Parental Stress and Family Quality of Life: Surveying Family Members of Persons with Intellectual Disabilities
Abstract
1. Introduction
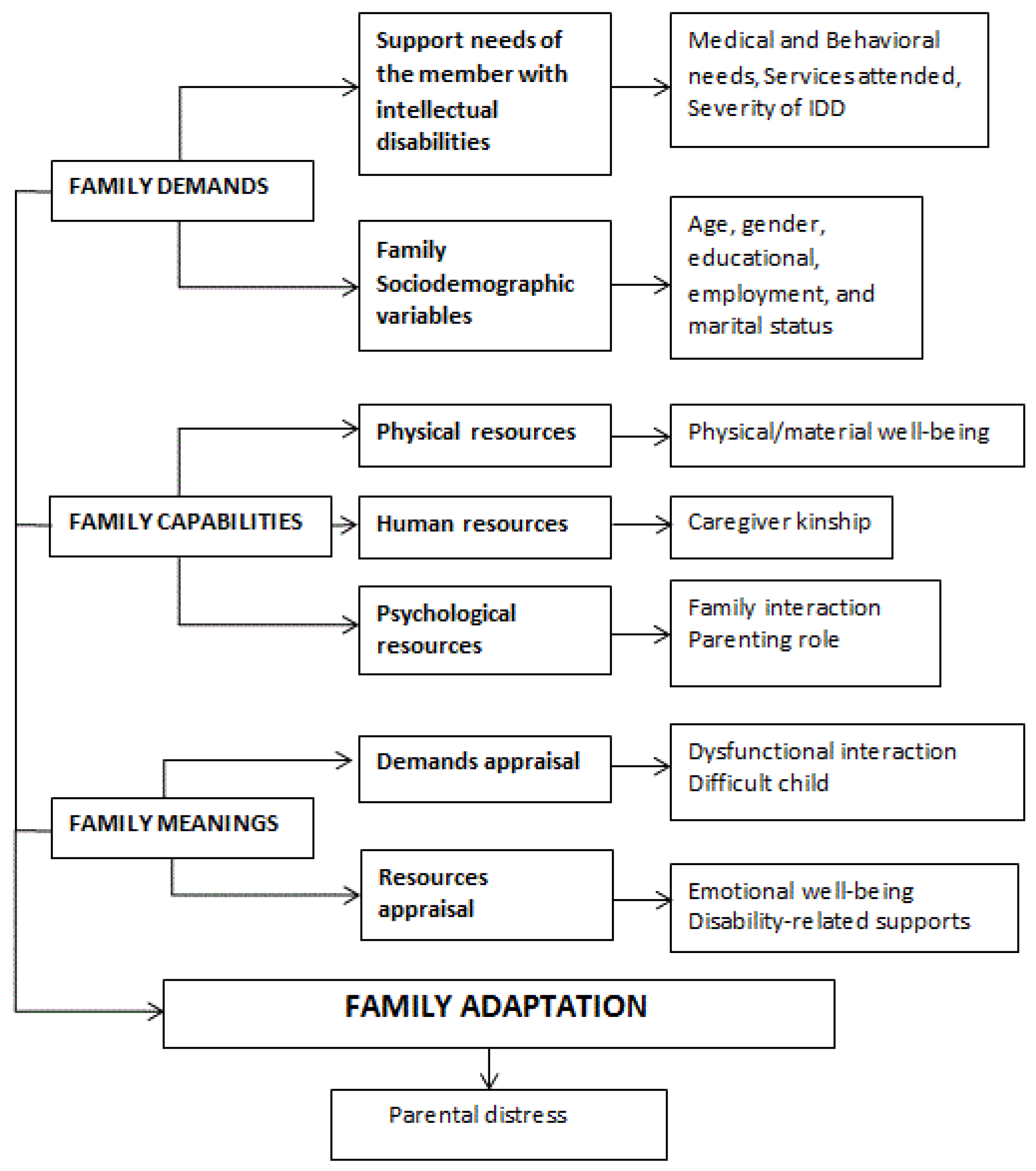
- (1)
- Family demands will contribute significantly to predict family adaptation, and there will be a negative and significant association between those variables.
- (2)
- Family capabilities, controlled for family demands, will contribute significantly to predicting family adaptation, and there will be a positive and significant association between those variables.
