“RA.DI.CA.” Splint for the Management of the Mandibular Functional Limitation: A Retrospective Study on Patients with Anterior Disc Displacement without Reduction
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
- Sociodemographic factors: gender, age, marital status, and occupation.
- Occlusion: occlusal and skeletal class, dental formula, occlusal abnormalities, incisal guide, loss of teeth and parafunctions. These parameters were collected on the basis of the clinical examination and upon standard lateral radiograph and dental orthopantomography.
- Medical History: previous trauma, previous click, and beginning of symptoms.
- Types of pain: temporomandibular pain (arthralgia/muscle pain), headache, familiar pain, neck pain, and emotional strain, according to verbal numeric scale (VNS) before (T0) and after treatment—i.e., the end of the joint rehabilitation—(T1) and during the follow-up—i.e., patient monitoring after completion of therapy—(T2).
- Functional aspects: maximum mouth opening and lateral excursions, expressed in mm before (T0) and after treatment (T1) and during the follow-up (T2).
- Hours per day of splint application and duration of therapy.
- Number of days necessary to resolution of closed-lock and degree of resolution.
- Presence of click after the treatment and perception of any occlusal change.
2.2. Sample Calculation
2.3. Data Collection
- T1
- H:
- healed, no sign, no symptom.
- I:
- improved, absence of initial dysfunctional signs and symptoms with occasional presence of slight symptomatology and no symptoms worsened.
- S:
- stationary, no change, neither improvement or worsening, of the previous state.
- W:
- worsened, at least one symptom or one sign worsened and none improved.
- T2
- H:
- healed,complete disappearance of the symptomatology present at T1.
- I:
- improved, disappearance of at least one sign or symptom present at T1.
- S:
- stationary, no change, neither improvement or worsening, of the previous state.
- W:
- worsened, worsening of at least one symptom compared to T1.
2.4. Statistical Analysis
2.5. Functional Characteristics of RA.DI.CA
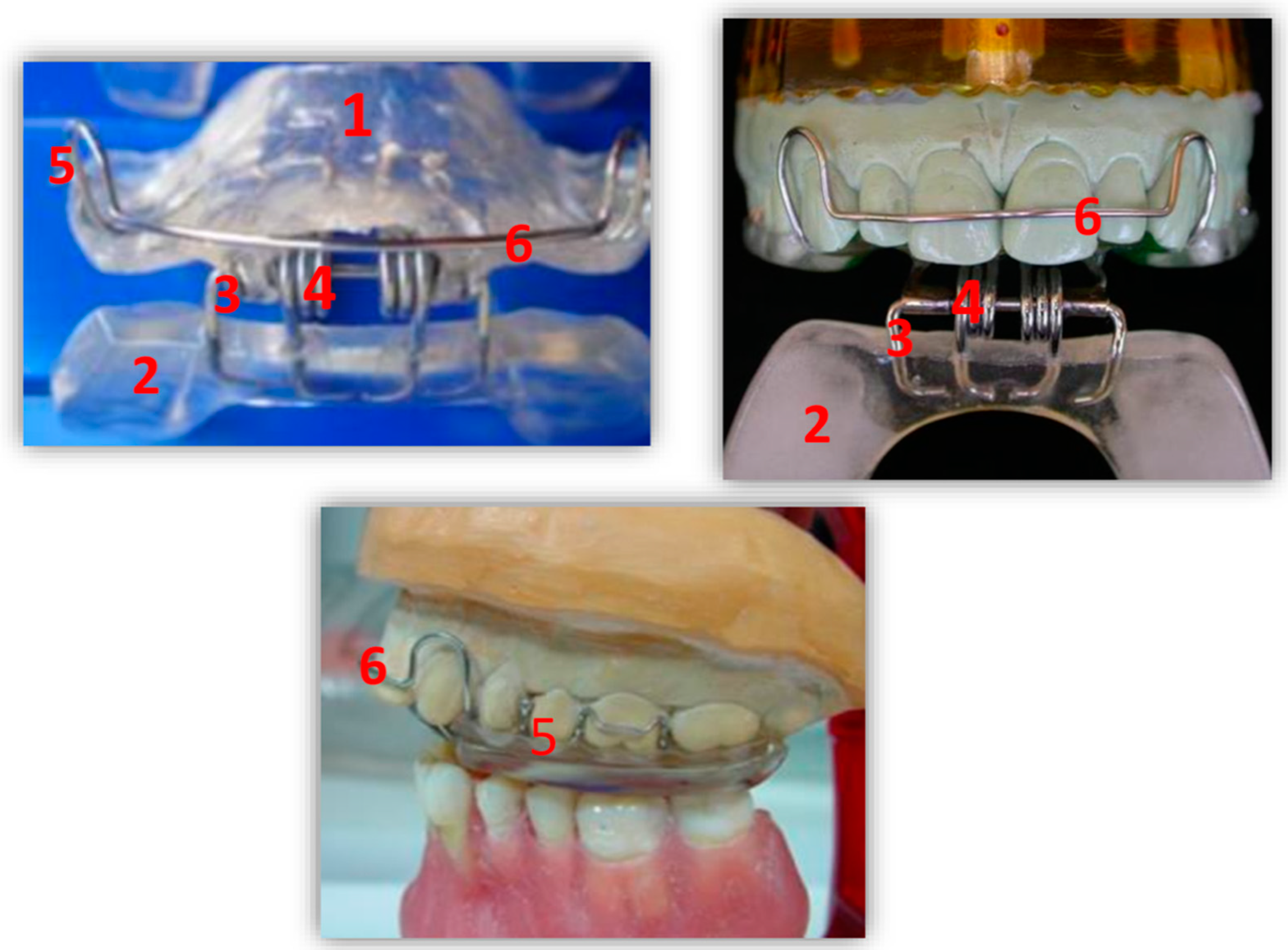
2.5.1. Design
- A heat-cured acrylic resin upper plate (1),
- A heat-cured acrylic resin lower plate (2),
- An anterior hinge (3),
- Two vestibular springs made with orthodontic wire (4),
- Two or more Adams clasps and/or two ball clasps (5),
- A vestibular steel arch (6).
2.5.2. Application Protocol of RA.DI.CA Splint
