Long-Term Benefits of Tailored Exercise in Severe Sarcoidosis: A Case Report
Abstract
1. Introduction
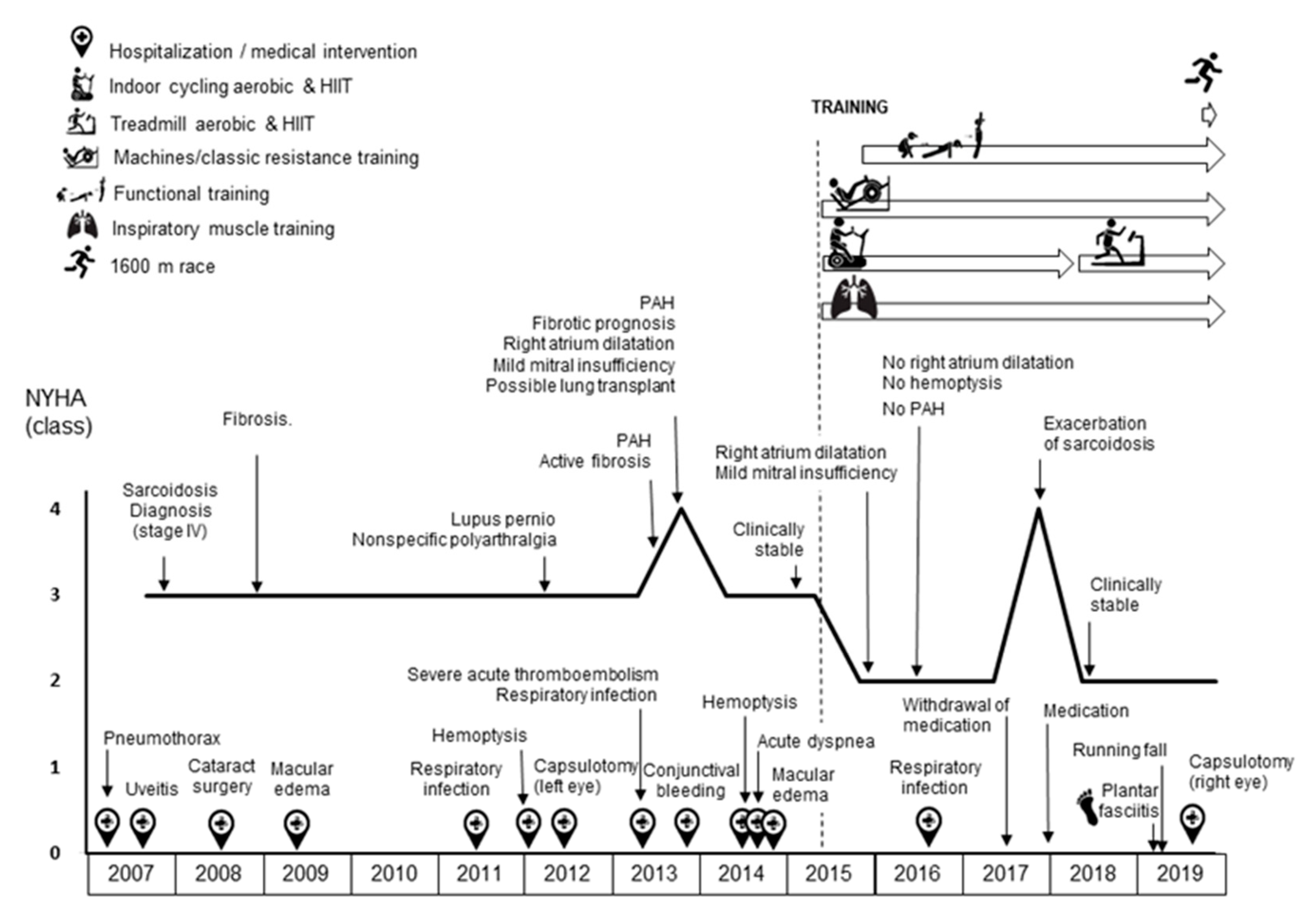
2. Experimental Section (Case Report)
2.1. Assessments
2.2. Exercise Training Intervention
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Arkema, E.V.; Cozier, Y.C. Epidemiology of sarcoidosis: Current findings and future directions. Ther. Adv. Chronic Dis. 2018, 9, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Tavana, S.; Alizadeh, M.; Mohajerani, S.; Hashemian, S. Pulmonary and extra-pulmonary manifestations of sarcoidosis. Niger. Med. J. 2015, 56, 258. [Google Scholar] [CrossRef] [PubMed]
- Voortman, M.; Hendriks, C.M.R.; Elfferich, M.D.P.; Bonella, F.; Møller, J.; de Vries, J.; Costabel, U.; Drent, M. The burden of sarcoidosis symptoms from a patient perspective. Lung 2019, 197, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Judson, M.A. The clinical features of sarcoidosis: A comprehensive review. Clin. Rev. Allergy Immunol. 2015, 49, 63–78. [Google Scholar] [CrossRef] [PubMed]
- Boucly, A.; Cottin, V.; Nunes, H.; Jaïs, X.; Tazi, A.; Prévôt, G.; Reynaud-Gaubert, M.; Dromer, C.; Viacroze, C.; Horeau-Langlard, D.; et al. Management and long-term outcomes of sarcoidosis-associated pulmonary hypertension. Eur. Respir. J. 2017, 50. [Google Scholar] [CrossRef]
- Moor, C.C.; Gür-Demirel, Y.; Wijsenbeek, M.S. Feasibility of a comprehensive home monitoring program for sarcoidosis. J. Personal. Med. 2019, 9, 23. [Google Scholar] [CrossRef]
- Cho, P.S.P.; Vasudevan, S.; Maddocks, M.; Spinou, A.; Mitchell, S.C.; Wood, C.; Jolley, C.J.; Birring, S.S. Physical inactivity in pulmonary sarcoidosis. Lung 2019, 197, 285–293. [Google Scholar] [CrossRef]
- Froidure, S.; Kyheng, M.; Grosbois, J.M.; Lhuissier, F.; Stelianides, S.; Wemeau, L.; Wallaert, B. Daily life physical activity in patients with chronic stage IV sarcoidosis: A multicenter cohort study. Health Sci. Rep. 2019, 2, e109. [Google Scholar] [CrossRef]
- Bahmer, T.; Watz, H.; Develaska, M.; Waschki, B.; Rabe, K.F.; Magnussen, H.; Kirsten, D.; Kirsten, A.-M. Physical activity and fatigue in patients with sarcoidosis. Respiration 2018, 95, 18–26. [Google Scholar] [CrossRef]
- Strookappe, B.; Saketkoo, L.A.; Elfferich, M.; Holland, A.; de Vries, J.; Knevel, T.; Drent, M. Physical activity and training in sarcoidosis: Review and experience-based recommendations. Expert Rev. Respir. Med. 2016, 10, 1057–1068. [Google Scholar] [CrossRef]
- Strookappe, B.; Elfferich, M.; Swigris, J.; Verschoof, A.; Veschakelen, J.; Knevel, T.; Drent, M. Benefits of physical training in patients with idiopathic or end-stage sarcoidosis-related pulmonary fibrosis: A pilot study. Sarcoidosis Vasc. Diffuse Lung Dis. 2015, 32, 43–52. [Google Scholar] [PubMed]
- Marcellis, R.; van der Veeke, M.; Mesters, I.; Drent, M.; de Bie, R.; de Vries, G.; Lenssen, A. Does physical training reduce fatigue in sarcoidosis? Sarcoidosis Vasc. Diffuse Lung Dis. 2015, 32, 53–62. [Google Scholar] [PubMed]
