Neonatal Transport in the Practice of the Crews of the Polish Medical Air Rescue: A Retrospective Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
- NACA 0—no body injuries or illnesses;
- NACA 1—body injuries or illnesses in case of which medical care is not necessary;
- NACA 2—body injuries or illnesses that require examination and treatment, but with no need of hospitalization;
- NACA 3—body injuries or illnesses with no acute life threat but requiring hospitalization;
- NACA 4—body injuries or illnesses that may lead to deterioration of vital signs;
- NACA 5—body injuries or illnesses posing a great threat to life;
- NACA 6—body injuries or illnesses leading to sudden cardiopulmonary arrest;
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jensen, S.K.; Bouhouch, R.R.; Walson, J.L.; Daelmans, B.; Bahl, R.; Darmstadt, G.L.; Dua, T. Enhancing the child survival agenda to promote, protect, and support early child development. Semin. Perinatol. 2015, 39, 373–386. [Google Scholar] [CrossRef] [PubMed]
- Kinney, M.V.; Cocoman, O.; Dickson, K.E.; Daelmans, B.; Zaka, N.; Rhoda, N.R.; Moxon, S.G.; Kak, L.; Lawn, J.E.; Khadka, N.; et al. Implementation of Every Newborn Action Plan: Progress and lessons learned. Semin. Perinatol. 2015, 39, 326–337. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Oza, S.; Hogan, D.; Perin, J.; Rudan, I.; Lawn, J.E.; Cousens, S.; Mathers, C.; Black, R.E. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: An updated systematic analysis. Lancet 2015, 385, 430–440. [Google Scholar] [CrossRef]
- Lawn, J.E.; Blencowe, H.; Oza, S.; You, D.; Lee, A.C.; Waiswa, P.; Lalli, M.; Bhutta, Z.; Barros, A.J. Every Newborn: Progress, priorities, and potential beyond survival. Lancet 2014, 384, 189–205. [Google Scholar] [CrossRef]
- Shiffman, J. Network advocacy and the emergence of global attention to newborn survival. Health Policy Plan. 2016, 31, i60–i73. [Google Scholar] [CrossRef]
- Szamotulska, K.; Mierzejewska, E. Infant and neonatal deaths in poland in 1995–2015. Dev. Period Med. 2017, 21, 104–110. [Google Scholar]
- Statistics Poland. Demographic Yearbook of Poland. Warsaw 2019. Available online: https://stat.gov.pl/obszary-tematyczne/roczniki-statystyczne/roczniki-statystyczne/rocznik-demograficzny-2019,3,13.html (accessed on 10 December 2019).
- Troszyński, M.; Niemiec, T.; Wilczyńska, A. Assessment of three-level selective perinatal care based on the analysis of early perinatal death rates and cesarean sections in Poland in 2008. Ginekol. Pol. 2009, 80, 670–677. [Google Scholar]
- Mirończuk, J.; Hołdy, J.; Abdel-Aziz, A.; Kinalski, M. Assessment of three-level selective perinatal care based on the analysis of early perinatal death rates in Podlaskie Voivodeship hospitals in 2004–2008. Gin. Pol. Med. Project. 2010, 3, 22–29. [Google Scholar]
- Aftyka, A.; Rybojad, B. Specialised transport of neonates—Who, when, how, and why? J. Health Health Nurs. Med. Rescue 2016, 3, 15–19. [Google Scholar]
