Establishing a Theory-Based Multi-Level Approach for Primary Prevention of Mental Disorders in Young People
Abstract
1. Our Current Approach to Tackle Rising Youth Mental Health Problems is Unsustainable
2. Including Context as Well as Individual Risk and Resilience Factors
3. The Covid-19 Pandemic Provides Further Evidence of Multi-Dimensional and Multi-Level Determinants of Mental Health
4. A Public Health Approach to Prevention: Shifting the Population Mean
5. Public Mental Health Prevention to Tackle Individual and Social Determinants
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- GBD Results Tool. 2017. Available online: http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2017-permalink/bd999a870fa2808a11ed33ca8dfad566 (accessed on 10 October 2020).
- Mokdad, A.H.; Forouzanfar, M.H.; Daoud, F.; Mokdad, A.A.; El Bcheraoui, C.; Moradi-Lakeh, M.; Kyu, H.H.; Barber, R.M.; Wagner, J.; Cercy, K.; et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2016, 387, 2383–2401. [Google Scholar] [CrossRef]
- Vos, T.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abate, K.H.; Abd-Allah, F.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F.; Aboyans, V.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- Mental Health of Children and Young People in England, 2020: Wave 1 Follow up to the 2017 Survey—NHS Digital. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2020-wave-1-follow-up (accessed on 30 October 2020).
- Bor, W.; Dean, A.J.; Najman, J.; Hayatbakhsh, R. Are child and adolescent mental health problems increasing in the 21st century? A systematic review. Aust. N. Z. J. Psychiatry 2014, 48, 606–616. [Google Scholar] [CrossRef] [PubMed]
- Coley, R.L.; O’Brien, M.; Spielvogel, B. Secular Trends in Adolescent Depressive Symptoms: Growing Disparities between Advantaged and Disadvantaged Schools. J. Youth Adolesc. 2019, 48, 2087–2098. [Google Scholar] [CrossRef] [PubMed]
- Twenge, J.M.; Joiner, T.E.; Rogers, M.L.; Martin, G.N. Increases in Depressive Symptoms, Suicide-Related Outcomes, and Suicide Rates among U.S. Adolescents After 2010 and Links to Increased New Media Screen Time. Clin. Psychol. Sci. 2018, 6, 3–17. [Google Scholar] [CrossRef]
- Patalay, P.; Gage, S.H. Changes in millennial adolescent mental health and health-related behaviours over 10 years: A population cohort comparison study. Int. J. Epidemiol. 2019, 48, 1650–1664. [Google Scholar] [CrossRef]
- Li, J.Y.; Li, J.; Liang, J.H.; Qian, S.; Jia, R.X.; Wang, Y.Q.; Xu, Y. Depressive symptoms among children and adolescents in China: A systematic review and meta-analysis. Med. Sci. Monit. 2019, 25, 7459–7470. [Google Scholar] [CrossRef]
- Van Vuuren, C.L.; Uitenbroek, D.G.; Van Der Wal, M.F.; Chinapaw, M.J.M. Sociodemographic differences in 10-year time trends of emotional and behavioural problems among adolescents attending secondary schools in amsterdam, the netherlands. Eur. Child Adolesc. Psychiatry 2018, 27, 1621–1631. [Google Scholar] [CrossRef]
- Houtrow, A.J.; Larson, K.; Olson, L.M.; Newacheck, P.W.; Halfon, N. Changing trends of childhood disability, 2001–2011. Pediatrics 2014, 134, 530–538. [Google Scholar] [CrossRef]
- Collishaw, S. Annual research review: Secular trends in child and adolescent mental health. J. Child Psychol. Psychiatry 2015, 56, 370–393. [Google Scholar] [CrossRef]
- Patton, G.C.; Coffey, C.; Romaniuk, H.; Mackinnon, A.; Carlin, J.B.; Degenhardt, L.; Olsson, C.A.; Moran, P. The prognosis of common mental disorders in adolescents: A 14-year prospective cohort study. Lancet 2014, 383, 1404–1411. [Google Scholar] [CrossRef]
- Jones, P.B. Adult mental health disorders and their age at onset. Br. J. Psychiatry 2013, 202, 5–10. [Google Scholar] [CrossRef]
- Rocha, T.B.M.; Graeff-Martins, A.S.; Kieling, C.; Rohde, L.A. Provision of mental healthcare for children and adolescents: A worldwide view. Curr. Opin. Psychiatry 2015, 28, 330–335. [Google Scholar] [CrossRef]
- Saxena, S.; Thornicroft, G.; Knapp, M.; Whiteford, H. Resources for mental health: Scarcity, inequity, and inefficiency. Lancet 2007, 370, 878–889. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Atlas: Child and Adolescent Mental Health Resources Global Concerns: Implications for the Future; World Health Organization: Geneva, Switzerland, 2005; Available online: https://apps.who.int/iris/handle/10665/43307 (accessed on 10 October 2020).
