The Association between Community Water Fluoridation and Bone Diseases: A Natural Experiment in Cheongju, Korea
Abstract
1. Introduction
2. Study Area and Data
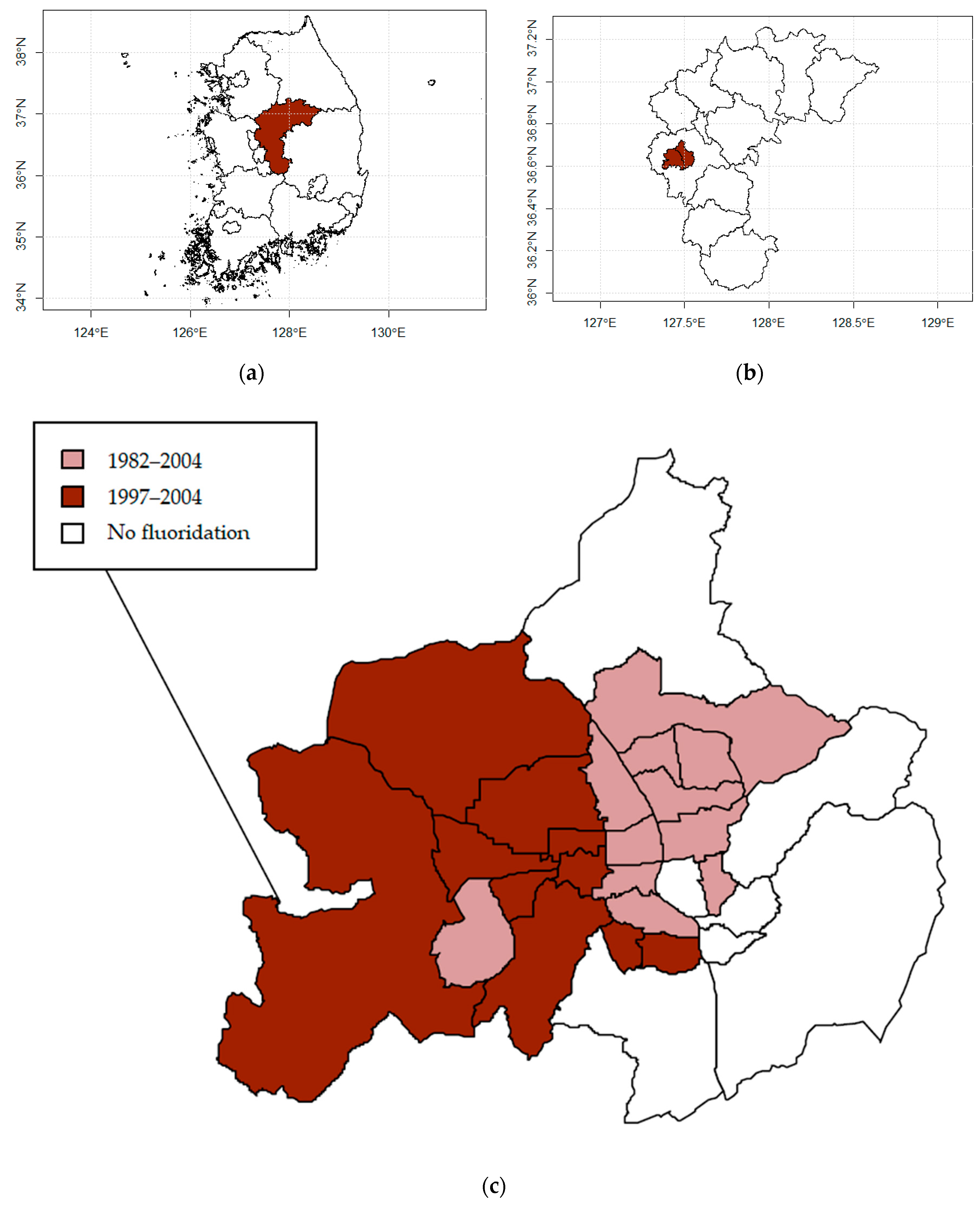
2.1. Study Design and Locations
2.2. Data Sources and Variables
3. Methodology
3.1. Modeling Health Risk
3.2. Spatio-Temporal Model