- Kullberg, S.; Rivera, N.; Eriksson, M.J.; Grunewald, J.; Eklund, A. High-intensity resistance training in newly diagnosed sarcoidosis- an exploratory study of effects on lung function, muscle strength, fatigue, dyspnea, health-related quality of life and lung immune cells. Eur. Clin. Respir. J. 2020, 7, 1730137. [Google Scholar] [CrossRef] [PubMed]
- Strookappe, B.; Swigris, J.; de Vries, J.; Elfferich, M.; Knevel, T.; Drent, M. Benefits of physical training in sarcoidosis. Lung 2015, 193, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Naz, I.; Ozalevli, S.; Ozkan, S.; Sahin, H. Efficacy of a structured exercise program for improving functional capacity and quality of life in patients with stage 3 and 4 sarcoidosis: A randomized controlled trial. J. Cardiopulm. Rehabil. Prev. 2018, 38, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Gibala, M.J.; Little, J.P.; Macdonald, M.J.; Hawley, J.A. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J. Physiol. 2012, 590, 1077–1084. [Google Scholar] [CrossRef] [PubMed]
- Grongstad, A.; Vøllestad, N.; Oldervoll, L.; Spruit, M.; Edvardsen, A. The effects of high- versus moderate-intensity exercise on fatigue in sarcoidosis. J. Clin. Med. 2019, 8, 460. [Google Scholar] [CrossRef]
- Gangemi, A.; Myers, C.N.; Zheng, M.; Brown, J.; Butler-Lebair, M.; Cordova, F.; Marchetti, N.; Criner, G.J.; Gupta, R.; Mamary, A.J. Mortality for sarcoidosis patients on the transplant wait list in the Lung Allocation Score era: Experience from a high volume center. Respir. Med. 2019, 157, 69–76. [Google Scholar] [CrossRef]
- Marcellis, R.G.J.; Lenssen, A.F.; de Vries, J.; Drent, M. Reduced muscle strength, exercise intolerance and disabling symptoms in sarcoidosis. Curr. Opin. Pulm. Med. 2013, 19, 524–530. [Google Scholar] [CrossRef]
- Brancaleone, P.; Perez, T.; Robin, S.; Neviere, R.; Wallaert, B. Clinical impact of inspiratory muscle impairment in sarcoidosis. Sarcoidosis Vasc. Diffuse Lung Dis. 2004, 21, 219–227. [Google Scholar]
- Hunninghake, G.W.; Costabel, U.; Ando, M.; Baughman, R.; Cordier, J.F.; Bois, R.; Eklund, A.; Kitaichi, M.; Lynch, J.; Rizzto, G.; et al. Statement on sarcoidosis. Am. J. Respir. Crit. Care Med. 1999, 160, 736–755. [Google Scholar] [CrossRef]
- González-Saiz, L.; Fiuza-Luces, C.; Sanchis-Gomar, F.; Santos-Lozano, A.; Quezada-Loaiza, C.A.; Flox-Camacho, A.; Munguía-Izquierdo, D.; Ara, I.; Santalla, A.; Morán, M.; et al. Benefits of skeletal-muscle exercise training in pulmonary arterial hypertension: The WHOLEi + 12 trial. Int. J. Cardiol. 2017, 231, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Zach, M.S. The physiology of forced expiration. Paediatr. Respir. Rev. 2000, 1, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Lopes, A.J.; Menezes, S.L.S.; Dias, C.M.; Oliveira, J.F.; Mainenti, M.R.M.; Guimarães, F.S. Cardiopulmonary exercise testing variables as predictors of long-term outcome in thoracic sarcoidosis. Braz. J. Med. Biol. Res. 2012, 45, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Lucía, A.; Hoyos, J.; Chicharro, J.L. Preferred pedalling cadence in professional cycling. Med. Sci. Sports Exerc. 2001, 33, 1361–1366. [Google Scholar] [CrossRef]