- Children’s Commissioner. Lightning Review: Access to Child and Adolescent Mental Health Services. 2016. Available online: https://www.childrenscommissioner.gov.uk/wp-content/uploads/2017/06/Childrens-Commissioners-Mental-Health-Lightning-Review.pdf (accessed on 28 October 2020).
- Alemán-Díaz, A.Y.; Backhaus, S.; Siebers, L.L.; Chukwujama, O.; Fenski, F.; Henking, C.N.; Kaminska, K.; Kuttumuratova, A.; Weber, M.W. Child and adolescent health in Europe: Monitoring implementation of policies and provision of services. Lancet Child Adolesc. Heal. 2018, 2, 891–904. [Google Scholar] [CrossRef]
- Tsuang, M.T.; Bar, J.L.; Stone, W.S.; Faraone, S. V Gene-environment interactions in mental disorders. World Psychiatry 2004, 3, 73–83. [Google Scholar] [PubMed]
- Arango, C.; Díaz-Caneja, C.M.; McGorry, P.D.; Rapoport, J.; Sommer, I.E.; Vorstman, J.A.; McDaid, D.; Marín, O.; Serrano-Drozdowskyj, E.; Freedman, R.; et al. Preventive strategies for mental health. Lancet Psychiatry 2018, 5, 591–604. [Google Scholar] [CrossRef]
- Carrasco-Barrios, M.T.; Huertas, P.; Martín, P.; Martín, C.; Castillejos-Anguiano, M.C.; Petkari, E.; Moreno-Küstner, B. Determinants of suicidality in the european general population: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 4115. [Google Scholar] [CrossRef]
- Lund, C.; Brooke-Sumner, C.; Baingana, F.; Baron, E.C.; Breuer, E.; Chandra, P.; Haushofer, J.; Herrman, H.; Jordans, M.; Kieling, C.; et al. Social determinants of mental disorders and the Sustainable Development Goals: A systematic review of reviews. Lancet Psychiatry 2018, 5, 357–369. [Google Scholar] [CrossRef]
- Moreno-Peral, P.; Conejo-Cerón, S.; Motrico, E.; Rodríguez-Morejón, A.; Fernández, A.; García-Campayo, J.; Roca, M.; Serrano-Blanco, A.; Rubio-Valera, M.; Ángel Bellón, J. Risk factors for the onset of panic and generalised anxiety disorders in the general adult population: A systematic review of cohort studies. J. Affect. Disord. 2014, 168, 337–348. [Google Scholar] [CrossRef]
- Cerdá, M.; Sagdeo, A.; Johnson, J.; Galea, S. Genetic and environmental influences on psychiatric comorbidity: A systematic review. J. Affect. Disord. 2010, 126, 14–38. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, K.H. Social determinants of health: The how, who, and where screenings are occurring; a systematic review. Soc. Work Health Care 2019, 58, 719–745. [Google Scholar] [CrossRef] [PubMed]
- Alegría, M.; NeMoyer, A.; Falgàs Bagué, I.; Wang, Y.; Alvarez, K. Social Determinants of Mental Health: Where We Are and Where We Need to Go. Curr. Psychiatry Rep. 2018, 20, 95. [Google Scholar] [CrossRef]