- (3)
- Family meanings, after controlling for demands and resources, will contribute significantly to the prediction of family adaptation, and the more positive the evaluation, the higher the family adaptation.
2. Materials and Methods
2.1. Procedure
2.2. Participants
2.3. Measures
2.4. Design and Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- John, A. Stress among mothers of children with intellectual disabilities in urban India: Role of gender and maternal coping. J. Appl. Res. Intellect. Disabil. 2012, 25, 372–382. [Google Scholar] [CrossRef]
- Peer, J.W. Coping Style as a Mediator of Stress Perception for Caregivers of Children with Developmental Disabilities. Available online: https://digitalcommons.wayne.edu/cgi/viewcontent.cgi?referer=&httpsredir=1&article=1202&context=oa_dissertations (accessed on 2 December 2020).
- Larcan, R.; Cuzzocrea, F. Funzionamento della famiglia e sviluppo psicosociale dei fratelli di individui con disabilità intellettive. (spanish adaptation from the original: Family functioning and psychosocial adjustment of siblings of children with intellectual disabilities). Psicol. Clin. Svilupp. 2011, 15, 123–153. [Google Scholar]
- Correia, R.A.; Seabra-Santos, M.J. Qualidade de vida familiar na deficiência intelectual: Revisão sistemática de estudos (spanish adaptation from the original: Family quality of life in intellectual disability: A systematic review of studies). Psicol. Teor. Pesqui. 2018, 34, e34414. [Google Scholar] [CrossRef]
- Sung, M.; Park, J. The effects of a family support program including respite care on parenting stress and family quality of life perceived by primary caregivers of children with disabilities in Korea. Int. J. Spec. Educ. 2012, 27, 188–198. [Google Scholar]
- Chou, Y.-C.; Lin, L.-C.; Chang, A.-L.; Schalock, R.L. The quality of life of family caregivers of adults with intellectual disabilities in Taiwan. J. Appl. Res. Intellect. Disabil. 2007, 20, 200–210. [Google Scholar] [CrossRef]
- Patterson, J. Integrating family resilience and family stress theory. J. Marriage Fam. 2002, 64, 349–360. [Google Scholar] [CrossRef]
- Patterson, J. Families experiencing stress: The family adjustment and adaptation response model. Fam. Syst. Med. 1988, 5, 202–237. [Google Scholar] [CrossRef]
- Patterson, J. Family resilience to the challenge of a child’s disability. Pediatr. Ann. 1991, 20, 491–499. [Google Scholar] [CrossRef]
- Rungreangkulkij, S.; Gilliss, C.L. Conceptual approaches to studying family caregiving for persons with severe mental illness. J. Fam. Nurs. 2000, 6, 341–366. [Google Scholar] [CrossRef]
- Abidin, R.R. Parenting Stress Index (PSI) Manual, 3rd ed.; Pediatric Psychology Press: Charlottesville, VA, USA, 1995. [Google Scholar]
- Bhopti, A.; Brown, T.; Lentin, P. Family quality of life: A key outcome in early childhood intervention services—A scoping review. J. Early Interv. 2016, 38, 191–211. [Google Scholar] [CrossRef]
- Beach Center on Disability. Family Quality of Life Scale; University of Kansas: Lawrence, KS, USA, 2001. [Google Scholar]
- Summers, J.A.; Poston, D.J.; Turnbull, A.P.; Marquis, J.; Hoffman, L.; Mannan, H.; Wang, M. Conceptualizing and measuring family quality of life. J. Intellect. Disabil. Res. 2005, 49, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.-Q.; Tang, C.; Zhu, S.-Y.; Liang, Y.-Y.; Zou, X.-B. Parenting stress and related factors in mothers of children with autism. Chin. Ment. Health J. 2009, 23, 629–633. [Google Scholar]
- Smith, T.B.; Oliver, M.N.I.; Innocenti, M.S. Parenting stress in families of children with disabilities. Am. J. Orthopsychiatry 2001, 71, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Cuzzocrea, F.; Larcan, R.; Westh, F. Family and parental functioning in parents of disabled children. Nord. Psychol. 2013, 65, 271–287. [Google Scholar] [CrossRef]
- Hassall, R.; Rose, J.; McDonald, J. Parenting stress in mothers of children with an intellectual disability: The effects of parental cognitions in relation to child characteristics and family support. J. Intellect. Disabil. Res. 2005, 49, 405–418. [Google Scholar] [CrossRef]