3. Results
3.1. T0–Baseline
3.2. T1—After Treatment
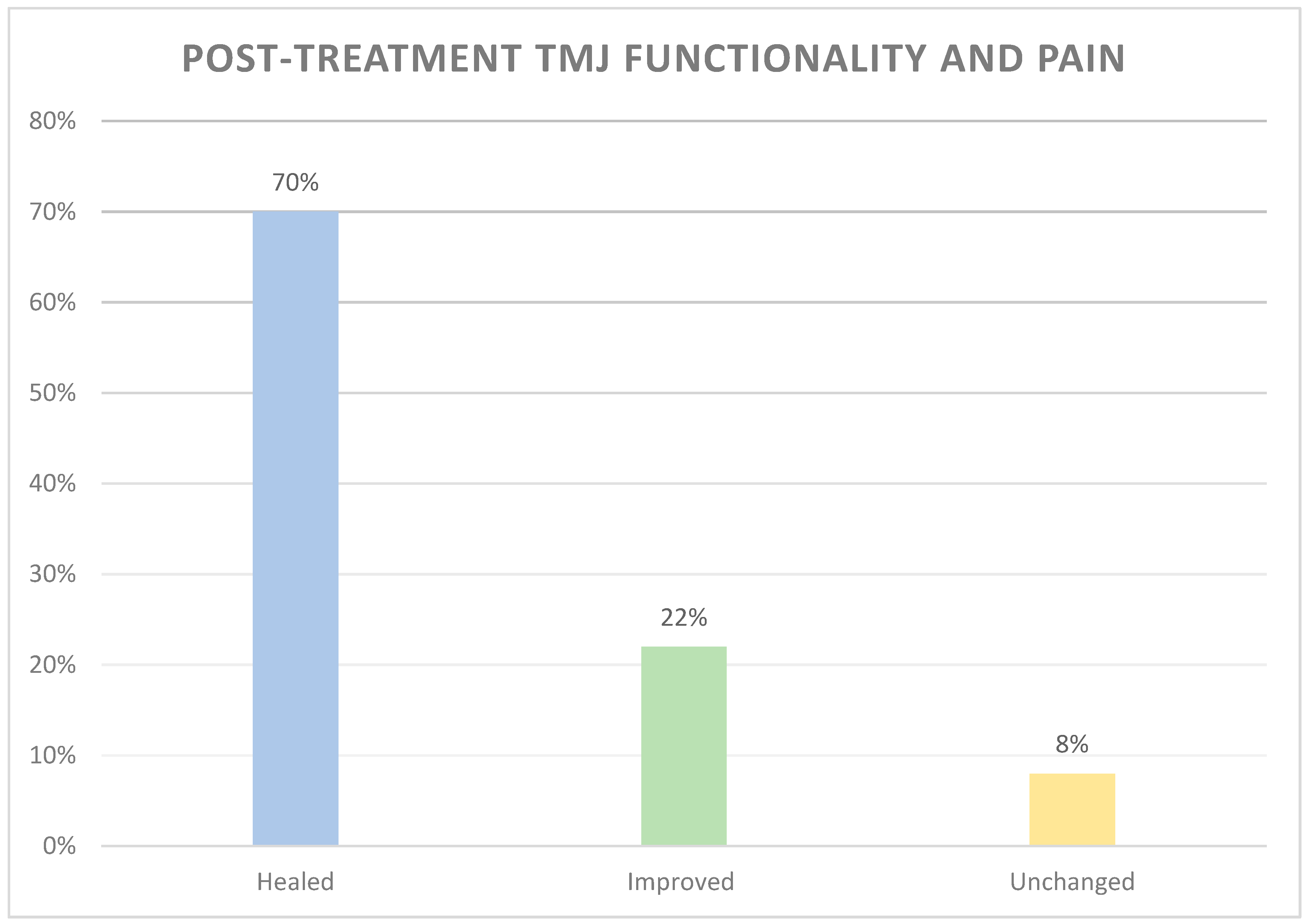
3.2.1. Effectiveness of RADICA Splint Therapy
3.2.2. Efficiency of RADICA Splint Therapy (Duration of Therapy)
- -
- 10 patients (23.8%) gained a complete condyle-disc ratio.
- -
- 19 patients (45.2%) gained a partial condyle-disc ratio.
- -
- 13 patients (30.9%) did not gain the condyle-disc ratio.
3.3. T2–Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Data Availability
References
- Cooper, B.C.; Kleinberg, I. Examination of a large patient population for the presence of symptoms and signs of temporomandibular disorders. CRANIO® 2007, 25, 114–126. [Google Scholar] [CrossRef] [PubMed]
- Miernik, M.; Więckiewicz, W. The Basic Conservative Treatment of Temporomandibular Joint Anterior Disc Displacement Without Reduction—Review. Adv. Clin. Exp. Med. 2015, 24, 731–735. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, S.F.; LeResche, L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J. Craniomandib. Disord. 1992, 6, 301–355. [Google Scholar] [PubMed]
- Di Paolo, C.; Rampello, A. Lock intrarticolare dell’ATM. Terapia non chirurgica. Dent. Cadmos 1993, 18, 48–74. [Google Scholar]
- Cascone, P.; Di Paolo, C. Patologia dell’Articolazione Temporomandibolare; Dall’eziopatogenesi alla terapia, Ed.; UTET: Torino, Italy, 2004; pp. 31–181. [Google Scholar]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- McNeill, C. Craniomandibular Disorders Guidelines for Evaluation Diagnosis and Management: The American Academy of Craniomandibular Disorders, 2nd ed.; Quintessence Publishing Co. Inc.: Chicago, IL, USA, 1990. [Google Scholar]
- Yura, S. Natural course of acute closed lock of the temporomandibular joint. Br. J. Oral Maxillofac. Surg. 2012, 50, 646–649. [Google Scholar] [CrossRef]
- Dimitroulis, G. The prevalence of osteoarthrosis in cases of advanced internal derangement of the Temporomandibular Joint: A clinical, surgical and histological study. Int. J. Oral Maxillofac. Surg. 2005, 34, 345–349. [Google Scholar] [CrossRef]
- Stiesch-Scholz, M.; Tschernitschek, H.; Rossbach, A. Early begin of splint therapy improves treatment outcome in patients with temporomandibular joint disc displacement without reduction. Clin. Oral Investig. 2002, 6, 119–123. [Google Scholar] [CrossRef]
- Schmitter, M.; Zahran, M.; Duc, J.-M.; Henschel, V.; Rammelsberg, P. Conservative Therapy in Patients with Anterior Disc Displacement without Reduction Using 2 Common Splints: A Randomized Clinical Trial. J. Oral Maxillofac. Surg. 2005, 63, 1295–1303. [Google Scholar] [CrossRef]