- Patel, V.; Burns, J.K.; Dhingra, M.; Tarver, L.; Kohrt, B.A.; Lund, C. Income inequality and depression: A systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry 2018, 17, 76–89. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, W.S.; Bauer, A.; Andrade, M.C.R.; York-Smith, M.; Pan, P.M.; Pingani, L.; Knapp, M.; Coutinho, E.S.F.; Evans-Lacko, S. Income inequality and mental illness-related morbidity and resilience: A systematic review and meta-analysis. Lancet Psychiatry 2017, 4, 554–562. [Google Scholar] [CrossRef]
- Arenas, D.J.; Thomas, A.; Wang, J.C.; DeLisser, H.M. A Systematic Review and Meta-analysis of Depression, Anxiety, and Sleep Disorders in US Adults with Food Insecurity. J. Gen. Intern. Med. 2019, 34, 2874–2882. [Google Scholar] [CrossRef]
- Hahad, O.; Lelieveld, J.; Birklein, F.; Lieb, K.; Daiber, A.; Münzel, T. Ambient air pollution increases the risk of cerebrovascular and neuropsychiatric disorders through induction of inflammation and oxidative stress. Int. J. Mol. Sci. 2020, 21, 4306. [Google Scholar] [CrossRef]
- Bronfenbrenner, U.; Morris, P.A. The Bioecological Model of Human Development. In Handbook of Child Psychology; Damon, W., Lerner, R.M., Lerne, R.M., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2007. [Google Scholar] [CrossRef]
- Krieger, N. Epidemiology and the web of causation: Has anyone seen the spider? Soc. Sci. Med. 1994, 39, 887–903. [Google Scholar] [CrossRef]
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Social Equity in Health; Stockholm Institute for Further Studies: Stockholm, Sweden, 1991. [Google Scholar]
- Ungar, M.; Ghazinour, M.; Richter, J. Annual Research Review: What is resilience within the social ecology of human development? J. Child Psychol. Psychiatry 2013, 54, 348–366. [Google Scholar] [CrossRef]
- Tol, W.A.; Song, S.; Jordans, M.J. Annual Research Review: Resilience and mental health in children and adolescents living in areas of armed conflict--a systematic review of findings in low- and middle-income countries. J. Child Psychol. Psychiatry 2013, 54, 445–460. [Google Scholar] [CrossRef]
- McDaid, D. Making the Long-Term Economic Case for Investing in Mental Health to Contribute to Sustainability; European Union: Brussels, Belgium, 2011. [Google Scholar]
- Pearcey, S.; Shum, A.; Waite, P.; Patalay, P.; Creswell, C. Report 04: Changes in Children and Young People’s Emotional and behavIoural Difficulties through Lockdown. 2020. Available online: http://cospaceoxford.org/wp-content/uploads/2020/07/CoSPACE-Report-4-June-2020.pdf (accessed on 28 October 2020).