- Narli, N.; Kırımi, E.; Uslu, S. Turkish Neonatal Society guideline on the safe transport of newborn. Turk. Pediatri Ars. 2018, 25, S18–S31. [Google Scholar] [CrossRef]
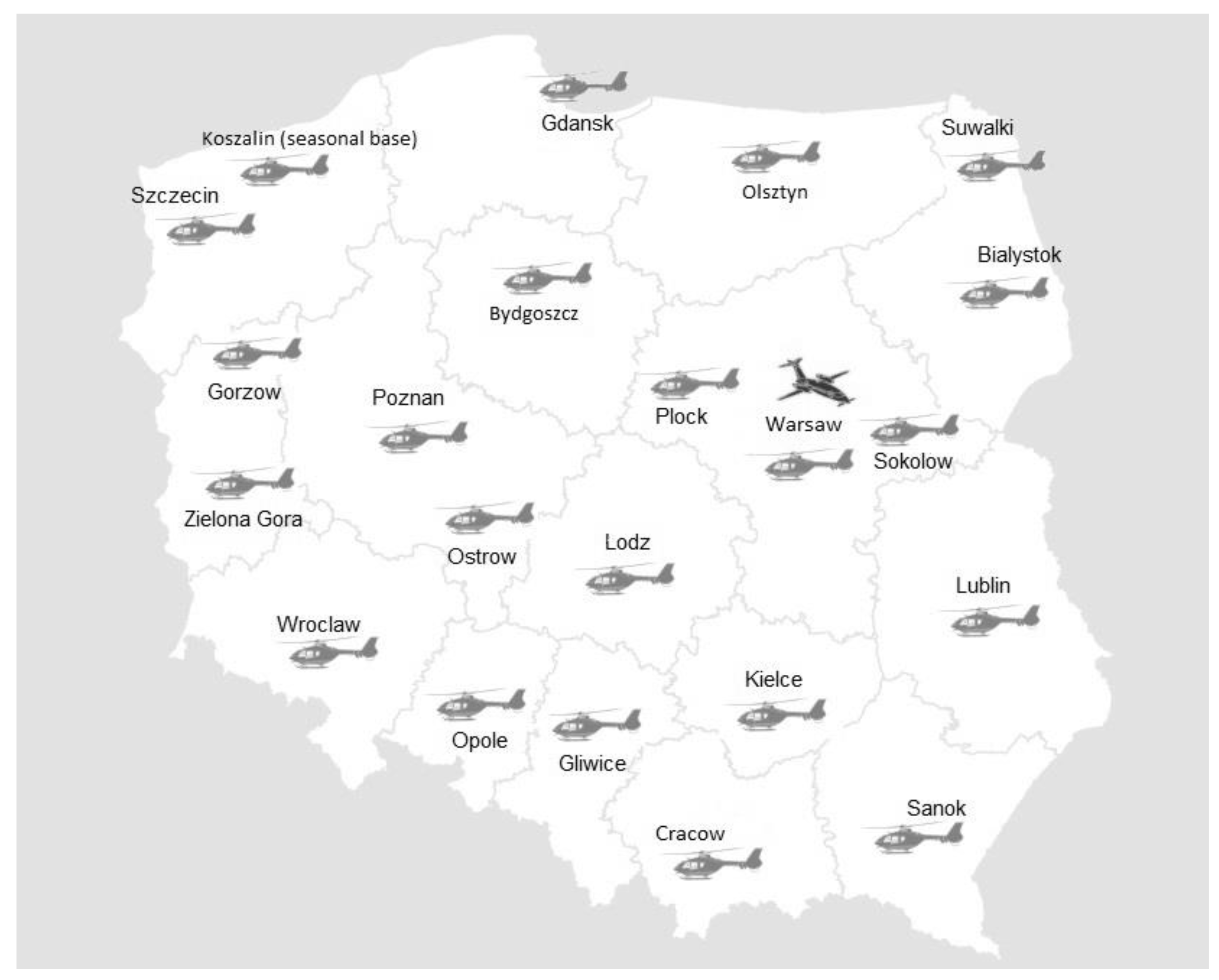
- Rzonca, P.; Galazkowski, R.; Podgorski, M. Role of Polish Medical Air Rescue in National Medical Rescue System. Disaster Emerg. Med. J. 2017, 2, 64–68. [Google Scholar] [CrossRef]
- Whyte, H.E.; Jefferies, A.L. Canadian Paediatric Society; Fetus and Newborn Committee. The interfacility transport of critically ill newborns. Paediatr Child. Health 2015, 20, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Gałazkowski, R. New possibilities in emergency medical transportation and emergency services of Polish Medical Air Rescue. Anestezjol. Intens. Ter. 2010, 42, 174–178. [Google Scholar] [PubMed]
- Raatiniemi, L.; Liisanantti, J.; Tommila, M.; Moilanen, S.; Ohtonen, P.; Martikainen, M.; Voipio, V.; Reitala, J.; Iirola, T. Evaluating helicopter emergency medical missions: A reliability study of the HEMS benefit and NACA scores. Acta Anaesthesiol. Scand. 2017, 61, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Weiss, M.; Bernoulli, L.; Zollinger, A. The NACA scale. Construct and predictive validity of the NACA scale for prehospital severity rating in trauma patients. Anaesthesist 2001, 50, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.Y.; Liu, X.X.; Hong, X.Y.; Liu, J.; Li, Q.P.; Feng, Z.C. Improved outcomes of transported neonates in Beijing: The impact of strategic changes in perinatal and regional neonatal transport network services. World J. Pediatr. 2014, 10, 251–255. [Google Scholar] [CrossRef]
- Bouchut, J.C.; Van Lancker, E.; Chritin, V.; Gueugniaud, P.Y. Physical stressors during neonatal transport: Helicopter compared with ground ambulance. Air Med. J. 2011, 30, 134–139. [Google Scholar] [CrossRef]
- Quinn, J.M.; Pierce, M.C.; Adler, M. Factors associated with mode of transport decision making for pediatric-neonatal interfacility transport. Air Med. J. 2015, 34, 44–51. [Google Scholar] [CrossRef]
- Moss, S.J.; Embleton, N.D.; Fenton, A.C. Towards safer neonatal transfer: The importance of critical incident review. Arch. Dis. Child. 2005, 90, 729–732. [Google Scholar] [CrossRef]
- Henry, S.; Trotman, H. Challenges in neonatal transport in Jamaica: A resource-limited setting. J. Trop. Pediatr. 2017, 63, 307–313. [Google Scholar] [CrossRef]
- Frid, I.; Ågren, J.; Kjellberg, M.; Normann, E.; Sindelar, R. Critically ill neonates displayed stable vital parameters and reduced metabolic acidosis during neonatal emergency airborne transport in Sweden. Acta Paediatr. 2018, 7, 1357–1361. [Google Scholar] [CrossRef] [PubMed]
- Kempley, S.T.; Sinha, A.K. Thames Regional Perinatal Group. Census of neonatal transfers in London and the South East of England. Arch. Dis. Child. Fetal. Neonatal. Ed. 2004, 89, F521–F526. [Google Scholar] [CrossRef] [PubMed]