- Tobing, L.E. Stress, Coping, and Psychological Distress of Mothers of Children with Pervasive Developmental Disorders; ProQuest Information & Learning: Ann Arbor, MI, USA, 2005. [Google Scholar]
- Cain Spannagel, S.A. The Impact of Access to Services and Symptom Severity on Parenting Stress and Stress-Related Growth in Parents of Children with Autism; ProQuest Information & Learning: Ann Arbor, MI, USA, 2012. [Google Scholar]
- Mak, W.W.S.; Ho, A.H.Y.; Law, R.W. Sense of coherence, parenting attitudes and stress among mothers of children with autism in Hong Kong. J. Appl. Res. Intellect. Disabil. 2007, 20, 157–167. [Google Scholar] [CrossRef]
- Goodman, S.J. Perceptions of Parent and Child Attachment in Parents of Children with Autism Spectrum Disorders; ProQuest Information & Learning: Ann Arbor, MI, USA, 2011. [Google Scholar]
- Woolfson, L.; Grant, E. Authoritative parenting and parental stress in parents of pre-school and older children with developmental disabilities. Child. Care Health Dev. 2006, 32, 177–184. [Google Scholar] [CrossRef]
- Hung, J.W.; Wu, Y.-H.; Yeh, C.-H. Comparing stress levels of parents of children with cancer and parents of children with physical disabilities. Psycho-Oncology 2004, 13, 898–903. [Google Scholar] [CrossRef]
- Parkes, J.; Caravale, B.; Marcelli, M.; Franco, F.; Colver, A. Parenting stress and children with cerebral palsy: A European cross-sectional survey. Dev. Med. Child. Neurol. 2011, 53, 815–821. [Google Scholar] [CrossRef]
- Huang, C.-Y.; Yen, H.-C.; Tseng, M.-H.; Tung, L.-C.; Chen, Y.-D.; Chen, K.-L. Impacts of autistic behaviors, emotional and behavioral problems on parenting stress in caregivers of children with autism. J. Autism Dev. Disord. 2014, 44, 1383–1390. [Google Scholar] [CrossRef]
- Sidhu, P.; Tung, S. Stress and coping in mothers of LD children with behaviour problems and typically developing children. Indian J. Community Psychol. 2014, 10, 310–322. [Google Scholar]
- Tervo, R.C. Developmental and behavior problems predict parenting stress in young children with global delay. J. Child. Neurol. 2012, 27, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Richman, D.M.; Belmont, J.M.; Kim, M.; Slavin, C.B.; Hayner, A.K. Parenting stress in families of children with Cornelia De Lange syndrome and down syndrome. J. Dev. Phys. Disabil. 2009, 21, 537–553. [Google Scholar] [CrossRef]
- Macias, M.M.; Saylor, C.F.; Rowe, B.P.; Bell, N.L. Age-related parenting stress differences in mothers of children with spina bifida. Psychol. Rep. 2003, 93, 1223–1232. [Google Scholar] [CrossRef]
- Park, J.; Turnbull, A.P.; Turnbull, H.R., III. Impacts of poverty on quality of life in families of children with disabilities. Except. Child. 2002, 68, 151–170. [Google Scholar] [CrossRef]
- Llewellyn, G.; McConnell, D.; Gething, L.; Cant, R.; Kendig, H. Health status and coping strategies among older parent-carers of adults with intellectual disabilities in an Australian sample. Res. Dev. Disabil. 2010, 31, 1176–1186. [Google Scholar] [CrossRef]
- Giné, C.; Gràcia, M.; Vilaseca, R.; Salvador Beltran, F.; Balcells-Balcells, A.; Dalmau Montalà, M.; Luisa Adam-Alcocer, A.; Teresa Pro, M.; Simó-Pinatella, D.; Maria Mas Mestre, J. Family quality of life for people with intellectual disabilities in Catalonia. J. Policy Pract. Intellect. Disabil. 2015, 12, 244–254. [Google Scholar] [CrossRef]
- Hu, X.; Wang, M.; Fei, X. Family quality of life of Chinese families of children with intellectual disabilities. J. Intellect. Disabil. Res. 2012, 56, 30–44. [Google Scholar] [CrossRef]
- Weeks, L.E.; Nilsson, T.; Bryanton, O.; Kozma, A. Current and future concerns of older parents of sons and daughters with intellectual disabilities. J. Policy Pract. Intellect. Disabil. 2009, 6, 180–188. [Google Scholar] [CrossRef]
- Rimmerman, A.; Portowicz, D.J. Analysis of resources and stress among parents of developmentally disabled children. Int. J. Rehabil. Res. 1987, 10, 439–445. [Google Scholar] [CrossRef]