- Rodríguez-Gómez, I.; Santalla, A.; Díez-Bermejo, J.; Munguía-Izquierdo, D.; Alegre, L.M.; Nogales-Gadea, G.; Arenas, J.; Martín, M.A.; Lucia, A.; Ara, I. A new condition in McArdle disease: Poor bone HealthBenefits of an active lifestyle. Med. Sci. Sports Exerc. 2018, 50, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.A.; Brooke-Wavell, K. Optimum frequency of exercise for bone health: Randomised controlled trial of a high-impact unilateral intervention. Bone 2010, 46, 1043–1049. [Google Scholar] [CrossRef]
- Kemmler, W.; Kohl, M.; von Stengel, S. Long-term effects of exercise in postmenopausal women: 16-year results of the Erlangen Fitness and Osteoporosis Prevention Study (EFOPS). Menopause 2017, 24, 45–51. [Google Scholar] [CrossRef]
- Lagally, K.M.; Robertson, R.J. Construct validity of the OMNI resistance exercise scale. J. Strength Cond. Res. 2006, 20, 252–256. [Google Scholar] [CrossRef]
- Schoenfeld, B.J.; Grgic, J.; Ogborn, D.; Krieger, J.W. Strength and hypertrophy adaptations between low- vs. High-load resistance training: A systematic review and meta-analysis. J. Strength Cond. Res. 2017, 31, 3508–3523. [Google Scholar] [CrossRef]
- Nunes, P.R.; Barcelos, L.C.; Oliveira, A.A.; Furlanetto, R.; Martins, F.M.; Resende, E.A.; Orsatti, F.L.; Júnior, R.F. Muscular strength adaptations and hormonal responses after two different multiple-set protocols of resistance training in postmenopausal women. J. Strength Cond. Res. 2019, 33, 1276–1285. [Google Scholar] [CrossRef] [PubMed]
- Valenzuela, P.L.; Maffiuletti, N.A.; Joyner, M.J.; Lucia, A.; Lepers, R. Lifelong endurance exercise as a countermeasure against age-related V˙ O 2 max decline: Physiological overview and insights from masters athletes. Sports Med. 2020, 50, 703–716. [Google Scholar] [CrossRef] [PubMed]
- Ozemek, C.; Laddu, D.R.; Lavie, C.J.; Claeys, H.; Kaminsky, L.A.; Ross, R.; Wisloff, U.; Arena, R.; Blair, S.N. An update on the role of cardiorespiratory fitness, structured exercise and lifestyle physical activity in preventing cardiovascular disease and health risk. Prog. Cardiovasc. Dis. 2018, 61, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Barnes, J.N.; Joyner, M.J. Physical activity and cardiovascular risk: 10 metabolic equivalents or bust. Mayo Clin. Proc. 2013, 88, 1353–1355. [Google Scholar] [CrossRef] [PubMed]
- Layton, A.M.; Armstrong, H.F.; Baldwin, M.R.; Podolanczuk, A.J.; Pieszchata, N.M.; Singer, J.P.; Arcasoy, S.M.; Meza, K.S.; D’Ovidio, F.; Lederer, D.J. Frailty and maximal exercise capacity in adult lung transplant candidates. Respir. Med. 2017, 131, 70–76. [Google Scholar] [CrossRef] [PubMed]
