International Prevalence and Correlates of Psychological Stress during the Global COVID-19 Pandemic
Abstract
1. Introduction
1.1. Background
1.2. Rationale and Hypotheses
2. Materials and Methods
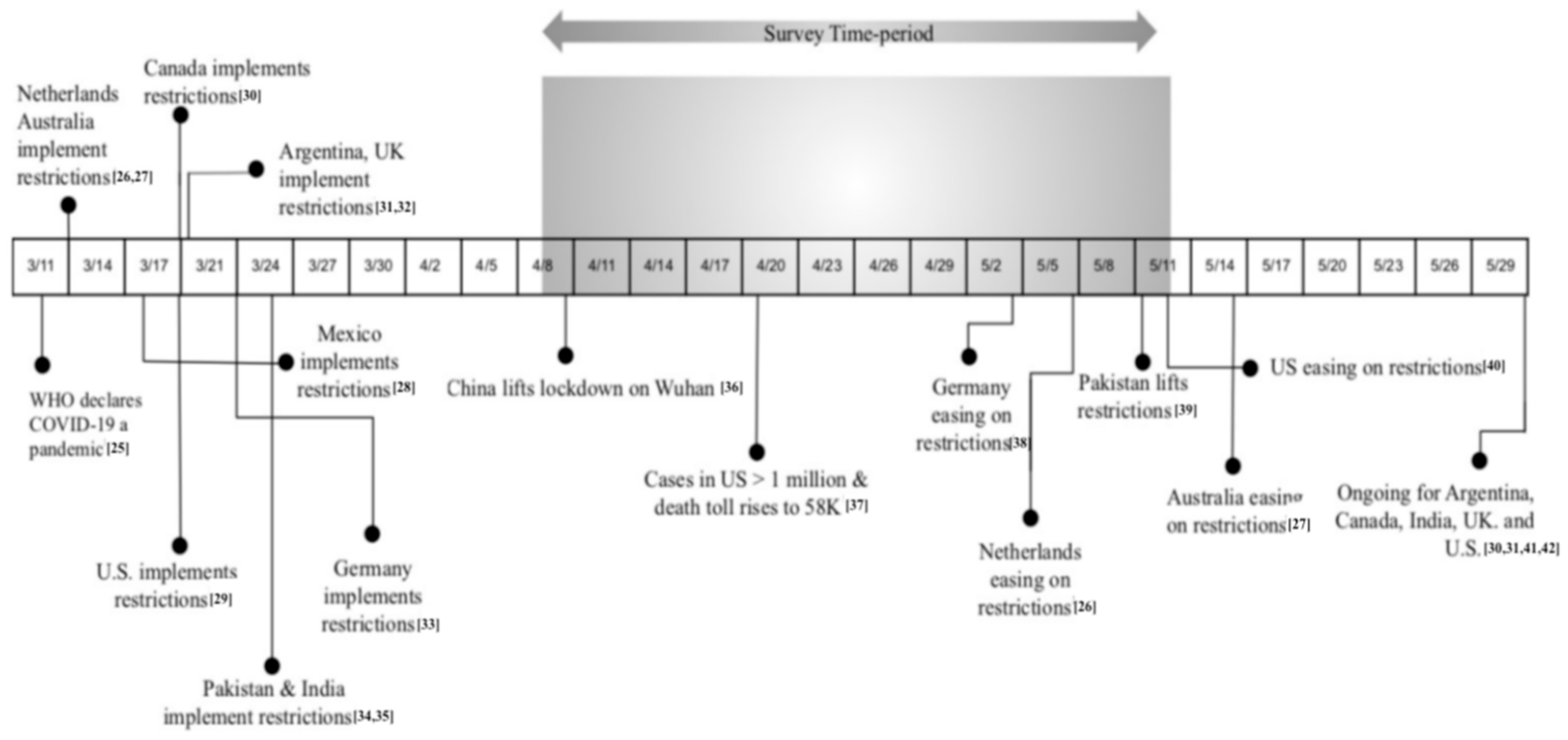
2.1. Study Design and Respondents
2.2. Measures
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Sociodemographic Factors and Perceived Stress
4.1.1. Gender and Age
4.1.2. Education
4.1.3. Race, Ethnicity, and Income
4.1.4. Remote Work
4.2. Personal Care/Burden and Perceived Stress
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Balkhair, A.A. COVID-19 Pandemic: A New Chapter in the History of Infectious Diseases. Oman. Med. J. 2020, 35, e123. [Google Scholar] [CrossRef] [PubMed]
- Marjanovic, Z.; Greenglass, E.R.; Coffey, S. The relevance of psychosocial variables and working conditions in predicting nurses’ coping strategies during the SARS crisis: An online questionnaire survey. Int. J. Nurs. Stud. 2007, 44, 991–998. [Google Scholar] [CrossRef] [PubMed]
- Tracy, M.; Norris, F.H.; Galea, S. Differences in the determinants of posttraumatic stress disorder and depression after a mass traumatic event. Depress. Anxiety 2011, 28, 666–675. [Google Scholar] [CrossRef] [PubMed]
- Galea, S.; Merchant, R.M.; Lurie, N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Intern. Med. 2020, 180, 817–818. Available online: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2764404 (accessed on 1 May 2020). [CrossRef]
- Butler, L.D.; Koopman, C.; Azarow, J.; Blasey, C.M.; Magdalene, J.C.; DiMiceli, S.; Seagraves, D.A.; Hastings, T.A.; Chen, X.; Garlan, R.W.; et al. Psychosocial Predictors of Resilience After the September 11, 2001 Terrorist Attacks. J. Nerv. Ment. Dis. 2009, 197, 266–273. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Norris, F.H.; Friedman, M.J.; Watson, P.J.; Byrne, C.M.; Diaz, E.; Kaniasty, K. 60,000 disaster victims speak: Part, I. An empirical review of the empirical literature, 1981–2001. Psychiatry 2002, 65, 207–239. [Google Scholar] [CrossRef]
- Galea, S.; Nandi, A.; Vlahov, D. The Epidemiology of Post-Traumatic Stress Disorder after Disasters. Epidemiol. Rev. 2005, 27, 78–91. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Flesia, L.; Fietta, V.; Colicino, E.; Segatto, B.; Monaro, M. Stable psychological traits predict perceived stress related to the COVID-19 outbreak. arXiv 2020. Available online: https://psyarxiv.com/yb2h8/ (accessed on 4 June 2020).