- Staunton, E.; Kehoe, C.; Sharkey, L. Families under pressure: Stress and quality of life in parents of children with an intellectual disability. Ir. J. Psychol. Med. 2020, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.; Bremer, E.; Lloyd, M. Autism spectrum disorder: Family quality of life while waiting for intervention services. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2017, 26, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Boehm, T.L.; Carter, E.W.; Taylor, J.L. Family quality of life during the transition to adulthood for individuals with intellectual disability and/or autism spectrum disorders. Am. J. Intellect. Dev. Disabil. 2015, 120, 395–411. [Google Scholar] [CrossRef] [PubMed]
- Bailey, D.B., Jr.; Nelson, L.; Hebbeler, K.; Spiker, D. Modeling the impact of formal and informal supports for young children with disabilities and their families. Pediatrics 2007, 120, e992–e1001. [Google Scholar] [CrossRef] [PubMed]
- Chou, Y.-C.; Chiao, C.; Fu, L.-Y. Health status, social support, and quality of life among family carers of adults with profound intellectual and multiple disabilities (PIMD) in Taiwan. J. Intellect. Dev. Disabil. 2011, 36, 73–79. [Google Scholar] [CrossRef]
- Ferrer, F.; Vilaseca, R.; Bersabé, R.M. The impact of demographic characteristics and the positive perceptions of parents on quality of life in families with a member with intellectual disability. J. Dev. Phys. Disabil. 2016, 28, 871–888. [Google Scholar] [CrossRef]
- Cohen, S.R.; Holloway, S.D.; Domínguez-Pareto, I.; Kuppermann, M. Receiving or believing in family support? Contributors to the life quality of Latino and non-Latino families of children with intellectual disability. J. Intellect. Disabil. Res. 2014, 58, 333–345. [Google Scholar] [CrossRef]
- Meral, B.F.; Cavkaytar, A.; Turnbull, A.P.; Mian, W. Family quality of life of Turkish families who have children with intellectual disabilities and autism. Res. Pract. Pers. Sev. Disabil. 2013, 38, 233–246. [Google Scholar] [CrossRef]
- Davis, K.; Gavidia-Payne, S. The impact of child, family, and professional support characteristics on the quality of life in families of young children with disabilities. J. Intellect. Dev. Disabil. 2009, 34, 153–162. [Google Scholar] [CrossRef]
- Lanfranchi, S.; Vianello, R. Stress, locus of control, and family cohesion and adaptability in parents of children with Down, Williams, Fragile X, Prader-Willi syndromes. Am. J. Intellect. Dev. Disabil. 2012, 117, 207–224. [Google Scholar] [CrossRef]
- Lightsey, O.R., Jr.; Sweeney, J. Meaning in life, emotion-oriented coping, generalized self-efficacy, and family cohesion as predictors of family satisfaction among mothers of children with disabilities. Fam. J. 2008, 16, 212–221. [Google Scholar] [CrossRef]
- Boyraz, G.; Sayger, T.V. Psychological well-being among fathers of children with and without disabilities: The role of family cohesion, adaptability, and paternal self-efficacy. Am. J. Men’s Health 2011, 5, 286–296. [Google Scholar] [CrossRef] [PubMed]
- Tsibidaki, A.; Tsamparli, A. Adaptability and cohesion of Greek families: Raising a child with a severe disability on the island of Rhodes. J. Fam. Stud. 2009, 15, 245–259. [Google Scholar] [CrossRef]
- Fordham, L.; Gibson, F.; Bowes, J. Information and professional support: Key factors in the provision of family-centred early childhood intervention services. Child. Care Health Dev. 2012, 38, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Jansen, S.L.G.; van der Putten, A.A.J.; Post, W.J.; Vlaskamp, C. Family-centredness of professionals who support people with profound intellectual and multiple disabilities: Validation of the Dutch ‘Measure of Processes of Care for Service Providers’ (MPOC-SP-PIMD). Res. Dev. Disabil. 2014, 35, 1623–1630. [Google Scholar] [CrossRef] [PubMed]
- Van Campen, C.; de Boer, A.H.; Iedema, J. Are informal caregivers less happy than noncaregivers? Happiness and the intensity of caregiving in combination with paid and voluntary work. Scand. J. Caring Sci. 2013, 27, 44–50. [Google Scholar] [CrossRef]
- Córdoba, L.; Mora, A.; Bedoya, Á.; Verdugo, M.A. Familias de adultos con discapacidad intelectual en Cali, Colombia, desde el modelo de Calidad de Vida. (spanish adaptation from the original: Families of adults with intellectual disability in Cali, Colombia, using the model Quality of Life). Psykhe Rev. Esc. Psicol. 2007, 16, 29–42. [Google Scholar]
