Impact of Extreme Temperatures on Ambulance Dispatches Due to Cardiovascular Causes in North-West Spain
Abstract
1. Introduction
2. Methods
2.1. Settings
2.2. Healthcare Data
2.3. Temperature Data
2.4. Statistical Analysis
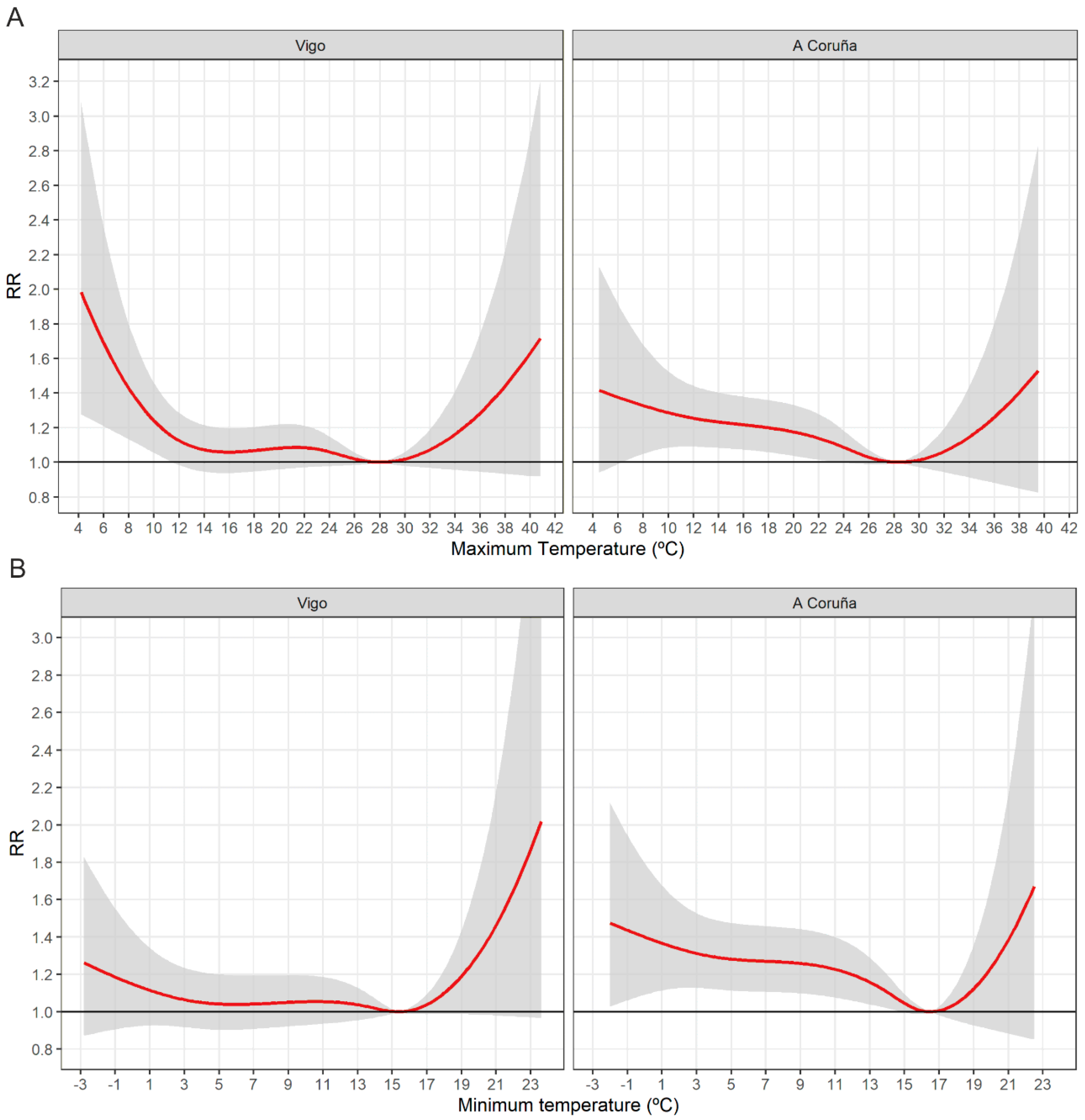
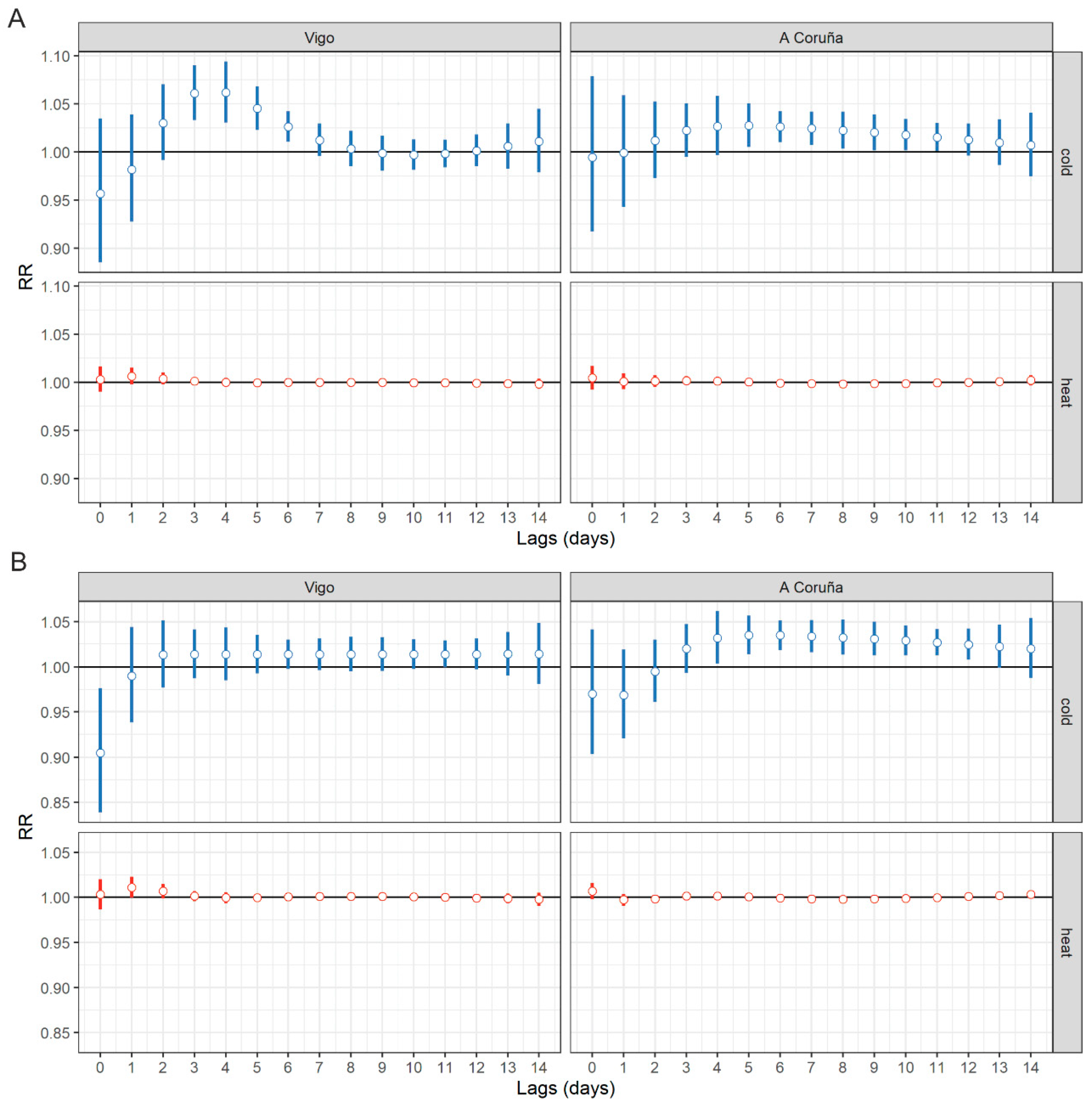
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AN/AF | Attributable number/fraction |
| RR | Relative risk |
| Tmin | Minimum temperature |
| Tmax | Maximum temperature |
| MMT | Minimum morbidity temperature |
| 95% CI | 95% confidence interval |
References
- Armstrong, B.G.; Chalabi, Z.; Fenn, B.; Hajat, S.; Kovats, S.; Milojevic, A.; Wilkinson, P. Association of mortality with high temperatures in a temperate climate: England and Wales. J. Epidemiol. Community Health 2011, 65, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Baccini, M.; Biggeri, A.; Accetta, G.; Kosatsky, T.; Katsouyanni, K.; Analitis, A.; Anderson, H.R.; Bisanti, L.; D’Ippoliti, D.; Danova, J.; et al. Heat effects on mortality in 15 European cities. Epidemiology 2008, 19, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Braga, A.L.; Zanobetti, A.; Schwartz, J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ. Health Perspect. 2002, 110, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Bhaskaran, K.; Hajat, S.; Haines, A.; Herrett, E.; Wilkinson, P.; Smeeth, L. Effects of ambient temperature on the incidence of myocardial infarction. Heart 2009, 95, 1760–1769. [Google Scholar] [CrossRef]