3.3. Sensitivity Analysis
3.4. Ethics Approval
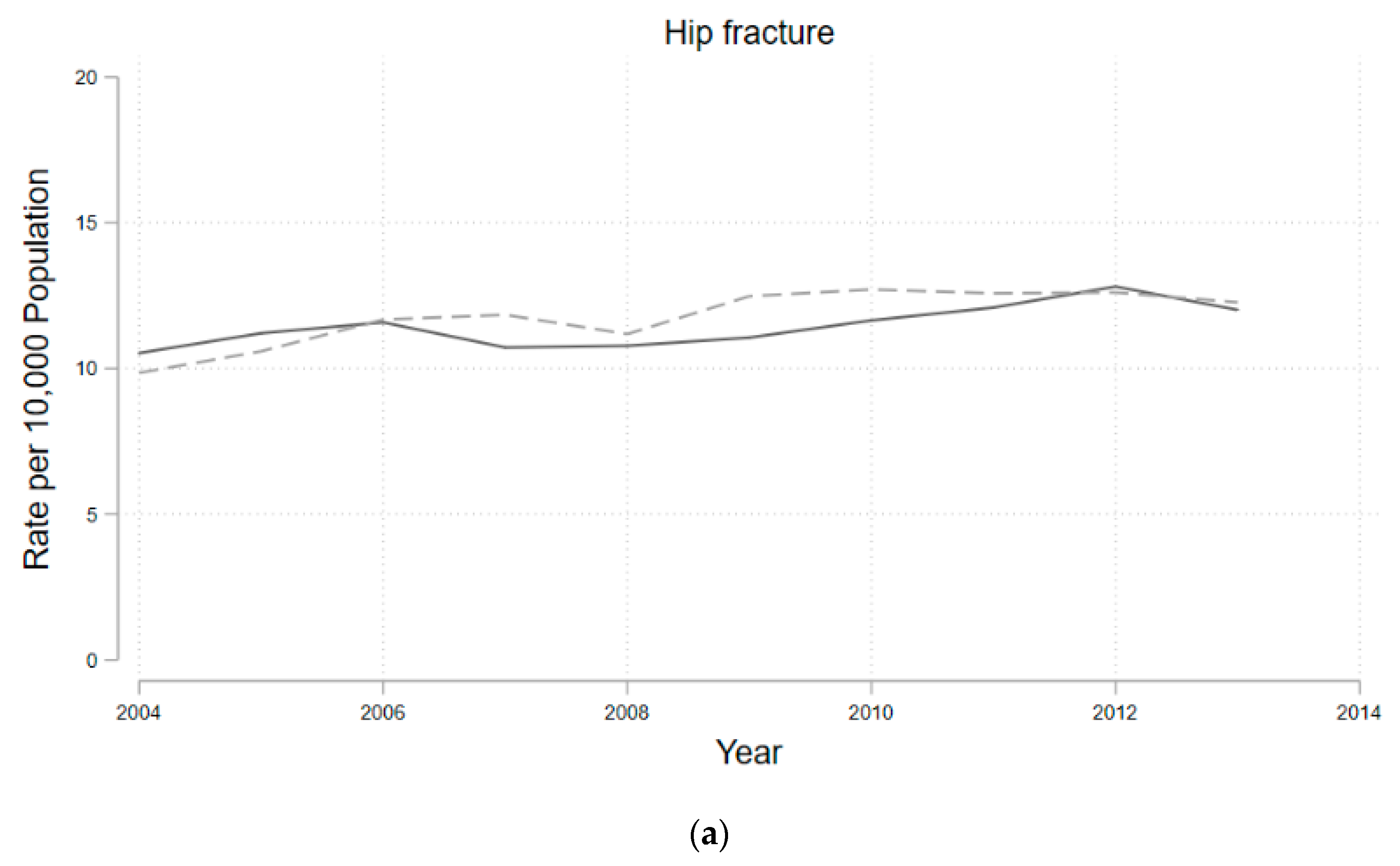
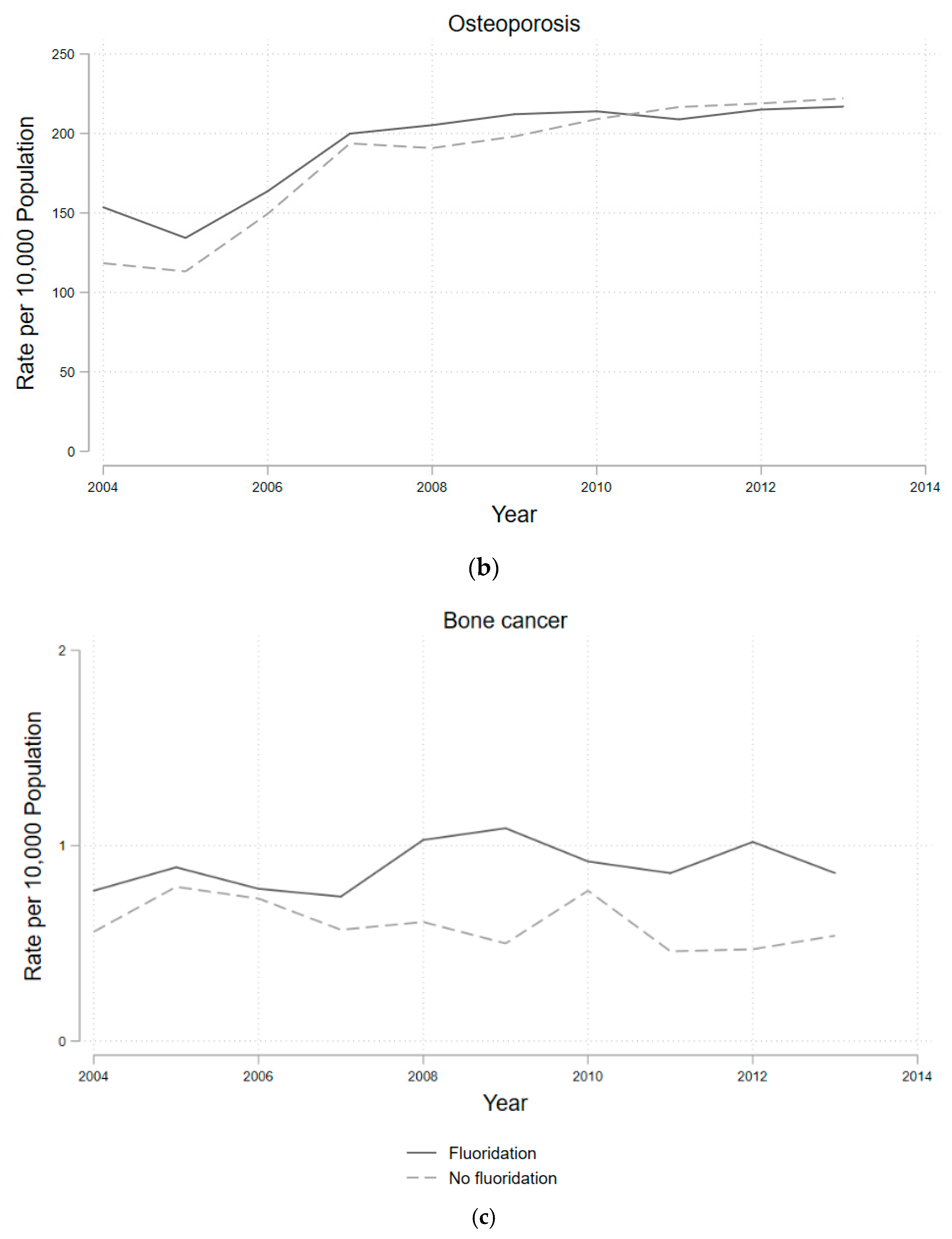
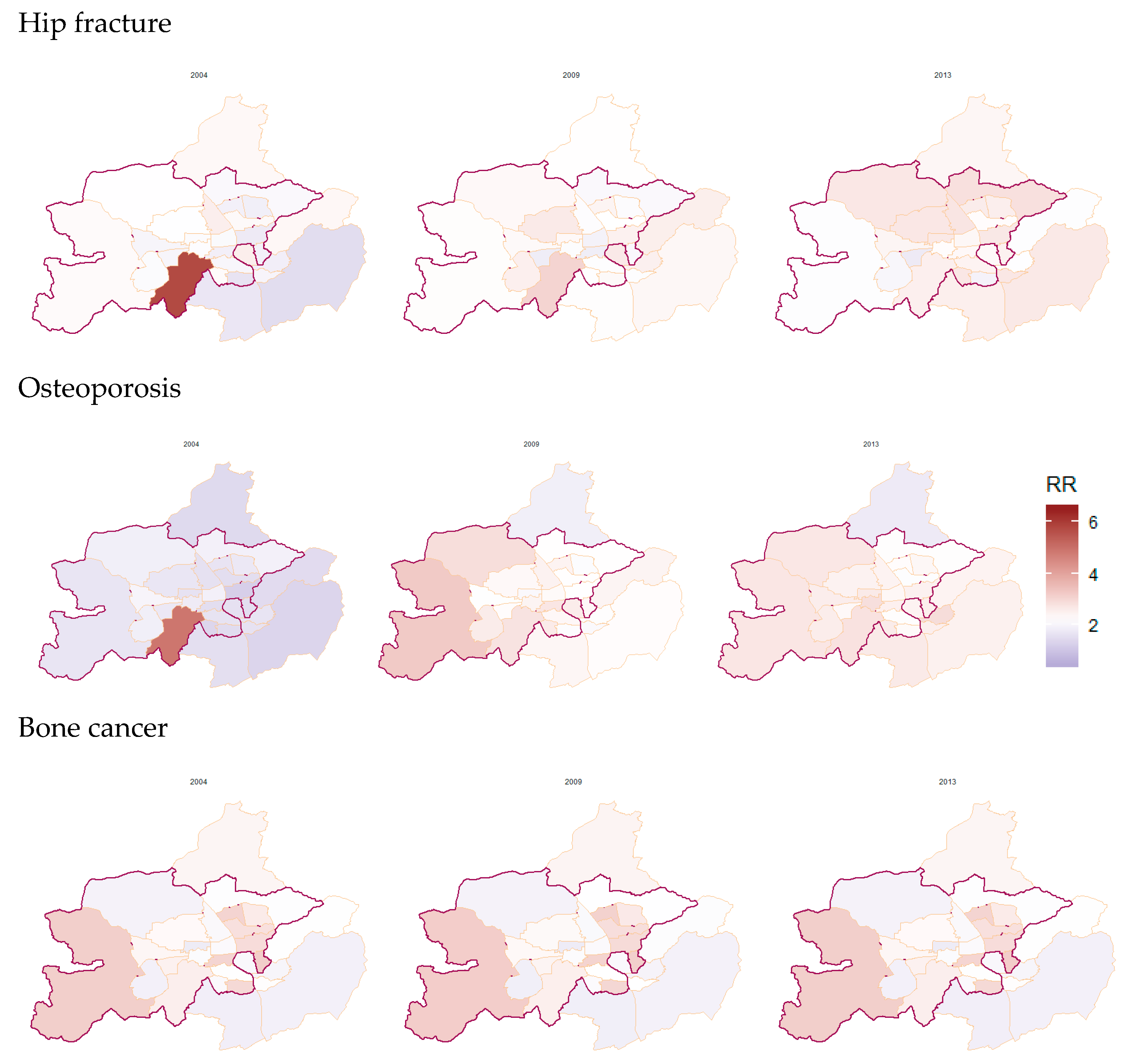
4. Results
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Community Water Fluoridation. Available online: https://www.cdc.gov/fluoridation/index.html (accessed on 10 March 2020).