- Limcaoco, R.S.G.; Mateos, E.M.; Fernandez, J.M.; Roncero, C. Anxiety, worry and perceived stress in the world due to the COVID-19 pandemic, March 2020. Preliminary results. Psychiatry Clin. Psychol. 2020. [Google Scholar] [CrossRef]
- Liu, N.; Zhang, F.; Wei, C.; Jia, Y.; Shang, Z.; Sun, L.; Wu, L.; Sun, Z.; Zhou, Y.; Wang, Y.; et al. Prevalence and predictors of PTSS during COVID-19 Outbreak in China Hardest-hit Areas: Gender differences matter. Psychiatry Res. 2020, 287, 112921. [Google Scholar] [CrossRef] [PubMed]
- Losada-Baltar, A.; Jiménez-Gonzalo, L.; Gallego-Alberto, L.; Pedroso-Chaparro, M.d.; Fernandes-Pires, J.; Márquez-González, M. “We Are Staying at Home.” Association of Self-perceptions of Aging, Personal and Family Resources, and Loneliness with Psychological Distress During the Lock-Down Period of COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020. [Google Scholar] [CrossRef] [PubMed]
- Tull, M.T.; Edmonds, K.A.; Scamaldo, K.M.; Richmond, J.R.; Rose, J.P.; Gratz, K.L. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Res. 2020, 289, 113098. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; di Marco, A.; Rossi, A.; Siracusano, A.; di Lorenzo, G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. An N=18147 web-based survey. medRxiv 2020, 14. [Google Scholar] [CrossRef]
- Taha, S.; Matheson, K.; Cronin, T.; Anisman, H. Intolerance of uncertainty, appraisals, coping, and anxiety: The case of the 2009 H1N1 pandemic. Br. J. Health Psychol. 2014, 19, 592–605. [Google Scholar] [CrossRef]
- Butler, S.M. After COVID-19—Thinking Differently About Running the Health Care System. JAMA Health Forum 2020, 1, e200478. [Google Scholar] [CrossRef]
- Denovan, A.; Dagnall, N.; Dhingra, K.; Grogan, S. Evaluating the Perceived Stress Scale among UK university students: Implications for stress measurement and management. Stud. High. Educ. 2019, 44, 120–133. [Google Scholar] [CrossRef]
- Berg, J.; Bonnet, F.; Soares, S. Working from Home: Estimating the Worldwide Potential. VoxEU.org. Available online: https://voxeu.org/article/working-home-estimating-worldwide-potential (accessed on 30 September 2020).