- Imran, N.; Aamer, I.; Sharif, M.I.; Bodla, Z.H.; Naveed, S. Psychological burden of quarantine in children and adolescents: A rapid systematic review and proposed solutions. Pakistan J. Med. Sci. 2020, 36, 1106–1116. [Google Scholar] [CrossRef] [PubMed]
- De Araújo, L.A.; Veloso, C.F.; de Campos Souza, M.; de Azevedo, J.M.C.; Tarro, G. The potential impact of the COVID-19 pandemic on child growth and development: A systematic review. J. Pediatr. (Rio. J) 2020, 23. [Google Scholar] [CrossRef]
- Xie, X.; Xue, Q.; Zhou, Y.; Zhu, K.; Liu, Q.; Zhang, J.; Song, R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020, 174, 898–900. [Google Scholar] [CrossRef] [PubMed]
- Stavridou, A.; Stergiopoulou, A.A.; Panagouli, E.; Mesiris, G.; Thirios, A.; Mougiakos, T.; Troupis, T.; Psaltopoulou, T.; Tsolia, M.; Sergentanis, T.N.; et al. Psychosocial consequences of COVID-19 in children, adolescents and young adults: A systematic review. Psychiatry Clin. Neurosci. 2020, 25. [Google Scholar] [CrossRef]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239. [Google Scholar] [CrossRef] [PubMed]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain. Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Troyer, E.A.; Kohn, J.N.; Hong, S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain. Behav. Immun. 2020, 87, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.S.; Lewis, G.; David, A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health 2020, 14, 20. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Hoffman, J.A.; Miller, E.A. Addressing the Consequences of School Closure Due to COVID-19 on Children’s Physical and Mental Well-Being. World Med. Heal. Policy 2020, 12, 300–310. [Google Scholar] [CrossRef]
- Orben, A.; Tomova, L.; Blakemore, S.J. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolesc. Heal. 2020, 4, 634–640. [Google Scholar] [CrossRef]
- Lee, J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc. Heal. 2020, 4, 421. [Google Scholar] [CrossRef]
- YoungMinds Coronavirus Report: Impact on Young People with Mental Health Needs. Available online: https://youngminds.org.uk/about-us/reports/coronavirus-impact-on-young-people-with-mental-health-needs/ (accessed on 28 October 2020).