- MacInnis, M.J.; Gibala, M.J. Physiological adaptations to interval training and the role of exercise intensity. J. Physiol. 2017, 595, 2915–2930. [Google Scholar] [CrossRef]
- Bloor, C.M. Angiogenesis during exercise and training. Angiogenesis 2005, 8, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Habedank, D.; Reindl, I.; Vietzke, G.; Bauer, U.; Sperfeld, A.; Wernecke, K.D.; Kleber, F.X. Ventilatory efficiency and exercise tolerance in 101 healthy volunteers. Eur. J. Appl. Physiol. Occup. Physiol. 1998, 77, 421–426. [Google Scholar] [CrossRef]
- Karadall, M.N.; Boşnak-Güçlü, M.; Camcıoğlu, B.; Kokturk, N.; Tüktaş, H. Effects of inspiratory muscle training in subjects with sarcoidosis: A randomized controlled clinical trial. Respir. Care 2016, 61, 483–494. [Google Scholar] [CrossRef]
- Souza, H.; Rocha, T.; Pessoa, M.; Rattes, C.; Brandão, D.; Fregonezi, G.; Campos, S.; Aliverti, A.; Dornelas, A. Effects of inspiratory muscle training in elderly women on respiratory muscle strength, diaphragm thickness and mobility. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 1545–1553. [Google Scholar] [CrossRef]
- Shei, R.J.; Paris, H.L.R.; Wilhite, D.P.; Chapman, R.F.; Mickleborough, T.D. The role of inspiratory muscle training in the management of asthma and exercise-induced bronchoconstriction. Phys. Sportsmed. 2016, 44, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, J.A.; Romer, L.; Rodman, J.; Miller, J.; Smith, C. Consequences of exercise-induced respiratory muscle work. Respir. Physiol. Neurobiol. 2006, 151, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Hoff, J.; Gran, A.; Helgerud, J. Maximal strength training improves aerobic endurance performance. Scand. J. Med. Sci. Sports 2002, 12, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Heggelund, J.; Fimland, M.S.; Helgerud, J.; Hoff, J. Maximal strength training improves work economy, rate of force development and maximal strength more than conventional strength training. Eur. J. Appl. Physiol. 2013, 113, 1565–1573. [Google Scholar] [CrossRef] [PubMed]
- Ono, Y.; Miyakoshi, N.; Kasukawa, Y.; Akagawa, M.; Kimura, R.; Nagahata, I.; Yuasa, Y.; Sato, C.; Shimada, Y. Diagnosis of presarcopenia using body height and arm span for postmenopausal osteoporosis. Clin. Interv. Aging. 2020, 15, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Stanbury, R.M.; Graham, E.M. Systemic corticosteroid therapy side effects and their management. Br. J. Ophthalmol. 1998, 82, 704–708. [Google Scholar] [CrossRef]
- Owczarek, J.; Jasińska, M.; Orszulak-Michalak, D. Drug-induced myopathies. An overview of the possible mechanisms. Pharmacol. Rep. 2005, 57, 23–34. [Google Scholar]
- Kamen, G. Aging, resistance training, and motor unit discharge behavior. Can. J. Appl. Physiol. 2005, 30, 341–351. [Google Scholar] [CrossRef]
- Jenkins, N.D.; Miramonti, A.A.; Hill, E.C.; Smith, C.M.; Cochrane-Snyman, K.C.; Housh, T.J.; Cramer, J.T. Greater neural adaptations following high- vs. low-load resistance training. Front. Physiol. 2017, 8, 331. [Google Scholar] [CrossRef]