- Royé, D.; Zarrabeitia, M.T.; Riancho, J.; Santurtún, A. A time series analysis of the relationship between apparent temperature, air pollutants and ischemic stroke in Madrid, Spain. Environ. Res. 2019, 173, 349–358. [Google Scholar]
- Comelli, I.; Ferro, J.; Lippi, G.; Comelli, D.; Sartori, E.; Cervellin, G. Incidence of acute-onset atrial fibrillation correlates with air temperature. Results of a nine-year survey. J. Epidemiol. Glob. Health 2014, 4, 151–157. [Google Scholar] [CrossRef]
- Błażejczyk, A.; Błażejczyk, K.; Baranowski, J.; Kuchcik, M. Heat stress mortality and desired adaptation responses of healthcare system in Poland. Int. J. Biometeorol. 2018, 62, 307–318. [Google Scholar] [CrossRef]
- Zhang, Y.; Yan, C.; Kan, H.; Cao, J.; Peng, L.; Xu, J.; Wang, W. Effect of ambient temperature on emergency department visits in Shanghai, China: A time series study. Environ. Health 2014, 13, 100. [Google Scholar] [CrossRef]
- Schwartz, J.; Samet, J.M.; Patz, J.A. Hospital admissions for heart disease: The effects of temperature and humidity. Epidemiology 2004, 15, 755–761. [Google Scholar] [CrossRef]
- Liu, Y.; Hoppe, B.O.; Convertino, M. Threshold Evaluation of Emergency Risk Communication for Health Risks Related to Hazardous Ambient Temperature. Risk Anal. 2018, 38, 2208–2221. [Google Scholar] [CrossRef]
- Iñiguez, C.; Royé, D.; Tobías, A. Contrasting patterns of temperature related mortality and hospitalisation by cardiovascular and respiratory diseases in 52 Spanish cities. Environ. Res. 2020, 192, 110191. [Google Scholar]