- Zotti, F.; Albanese, M.; Rodella, L.F.; Nocini, P.F. Platelet-Rich Plasma in Treatment of Temporomandibular Joint Dysfunctions: Narrative Review. Int. J. Mol. Sci. 2019, 20, 277. [Google Scholar] [CrossRef]
- Al-Delayme, R.M.A.; Alnuamy, S.H.; Hamid, F.T.; Azzamily, T.J.; Ismaeel, S.A.; Sammir, R.; Hadeel, M.; Nabeel, J.; Shwan, R.; Alfalahi, S.J.; et al. The Efficacy of Platelets Rich Plasma Injection in the Superior Joint Space of the Temporomandibular Joint Guided by Ultra Sound in Patients with Non-reducing Disk Displacement. J. Maxillofac. Oral Surg. 2017, 16, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Kurina, H.; Kurashina, K.; Ohtsuka, A. Efficacy of mandibular manipulation technique in reducing the permanently displaced temporomandibular joint disc. J. Oral Maxillofac. Surg. 1999, 57, 784–787. [Google Scholar]
- Dimitroulis, G. Management of temporomandibular joint disorders: A surgeon’s perspective. Aust. Dent. J. 2018, 63, S79–S90. [Google Scholar] [CrossRef] [PubMed]
- Haketa, T.; Kino, K.; Sugisaki, M.; Takaoka, M.; Ohta, T. Randomized Clinical Trial of Treatment for TMJ Disc Displacement. J. Dent. Res. 2010, 89, 1259–1263. [Google Scholar] [CrossRef]
- Shoji, Y.N. Nonsurgical treatment of anterior disk displacement of the temporomandibular joint: A case report on the relationship between condylar rotation and translation. CRANIO® 1995, 13, 270–273. [Google Scholar] [CrossRef]
- Meshkova, D.T.; Di Giacomo, P.; Panti, F.; D’Urso, A.; Serritella, E.; Di Paolo, C. Application of a Systematic Protocol in the Treatment of TMDs with Occlusal Appliances: Effectiveness and Efficiency in a Longitudinal Retrospective Study with Medium-Term Follow-Up. J. Int. Soc. Prev. Community Dent. 2019, 9, 372–382. [Google Scholar]
- Di Paolo, C.; Accivile, E.; Chimenti, C.; Carbonelli, A. Electrognathography: Diagnostic adjunct in the treatment of closed-lock joint. Dent. Cadmos 1987, 55, 67–72. [Google Scholar]
- Di Paolo, C.; Liberatore, G.M.; Rampello, A.; Panti, F. A longitudinal analysis of dysfunctional pathology of the TMJ: An assessment of a sample of patients undergoing nonsurgical therapy. Minerva Stomatol. 1994, 43, 565. [Google Scholar]
- De Boever, J.A.; Carlsson, G.E.; Klineberg, I.J. Review—Need for occlusal therapy and prosthodontic treatment in the management of temporomandibular disorders, Part II, Tooth loss and prosthodontic treatment. J. Oral Rehabil. 2000, 27, 647–659. [Google Scholar] [CrossRef]