- Yan Leung, K.K.; Lee, S.L.; Wong, M.S.R.; Wong, W.H.; Yung, T.C. Clinical outcomes of critically ill infants requiring interhospital transport to a paediatric tertiary centre in Hong Kong. Pediatr. Respirol. Crit. Care Med. 2019, 3, 28–35. [Google Scholar] [CrossRef]
- Purisch, S.E.; Gyamfi-Bannerman, C. Epidemiology of preterm birth. Semin. Perinatol. 2017, 41, 387–391. [Google Scholar] [CrossRef]
- Frey, H.A.; Klebanoff, M.A. The epidemiology, etiology, and costs of preterm birth. Semin. Fetal. Neonatal. Med. 2016, 21, 68–73. [Google Scholar] [CrossRef]
- Platt, M.J. Outcomes in preterm infants. Public Health 2014, 128, 399–403. [Google Scholar] [CrossRef]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Egbe, A.; Uppu, S.; Lee, S.; Stroustrup, A.; Ho, D.; Srivastava, S. Congenital malformations in the newborn population: A population study and analysis of the effect of sex and prematurity. Pediatr. Neonatol. 2015, 56, 25–30. [Google Scholar] [CrossRef]
- Dursun, A.; Zenciroglu, A.; Hakan, N.; Karadag, N.; Karagol, B.S.; Aydin, B.; Dilli, D.; Okumus, N.; Beken, S.J. Distribution of congenital anomalies in a neonatal intensive care unit in Turkey. Matern. Fetal Neonatal Med. 2014, 27, 1069–1074. [Google Scholar] [CrossRef]
- Bastug, O.; Gunes, T.; Korkmaz, L.; Elmali, F.; Kucuk, F.; Adnan Ozturk, M.; Kurtoglu, S. An evaluation of intra-hospital transport outcomes from tertiary neonatal intensive care unit. J. Matern. Fetal Neonatal Med. 2016, 29, 1993–1998. [Google Scholar] [CrossRef]
- Xu, X.J.; Li, L.N.; Wu, W.Y. Importance of stabilization of the neonatal transport network in critically ill neonates. J. Int. Med. Res. 2019, 47, 3737–3744. [Google Scholar] [CrossRef] [PubMed]
- McAdams, R.M.; Dotzler, S.A.; Pole, G.L.; Kerecman, J.D. Long-distance air medical transport of extremely low birth weight infants with pneumoperitoneum. J. Perinatol. 2008, 28, 330–334. [Google Scholar] [CrossRef] [PubMed]
- Berge, S.D.; Berg-Utby, C.; Skogvoll, E. Helicopter transport of sick neonates: A 14-year population-based study. Acta Anaesthesiol. Scand. 2005, 49, 999–1003. [Google Scholar] [CrossRef] [PubMed]
- Lang, A.; Brun, H.; Kaaresen, P.I.; Klingenberg, C. A population based 10-year study of neonatal air transport in North Norway. Acta Paediatr. 2007, 96, 995–999. [Google Scholar] [CrossRef] [PubMed]
- Orr, R.A.; Felmet, K.A.; Han, Y.; McCloskey, K.A.; Dragotta, M.A.; Bills, D.M.; Kuch, B.A.; Watson, R.S. Pediatric specialized transport teams are associated with improved outcomes. Pediatrics 2009, 124, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Hamrin, T.H.; Berner, J.; Eksborg, S.; Radell, P.J.; Fläring, U. Characteristics and outcomes of critically ill children following emergency transport by a specialist paediatric transport team. Acta Paediatr. 2016, 105, 1329–1334. [Google Scholar] [CrossRef] [PubMed]