- Power, K. The COVID-19 pandemic has increased the care burden of women and families. Sustain. Sci. Pract. Policy 2020, 16, 67–73. [Google Scholar] [CrossRef]
- Sim, K.; Huak Chan, Y.; Chong, P.N.; Chua, H.C.; Wen Soon, S. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J. Psychosom. Res. 2010, 68, 195–202. [Google Scholar] [CrossRef]
- Ranasinghe, C.; Ozemek, C.; Arena, R. Exercise and well-being during COVID 19—Time to boost your immunity. Expert Rev. Anti-Infect. Ther. 2020, 18, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Polizzi, C.; Lynn, S.J.; Perry, A. Stress and Coping in the Time of COVID-19: Pathways to Resilience and Recovery. Available online: https://www.clinicalneuropsychiatry.org/download/stress-and-coping-in-the-time-of-covid-19-pathways-to-resilience-and-recovery/ (accessed on 4 June 2020).
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Available online: https://www.ncbi.nlm.nih.gov/pubmed/32191675 (accessed on 20 May 2020).
- COVID19 in The Netherlands: A Timeline. 2020. Available online: https://www.containmentnu.nl/en/articles/timeline (accessed on 2 June 2020).
- Lupton, D. Timeline of COVID-19 in Australia. Available online: https://medium.com/@deborahalupton/timeline-of-covid-19-in-australia-1f7df6ca5f23 (accessed on 17 August 2020).
- Suspenden 66 Establecimientos No Esenciales en CDMX. Available online: https://www.msn.com/es-mx/noticias/mexico/suspenden-66-establecimientos-no-esenciales-en-cdmx/ar-BB13HEdA (accessed on 2 June 2020).
- Calfas, J.; Stancati, M.; Yap, C.-W. California Orders Lockdown for State’s 40 Million Residents. The Wall Street Journal. Available online: https://www.wsj.com/articles/china-reports-no-new-domestic-coronavirus-infections-for-the-first-time-since-outbreak-started-11584611233 (accessed on 2 June 2020).
- Government of Canada. Coronavirus Disease (COVID-19): Who Can Travel to Canada–Citizens, Persons Registered under Canada’s Indian Act, Permanent Residents, Foreign Nationals and Refugees. Available online: https://www.canada.ca/en/immigration-refugees-citizenship/services/coronavirus-covid19/travel-restrictions-exemptions.html (accessed on 13 August 2020).
- Rosario, J.; Gillespie, P. Argentina Orders ‘Exceptional’ Lockdown in Bid to Stem Virus. Available online: https://www.bloomberg.com/news/articles/2020-03-20/argentina-orders-exceptional-lockdown-in-bid-to-contain-virus (accessed on 20 March 2020).