- Pisula, E.; Porębowicz-Dörsmann, A. Family functioning, parenting stress and quality of life in mothers and fathers of Polish children with high functioning autism or Asperger syndrome. PLoS ONE 2017, 12, e0186536. [Google Scholar] [CrossRef]
- Liesen, A.M. The Influence of Coping Processes and Social Supports on Stress and Quality of Life Outcomes of Parents of Children with Autism Spectrum Disorders; ProQuest Information & Learning: Ann Arbor, MI, USA, 2014. [Google Scholar]
- Macek, K. Parental Distress in Mothers of Children with Developmental Disabilities; ProQuest Information & Learning: Ann Arbor, MI, USA, 2014. [Google Scholar]
- WHO. International Statistical Classification of Diseases and Related Health Problems, Eleventh Revision (ICD-11); WHO: Geneva, Switzerland, 2018. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- AAIDD Ad Hoc Committee on Terminology and Classification. Intellectual Disability: Definition, Classification, and Systems of Support, 11th ed.; AAIDD: Washington, DC, USA, 2010. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; Text Rev.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Wang, J.; Hu, Y.-J.; Wang, Y.; Chen, Y.-P.; Wang, H.; Sun, C.-H.; Xia, W.; Wu, L.-J. Parenting stress in mothers of children with autism: A 6-month follow-up study. Chin. Ment. Health J. 2013, 27, 669–673. [Google Scholar]
- Díaz-Herrero, Á.; de la Nuez, A.G.B.; López Pina, J.A.; Pérez-López, J.; Martínez-Fuentes, M.T. Estructura factorial y consistencia interna de la versión Española del Parenting Stress Index-Short Form. (spanish adaptation from the original: Factor structure and internal consistency of the Spanish version of the Parenting Stress Index-Short Form). Psicothema 2010, 22, 1033–1038. [Google Scholar]
- Díaz-Herrero, Á.; López-Pina, J.A.; Pérez-López, J.; de la Nuez, A.G.B.; Martínez-Fuentes, M.T. Validity of the Parenting Stress Index-Short Form in a sample of Spanish fathers. Span. J. Psychol. 2011, 14, 990–997. [Google Scholar] [CrossRef] [PubMed]
- Rivas, G.R.; Arruabarrena, I.; de Paúl, J. Parenting Stress Index-Short Form: Psychometric properties of the Spanish version in mothers of children aged 0 to 8 Years. Psychosoc. Interv. 2020. [Google Scholar] [CrossRef]
- Jenaro, C.; Gutiérrez, B. Análisis de la Escala de Estrés Parental-Forma Abreviada en padres de hijos con discapacidad intelectual mediante el Modelo de Rasch (spanish adaptation from the original: Analysis of the Parenting Stress Index- Short Form on parents of children with intellectual disabilities with the Rasch Model). Rev. Iberoam. Diagn. Eval. Psicol. 2015, 39, 68–76. [Google Scholar]
- Reitman, D.; Currier, R.O.; Stickle, T.R. A critical evaluation of the Parenting Stress Index-Short Form (PSI-SF) in a Head Start population. J. Clin. Child Adolesc. Psychol. 2002, 31, 384–392. [Google Scholar] [CrossRef]
- Verdugo, M.A.; Córdoba, L.; Gómez, J. Spanish adaptation and validation of the Family Quality of Life Survey. J. Intellect. Disabil. Res. JIDR 2005, 49, 794–798. [Google Scholar] [CrossRef]
- Verdugo, M.A.; Rodríguez, A.; Sáinz, F. Escala de calidad de vida familiar. In Manual de Aplicación; INICO, Universidad de Salamanca: Salamanca, Spain, 2012. [Google Scholar]
- Balcells-Balcells, A.; Giné, C.; Guàrdia-Olmos, J.; Summers, J.A. Family quality of life: Adaptation to Spanish population of several family support questionnaires. J. Intellect. Disabil. Res. 2011, 55, 1151–1163. [Google Scholar] [CrossRef]
- Thompson, J.R.; Bryant, B.; Campbell, E.M.; Craig, E.M.; Hughes, C.; Rotholz, D.A.; Schalock, R.L.; Silverman, W.; Tasse, M.; Wehmeyer, M.L. Supports Intensity Scale; American Association on Intellectual and Developmental Disabilities: Washington, DC, USA, 2004. [Google Scholar]
- American Association on Mental Retardation. Supports Intensity Scale: Information; American Association on Mental Retardation: Washington, DC, USA, 2004; Available online: https://www.aaidd.org/docs/default-source/sis-docs/sisoverview.pdf (accessed on 2 December 2020).