- Abdulraheem, M.A.; Tongo, O.O.; Orimadegun, A.E.; Akinbami, O.F. Neonatal transport practices in Ibadan, Nigeria. Pan Afr. Med. J. 2016, 24, 216. [Google Scholar] [CrossRef]
- Duritza, K. Neonatal Transport—A Family Support Module. Newborn Infant Nurs. Rev. 2009, 9, 212–218. [Google Scholar] [CrossRef]
- Joyce, C.N.; Libertin, R.; Bigham, M.T. Family-centered care in pediatric critical care transport. Air Med. J. 2015, 34, 32–36. [Google Scholar] [CrossRef]
- Gałązkowski, R.; Świeżewski, S.P.; Rabczenko, D.; Wejnarski, A.; Timler, D.; Michalak, G.; Kotela, I. Rescue procedures in the major trauma of upper extremities—The role of the polish medical air rescue in the therapeutic process. Med. Pr. 2014, 65, 765–776. [Google Scholar] [CrossRef]
- Wejnarski, A.; Leszczyński, P.; Świeżewski, S.; Podgórski, M.; Farkowski, M.M.; Sterliński, M.; Panczyk, M.; Gotlib, J.; Rabczenko, D.; Gałązkowski, R. Characteristics of aeromedical transport, both inter-hospital and directly from the scene of the incident, in patients with acute myocardial infarction or acute trauma between 2011–2016 in Poland: A case-control study. Adv. Clin. Exp. Med. 2019, 28, 1495–1505. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total | Classification of Patient Based on the Date of Delivery | p-Value | |
|---|---|---|---|---|
| Preterm Infant | Full-Term Newborn | |||
| Sex—n (%) | ||||
| Female | 196 (44.95) | 93 (47.45) | 103 (52.55) | 0.4403 |
| Male | 240 (55.05) | 105 (43.75) | 135 (56.25) | |
| Patient classification based on the date of delivery—n (%) | ||||
| Preterm infant | 198 (45.41) | - | - | - |
| Full-term newborn | 238 (54.59) | - | - | |
| Age during transport (days)—M (SD) | 37.53 (43.53) | 50.40 (44.49) | 26.82 (39.73) | 0.0000 |
| Body weight during transport (g)—M (SD) | 3121.18 (802.64) | 2609.07 (702.68) | 3547.24 (608.78) | 0.0000 |
| Diagnosis based on ICD classification 10—n (%) | ||||
| Congenital heart malformations | 180 (41.28) | 68 (34.34) | 112 (47.06) | 0.0270 |
| Congenital malformations of the circulatory system | 85 (19.50) | 43 (21.72) | 42 (17.65) | |
| Congenital malformations of the gastrointestinal system | 60 (13.76) | 34 (17.17) | 26 (10.92) | |
| Respiratory disorders originating in the perinatal period | 41 (9.40) | 21 (10.61) | 20 (8.40) | |
| Congenital malformations of the nervous system | 18 (4.13) | 12 (6.06) | 6 (2.52) | |
| Congenital malformations affecting multiple systems | 15 (3.44) | 4 (2.02) | 11 (4.62) | |
| Other diagnoses | 37 (8.49) | 16 (8.08) | 21 (8.82) | |
| State of consciousness—n (%) | ||||
| Conscious | 319 (73.17) | 142 (71.82) | 177 (74.37) | 0.5337 |
| Sedation | 117 (26.83) | 56 (28.28) | 61 (25.63) | |
| Skin coloring—n (%) | ||||
| Normal | 353 (80.96) | 164 (82.83) | 189 (79.41) | 0.3415 |
| Pale | 40 (9.17) | 19 (9.60) | 21 (8.82) | |
| Yellowish | 43 (9.86) | 15 (7.58) | 28 (11.76) | |
| Cyanosis—n (%) | ||||
| Yes | 44 (10.09) | 23 (11.62) | 21 (8.82) | 0.3351 |