- Holmes, F. COVID-19 Timeline. Available online: https://bfpg.co.uk/2020/04/covid-19-timeline/ (accessed on 16 September 2020).
- Der Spiegel. An Overview of the Updated Restrictions on Public Life in Germany. Available online: https://www.spiegel.de/consenta?targetUrl=https%3A%2F%2Fwww.spiegel.de%2Finternational%2Fgermany%2Fgermany-imposes-tougher-restrictions-on-public-life-a-fe5a067b-ee7a-4521-9940-edfa637f90de (accessed on 2 June 2020).
- The Statesman. Coronavirus Pandemic: Pakistan to Extend Lockdown for 2 More Weeks as Death Toll Reaches. Available online: https://www.thestatesman.com/world/coronavirus-pandemic-pakistan-extend-lockdown-2-weeks-death-toll-reaches-31-1502872742.html (accessed on 2 June 2020).
- Gettleman, J.; Schultz, K. Modi Orders 3-Week Total Lockdown for All 1.3 Billion Indians. Available online: https://www.nytimes.com/2020/03/24/world/asia/india-coronavirus-lockdown.html (accessed on 24 March 2020).
- China’s Wuhan Officially Lifts Lockdown. Available online: https://www.bloomberg.com/news/videos/2020-04-08/china-s-wuhan-officially-lifts-lockdown-video (accessed on 20 May 2020).
- Jeffery, L. U.S. Surpasses 1 Million Coronavirus Cases. NPR. Available online: https://www.npr.org/sections/coronavirus-live-updates/2020/04/28/846741935/u-s-surpasses-1-million-coronavirus-cases (accessed on 20 May 2020).
- Donahue, P.; Delfs, A. Merkel Allows Smaller German Shops to Reopen in Lockdown Easing. Available online: https://www.bloomberg.com/news/articles/2020-04-15/germany-likely-to-extend-national-lockdown-measures-until-may-3-k913n3v2 (accessed on 20 May 2020).
- Pakistan South Central Asia. Available online: https://www.osac.gov/Country/Pakistan/Detail (accessed on 20 May 2020).
- Coronavirus Reopening. USA Today. 2 May 2020. Available online: https://www.usatoday.com/storytelling/coronavirus-reopening-america-map/ (accessed on 2 June 2020).
- Raszewski, E.; Garrison, C. Buenos Aires Lockdown Extended until June 7 after Rise in Coronavirus Cases. Available online: https://www.reuters.com/article/us-health-coronavirus-argentina/buenos-aires-lockdown-extended-until-june-7-after-rise-in-coronavirus-cases-idUSKBN22Z0YB?il=0 (accessed on 23 May 2020).
- Coronavirus Lockdown Extended till 31 May, Says NDMA. Available online: https://www.livemint.com/news/india/covid-19-lockdown-4-0-coronavirus-lockdown-extended-till-31-may-says-ndma-11589715203633.html (accessed on 17 May 2020).
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Woods, D.; Harms, P.; Lowman, G.; DeSimone, J. Response Speed and Response Consistency as Mutually Validating Indicators of Data Quality in Online Samples. Soc. Psychol. Personal. Sci. 2017. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 1st ed.; Academic Press: New York, NY, USA, 1977. [Google Scholar]
- Hamza Shuja, K.; Aqeel, M.; Jaffar, A.; Ahmed, A. COVID-19 Pandemic and Impending Global Mental Health Implications. Psychiat. Danub. 2020, 32, 32–35. [Google Scholar] [CrossRef]
- González-Ramírez, M.T.; Rodríguez-Ayán, M.N.; Hernández, R.L. The Perceived Stress Scale (PSS): Normative Data and Factor Structure for a Large-Scale Sample in Mexico. Span. J. Psychol. 2013, 16, E47. Available online: https://www.cambridge.org/core/journals/spanish-journal-of-psychology/article/perceived-stress-scale-pss-normative-data-and-factor-structure-for-a-largescale-sample-in-mexico/752B62D15A932A2D148D04376E949F67#fndtn-information (accessed on 28 April 2020).