- Duong, M.T.; Bruns, E.J.; Lee, K.; Cox, S.; Coifman, J.; Mayworm, A.; Lyon, A.R. Rates of Mental Health Service Utilization by Children and Adolescents in Schools and Other Common Service Settings: A Systematic Review and Meta-Analysis. Adm. Policy Ment. Heal. Ment. Heal. Serv. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Straatmann, V.S.; Lai, E.; Lange, T.; Campbell, M.C.; Wickham, S.; Andersen, A.M.N.; Strandberg-Larsen, K.; Taylor-Robinson, D. How do early-life factors explain social inequalities in adolescent mental health? Findings from the UK Millennium Cohort Study. J. Epidemiol. Community Health 2019, 73, 1049–1060. [Google Scholar] [CrossRef]
- Wickham, S.; Whitehead, M.; Taylor-Robinson, D.; Barr, B. The effect of a transition into poverty on child and maternal mental health: A longitudinal analysis of the UK Millennium Cohort Study. Lancet Public Heal. 2017, 2, e141–e148. [Google Scholar] [CrossRef]
- Reiss, F. Socioeconomic inequalities and mental health problems in children and adolescents: A systematic review. Soc. Sci. Med. 2013, 90, 24–31. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Henssler, J.; Stock, F.; van Bohemen, J.; Walter, H.; Heinz, A.; Brandt, L. Mental health effects of infection containment strategies: Quarantine and isolation—A systematic review and meta-analysis. Eur. Arch. Psychiatry Clin. Neurosci. 2020, 6, 1–12. [Google Scholar] [CrossRef]
- Hossain, M.M.; Sultana, A.; Purohit, N. Mental health outcomes of quarantine and isolation for infection prevention: A systematic umbrella review of the global evidence. Epidemiol. Health 2020, 42, e2020038. [Google Scholar] [CrossRef]
- McElroy, E.; Patalay, P.; Moltrecht, B.; Shevlin, M.; Shum, A.; Creswell, C.; Waite, P. Demographic and health factors associated with pandemic anxiety in the context of COVID-19. Br. J. Health Psychol. 2020, 25. [Google Scholar] [CrossRef]
- Iob, E.; Steptoe, A.; Fancourt, D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br. J. Psychiatry 2020, 217, 543–546. [Google Scholar] [CrossRef] [PubMed]
- Wright, L.; Steptoe, A.; Fancourt, D. Are we all in this together? Longitudinal assessment of cumulative adversities by socioeconomic position in the first 3 weeks of lockdown in the UK. J. Epidemiol. Community Health 2020, 74, 683–688. [Google Scholar] [PubMed]
- Burgess, R. COVID-19 mental-health responses neglect social realities. Nature 2020. [Google Scholar] [CrossRef] [PubMed]
- Rose, G. Sick individuals and sick populations. Int. J. Epidemiol. 1985, 14, 32–38. [Google Scholar] [CrossRef]