- Ran, T.; Chattopadhyay, S.K. Community Preventive Services Task Force. Economic evaluation of community water fluoridation: A community guide systematic review. Am. J. Prev. Med. 2016, 50, 790–796. [Google Scholar] [CrossRef]
- Griffin, S.O.; Regnier, E.; Griffin, P.M.; Huntley, V. Effectiveness of fluoride in preventing caries in adults. J. Dent. Res. 2007, 86, 410–415. [Google Scholar] [CrossRef]
- Armfield, J.M. When public action undermines public health: A critical examination of antifluoridationist literature. Aust. N. Z. Health Policy 2007, 4. [Google Scholar] [CrossRef]
- Kim, H.N.; Kim, J.H.; Kim, S.Y.; Kim, J.B. Associations of Community Water Fluoridation with Caries Prevalence and Oral Health Inequality in Children. Int. J. Environ. Res. Public Health 2017, 14, 631. [Google Scholar] [CrossRef]
- Aoun, A.; Darwiche, F.; Al Hayek, S.; Doumit, J. The Fluoride Debate: The Pros and Cons of Fluoridation. Prev. Nutr. Food Sci. 2018, 23, 171–180. [Google Scholar] [CrossRef]
- Thornton-Evans, G.; Junger, M.L.; Lin, M.; Wei, L.; Espinoza, L.; Beltran-Aguilar, E. Use of toothpaste and toothbrushing patterns among children and adolescents—The United States, 2013–2016. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Osterman, J.W. Evaluating the impact of municipal water fluoridation on the aquatic environment. Am. J. Public Health 1990, 80, 1230–1235. [Google Scholar] [CrossRef]
- McDonagh, M.S.; Whiting, P.F.; Wilson, P.M.; Sutton, A.J.; Chestnutt, I.; Cooper, J.; Misso, K.; Bradley, M.; Treasure, E.; Kleijnen, J. Systematic review of water fluoridation. BMJ 2000, 321, 855–859. [Google Scholar] [CrossRef]
- Morabia, A. Community water fluoridation: Open discussions strengthen public health. Am. J. Public Health 2016, 106, 209–210. [Google Scholar] [CrossRef]
- Korea Health Promotion Institution. A Community Health Promotion Programme Report Dental Health. 2003. Available online: https://www.khealth.or.kr/kps (accessed on 7 December 2019).
- Cho, H.J.; Jin, B.H.; Park, D.Y.; Jung, S.H.; Lee, H.S.; Paik, D.I.; Bae, K.H. Systemic effect of water fluoridation on dental caries prevalence. Commun. Dent. Oral Epidemiol. 2014, 42, 341–348. [Google Scholar] [CrossRef]
- Kim, M.J.; Kim, H.N.; Jun, E.J.; Ha, J.E.; Han, D.H.; Kim, J.B. Association between estimated fluoride intake and dental caries prevalence among 5-year-old children in Korea. BMC Oral Health 2015, 15, 169. [Google Scholar] [CrossRef][Green Version]
- Han, S.J.; Kwon, Y.B.; Kim, S.Y.; Kim, J.S.; Lee, J.H.; Kim, J.B. Factors related to the difference in the incidence of caries between children in fluoridated and non-fluoridated areas. J. Korean Acad. Oral Health 2018, 42, 136–144. [Google Scholar] [CrossRef]
- Ok, T.Y.; Kwon, Y.B.; Kim, J.S.; Kim, S.Y.; Lee, J.H.; Kim, H.N.; Kim, J.B. Caries reduction effect of permanent teeth from community water fluoridation program for 17 years in Jinju city. J. Korean Acad. Oral Health 2019, 43, 63–71. [Google Scholar] [CrossRef]