- Martin, P. The Effect of a Virus on Adult Development. J. Adult Dev. 2020, 27, 1–2. [Google Scholar] [CrossRef]
- Klein, E.M.; Brähler, E.; Dreier, M.; Reinecke, L.; Müller, K.W.; Schmutzer, G.; Wölfling, K.; Beutel, M.E. The German version of the Perceived Stress Scal—Psychometric characteristics in a representative German community sample. BMC Psychiatry 2016, 16, 159. [Google Scholar] [CrossRef]
- Pangtey, R.; Basu, S.; Meena, G.S.; Banerjee, B. Perceived Stress and its Epidemiological and Behavioral Correlates in an Urban Area of Delhi, India: A Community-Based Cross-Sectional Study. Indian J. Psychol. Med. 2020, 42, 80–86. [Google Scholar] [CrossRef]
- Huang, F.; Wang, H.; Wang, Z.; Zhang, J.; Du, W.; Su, C.; Jia, X.; Ouyang, Y.; Wang, Y. Psychometric properties of the perceived stress scale in a community sample of Chinese. BMC Psychiatry 2020, 20, 130. [Google Scholar] [CrossRef]
- Baik, S.H.; Fox, R.S.; Mills, S.D.; Roesch, S.C.; Sadler, G.R.; Klonoff, E.A.; Malcarne, V.L. Reliability and validity of the Perceived Stress Scale-10 in Hispanic Americans with English or Spanish language preference. J. Health Psychol. 2019, 24, 628–639. [Google Scholar] [CrossRef]
- Cohen, S.; Janicki-Deverts, D. Who’s Stressed? Distributions of Psychological Stress in the United States in Probability Samples from 1983, 2006, and 20091: Psychological Stress in the U.S. J. Appl. Soc. Psychol. 2012, 42, 1320–1334. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7061893/ (accessed on 29 May 2020). [CrossRef] [PubMed]
- Chiu, I.-M.; Cheng, C.-Y.; Zhang, H.; Lin, C.-H.R. Self-screening to reduce medical resource consumption facing the COVID-19 pandemic. Emerg. Med. J. 2020, 37, 255. [Google Scholar] [CrossRef] [PubMed]
- IBISWorld Industry Insider. Effects of COVID-19 on Global Healthcare Systems. Available online: https://www.ibisworld.com/industry-insider/coronavirus-insights/effects-of-covid-19-on-global-healthcare-systems/ (accessed on 4 June 2020).
- Brynjolfsson, E.; Horton, J.; Ozimek, A. COVID-19 and Remote Work: An Early Look at US Data. MIT Initiat. Digit. Econ. 2020. [Google Scholar] [CrossRef]
- Williams, R.D.; Brundage, J.A.; Williams, E.B. Moral Injury in Times of COVID-19. J. Health Serv. Psychol. 2020, 2, 1–5. [Google Scholar] [CrossRef] [PubMed]


| Demographics | N | % | Mean | SD |
|---|---|---|---|---|
| Total | 1685 | 100% | 19.08 | 7.17 |
| Age (Years) | ||||
| 18–24 years old | 279 | 16.56% | 20.14 | 7.26 |
| 25–34 years old | 429 | 25.46% | 20.57 | 7.07 |
| 35–44 years old | 381 | 22.61% | 19.86 | 6.75 |