- Sipilä, S.; Törmäkangas, T.; Sillanpää, E.; Aukee, P.; Kujala, U.M.; Kovanen, V.; Laakkonen, E.K. Muscle and bone mass in middle-aged women: Role of menopausal status and physical activity. J. Cachexia Sarcopenia Muscle. 2020, 11, 698–709. [Google Scholar] [CrossRef]
- García-Bustínduy, M.; Gantes, M.A. Corticoides y osteoporosis. Actas Dermo Sifiliogr. 2007, 98, 526–530. [Google Scholar] [CrossRef]
- Greendale, G.A.; Sternfeld, B.; Huang, M.; Han, W.; Karvonen-Gutierrez, C.; Ruppert, K.; Cauley, J.A.; Finkelstein, J.S.; Jiang, S.-F.; Karlamangla, A.S. Changes in body composition and weight during the menopause transition. JCI Insight. 2019, 4, e124865. [Google Scholar] [CrossRef] [PubMed]
| Period | Days/Week | Exercise Mode | Total Session Duration (Min) | Between Intervals | Intervals/Sprints | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Average Internal Load | Average HR (Beats·Min−1) | Average %HRmax | Average SpO2 (%) | Number × Duration/Recovery | RPE (0–10) | Average HR (Beats·Min−1) | HR (%HRmax) | Average SPO2MIN (%) | ||||
| July–September 2015 | 4 | Cycling | 30 | 50% (VT-RCP) | 125 | 74 | 96 | 10–15 × 8 s/2–3 min | 9 | 130 | 77 | 93 |
| October–December 2015 | 3–4 | Cycling | 40–60 | 50%(VT-RCP) | 132 | 79 | 94 | 14–30 × 8 s/2–3 min | 8 | 135 | 80 | 93 |
| January–March 2016 | 3–4 | Cycling | 60 | 50% (VT-RCP) | 135 | 81 | 95 | 30 × 5–10 s/1 min | 7 | 141 | 84 | 91 |
| April–June 2016 | 3 | Cycling | 60 | 50% (VT-RCP) | 125 | 75 | 94 | 30 × 5 s/1 min | 7 | 135 | 81 | 91 |
| July–September 2016 | 3 | Cycling | 60–45 | 50% (VT-RCP) | 125 | 75 | 95 | 30–23 × 10 s/2 min | 7 | 135 | 81 | 90 |
| October–November 2016 | 3–4 | Cycling | 45 | 50% (VT-RCP) | 125 | 75 | 94 | 23 × 10 s/2 min | 7 | 135 | 81 | 90 |
| December 2016 | Decrease in medication (corticosteroids) | |||||||||||
| January–March 2017 | 3 | Cycling | 45–60 | 50% (VT-RCP) | 135 | 94 | 23–30 × 10 s/2 min | 8 | 145 | 87 | 90 | |
| April 2017 | 2 | Cycling | 60 | 50% (VT-RCP) | 135 | 81 | 94 | 30 × 10 s/2 min | 8 | 145 | 87 | 89 |
| May–June 2017 | Progressive withdrawal of medication | |||||||||||
| July–September 2017 | 2–3 | Cycling | 30–60 | 50% (VT-RCP) | 130 | 78 | 94 | 15–30 × 10 s/2 min | 7 | 145 | 87 | 90 |
| October–November 2017 | 3 | Cycling | 45–60 | 50% (VT-RCP) | 135 | 81 | 94 | 23–30 × 10 s/2 min | 7 | 145 | 87 | 90 |
| December 2017 | Exacerbation of sarcoidosis | |||||||||||
| January–March 2018 | 2 | Cycling | 60 | 50% (VT-RCP) | 135 | 82 | 94 | 30 × 10 s/2 min | 6 | 143 | 87 | 89 |
| April–June 2018 | 3 | Running | 30 | 7 km·h−1 | 135 | 82 | 90 | 12 × 15 s (15 km·h−1)/2.5 min | 9 | 140 | 85 | 89 |
| July–September 2018 | 2–3 | Running | 40–60 | 7 km·h−1 | 140 | 85 | 92 | 16–24 × 15 s (15 km·h−1)/2.5 min | 9 | 155 | 94 | 91 |
| October–December 2018 | 2 | Running | 40–60 | 7 km·h−1 | 142 | 86 | 93 | 16–24 × 15 s (15–18 km·h−1)/2.5 min | 9 | 165 | 100 | 89 |
| January–March 2019 | Plantar fasciitis | |||||||||||