- Green, R.; Lanphear, B.; Hornung, R.; Flora, D.; Martinez-Mier, E.A.; Neufeld, R.; Ayotte, P.; Muckle, G.; Till, C. Association between maternal fluoride exposure during pregnancy and IQ scores in offspring in Canada. JAMA Pediatr. 2019, 173, 940–948. [Google Scholar] [CrossRef]
- Till, C.; Green, R.; Flora, D.; Hornung, R.; Martinez-Mier, E.A.; Blazer, M.; Farmus, L.; Ayotte, P.; Muckle, G.; Lanphear, B. Fluoride exposure from infant formula and child IQ in a Canadian birth cohort. Environ. Int. 2020, 134, 105315. [Google Scholar] [CrossRef]
- Riddell, J.K.; Malin, A.J.; Flora, D.; McCague, H.; Till, C. Association of water fluoride and urinary fluoride concentrations with attention deficit hyperactivity disorder in Canadian youth. Environ. Int. 2019, 133, 105190. [Google Scholar] [CrossRef]
- Park, E.Y.; Hwang, S.S.; Kim, J.Y.; Cho, S.H. Effects of Long-term Fluoride in Drinking Water on Risks of Hip Fracture of the Elderly: An Ecologic Study Based on Database of Hospitalization Episodes. J. Prev. Med. Public Health 2008, 41, 147–152. [Google Scholar] [CrossRef]
- Han, Y.J.; Min, J.Y.; Han, D.H.; Kim, H.D.; Paek, D.M. The Effect of Adjusted Water Fluoridation on Bone Mineral Density. Korean J. Environ. Health Sci. 2008, 34, 261–270. [Google Scholar] [CrossRef]
- Ryu, D.R. Introduction to the medical research using national health insurance claims database. Ewha Med. J. 2017, 40, 66–70. [Google Scholar] [CrossRef]
- Kim, L.; Sakong, J.; Kim, Y.; Kim, S.; Kim, S.; Tchoe, B.; Jeong, H.; Lee, T. Developing the inpatient sample for the National Health Insurance claims data. Health Policy Manag. 2013, 23, 152–161. [Google Scholar] [CrossRef]
- Knorr-Held, L. Bayesian modelling of inseparable space-time variation in disease risk. Stat. Med. 2000, 19, 2555–2567. [Google Scholar] [CrossRef]
- Lee, D.; Rushworth, A.; Napier, G. Spatio-temporal areal unit modelling in R with conditional autoregressive priors using the CARBayesST package. J. Stat. Softw. 2018, 84. [Google Scholar] [CrossRef]
- Anderson, C.; Ryan, L. A comparison of Spatio-temporal disease mapping approaches including an application to ischaemic heart disease in New South Wales, Australia. Int. J. Environ. Res. Public Health 2017, 14, 146. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.H.; Huang, G.L.; Lin, D.R.; Wan, C.C.; Wang, Y.D.; Song, J.K.; Xu, P. Exposure to fluoride in drinking water and hip fracture risk: A meta-analysis of observational studies. PLoS ONE 2015, 10, e0126488. [Google Scholar] [CrossRef]
- Phipps, K.R.; Orwoll, E.S.; Mason, J.D.; Cauley, J.A. Community water fluoridation, bone mineral density, and fractures: Prospective study of effects in older women. BMJ 2000, 321, 860–864. [Google Scholar] [CrossRef]
- O’Sullivan, V.; O’Connell, B.C. Water fluoridation, dentition status and bone health of older people in Ireland. Commun. Dent. Oral Epidemiol. 2015, 43, 58–67. [Google Scholar] [CrossRef]
- Public Health. Water Fluoridation: Health Monitoring Report for England. 2018. Available online: https://www.gov.uk/government/publications/water-fluoridation-health-monitoring-report-for-england22 (accessed on 18 February 2020).