| 45–54 years old | 310 | 18.40% | 18.1 | 6.53 |
| 55–64 years old | 173 | 10.27% | 16.8 | 7 |
| 65–74 years old | 77 | 4.57% | 16.26 | 7.49 |
| 75 years or older | 36 | 2.14% | 10.36 | 5.64 |
| Gender | ||||
| Male | 627 | 37.21% | 17.2 | 7.05 |
| Female | 1047 | 62.14% | 20.17 | 7 |
| Other | 11 | 0.65% | 21.91 | 7.84 |
| Marital Status | ||||
| Married | 841 | 49.91% | 18.42 | 7.07 |
| Widowed | 20 | 1.19% | 17.05 | 9.08 |
| Divorced | 88 | 5.22% | 18.55 | 6.8 |
| Separated | 22 | 1.31% | 18.59 | 6.7 |
| Partnered | 198 | 11.75% | 20.2 | 7.61 |
| Single | 441 | 4.45% | 19.92 | 7.13 |
| Other | 75 | 26.17% | 19.91 | 6.29 |
| Education (Years) | ||||
| High school graduate (high school diploma or equivalent including General Education Development (GED) | 79 | 4.69% | 19.24 | 8.76 |
| Some college but no degree | 223 | 13.23% | 19.7 | 7.48 |
| Associate degree in college (2-year) | 83 | 4.93% | 19.52 | 6.65 |
| Bachelor’s degree in college (4-year) | 526 | 31.22% | 19.54 | 7.09 |
| Master’s degree | 425 | 25.22% | 18.77 | 6.72 |
| Doctoral degree | 255 | 15.13% | 18.1 | 7.01 |
| Professional degree (Juris Doctor (JD), Medical Doctor (MD) | 94 | 5.58% | 18.54 | 7.88 |
| Employment Status * | ||||
| Working (full-time) | 977 | 55.07% | 18.77 | 6.94 |
| Working (part-time) | 163 | 9.19% | 19.61 | 7.21 |
| Unemployed | 104 | 5.86% | 20.72 | 7.39 |
| Retired | 70 | 5.81% | 22.2 | 7.47 |
| Not working due to disability | 103 | 1.30% | 14.51 | 7.15 |
| Student | 23 | 13.59% | 22.04 | 6 |
| Other | 241 | 5.24% | 20.52 | 7.17 |
| Laid off or looking for work due to COVID-19 | 93 | 3.95% | 19.54 | 7.46 |
| Countries * | ||||
| United States of America | 869 | 51.20% | 18.99 | 7.42 |
| Pakistan | 153 | 8.97% | 18.27 | 6.39 |
| Canada | 88 | 5.16% | 19.9 | 7.06 |
| Netherlands | 81 | 4.75% | 18.94 | 7.87 |
| Germany | 53 | 3.17% | 18.25 | 6.27 |
| Mexico | 47 | 3.05% | 17.87 | 6.19 |
| Australia | 45 | 2.76% | 20.2 | 7.08 |
| Argentina | 44 | 2.64% | 19.86 | 7.27 |
| United Kingdom | 38 | 2.23% | 21.32 | 6.51 |
| India | 38 | 2.23% | 19.55 | 6.31 |
| China | 33 | 1.99% | 17.15 | 4.47 |
| Other Countries ** | ||||
| Total | 196 | 11.63% | 19.70 | 7.20 |
| U.S. Regions | ||||
| Northeast | 99 | 12.4% | 20.42 | 6.74 |
| South | 201 | 25.3% | 19.39 | 7.6 |
| Midwest | 74 | 9.32% | 18.98 | 7.96 |
| West | 420 | 52.90% | 18.49 | 7.35 |
| Dependents | ||||
| 0 | 826 | 49.02% | 19.32 | 7.48 |
| 1 | 242 | 14.36% | 18.62 | 7.19 |
| 2 | 290 | 17.21% | 19.33 | 6.82 |
| 3 | 166 | 9.74% | 18.63 | 6.78 |
| 4 | 75 | 4.40% | 19.04 | 6.64 |
| 5+ | 86 | 5.04% | 18.09 | 6.28 |