| No | 392 (89.91) | 175 (88.38) | 217 (91.18) | |
| Respiratory effort—n (%) | ||||
| Present | 52 (11.93) | 23 (11.62) | 29 (12.18) | 0.6889 |
| No | 341 (78.21) | 158 (79.80) | 183 (76.89) | |
| Apnea | 43 (9.86) | 17 (8.59) | 26 (10.92) | |
| Breath count (breaths per minute)—M (SD) | 36.36 (16.95) | 36.26 (16.03) | 36.44 (17.71) | 0.7738 |
| Saturation (%)—M (SD) | 93.55 (6.49) | 93.99 (6.36) | 93.18 (6.59) | 0.1296 |
| Heart rate (beats per minute)—M (SD) | 141.86 (17.27) | 141.18 (16.94) | 142.44 (17.55) | 0.9016 |
| Systolic pressure (mmHg)—M (SD) | 76.60 (14.56) | 75.36 (13.33) | 77.63 (15.46) | 0.2056 |
| Diastolic pressure (mmHg)—M (SD) | 45.23 (10.62) | 44.46 (9.58) | 45.87 (11.39) | 0.3549 |
| NACA—M (SD) | 3.66 (0.80) | 3.57 (0.80) | 3.74 (0.79) | 0.0228 |
| * Medical Emergency Procedures—n (%) | ||||
| Oxygen therapy | 65 (14.91) | 35 (17.68) | 30 (12.61) | 0.1388 |
| Mechanical ventilation—respirator | 75 (17.20) | 34 (17.17) | 41 (17.23) | 0.9879 |
| Intubation | 119 (27.29) | 55 (27.78) | 64 (26.89) | 0.8360 |
| ** Medications during transport—n (%) | ||||
| Antibiotics | 131 (30.05) | 55 (27.78) | 76 (31.93) | 0.3461 |
| Prostaglandin E1 | 144 (33.03) | 41 (20.71) | 103 (43.28) | 0.0000 |
| Glucose | 192 (44.04) | 99 (50 00) | 93 (39.08) | 0.0222 |
| Furosemide | 63 (14.45) | 20 (10.10) | 43 (18.07) | 0.0185 |
| Vitamins | 78 (17.89) | 50 (25.25) | 28 (11.76) | 0.0003 |
| Parenteral nutrition | 60 (13.76) | 31 (15.66) | 29 (12.18) | 0.2948 |
| Type of Aircraft—n (%) | |
| Helicopter | 67 (15.37) |
| Airplane | 369 (84.63) |
| Type of mission—n (%) | |
| Rescue transport | 90 (20.64) |
| Medical transport | 346 (79.36) |
| Season of the year—n (%) | |
| Spring | 126 (28.90) |
| Summer | 110 (25.23) |
| Autumn | 103 (23.62) |
| Winter | 97 (22.25) |
| Days of transport—n (%) | |
| Weekdays | 381 (87.39) |
| Weekend | 55 (12.61) |
| Referral level of target hospital—n (%) | |
| II level | 95 (21.79) |
| III level | 341 (78.21) |
| Accompanying person during transport—n (%) | |
| Parent | 186 (42.66) |
| No accompanying person | 250 (57.34) |
| Time of transport (min)—M (SD) | 49.92 (27.70) |
| Time from taking care of patient to patient transfer to target hospital (min)—M (SD) | 86.29 (33.57) |
| Time from receipt of call to patient transfer (min)—M (SD) | 269.16 (118.55) |
| Distance (km)—M (SD) | 304.27 (93.05) |
| Variable | Classification of Patients Based on due Date | p-Value | |
|---|---|---|---|
| Preterm Infant | Full-Term Newborn | ||
| Type of mission—n (%) | |||
| Rescue transport | 29 (14.65) | 61 (25.63) | 0.0048 |
| Medical transport | 169 (85.35) | 177 (74.37) | |
| Referral level of target hospital—n (%) | |||
| II level | 40 (20.20) | 55 (23.11) | 0.4641 |
| III level | 158 (79.80) | 183 (76.89) | |
| Accompanying person during transport—n (%) | |||
| Parent | 72 (36.36) | 114 (47.90) | 0.0153 |
| No accompanying person | 126 (63.64) | 121 (50.84) | |