- Di Paolo, C.; Cascone, P. Ruolo dei fattori occlusali nell’eziopatogenesi dei DTM—Considerazioni clinico-statistiche. Dent. Cadmos 1998, 17, 31–35. [Google Scholar]
- Gotou, M.; Nagata, K.; Sugawara, Y. Short-term effectiveness of the Jog- manipulation technique for temporomandibular disorders (TMD)patients with limited mouth opening—A randomized controlled trial. J. Jpn. Soc. TMJ 2010, 22, 84–91. [Google Scholar]
- Tuncer, A.B.; Ergun, N.; Tuncer, A.H.; Karahan, S. Effectiveness of manual therapy and home physical therapy in patients with temporomandibular disorders: A randomized controlled trial. J. Bodyw. Mov. Ther. 2013, 17, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, H.; Fukumura, Y.; Suzuki, S.; Fujita, S.; Kenzo, O.; Yoshikado, R.; Nakagawa, M.; Inoue, A.; Sako, J.; Yamada, K.; et al. Simple Manipulation Therapy for Temporomandibular joint Internal Derangement with Closed Lock. Asian J. Oral Maxillofac. Surg. 2005, 17, 256–260. [Google Scholar] [CrossRef]
- Lee, H.S.; Baek, H.S.; Song, D.S.; Kim, H.C.; Kim, H.G.; Kim, B.J.; Kim, M.S.; Shin, S.H.; Jung, S.H.; Kim, C.H. Effect of simultaneous therapy of arthrocentesis and occlusal splints on temporomandibular disorders: Anterior disc displacement without reduction. J. Korean Assoc. Oral Maxillofac. Surg. 2013, 39, 14–20. [Google Scholar] [CrossRef]
- Kai, S.; Kai, H.; Tabata, O.; Shiratsuchi, Y.; Ohishi, M. Long-term outcomes of nonsurgical treatment in nonreducing anteriorly displaced disk of the temporomandibular joint. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1998, 85, 258–267. [Google Scholar] [CrossRef]
- Sears, V.H. Occlusal pivots. J. Prosthet. Dent. 1956, 6, 332–336. [Google Scholar] [CrossRef]
- Moncayo, S. Biomechanics of pivoting appliances. J. Orofac. Pain 1994, 8, 190–196. [Google Scholar]
- Muhtarogullari, M.; Avci, M.; Yuzugullu, B. Efficiency of pivot splints as jaw exercise apparatus in combination with stabilization splints in anterior disc displacement without reduction: A retrospective study. Head Face Med. 2014, 9, 10–42. [Google Scholar] [CrossRef]
- Stiesch-Scholz, M.; Kempert, J.; Wolter, S.; Tschernitschek, H.; Rossbach, A. Comparative study on splint therapy of anterior disc displacement without reduction. J. Oral Rehabil. 2005, 32, 474–479. [Google Scholar] [CrossRef]