| Remote Work | ||||
| N/A | 544 | 32.28% | 18.88 | 7.61 |
| <1 h | 27 | 2.68% | 17.59 | 6.42 |
| 1–5 h | 241 | 23.91% | 19.51 | 6.52 |
| 5–8 h | 447 | 44.35% | 18.98 | 6.75 |
| >8 h | 293 | 29.07% | 19.14 | 7.24 |
| Homeschooling | ||||
| Yes | 517 | 30.68% | 19.46 | 7.61 |
| No | 813 | 48.25% | 18.64 | 7.31 |
| N/A | 355 | 21.07% | 19.5 | 6.59 |
| Healthcare Industry Workers | ||||
| Yes | 180 | 10.68% | 18.78 | 6.79 |
| No | 1505 | 89.32% | 19.12 | 7.22 |
| Demographics | Beta Coef | Std Error | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Marital Status | |||||
| Widowed | −2.75 | 3.89 | −10.41 | 4.90 | 0.48 |
| Divorced | −0.67 | 1.03 | −2.08 | 1.95 | 0.95 |
| Separated | −1.46 | 1.87 | −5.15 | 2.22 | 0.43 |
| Partnered | 0.46 | 0.82 | −1.15 | 2.06 | 0.58 |
| Other | 0.29 | 1.43 | −2.51 | 3.10 | 0.21 |
| Single | 0.41 | 0.72 | −1.01 | 1.82 | 0.56 |
| Age | |||||
| 25–34 | 0.85 | 1.00 | −1.10 | 2.90 | 0.39 |
| 35–44 | −0.13 | 1.11 | −2.32 | 2.06 | 0.91 |
| 45–54 | −1.32 | 1.13 | −3.54 | 0.89 | 0.24 |
| 55–64 | −2.14 | 1.23 | −4.54 | 0.27 | 0.08 |
| 65–74 | −2.04 | 1.75 | −5.48 | 1.40 | 0.25 |
| 75+ | −7.13 | 3.65 | −14.29 | 0.03 | 0.05 |
| Gender | |||||
| Female | 3.17 | 0.51 | 2.18 | 4.16 | 0.00 |
| Other | 1.19 | 2.76 | −4.23 | 6.62 | 0.67 |
| Education | |||||
| Some college/no degree | 3.25 | 1.65 | 0.02 | 6.48 | 0.05 |
| Two-year | 3.18 | 2.02 | −0.79 | 7.16 | 0.12 |
| Four-year | 3.28 | 1.58 | 0.18 | 6.38 | 0.04 |
| Master’s | 2.11 | 1.60 | −1.03 | 5.26 | 0.18 |
| Doctoral | 2.74 | 1.62 | −0.43 | 5.92 | 0.09 |
| Professional Degree (JD/MD) | 1.47 | 1.76 | −1.98 | 4.92 | 0.40 |
| Employment Status | |||||
| Employed part-time | −0.25 | 0.86 | −1.93 | 1.43 | 0.77 |
| Unemployed | 0.31 | 2.02 | −3.65 | 4.27 | 0.87 |
| Laid off due to COVID | 1.97 | 2.09 | −2.13 | 6.08 | 0.35 |
| Retired | −0.95 | 2.78 | −6.41 | 4.51 | 0.73 |
| Student | 1.82 | 1.00 | −0.15 | 3.79 | 0.07 |
| Other | −0.91 | 1.42 | −3.69 | 1.87 | 0.52 |
| Income Bracket | |||||
| 10,000 to 50,000 | 1.30 | 1.06 | −0.78 | 3.39 | 0.22 |
| 50,000 to 75,000 | 0.18 | 1.18 | −2.12 | 2.49 | 0.87 |
| 75,000 to 100,000 | 0.15 | 1.25 | −2.31 | 2.61 | 0.91 |
| 100,000 to 125,000 | −0.47 | 1.24 | −2.90 | 1.96 | 0.71 |
| 125,000 to 150,000 | −0.15 | 1.25 | −2.60 | 2.31 | 0.91 |
| 150,000 to 175,000 | 1.74 | 1.36 | −0.92 | 4.40 | 0.20 |
| 175,000 to 200,000 | 1.11 | 1.32 | −1.48 | 3.71 | 0.40 |
| Greater than 200,000 | 0.45 | 1.12 | −1.75 | 2.65 | 0.69 |
| Composites | |||||
| Personal Burden Composite | 0.66 | 0.41 | −0.15 | 1.47 | 0.11 |