- Verdugo, M.A.; Arias, B.; Ibáñez, A. Escala de Intensidad de Apoyos. Manual (Spanish Adaptation from the Original: Supports Intensity Scale); TEA: Madrid, Spain, 2007. [Google Scholar]
- Fernández Faúndez, E.M.; Arias Martínez, B.; Gómez Sánchez, L.E.; Jorrín Abellán, I.M. Calidad de vida en familias de personas mayores con discapacidad intelectual. Siglo Cero 2012, 43, 31–48. [Google Scholar]
- Rodríguez Aguilella, A.; Verdugo Alonso, M.Á.; Sánchez, M.C. Calidad de vida familiar y apoyos para los progenitores de personas con discapacidad intelectual en proceso de envejecimiento. Siglo Cero 2008, 39, 19–34. [Google Scholar]
- Byiers, B.J.; Tervo, R.C.; Feyma, T.J.; Symons, F.J. Seizures and pain uncertainty associated with parenting stress and Rett syndrome. J. Child Neurol. 2014, 29, 526–529. [Google Scholar] [CrossRef]
- Al-Yagon, M.; Margalit, M. Positive and negative affect among mothers of children with intellectual disabilities. Br. J. Dev. Disabil. 2009, 55, 109–127. [Google Scholar] [CrossRef]
- Camargo de Oliveira, É.B.; Pereira, R.C.M.; Apis, A.; Germano, C.M.R.; Pilotto, R.F.; Melo, D.G. Qualidade de vida de famílias de filhos com deficiência intelectual moderada (spanish adaptation from the original: Quality of life in families with children with moderate intellectual disability). J. Bras. Psiquiatr. 2019, 68, 101–109. [Google Scholar] [CrossRef]
- Thompson, S.; Hiebert-Murphy, D.; Trute, B. Parental perceptions of family adjustment in childhood developmental disabilities. J. Intellect. Disabil. 2012, 17, 24–37. [Google Scholar] [CrossRef] [PubMed]
- Wakimizu, R.; Yamaguchi, K.; Fujioka, H. Family empowerment and quality of life of parents raising children with Developmental Disabilities in 78 Japanese families. Int. J. Nurs. Sci. 2016, 4, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Ylvén, R.; Björck-Åkesson, E.; Granlund, M. Literature review of positive functioning in families with children with a disability. J. Policy Pract. Intellect. Disabil. 2006, 3, 253–270. [Google Scholar] [CrossRef]
- Zhang, Y.; Yi, C.-L. Relationship between depression and related factors of parents with disabled children. Chin. J. Clin. Psychol. 2011, 19, 776–778. [Google Scholar]
- Hall, H.R.; Neely-Barnes, S.L.; Graff, J.C.; Krcek, T.E.; Roberts, R.J.; Hankins, J.S. Parental stress in families of children with a genetic disorder/disability and the resiliency model of family stress, adjustment, and adaptation. Issues Compr. Pediatr. Nurs. 2012, 35, 24–44. [Google Scholar] [CrossRef]
- Martin, D. The Impact of Respite, Coping Style, and Child’s Adaptive Functioning on Parental Stress; ProQuest Information & Learning: Ann Arbor, MI, USA, 2001. [Google Scholar]
- Woodman, A.C.; Hauser-Cram, P. The role of coping strategies in predicting change in parenting efficacy and depressive symptoms among mothers of adolescents with developmental disabilities. J. Intellect. Disabil. Res. 2013, 57, 513–530. [Google Scholar] [CrossRef]
- Cuzzocrea, F.; Larcan, R.; Costa, S.; Gazzano, C. Parents’ competence and social skills in siblings of disabled children. Soc. Behav. Personal. 2014, 42, 45–58. [Google Scholar] [CrossRef]
