among people who inject drugs by 2030—What will it take to get there? J. Int. AIDS Soc. 2017, 20, 22146. [Google Scholar] [CrossRef] [PubMed]
- Grebely, J.; Hajarizadeh, B.; Lazarus, J.V.; Bruneau, J.; Treloar, C. Elimination of hepatitis c virus infection among people who use drugs: Ensuring equitable access to prevention, treatment, and care for all. Int. J. Drug Policy 2019, 72, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Pedlar, A.; Sandhu, P.J. Promoting treatment for hepatitis c in people who inject drugs: A review of the barriers and opportunities. J. Am. Assoc. Nurse Pract. 2019. [Google Scholar] [CrossRef] [PubMed]
| Treatment Strategy | Total Treatment Costs/Person (US$) | QALYs/Person | Incremental Costs/Person (US$) | Incremental QALYs/Person | ICER (Incremental Costs/Incremental QALYs) |
|---|---|---|---|---|---|
| DCV+ASV-based regimen | |||||
| DCV+ASV (at F0) | $16,224.250 | 14.566 | - | - | - |
| DCV+ASV (at acute) | $14,486.975 | 14.573 | −$1737.275 | 0.007 | dominant |
| PegIFN-based regimen | |||||
| PegIFN+RBV (at F0) | $22,101.584 | 14.116 | - | - | - |
| PegIFN (at acute) | $19,734.794 | 14.148 | −2366.790 | 0.032 | dominant |
| Treatment Strategy | Total Treatment Costs/Person (US$) | QALYs/Person | Incremental Costs/Person (US$) | Incremental QALYs/Person | ICER (Incremental Costs/Incremental QALYs) |
|---|---|---|---|---|---|
| DCV+ASV-based regimen | |||||
| DCV+ASV (at F3) | $14,488.762 | 14.107 | - | - | |
| DCV+ASV (at F0) | $16,224.250 | 14.566 | $1735.488 | 0.459 | $3780.20 |
| PegIFN-based regimen | |||||
| PegIFN+RBV (at F3) | $16,876.220 | 13.771 | - | - | - |
| PegIFN+RBV (at F0) | $22,101.584 | 14.116 | $5225.364 | 0.345 | $15,145.98 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.; Zhang, H.; Zhang, L.; Zou, X.; Ling, L. Economic Evaluation of Hepatitis C Treatment Extension to Acute Infection and Early-Stage Fibrosis Among Patients Who Inject Drugs in Developing Countries: A Case of China. Int. J. Environ. Res. Public Health 2020, 17, 800. https://doi.org/10.3390/ijerph17030800
Liu Y, Zhang H, Zhang L, Zou X, Ling L. Economic Evaluation of Hepatitis C Treatment Extension to Acute Infection and Early-Stage Fibrosis Among Patients Who Inject Drugs in Developing Countries: A Case of China. International Journal of Environmental Research and Public Health. 2020; 17(3):800. https://doi.org/10.3390/ijerph17030800
Chicago/Turabian StyleLiu, Yin, Hui Zhang, Lei Zhang, Xia Zou, and Li Ling. 2020. "Economic Evaluation of Hepatitis C Treatment Extension to Acute Infection and Early-Stage Fibrosis Among Patients Who Inject Drugs in Developing Countries: A Case of China" International Journal of Environmental Research and Public Health 17, no. 3: 800. https://doi.org/10.3390/ijerph17030800
APA StyleLiu, Y., Zhang, H., Zhang, L., Zou, X., & Ling, L. (2020). Economic Evaluation of Hepatitis C Treatment Extension to Acute Infection and Early-Stage Fibrosis Among Patients Who Inject Drugs in Developing Countries: A Case of China. International Journal of Environmental Research and Public Health, 17(3), 800. https://doi.org/10.3390/ijerph17030800