- Royé, D.; Figueiras, A.; Taracido, M. Short-term effects of heat and cold on respiratory drug use. A time-series epidemiological study in A Coruña, Spain. Pharmacoepidemiol. Drug Saf. 2018, 27, 638–644. [Google Scholar]
- Carracedo-Martinez, E.; Sanchez, C.; Taracido, M.; Saez, M.; Jato, V.; Figueiras, A. Effect of short-term exposure to air pollution and pollen on medical emergency calls: A case-crossover study in Spain. Allergy 2008, 63, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Armstrong, B. Reducing and meta-analysing estimates from distributed lag non-linear models. BMC Med. Res. Methodol. 2013, 13, 1. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat. Med. 2012, 31, 3821–3839. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Gasparrini, A.; Hajat, S.; Smeeth, L.; Armstrong, B. Time series regression studies in environmental epidemiology. Int. J. Epidemiol. 2013, 42, 1187–1195. [Google Scholar] [CrossRef]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobias, A.; Tong, S.; Rocklöv, J.; Forsberg, B.; et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Tobías, A.; Armstrong, B.; Gasparrini, A. Brief Report: Investigating Uncertainty in the Minimum Mortality Temperature: Methods and Application to 52 Spanish Cities. Epidemiology 2017, 28, 72–76. [Google Scholar] [CrossRef]
- Gasparrini, A.; Leone, M. Attributable risk from distributed lag models. BMC Med. Res. Methodol. 2014, 14, 55. [Google Scholar] [CrossRef]
- Core Team, R. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019; Available online: https://www.R-project.org/ (accessed on 3 March 2020).