- Ohnuki, T.; Fukuda, M.; Nakata, A.; Nagai, H.; Takahashi, T.; Sasano, T.; Miyamoto, Y. Evaluation of the position, mobility, and morphology of the disc by MRI before and after four different treatments for temporomandibular joint disorders. Dentomaxillofac. Radiol. 2006, 35, 103–109. [Google Scholar] [CrossRef]
- Lundh, H.; Westesson, P.L.; Eriksson, L.; Brooks, S.L. Temporomandibular joint disk displacement without reduction. Oral Surg. Oral Med. Oral Pathol. 1992, 73, 655–658. [Google Scholar] [CrossRef]
- Rocabado, M. Joint distraction with a functional maxillomandibular orthopedic appliance. J. Craniomandib. Pract. 1984, 2, 358–363. [Google Scholar] [CrossRef] [PubMed]
- Festa, F. Joint distraction and condyle advancement with a modified functional distraction appliance. CRANIO® 1985, 3, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Festa, F. Modified functional distraction appliance an appliance for chronic lock and ankylosis. CRANIO® 1995, 13, 137–138. [Google Scholar] [CrossRef]
- Eberhard, D.; Bantleon, H.P.; Steger, W. The efficacy of anterior repositioning splint therapy studied by magnetic resonance imaging. Eur. J. Orthod. 2002, 24, 343–352. [Google Scholar] [CrossRef]
- Simmons, H.C.; Gibbs, S.J. Recapture of temporomandibular joint disks using anterior repositioning appliances: An MRI study. CRANIO® 1995, 13, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Craane, B.; Dijkstra, P.U.; Stappaerts, K.; De Laat, A. Randomized controlled trial on physical therapy for TMJ closed lock. J. Dent. Res. 2012, 91, 364–369. [Google Scholar] [CrossRef]
- Nagata, K.; Hori, S.; Mizuhashi, R.; Yokoe, T.; Atsumi, Y.; Wataru, N.; Goto, M. Efficacy of mandibular manipulation technique for temporomandibular disorders patients with mouth opening limitation: A randomized controlled trial for comparison with improved multimodal therapy. J. Prosthodont. Res. 2019, 63, 202–209. [Google Scholar] [CrossRef]
- Choi, B.H.; Yoo, J.H.; Lee, W.Y.; Do, K. Comparison of magnetic resonance imaging before and after nonsurgical treatment of closed lock. Oral Surg. Oral Med. Oral Pathol. 1994, 78, 301. [Google Scholar] [CrossRef]
- Kirk, W. Magnetic resonance imaging and tomographic evaluation of occlusal appliance treatment for advanced internal derangement of the temporomandibular joint. J. Oral Maxillofac. Surg. 1991, 49, 9–12. [Google Scholar] [CrossRef]
- McNeill, C. The optimum temporomandibular joint condyle position in clinical practice. Int. J. Periodont. Restor. Dent. 1985, 5, 71–72. [Google Scholar]