| April–June 2019 | 2 | Cycling | 30–45 | 50% (VT-RCP) | 135 | 82 | 93 | 10–23 × 8 s/2–3 min | 5 | 145 | 88 | 89 |
| July–September 2019 | 2 | Running | 45 | 7 km·h−1 | 135 | 82 | 94 | 23 × 10 s (15 km·h−1)/2 min * | 9 | 155 | 95 | 85 |
| October–December 2019 | 2 | Running | 50–45 | 7 km·h−1 | 135 | 82 | 94 | 25–23 × 10 s (15 km·h−1)/2 min ** | 9 | 155 | 95 | 85 |
| Period | Days/Week | Classic Resistance Training | Days/Week | Functional Training | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Modified Chest Fly Machine * | Leg Press | Modified Behind the Neck Lat Pulldown ** | Planks *** | Russian Belt Squat | Clean & Jerk/Split | Step-Full Squat | Lunges | Squat Jumps | Burpees | |||
| July–September 2015 | 2 | 3 × 5–10 kg (8–92%) | 3 × 6–10/30 kg (6–94%) | 3 × 5–15 kg (7–88%) | 2/4 × 6 (8–94%) | |||||||
| October–December 2015 | 2 | 4 × 7–10 kg (8–91%) | 4 × 7–30/40 kg (6–94%) | 4 × 7–15 kg (7–88%) | 4 × 7 (7–92%) | |||||||
| January–March 2016 | 2 | 4 × 8−15 kg (9–91%) | 4 × 8−50 kg (6–95%) | 4 × 8–25 kg (8–88%) | 4 × 8 (7–94%) | 2 | 3 × 15 (8–90%) | 3 × 15 (5–93%) | 3 × 1/12 (7–90%) | |||
| April–June 2016 | 2 | 4 × 8−15 kg (9–92%) | 4 × 8−50 kg (6–95%) | 4 × 8–25 kg (8–88%) | 4 × 8 (7–94%) | 4 × 8–10 kg (9–90%) | 2 | 3 × 15 (6–90%) | 3 × 15 (5–93%) | 3 × 12 (8–90%) | 3 × 8 (9–89%) | |
| July–September 2016 | 2 | 4 × 8−15 kg (8–92%) | 4 × 8 −50/60 kg (7–95%) | 4 × 8–25 kg (7–88%) | 4 × 8 (7–94%) | 4 × 8–10 kg (8–90%) | 2 | 3 × 15 (5–90%) | 3 × 15 (5–94%) | 3 × 12 (7–88%) | 3 × 8 (9–88%) | |
| October–December 2016 | Decrease in medication (corticosteroids) | |||||||||||
| January–March 2017 | 2 | 4 × 8−15 kg (8–92%) | 4 × 8 −50/60 kg (8–95%) | 4 × 8–25 kg (8–85%) | 4 × 8 (7–94%) | 2 | 0/3 × 15 (6–90%) | 0/15 (5–92%) | 0/3 × 12 (8–88%) | 0/3 × 0/8 (9–85%) | ||
| April 2017 | 2 | 4 × 8−20 kg (9–90%) | 4 × 8 −60 kg (8–94%) | 4 × 8–25 kg (8–85%) | 4 × 8 (7–94%) | 4 × 8–10 kg (8–88%) | 2 | 3 × 15 (6–90%) | 15 (5–92%) | 3 × 12 (8–88%) | ||
| May–June 2017 | Progressive withdrawal of medication | |||||||||||
| July–September 2017 | 0–2 | 4 × 8−20 kg (8–90%) | 4 × 8 −60 kg (7–94%) | 4 × 8–25 kg (8–85%) | 4 × 8 (7–95%) | 4 × 8–10 kg (8–88%) | 0–2 | 0/3 × 12 (8–88%) | 0/3 × 12 (9–88%) | 0/3 × 10 (9–88%) | ||
| October–December 2017 | Exacerbation of sarcoidosis | |||||||||||
| January–March 2018 | 2 | 4 × 8−20/15 kg (7–90%) | 4 × 8 −60/70 kg (7–94%) | 4 × 8–20 kg (7–89%) | 4 × 8 (7–95%) | 4 × 8 –10 kg (8–90%) | 4 × 6–7.5 kg (9–88%) | 2 | 3 × 15 (6–94%) | 3 × 15 (5–94%) | 3 × 12 (6–88%) | |
| April–June 2018 | 2 | 4 × 8−15 kg (8–88%) | 4 × 8−60 kg (7–94%) | 4 × 8–20 kg (7–89%) | 4 × 8 (7–95%) | 4 × 8–8 kg (8–89%) | 4 × 6–7.5 kg (9–88%) | 2 | 3 × 15 (5–94%) | 2 × 15 (5–94%) | 2 × 12 (5–90%) | |
| July–September 2018 | 0–2 | 2/4 × 8−20 kg (7–92%) | 4 × 8−70 kg (7–92%) | 2/4 × 8–25 kg (8–88%) | 2/4 × 8 (7–95%) | 2/4 × 8–8 kg (7–92%) | 4 v 6–7.5 kg (9–88%) | 1–2 | 3 × 15 (5–94%) | 0/2 × 15 (5–94%) | 0/2 × 12 (5–90%) | |