- Mehta, N.; Croudace, T.; Davies, S.C. Public mental health: Evidenced-based priorities. Lancet 2015, 385, 1472–1475. [Google Scholar] [CrossRef]
- Hosman, C.; Jane-Llopis, E.; Saxena, S. (Eds.) Prevention of Mental Disorders: Effective Interventions and Policy Options; Oxford University Press: Oxford, UK, 2005. [Google Scholar]
- Caspi, A.; Houts, R.M.; Belsky, D.W.; Goldman-Mellor, S.J.; Harrington, H.; Israel, S.; Meier, M.H.; Ramrakha, S.; Shalev, I.; Poulton, R.; et al. The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clin. Psychol. Sci. 2014, 2, 119–137. [Google Scholar] [CrossRef]
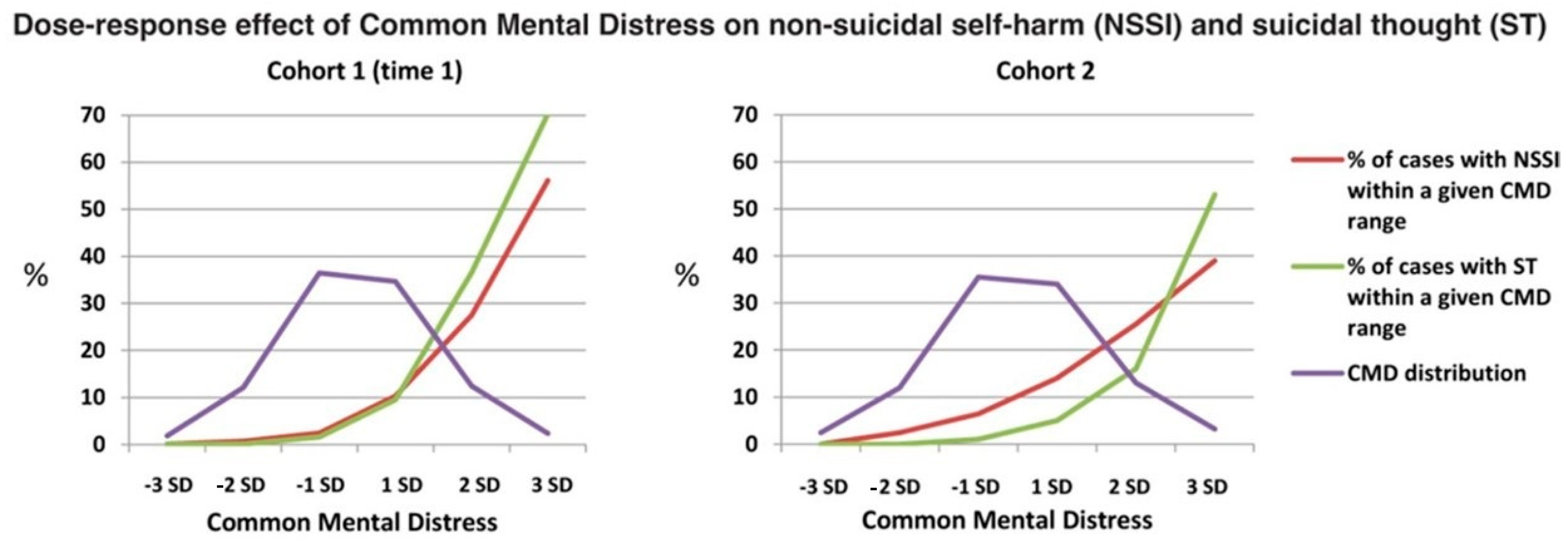
- Polek, E.; Neufeld, S.A.S.; Wilkinson, P.; Goodyer, I.; St Clair, M.; Prabhu, G.; Dolan, R.; Bullmore, E.T.; Fonagy, P.; Stochl, J.; et al. How do the prevalence and relative risk of non-suicidal self-injury and suicidal thoughts vary across the population distribution of common mental distress (the p factor)? Observational analyses replicated in two independent UK cohorts of young people. BMJ Open 2020, 10, e032494. [Google Scholar] [CrossRef]
- Patalay, P.; Fonagy, P.; Deighton, J.; Belsky, J.; Vostanis, P.; Wolpert, M. A general psychopathology factor in early adolescence. Br. J. Psychiatry 2015, 207, 15–22. [Google Scholar] [CrossRef]
- Stochl, J.; Khandaker, G.M.; Lewis, G.; Perez, J.; Goodyer, I.M.; Zammit, S.; Sullivan, S.; Croudace, T.J.; Jones, P.B. Mood, anxiety and psychotic phenomena measure a common psychopathological factor. Psychol. Med. 2015, 45, 1483–1493. [Google Scholar] [CrossRef] [PubMed]
- Krueger, R.F. The structure of common mental disorders. Arch. Gen. Psychiatry 1999, 56, 921–926. [Google Scholar] [CrossRef] [PubMed]
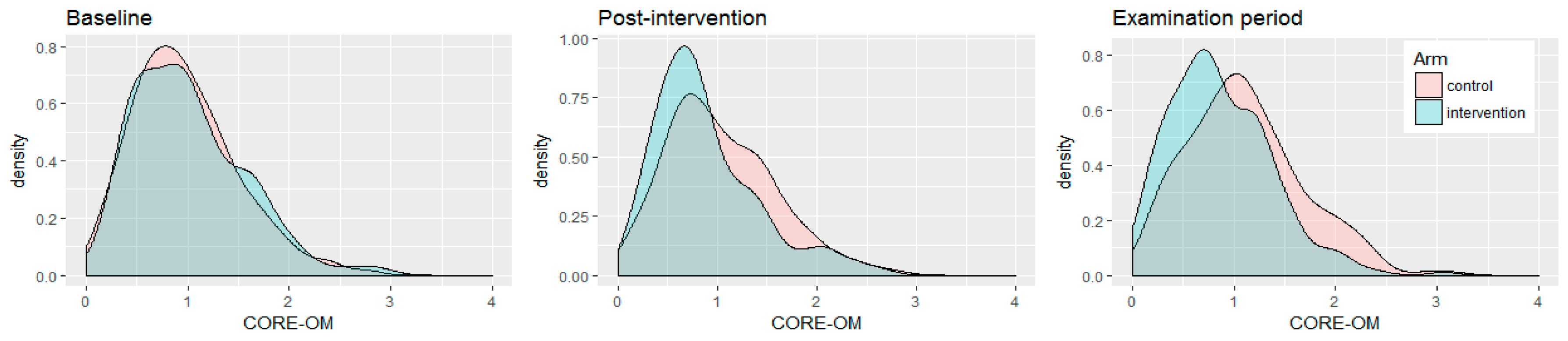
- Galante, J.; Dufour, G.; Vainre, M.; Wagner, A.P.; Stochl, J.; Benton, A.; Lathia, N.; Howarth, E.; Jones, P.B. A mindfulness-based intervention to increase resilience to stress in university students (the Mindful Student Study): A pragmatic randomised controlled trial. Lancet Public Health 2018, 3, e72–e81. [Google Scholar] [CrossRef]
- Connell, J.; Barkham, M.; Mellor-Clark, J. The effectiveness of UK student counselling services: An analysis using the CORE System. Br. J. Guid. Couns. 2008, 36, 1–18. [Google Scholar] [CrossRef]