| Time of transport—M (SD) | 51.07 (27.87) | 48.97 (27.59) | 0.1950 |
| Time of taking care of patient—M (SD) | 86.10 (31.69) | 86.45 (35.12) | 0.2660 |
| Time from receipt of call to patient transfer—M (SD) | 258.58 (108.74) | 278.07 (125.77) | 0.1231 |
| Distance—M (SD) | 306.40 (94.18) | 302.51 (92.28) | 0.8150 |
| Diagnosis—n (%) | Classification of Patient Based on the Date of Delivery | Sex | ||||||
|---|---|---|---|---|---|---|---|---|
| Preterm Infant | Full-Term Newborn | Odds Ratio (OR) | 95% CI | Female | Male | OR | 95% CI | |
| Congenital heart malformations | 68 (34.34) | 112 (47.06) | 0.59 | 0.40–0.87 | 80 (40.82) | 100 (41.67) | 0.97 | 0.66–1.42 |
| Congenital malformations of the circulatory system | 43 (21.72) | 42 (17.65) | 1.30 | 0.81–2.08 | 35 (17.86) | 50 (20.83) | 0.83 | 0.51–1.34 |
| Congenital malformations of the gastrointestinal system | 34 (17.17) | 26 (10.92) | 1.70 | 0.98–2.93 | 29 (14.80) | 31 (12.92) | 1.17 | 0.68–2.02 |
| Respiratory disorders originating in the perinatal period | 21 (10.61) | 20 (8.40) | 1.29 | 0.68–2.46 | 18 (9.18) | 23 (9.58) | 0.95 | 0.50–1.82 |
| Congenital malformations of the nervous system | 12 (6.06) | 6 (2.52) | 2.50 | 0.92–6.77 | 8 (4.08) | 10 (4.17) | 0.98 | 0.38–2.53 |
| Congenital malformations affecting multiple systems | 4 (2.02) | 11 (4.62) | 0.43 | 0.13–1.36 | 7 (3.57) | 8 (4.17) | 1.07 | 0.38–3.02 |
| Other diagnoses | 16 (8.08) | 21 (8.82) | 0.91 | 0.46–1.79 | 19 (9.69) | 18 (7.50) | 1.32 | 0.67–2.60 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rzońca, E.; Świeżewski, S.P.; Gałązkowski, R.; Bień, A.; Kosowski, A.; Leszczyński, P.; Rzońca, P. Neonatal Transport in the Practice of the Crews of the Polish Medical Air Rescue: A Retrospective Analysis. Int. J. Environ. Res. Public Health 2020, 17, 705. https://doi.org/10.3390/ijerph17030705
Rzońca E, Świeżewski SP, Gałązkowski R, Bień A, Kosowski A, Leszczyński P, Rzońca P. Neonatal Transport in the Practice of the Crews of the Polish Medical Air Rescue: A Retrospective Analysis. International Journal of Environmental Research and Public Health. 2020; 17(3):705. https://doi.org/10.3390/ijerph17030705
Chicago/Turabian StyleRzońca, Ewa, Stanisław Paweł Świeżewski, Robert Gałązkowski, Agnieszka Bień, Arkadiusz Kosowski, Piotr Leszczyński, and Patryk Rzońca. 2020. "Neonatal Transport in the Practice of the Crews of the Polish Medical Air Rescue: A Retrospective Analysis" International Journal of Environmental Research and Public Health 17, no. 3: 705. https://doi.org/10.3390/ijerph17030705
APA StyleRzońca, E., Świeżewski, S. P., Gałązkowski, R., Bień, A., Kosowski, A., Leszczyński, P., & Rzońca, P. (2020). Neonatal Transport in the Practice of the Crews of the Polish Medical Air Rescue: A Retrospective Analysis. International Journal of Environmental Research and Public Health, 17(3), 705. https://doi.org/10.3390/ijerph17030705