| October–December 2018 | 0–2 | 2 × 8−20 kg (7–92%) | 4 × 8−70 kg (7–94%) | 2 × 8–20 kg (7–88%) | 2 × 8 (7–95%) | 2 × 8–8 kg (7–92%) | 4 × 6–7.5 kg (9–86%) | 1–2 | 3 × 15 (5–94%) | 0/3 × 15 (5–95%) | 0/3 × 12 (5–90%) | 0/3 × 10 (9–85%) |
| January–March 2019 | 1–2 | 2/3 × 8−20 kg (9–88%) | 2/3 × 8−70 kg (9–93%) | 2/3 × 8–25 kg (9–88%) | 2/3 × 8 (8–95%) | 2/3 × 8–8 kg (8–90%) | Plantar fasciitis | |||||
| April–June 2019 | 1 | 2/3 × 8−20 kg (9–88%) | 2/3 × 8−70 kg (8–93%) | 2/4 × 8–25 kg (9–85%) | 2/4 × 8 (8–93%) | 2/3 × 8–8 kg (9–90%) | 1 | 3 × 15 (8–90%) | 3 × 15 (8–92%) | 3 × 12 (7–90%) | 4 static planks | |
| July–September 2019 | 1 | 4 × 8−20 kg (8–92%) | 4 × 8−70 kg (7–94%) | 4 × 8–25 kg (7–85%) | 4 × 8 (9–88%) | 1 | 3 × 15 (8–90%) | 3 × 15 (8–90%) | 3 × 12 (6–90%) | 4 static planks | ||
| October–December 2019 | 1 | 4 × 8−20 kg (7–92%) | 4 × 8−70 kg (7–95%) | 4 × 8–25 kg (7–85%) | 4 × 8 (9–88%) | 1 | 3 × 15 (9–90%) | 3 × 15 (8–90%) | 3 × 12 (6–90%) | 4 static planks | ||
| Variables | Pretraining | December 2015 | June 2016 | December 2016 | June 2017 | December 2017 | June 2018 | December 2018 | June 2019 | December 2019 | Change from Baseline to 4.5 Years Later (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Peak values | |||||||||||
| VO2peak (mL·kg−1·min−1) | 20.1 | 22.4 | 30.2 | 23.6 | 24.4 | 25.2 | 28.9 | 28.3 | 26.6 | 28.9 | +44% |
| VO2peak (mL·min−1) | 1086 | 1212 | 1631 | 1275 | 1316 | 1360 | 1560 | 1550 | 1502 | 1561 | +44% |
| PPO (watts) | 100 | 119 | 123 | 130 | 125 | 120 | 130 | 127 | 130 | 124 | +24% |
| HRpeak (bpm) | 166 | 164 | 164 | 167 | 162 | 170 | 170 | 166 | 170 | 172 | +4% |
| HR (% HRmax) | 99 | 98 | 98 | 100 | 98 | 102 | 103 | 100 | 104 | 105 | +6% |
| VEpeak (L/min) | 62 | 59 | 73 | 65 | 83 | 87 | 81 | 97 | 77 | 99 | +60% |
| SpO2peak (%) | 93 | 91 | 91 | 88 | 89 | 88 | 89 | 89 | 89 | 91 | −2% |
| VT | |||||||||||
| VO2 (mL·kg−1·min−1) | 11.7 | 14.2 | 18.7 | 11.2 | 12.8 | 15.4 | 17.9 | 11.7 | 15.6 | 15.1 | +29% |
| PO (watts) | 47 | 57 | 66 | 35 | 47 | 50 | 47 | 41 | 60 | 42 | −11% |
| VE·VO2−1 | 38 | 29 | 31 | 28 | 31 | 27 | 29 | 25 | 28 | 26 | −32% |
| VE·VCO2−1 | 39 | 39 | 35 | 35 | 39 | 33 | 38 | 35 | 34 | 38 | −3% |
| RCP | |||||||||||
| VO2 (mL·kg−1·min−1) | 17.4 | 18.1 | 26.6 | 19.8 | 19.3 | 21.2 | 24.1 | 22.3 | 18.3 | 23.9 | +37% |
| PO (watts) | 77 | 87 | 103 | 106 | 89 | 87 | 83 | 102 | 95 | 90 | +17% |
| VE·VO2−1 | 42 | 42 | 35 | 36 | 36 | 35 | 35 | 36 | 32 | 36 | −14% |
| VE·VCO2−1 | 36 | 37 | 33 | 32 | 35 | 32 | 36 | 32 | 33 | 37 | +3% |
| Variables | Oct. | June | December | June | December | June | December | June | December | Change from Baseline to 3.5 Years Later (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| 2007 | 2016 | 2016 | 2017 | 2017 | 2018 | 2018 | 2019 | 2019 | ||
| BMD (g·cm−2) | ||||||||||
| Whole body | 1.11 | 1.07 | 1.07 | 1.05 | 1.06 | 1.04 | 1.02 | 1.06 | −4.5 | |
| Subtotal body | 0.91 | 0.89 | 0.89 | 0.87 | 0.88 | 0.86 | 0.86 | 0.89 | −2.2 | |