- Onozuka, D.; Hagihara, A. All-Cause and Cause-Specific Risk of Emergency Transport Attributable to Temperature: A Nationwide Study. Medicine 2016, 94, e2259. [Google Scholar] [CrossRef]
- Hensel, M.; Stuhr, M.; Geppert, D.; Kersten, J.F.; Lorenz, J.; Kerner, T. Relationship between ambient temperature and frequency and severity of cardiovascular emergencies: A prospective observational study based on out-of-hospital care data. Int. J. Cardiol. 2017, 228, 553–557. [Google Scholar] [CrossRef] [PubMed]
- McGuinn, L.; Hajat, S.; Wilkinson, P.; Armstrong, B.; Anderson, H.R.; Monk, V.; Harrison, R. Ambient temperature and activation of implantable cardioverter defibrillators. Int. J. Biometeorol. 2013, 57, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Vencloviene, J.; Babarskiene, R.M.; Dobozinskas, P.; Dedele, A.; Lopatiene, K.; Ragaisyte, N. The short-term associations of weather and air pollution with emergency ambulance calls for paroxysmal atrial fibrillation. Environ. Sci. Pollut. Res. Int. 2017, 24, 15031–15043. [Google Scholar] [CrossRef] [PubMed]
- Vencloviene, J.; Babarskiene, R.; Dobozinskas, P.; Siurkaite, V. Effects of weather conditions on emergency ambulance calls for acute coronary syndromes. Int. J. Biometeorol. 2015, 59, 1083–1093. [Google Scholar] [CrossRef] [PubMed]
- García-Lledó, A.; Rodríguez-Martín, S.; Tobías, A.; Alonso-Martín, J.; Ansede-Cascudo, J.C.; De Abajo, F.J. Heat waves, ambient temperature, and risk of myocardial infarction: An ecological study in the Community of Madrid. Rev. Esp. Cardiol. 2020, 73, 300–306. [Google Scholar] [CrossRef]
- Fernández-García, J.M.; Díaz, O.D.; Hidalgo, J.J.T.; Fernández, J.R.; Sánchez-Santos, L. Influencia del clima en el infarto de miocardio en Galicia. Med. Clin. 2015, 145, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Morabito, M.; Crisci, A.; Vallorani, R.; Modesti, P.A.; Gensini, G.F.; Orlandini, S.; Morabito, M. Innovative approaches helpful to enhance knowledge on weather-related stroke events over a wide geographical area and a large population. Stroke 2011, 42, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Milo-Cotter, O.; Setter, I.; Uriel, N.; Kaluski, E.; Vered, Z.; Golik, A.; Cotter, G. The daily incidence of acute heart failure is correlated with low minimal night temperature: Cold immersion pulmonary edema revisited? J. Card. Fail. 2006, 12, 114–119. [Google Scholar] [CrossRef]
- Stewart, S.; McIntyre, K.; Capewell, S.; McMurray, J.J. Heart failure in a cold climate. Seasonal variation in heart failure-related morbidity and mortality. J. Am. Coll. Cardiol. 2002, 39, 760–766. [Google Scholar] [CrossRef]
- Sangkharat, K.; Mahmood, M.A.; Thornes, J.E.; Fisher, P.A.; Pope, F.D. Impact of extreme temperatures on ambulance dispatches in London, UK. Environ. Res. 2020, 182, 109100. [Google Scholar] [CrossRef]
- Cui, Y.; Ai, S.; Liu, Y.; Qian, Z.; Wang, C.; Sun, J.; Sun, X.; Zhang, S.; Syberg, K.M.; Howard, S.; et al. Hourly associations between ambient temperature and emergency ambulance calls in one central Chinese city: Call for an immediate emergency plan. Sci. Total Environ. 2020, 711, 135046. [Google Scholar] [CrossRef] [PubMed]
- Barnett, A.G.; Tong, S.; Clements, A.C. What measure of temperature is the best predictor of mortality? Environ. Res. 2010, 110, 604–611. [Google Scholar] [CrossRef] [PubMed]
- Alessandrini, E.; Sajani, S.Z.; Scotto, F.; Miglio, R.; Marchesi, S.; Lauriola, P. Emergency ambulance dispatches and apparent temperature: A time series analysis in Emilia-Romagna, Italy. Environ. Res. 2011, 111, 1192–1200. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Yu, I.T.; Tse, L.A.; Tian, L.; Wang, X.; Wong, T.W. Is greater temperature change within a day associated with increased emergency hospital admissions for heart failure? Circ. Heart Fail. 2013, 6, 930–935. [Google Scholar] [CrossRef]