- Galante, J.; Dufour, G.; Benton, A.; Howarth, E.; Vainre, M.; Croudace, T.J.; Wagner, A.P.; Stochl, J.; Jones, P.B. Protocol for the Mindful Student Study: A randomised controlled trial of the provision of a mindfulness intervention to support university students’ well-being and resilience to stress. BMJ Open 2016, 6, e012300. [Google Scholar] [CrossRef]
- Shinde, S.; Weiss, H.A.; Varghese, B.; Khandeparkar, P.; Pereira, B.; Sharma, A.; Gupta, R.; Ross, D.A.; Patton, G.; Patel, V. Promoting school climate and health outcomes with the SEHER multi-component secondary school intervention in Bihar, India: A cluster-randomised controlled trial. Lancet 2018, 392, 2465–2477. [Google Scholar] [CrossRef]
- Kutcher, S.; Wei, Y. School mental health: A necessary component of youth mental health policy and plans. World Psychiatry 2020, 19, 174–175. [Google Scholar] [CrossRef]
- Bafunno, D.; Catino, A.; Lamorgese, V.; Del Bene, G.; Longo, V.; Montrone, M.; Pesola, F.; Pizzutilo, P.; Cassiano, S.; Mastrandrea, A.; et al. Impact of tobacco control interventions on smoking initiation, cessation, and prevalence: A systematic review. J. Thorac. Dis. 2020, 12, 3844–3856. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Fact Sheet: Tobacco. Available online: https://www.who.int/news-room/fact-sheets/detail/tobacco (accessed on 28 October 2020).
- Garcia-Carrion, R.; Villarejo, B.C.; Villardón-Gallego, L. Children and adolescents mental health: A systematic review of interaction-based interventions in schools and communities. Front. Psychol. 2019, 10, 918. [Google Scholar] [CrossRef]
- Castillo, E.G.; Ijadi-Maghsoodi, R.; Shadravan, S.; Moore, E.; Mensah, M.O.; Docherty, M.; Aguilera Nunez, M.G.; Barcelo, N.; Goodsmith, N.; Halpin, L.E.; et al. Community Interventions to Promote Mental Health and Social Equity. Curr. Psychiatry Rep. 2019, 21, 35. [Google Scholar] [CrossRef]
- Rao, D.; Elshafei, A.; Nguyen, M.; Hatzenbuehler, M.L.; Frey, S.; Go, V.F. A systematic review of multi-level stigma interventions: State of the science and future directions. BMC Med. 2019, 17, 41. [Google Scholar] [CrossRef]
- Cleary, P.D.; Gross, C.P.; Zaslavsky, A.M.; Taplin, S.H. Multilevel interventions: Study design and analysis issues. J. Natl. Cancer Inst. Monogr. 2012, 2012, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Weiner, B.; Dorsey, S. Multilevel Interventions: State of the Science in Global Mental Health. Available online: https://www.nimh.nih.gov/news/media/2018/multilevel-interventions-state-of-the-science-in-global-mental-health.shtml (accessed on 28 October 2020).