- Antonakis, J.; Bendahan, S.; Jacquart, P.; Lalive, R. Causality and endogeneity: Problems and solutions. In The Oxford Handbook of Leadership and Organizations; Day, D.V., Ed.; Oxford University Press: New York, NY, USA, 2014; pp. 93–117. [Google Scholar]
| Variables (and Codes) | N | % |
|---|---|---|
| Gender of caregivers | ||
| Male (1) | 158 | 30.7 |
| Female (2) | 357 | 69.3 |
| Caregivers kinship | ||
| Parent (1) | 379 | 73.6 |
| Sibling (2) | 101 | 19.8 |
| Other (3) | 35 | 6.8 |
| Marital status of caregivers | ||
| Married (1) | 364 | 70.7 |
| Living alone (widow, single, divorced) (2) | 117 | 29.0 |
| Educational status of caregivers | ||
| Primary education (1) | 191 | 37.1 |
| Secondary education (2) | 144 | 28.0 |
| High school (3) | 58 | 11.3 |
| University studies (4) | 122 | 23.7 |
| Employment status of caregivers | ||
| Working (1) | 211 | 41.0 |
| Not Working (2) | 237 | 59.0 |
| Gender of individual with disability | ||
| Male (1) | 308 | 59.8 |
| Female (2) | 207 | 40.2 |
| Severity of Intellectual disability | ||
| Mild (1) | 97 | 19.8 |
| Moderate (2) | 234 | 45.4 |
| Severe (3) | 159 | 30.9 |
| Profound (4) | 25 | 4.9 |
| Number of services attended (occupational, recreational…) | ||
| None (0) | 10 | 1.9 |
| One (1) | 285 | 51.5 |
| Two (2) | 155 | 30.1 |
| Three (3) | 60 | 11.7 |
| Four (4) | 25 | 4.9 |
| Goodness-of-Fit Statistics | Values |
|---|---|
| Degrees of Freedom | 256 |
| Satorra-Bentler Scaled Chi-Square (p = 1.00) | 35.21 |
| Root Mean Square Error of Approximation (RMSEA) | 0.0 |
| P-Value for Test of Close Fit (RMSEA <0.05) | 1.00 |
| Expected Cross-Validation Index (ECVI) | 16.04 |
| ECVI for Saturated Model | 27.08 |
| ECVI for Independence Model | 50.56 |
| Independence Akaike Information Criterion (AIC) | 1213.34 |
| Model AIC | 155.21 |
| Saturated AIC | 650.00 |
| Independence Consistent Akaike Information Criterion (CAIC) | 1268.81 |
| Model CAIC | 288.35 |
| Saturated CAIC | 1371.13 |
| Normed Fit Index (NFI) | 0.97 |
| Non-Normed Fit Index (NNFI) | 1.00 |
| Comparative Fit Index (CFI) | 1.00 |
| Incremental Fit Index (IFI) | 1.00 |
| Root Mean Square Residual (RMR) | 0.073 |
| Standardized RMR | 0.073 |
| Goodness of Fit Index (GFI) | 0.98 |
| Adjusted Goodness of Fit Index (AGFI) | 0.97 |
| Parsimony Goodness of Fit Index (PGFI) | 0.80 |
| Variables | Parental Distress |
|---|---|
| Caregivers | |
| Gender | 0.069 |
| Age | 0.082 |
| Marital status | 0.006 |
| Educational status | −0.067 |
| Employment status | 0.100 |
| Individual with disability | |
| Age | −0.072 |
| Gender | −0.009 |
| Number of services received | −0.072 |
| Severity of Behavioral needs | 0.224 ** |
| Severity of Medical needs | 0.168 ** |
| Severity of the intellectual disability | 0.176 ** |
| Family capabilities | |
| Physical/Material Well-being | −0.170 ** |
| Caregivers’ kinship | −0.150 ** |
| Family interaction | −0.328 ** |
| Parenting | −0.281 ** |
| Family meaning | |
| Dysfunctional interaction | 0.606 ** |