- Kelsey, J.L. Risk factors for osteoporosis and associated fractures. Public Health Rep. 1989, 104, 14. [Google Scholar]
- Tuck, S.P.; Datta, H.K. Osteoporosis in the aging male: Treatment options. Clin. Interv. Aging 2007, 2, 521. [Google Scholar] [CrossRef][Green Version]
- Khosla, S.; Melton, L.J., III; Atkinson, E.J.; O’fallon, W.M.; Klee, G.G.; Riggs, B.L. Relationship of serum sex steroid levels and bone turnover markers with bone mineral density in men and women: A key role for bioavailable estrogen. J. Clin. Endocrinol. Metab. 1998, 83, 2266–2274. [Google Scholar]
- Peres, M.A.; Peres, K.G.; Barbato, P.R.; Höfelmann, D.A. Access to fluoridated water and adult dental caries: A natural experiment. J. Dent. Res. 2016, 95, 868–874. [Google Scholar] [CrossRef]
- Berry, S.D.; Zullo, A.R.; McConeghy, K.; Lee, Y.; Daiello, L.; Kiel, D.P. Defining hip fracture with claims data: Outpatient and provider claims matter. Osteoporos. Int. 2017, 28, 2233–2237. [Google Scholar] [CrossRef] [PubMed]
| Variables | CWF | Non-CWF | ||
|---|---|---|---|---|
| No. of Residents | % | No. of Residents | % | |
| Total | 4,406,021 | 2,270,959 | ||
| Gender | ||||
| Male | 2,200,104 | 49.9 | 1,126,495 | 49.6 |
| Female | 2,205,917 | 50.1 | 1,144,464 | 50.4 |
| Age (years) | ||||
| <20 | 1,135,966 | 25.8 | 603,984 | 26.6 |
| 20–39 | 1,473,753 | 33.4 | 650,749 | 28.7 |
| 40–59 | 1,292,255 | 29.3 | 813,074 | 35.8 |
| 60–79 | 445,321 | 10.1 | 177,593 | 7.8 |
| ≥80 | 58,726 | 1.33 | 25,559 | 1.13 |
| Population density (people per km2) | 5.1 | 3.4 | ||
| Number of towns (N) | 21 | 9 | ||
| Education level * | ||||
| Middle school or lower | 1689 | 36.8 | 2541 | 34.9 |
| High school | 1433 | 31.2 | 2140 | 29.4 |
| College or higher | 1469 | 32.0 | 2607 | 35.8 |
| Period of residence * | ||||
| >1 year | 324 | 23.5 | 691 | 34.1 |
| 1–5 years | 493 | 35.8 | 1002 | 49.4 |
| 5–10 years | 397 | 28.9 | 462 | 22.8 |
| 10–25 years | 362 | 26.3 | 461 | 22.7 |
| ≥25 years | 124 | 9.01 | 104 | 5.13 |
| Source of water * | ||||
| Community water system | 4363 | 98.8 | 2681 | 98.6 |
| Village water (temporal) | 6 | 0.14 | 0 | 0.00 |
| None | 49 | 1.11 | 39 | 1.43 |
| Types of drinking water | ||||
| Drinking tap water | 812 | 47.8 | 1237 | 45.5 |
| Purified tap water | 524 | 30.9 | 860 | 31.6 |
| Bottled water | 238 | 14.0 | 427 | 15.7 |
| Others | 124,691 | 7.30 | 196 | 7.21 |
| Total | Male | Female | |
|---|---|---|---|
| RR * (95% CrI **) | |||
| Hip Fracture | 0.95 (0.87–1.05) | 0.88 (0.75–1.01) | 0.99 (0.89–1.09) |
| Osteoporosis | 0.94 (0.87–1.02) | 0.86 (0.76–0.97) | 0.95 (0.87–1.03) |
| Bone Cancer | 1.20 (0.89–1.61) | 1.26 (0.84–1.88) | 1.03 (0.87–1.22) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, N.; Kang, S.; Lee, W.; Hwang, S.-s. The Association between Community Water Fluoridation and Bone Diseases: A Natural Experiment in Cheongju, Korea. Int. J. Environ. Res. Public Health 2020, 17, 9170. https://doi.org/10.3390/ijerph17249170
Lee N, Kang S, Lee W, Hwang S-s. The Association between Community Water Fluoridation and Bone Diseases: A Natural Experiment in Cheongju, Korea. International Journal of Environmental Research and Public Health. 2020; 17(24):9170. https://doi.org/10.3390/ijerph17249170
Chicago/Turabian StyleLee, Naae, Sungchan Kang, Woojoo Lee, and Seung-sik Hwang. 2020. "The Association between Community Water Fluoridation and Bone Diseases: A Natural Experiment in Cheongju, Korea" International Journal of Environmental Research and Public Health 17, no. 24: 9170. https://doi.org/10.3390/ijerph17249170
APA StyleLee, N., Kang, S., Lee, W., & Hwang, S.-s. (2020). The Association between Community Water Fluoridation and Bone Diseases: A Natural Experiment in Cheongju, Korea. International Journal of Environmental Research and Public Health, 17(24), 9170. https://doi.org/10.3390/ijerph17249170