- Evans, R.E.; Craig, P.; Hoddinott, P.; Littlecott, H.; Moore, L.; Murphy, S.; O’Cathain, A.; Pfadenhauer, L.; Rehfuess, E.; Segrott, J.; et al. When and how do ‘effective’interventions need to be adapted and/or re-evaluated in new contexts? The need for guidance. J. Epidemiol. Community Health 2019, 73. [Google Scholar] [CrossRef] [PubMed]
- Howarth, E.; Devers, K.; Moore, G.; O’Cathain, A.; Dixon-Woods, M. Contextual issues and qualitative research. In Challenges, Solutions and Future Directions in the Evaluation of Service Innovations in Health Care and Public Health; NIHR Journals Library: Southampton, UK, 2016. [Google Scholar]
- Lund, C.; De Silva, M.; Plagerson, S.; Cooper, S.; Chisholm, D.; Das, J.; Knapp, M.; Patel, V. Poverty and mental disorders: Breaking the cycle in low-income and middle-income countries. Lancet 2011, 378, 1502–1514. [Google Scholar] [CrossRef]
- Shamrova, D.P.; Cummings, C.E. Participatory action research (PAR) with children and youth: An integrative review of methodology and PAR outcomes for participants, organizations, and communities. Child. Youth Serv. Rev. 2017, 81, 400–412. [Google Scholar] [CrossRef]
- Sellars, E.; Pavarini, G.; Michelson, D.; Creswell, C.; Fazel, M. Young people’s advisory groups in health research: Scoping review and mapping of practices. Arch. Dis. Child. 2020. [Google Scholar] [CrossRef] [PubMed]
- Fazel, M.; Hoagwood, K. School mental health: Integrating Youth Voices to Shift the Paradigm. Lancet Child Adolesc. Health 2020, in press. [Google Scholar]
- Burgess, R.A.; Jain, S.; Petersen, I.; Lund, C. Social interventions: A new era for global mental health? The Lancet Psychiatry 2020, 7, 118–119. [Google Scholar] [CrossRef]
- Trickett, E.J.; Beehler, S. The Ecology of Multilevel Interventions to Reduce Social Inequalities in Health. Am. Behav. Sci. 2013, 57, 1227–1246. [Google Scholar] [CrossRef]
- Hall, K.L.; Oh, A.; Perez, L.G.; Rice, E.L.; Patel, M.; Czajkowski, S.; Klesges, L. The ecology of multilevel intervention research. Transl. Behav. Med. 2018, 8, 968–978. [Google Scholar] [CrossRef]
| Determinant | Demographic | Socio-Cultural | Economic | Environmental |
|---|---|---|---|---|
| COVID-19 unrelated | Gender | Adversity and stressful life events | Socio-economic disadvantage | Urbanicity |
| Age | Poor family, peer, and community connections | Poverty | Neighbourhood safety | |
| Discrimination | Financial strain | Air pollution | ||
| Income inequality | Climate change | |||
| Employment conditions | ||||
| Food insecurity | ||||
| Housing instability | ||||
| COVID-19 related | Social isolation | Job loss or instability | ||
| Social deprivation | Socio-economic uncertainty | |||
| Loss of loved ones | Inequity | |||
| Domestic violence and child maltreatment during isolation periods | Transition into income poverty during early childhood | |||
| Stigma | Accommodation issues | |||
| Fear of infecting others | ||||
| Exposure to frightful news | ||||
| Lack of control |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lo Moro, G.; Soneson, E.; Jones, P.B.; Galante, J. Establishing a Theory-Based Multi-Level Approach for Primary Prevention of Mental Disorders in Young People. Int. J. Environ. Res. Public Health 2020, 17, 9445. https://doi.org/10.3390/ijerph17249445
Lo Moro G, Soneson E, Jones PB, Galante J. Establishing a Theory-Based Multi-Level Approach for Primary Prevention of Mental Disorders in Young People. International Journal of Environmental Research and Public Health. 2020; 17(24):9445. https://doi.org/10.3390/ijerph17249445
Chicago/Turabian StyleLo Moro, Giuseppina, Emma Soneson, Peter B. Jones, and Julieta Galante. 2020. "Establishing a Theory-Based Multi-Level Approach for Primary Prevention of Mental Disorders in Young People" International Journal of Environmental Research and Public Health 17, no. 24: 9445. https://doi.org/10.3390/ijerph17249445
APA StyleLo Moro, G., Soneson, E., Jones, P. B., & Galante, J. (2020). Establishing a Theory-Based Multi-Level Approach for Primary Prevention of Mental Disorders in Young People. International Journal of Environmental Research and Public Health, 17(24), 9445. https://doi.org/10.3390/ijerph17249445