| Personal Care Composite | −0.39 | 0.06 | −0.50 | −0.28 | 0.00 |
| Family or Friends with COVID | 0.60 | 0.55 | −0.48 | 1.68 | 0.28 |
| Hours of Daily Remote Work | −0.08 | 0.33 | −0.73 | 0.57 | 0.80 |
| Change in Work Expectations | −0.40 | 0.14 | −0.67 | −0.12 | 0.01 |
| Increase in personal care Composite | −1.32 | 0.52 | −2.35 | −0.30 | 0.01 |
| U.S. Regions | |||||
| Northeast | 0.45 | 0.97 | −1.46 | 2.36 | 0.64 |
| South | −0.92 | 0.87 | −2.62 | 0.79 | 0..29 |
| Midwest | −0.15 | 1.16 | −2.42 | 2.12 | 0.89 |
| West | −1.36 | 0.72 | −2.76 | 0.05 | 0.06 |
| Country (n > 30) | |||||
| Pakistan | −2.43 | 1.09 | −4.58 | −0.28 | 0.03 |
| Germany | −4.63 | 1.55 | −7.68 | −1.58 | 0.00 |
| Canada | 0.75 | 1.17 | −1.54 | 3.04 | 0.52 |
| India | 0.08 | 2.02 | −3.89 | 4.04 | 0.97 |
| Netherlands | −1.77 | 1.38 | −4.48 | 0.94 | 0.20 |
| Mexico | −2.75 | 1.42 | −5.48 | −0.03 | 0.05 |
| United Kingdom | −1.53 | 1.99 | −4.33 | 1.27 | 0.28 |
| China | −1.68 | 1.47 | −5.59 | 2.23 | 0.40 |
| Australia | −0.02 | 2.06 | −2.93 | 2.88 | 0.98 |
| Argentina | 2.35 | 2.86 | −1.69 | 6.41 | 0.25 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adamson, M.M.; Phillips, A.; Seenivasan, S.; Martinez, J.; Grewal, H.; Kang, X.; Coetzee, J.; Luttenbacher, I.; Jester, A.; Harris, O.A.; et al. International Prevalence and Correlates of Psychological Stress during the Global COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 9248. https://doi.org/10.3390/ijerph17249248
Adamson MM, Phillips A, Seenivasan S, Martinez J, Grewal H, Kang X, Coetzee J, Luttenbacher I, Jester A, Harris OA, et al. International Prevalence and Correlates of Psychological Stress during the Global COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2020; 17(24):9248. https://doi.org/10.3390/ijerph17249248
Chicago/Turabian StyleAdamson, Maheen M., Angela Phillips, Srija Seenivasan, Julian Martinez, Harlene Grewal, Xiaojian Kang, John Coetzee, Ines Luttenbacher, Ashley Jester, Odette A. Harris, and et al. 2020. "International Prevalence and Correlates of Psychological Stress during the Global COVID-19 Pandemic" International Journal of Environmental Research and Public Health 17, no. 24: 9248. https://doi.org/10.3390/ijerph17249248
APA StyleAdamson, M. M., Phillips, A., Seenivasan, S., Martinez, J., Grewal, H., Kang, X., Coetzee, J., Luttenbacher, I., Jester, A., Harris, O. A., & Spiegel, D. (2020). International Prevalence and Correlates of Psychological Stress during the Global COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 17(24), 9248. https://doi.org/10.3390/ijerph17249248