| Pelvic | 1.09 | 1.06 | 1.06 | 1.06 | 1.07 | 1.01 | 1.05 | 1.10 | 0.9 | |
| Arms (mean) | 0.67 | 0.65 | 0.65 | 0.64 | 0.65 | 0.65 | 0.64 | 0.65 | −3.0 | |
| Legs (mean) | 1.10 | 1.09 | 1.08 | 1.06 | 1.04 | 1.06 | 1.06 | 1.06 | −3.6 | |
| Lumbar (mean L1–L4) | 1.24 | 0.98 | 0.97 | 0.96 | 0.94 | 0.92 | 0.92 | 0.93 | 0.96 | −2.0 |
| T-Score spine | 0.4 | −0.6 | −0.7 | −0.8 | −0.9 | −1.2 | −1.1 | −1.1 | −0.8 | |
| Z-Score spine | 1.1 | 0.4 | 0.3 | 0.3 | 0.1 | −0.1 | 0.0 | 0.1 | 0.4 | |
| Femoral neck | 1.01 | 0.83 | 0.76 | 0.81 | 0.84 | 0.76 | 0.73 | 0.74 | 0.73 | −12.0 |
| T-Score femoral neck | 0.2 | −0.1 | −0.8 | −0.3 | −0.1 | −0.8 | −1.2 | −1.0 | −1.1 | |
| Z-Score femoral neck | 0.7 | 0.8 | 0.2 | 0.7 | 1.0 | 0.2 | 0.1 | 0.1 | 0.1 | |
| Lean mass (kg) | ||||||||||
| Whole body | 40.4 | 38.5 | 39.6 | 38.5 | 40.4 | 39.2 | 38.4 | 35.8 | −11.4 | |
| Subtotal body | 35.6 | 33.6 | 34.6 | 33.7 | 35.5 | 34.4 | 35.4 | 33.0 | −7.3 | |
| Trunk | 19.0 | 17.7 | 18.6 | 17.5 | 18.6 | 18.9 | 19.4 | 17.2 | −9.5 | |
| Arms (mean) | 2.0 | 1.9 | 2.0 | 1.9 | 2.1 | 1.9 | 1.8 | 1.9 | −5.0 | |
| Legs (mean) | 6.3 | 6.1 | 6.1 | 6.2 | 6.4 | 5.9 | 6.3 | 6.0 | −4.8 | |
| Fat mass (kg) | ||||||||||
| Whole body | 10.3 | 12.9 | 12.9 | 12.1 | 13.9 | 14.1 | 16.3 | 15.9 | 54.4 | |
| Subtotal body | 9.6 | 12.2 | 12.1 | 11.4 | 13.2 | 13.3 | 15.6 | 15.2 | 58.3 | |
| Trunk | 3.7 | 4.9 | 4.7 | 4.6 | 5.3 | 5.4 | 6.2 | 6.3 | 70.3 | |
| Arms (mean) | 0.3 | 0.4 | 0.4 | 0.4 | 0.5 | 0.5 | 0.7 | 0.6 | 100 | |
| Legs (mean) | 2.6 | 3.2 | 3.3 | 3.0 | 3.5 | 3.4 | 4.0 | 3.9 | 50 | |
| Fat mass (%) | 20.3 | 26.0 | 24.6 | 23.9 | 25.6 | 26.4 | 28.8 | 29.7 | 46.3 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herrera-Olivares, A.M.; García-Manso, J.M.; Rodríguez-Gómez, I.; Ara, I.; Lucia, A.; Santalla, A. Long-Term Benefits of Tailored Exercise in Severe Sarcoidosis: A Case Report. Int. J. Environ. Res. Public Health 2020, 17, 9512. https://doi.org/10.3390/ijerph17249512
Herrera-Olivares AM, García-Manso JM, Rodríguez-Gómez I, Ara I, Lucia A, Santalla A. Long-Term Benefits of Tailored Exercise in Severe Sarcoidosis: A Case Report. International Journal of Environmental Research and Public Health. 2020; 17(24):9512. https://doi.org/10.3390/ijerph17249512
Chicago/Turabian StyleHerrera-Olivares, Alba M., Juan M. García-Manso, Irene Rodríguez-Gómez, Ignacio Ara, Alejandro Lucia, and Alfredo Santalla. 2020. "Long-Term Benefits of Tailored Exercise in Severe Sarcoidosis: A Case Report" International Journal of Environmental Research and Public Health 17, no. 24: 9512. https://doi.org/10.3390/ijerph17249512
APA StyleHerrera-Olivares, A. M., García-Manso, J. M., Rodríguez-Gómez, I., Ara, I., Lucia, A., & Santalla, A. (2020). Long-Term Benefits of Tailored Exercise in Severe Sarcoidosis: A Case Report. International Journal of Environmental Research and Public Health, 17(24), 9512. https://doi.org/10.3390/ijerph17249512