| Difficult Child | 0.580 ** |
| Emotional Well-being | −0.357 ** |
| Disability-Related Support | −0.224 ** |
| Variables | Block 1 | Block 2 | Block 3 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | t | p | B | SE | β | t | p | B | SE | β | t | p | |
| Support needs | |||||||||||||||
| Behavioral needs | 0.71 | 0.19 | 0.17 | 3.68 | <0.01 | 0.63 | 0.18 | 0.15 | 3.49 | <0.01 | −0.22 | 0.16 | −0.05 | −1.40 | 0.16 |
| Medical needs | 0.40 | 0.26 | 0.07 | 1.52 | 0.13 | 0.59 | 0.25 | 0.10 | 2.39 | 0.02 | 0.47 | 0.20 | 0.08 | 2.35 | 0.02 |
| Severity of Intellectual disabilities | 1.53 | 0.58 | 0.12 | 2.66 | 0.01 | 1.40 | 0.54 | 0.11 | 2.62 | 0.01 | 0.88 | 0.43 | 0.07 | 2.02 | 0.04 |
| Family capabilities | |||||||||||||||
| Kinship | −2.80 | 0.69 | −0.16 | −4.07 | <0.01 | −1.47 | 0.56 | −0.09 | −2.62 | 0.01 | |||||
| Physical/Material Wellbeing | 0.25 | 0.56 | 0.02 | 0.45 | 0.65 | 0.03 | 0.51 | 0.00 | 0.05 | 0.96 | |||||
| Family Interaction | −2.99 | 0.69 | −0.25 | −4.33 | <0.01 | −1.68 | 0.58 | −0.14 | −2.91 | <0.01 | |||||
| Parenting | −1.22 | 0.66 | −0.11 | −1.85 | 0.06 | 0.27 | 0.59 | 0.02 | 0.45 | 0.65 | |||||
| Family appraisal | |||||||||||||||
| Dysfunctional interaction | 0.39 | 0.05 | 0.35 | 7.57 | <0.01 | ||||||||||
| Difficult behaviors | 0.29 | 0.05 | 0.28 | 5.79 | <0.01 | ||||||||||
| Emotional well-being | −1.69 | 0.45 | −0.17 | −3.81 | <0.01 | ||||||||||
| Disability-Related Support | 0.63 | 0.51 | 0.06 | 1.24 | 0.22 | ||||||||||
| R | 0.253 | 0.453 | 0.700 | ||||||||||||
| R2 | 0.064 ** | 0.205 ** | 0.490 ** | ||||||||||||
| Adj R2 | 0.058 | 0.194 | 0.479 | ||||||||||||
| SE | 9.83 | 9.10 | 7.31 | ||||||||||||
| F(dfn,dfd) | F(3, 505) = 11.512 ** | F(7, 501) = 18.451 ** | F(11,497) = 43.384 ** | ||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jenaro, C.; Flores, N.; Gutiérrez-Bermejo, B.; Vega, V.; Pérez, C.; Cruz, M. Parental Stress and Family Quality of Life: Surveying Family Members of Persons with Intellectual Disabilities. Int. J. Environ. Res. Public Health 2020, 17, 9007. https://doi.org/10.3390/ijerph17239007
Jenaro C, Flores N, Gutiérrez-Bermejo B, Vega V, Pérez C, Cruz M. Parental Stress and Family Quality of Life: Surveying Family Members of Persons with Intellectual Disabilities. International Journal of Environmental Research and Public Health. 2020; 17(23):9007. https://doi.org/10.3390/ijerph17239007
Chicago/Turabian StyleJenaro, Cristina, Noelia Flores, Belén Gutiérrez-Bermejo, Vanessa Vega, Carmen Pérez, and Maribel Cruz. 2020. "Parental Stress and Family Quality of Life: Surveying Family Members of Persons with Intellectual Disabilities" International Journal of Environmental Research and Public Health 17, no. 23: 9007. https://doi.org/10.3390/ijerph17239007
APA StyleJenaro, C., Flores, N., Gutiérrez-Bermejo, B., Vega, V., Pérez, C., & Cruz, M. (2020). Parental Stress and Family Quality of Life: Surveying Family Members of Persons with Intellectual Disabilities. International Journal of Environmental Research and Public Health, 17(23), 9007. https://doi.org/10.3390/ijerph17239007