- Al-Baghdadi, M.; Durham, J.; Araujo-Soares, V.; Robalino, S.; Errington, L.; Steele, J. TMJ disc displacement without reduction management: A systematic review. J. Dent. Res. 2014, 93, 37S–51S. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Before Treatment (Mean ± SD) | Before Treatment (Median) | After Treatment T1 (Mean ± SD) | After Treatment T1 (Median) | Wilcoxon Test (W) | Z Test Value | p Value |
|---|---|---|---|---|---|---|---|
| Joint pain | 63 ± 10.67 | 63 | 8.32 ± 13.12 | 6 | 8385 | 8.72 | <0.0001 |
| Neck pain | 59.67 ± 13.52 | 61 | 20.09 ± 21.10 | 15 | 3741 | 7.40 | <0.0001 |
| Headache | 60.40 ± 16.54 | 62 | 13.3 ± 20.63 | 0 | 5565 | 8.89 | <0.0001 |
| Mouth opening | 30.27 ± 4.45 | 30 | 41.44 ± 5.44 | 40 | 9870 | 10.26 | <0.0001 |
| Study Variable | Average Time of Recovery (in Months) |
|---|---|
| Jaw Limitation | 3.8 ± 1.2 |
| Tmd Pain | 6.4 ± 1.7 |
| Neck Pain | 8.1 ± 1.8 |
| Headache | 9.6 ± 2.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Paolo, C.; Falisi, G.; Panti, F.; Di Giacomo, P.; Rampello, A. “RA.DI.CA.” Splint for the Management of the Mandibular Functional Limitation: A Retrospective Study on Patients with Anterior Disc Displacement without Reduction. Int. J. Environ. Res. Public Health 2020, 17, 9057. https://doi.org/10.3390/ijerph17239057
Di Paolo C, Falisi G, Panti F, Di Giacomo P, Rampello A. “RA.DI.CA.” Splint for the Management of the Mandibular Functional Limitation: A Retrospective Study on Patients with Anterior Disc Displacement without Reduction. International Journal of Environmental Research and Public Health. 2020; 17(23):9057. https://doi.org/10.3390/ijerph17239057
Chicago/Turabian StyleDi Paolo, Carlo, Giovanni Falisi, Fabrizio Panti, Paola Di Giacomo, and Alessandro Rampello. 2020. "“RA.DI.CA.” Splint for the Management of the Mandibular Functional Limitation: A Retrospective Study on Patients with Anterior Disc Displacement without Reduction" International Journal of Environmental Research and Public Health 17, no. 23: 9057. https://doi.org/10.3390/ijerph17239057
APA StyleDi Paolo, C., Falisi, G., Panti, F., Di Giacomo, P., & Rampello, A. (2020). “RA.DI.CA.” Splint for the Management of the Mandibular Functional Limitation: A Retrospective Study on Patients with Anterior Disc Displacement without Reduction. International Journal of Environmental Research and Public Health, 17(23), 9057. https://doi.org/10.3390/ijerph17239057