- Williams, S.; Nitschke, M.; Sullivan, T.; Tucker, G.R.; Weinstein, P.; Pisaniello, D.L.; Parton, K.A.; Bi, P. Heat and health in Adelaide, South Australia: Assessment of heat thresholds and temperature relationships. Sci. Total Environ. 2012, 414, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Turner, L.R.; Connell, D.; Tong, S. Exposure to hot and cold temperatures and ambulance attendances in Brisbane, Australia: A time-series study. BMJ Open 2012, 2, e001074. [Google Scholar] [CrossRef]
- Ma, W.; Chen, R.; Kan, H. Temperature-related mortality in 17 large Chinese cities: How heat and cold affect mortality in China. Environ. Res. 2014, 134, 127–133. [Google Scholar] [CrossRef]
- Kysely, J.; Pokorna, L.; Kyncl, J.; Kriz, B. Excess cardiovascular mortality associated with cold spells in the Czech Republic. BMC Public Health 2009, 9, 19. [Google Scholar] [CrossRef]
- Claeys, M.J.; Rajagopalan, S.; Nawrot, T.S.; Brook, R.D. Climate and environmental triggers of acute myocardial infarction. Eur. Heart J. 2017, 38, 955–960. [Google Scholar] [CrossRef]
- Bhatnagar, A. Environmental determinants of cardiovascular disease. Circ. Res. 2017, 121, 162–180. [Google Scholar] [CrossRef]
- Xie, W.; Li, G.; Zhao, D.; Xie, X.; WAei, Z.; Wang, W.; Wang, M.; Li, G.; Liu, W.; Sun, J.; et al. Relationship between fine particulate air pollution and ischaemic heart disease morbidity and mortality. Heart 2015, 101, 257–263. [Google Scholar] [CrossRef] [PubMed]
| Maximum Temperatures (°C) | Minimum Temperatures (°C) | Calls (Number) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| City | Mean | Minimum | Maximum | Mean | Minimum | Maximum | Total | Mean | Maximum |
| Vigo | 18.9 | 4.2 | 40.8 | 10.1 | −2.8 | 22.5 | 37278 | 7.9 | 23 |
| A Coruña | 19.2 | 4.5 | 39.5 | 10.5 | −2.0 | 23.6 | 33259 | 7.1 | 18 |
| City | Exposure | Effect | * AF% (95 CI%) | ‡ AN (95 CI%) |
|---|---|---|---|---|
| A Coruña | Maximum | cold | 14 (5.4. 21.6) | 4650 (1782, 7199) |
| A Coruña | Maximum | heat | 0.3 (−0.3. 0.8) | 103 (−96, 270) |
| Vigo | Maximum | cold | 7.4 (−1.8. 15.3) | 2751 (−659, 5710) |
| Vigo | Maximum | heat | 0.4 (−0.2. 0.9) | 142 (−59, 319) |
| A Coruña | Minimum | cold | 15.7 (7.3. 23.5) | 5224 (2443, 7823) |
| A Coruña | Minimum | heat | 0.3 (−0.2. 0.7) | 89 (−81, 231) |
| Vigo | Minimum | cold | 3.9 (−5.6. 12.5) | 1448 (−2083, 4666) |
| Vigo | Minimum | heat | 0.5 (−0.1. 0.9) | 169 (−32, 339) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romani, S.G.; Royé, D.; Sánchez Santos, L.; Figueiras, A. Impact of Extreme Temperatures on Ambulance Dispatches Due to Cardiovascular Causes in North-West Spain. Int. J. Environ. Res. Public Health 2020, 17, 9001. https://doi.org/10.3390/ijerph17239001
Romani SG, Royé D, Sánchez Santos L, Figueiras A. Impact of Extreme Temperatures on Ambulance Dispatches Due to Cardiovascular Causes in North-West Spain. International Journal of Environmental Research and Public Health. 2020; 17(23):9001. https://doi.org/10.3390/ijerph17239001
Chicago/Turabian StyleRomani, Santiago Gestal, Dominic Royé, Luis Sánchez Santos, and Adolfo Figueiras. 2020. "Impact of Extreme Temperatures on Ambulance Dispatches Due to Cardiovascular Causes in North-West Spain" International Journal of Environmental Research and Public Health 17, no. 23: 9001. https://doi.org/10.3390/ijerph17239001
APA StyleRomani, S. G., Royé, D., Sánchez Santos, L., & Figueiras, A. (2020). Impact of Extreme Temperatures on Ambulance Dispatches Due to Cardiovascular Causes in North-West Spain. International Journal of Environmental Research and Public Health, 17(23), 9001. https://doi.org/10.3390/ijerph17239001





