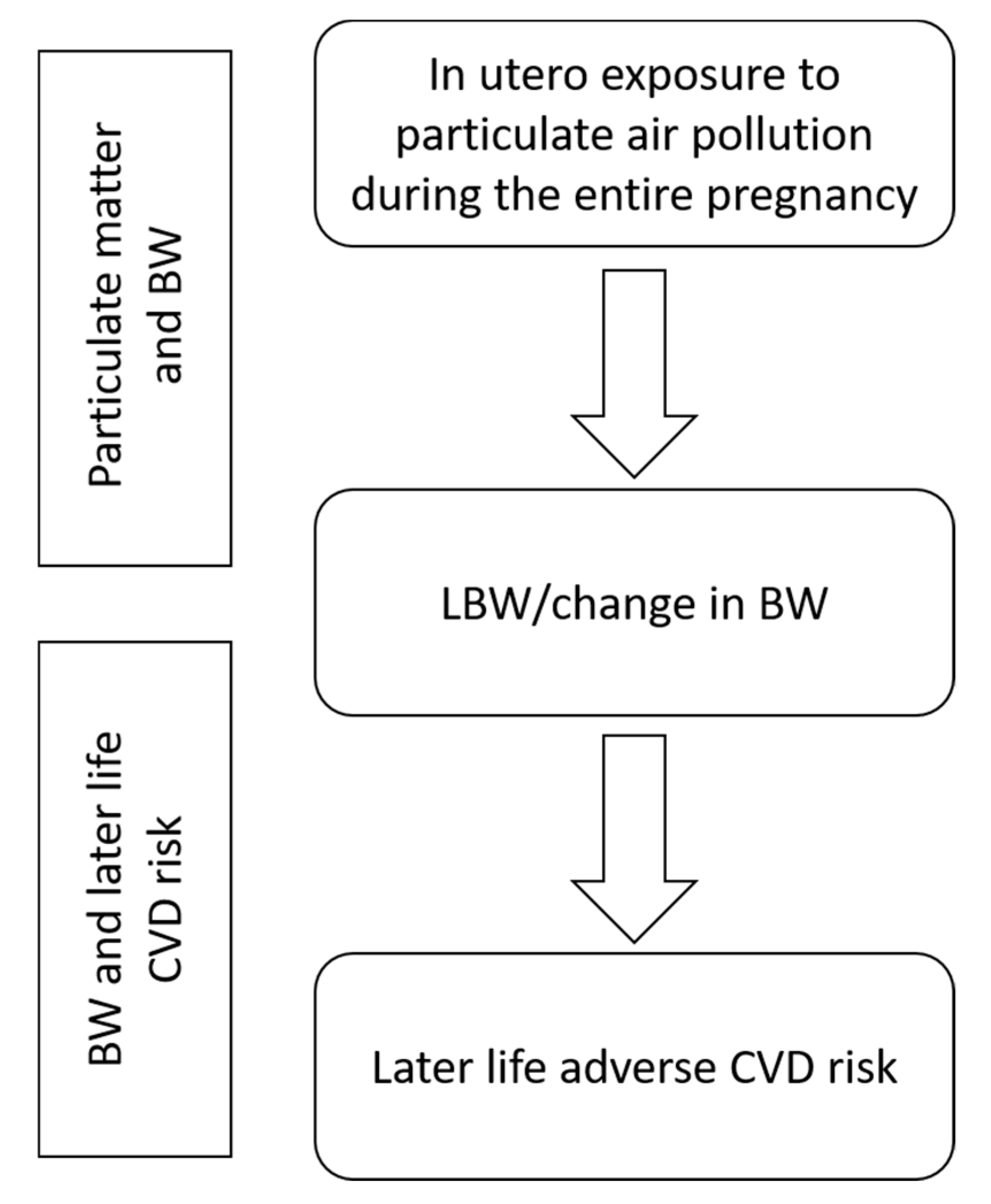
In Utero Exposure to Particulate Air Pollution during Pregnancy: Impact on Birth Weight and Health through the Life Course
Abstract
1. Introduction
2. Methods
3. Results
3.1. Particulate Matter and Birth Weight
3.2. Birth Weight and Later Life CVD Risk
4. Discussion
5. Conclusions
Supplementary Materials
Funding
Acknowledgments
Conflicts of Interest
References
- Barker, D.J.; Eriksson, J.G.; Forsén, T.; Osmond, C. Fetal origins of adult disease: Strength of effects and biological basis. Int. J. Epidemiol. 2002, 31, 1235–1239. [Google Scholar] [CrossRef] [PubMed]
- Calkins, K.; Devaskar, S.U. Fetal origins of adult disease. Curr. Probl. Pediatric Adolesc. Health Care 2011, 41, 158–176. [Google Scholar] [CrossRef] [PubMed]
- Barker, D.J. The origins of the developmental origins theory. J. Intern. Med. 2007, 261, 412–417. [Google Scholar] [CrossRef] [PubMed]
- Courtney, R. The health consequences of smoking—50 years of progress: A report of the surgeon general, 2014 US Department of Health and Human Services Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014 1081 pp. Online (grey literature): http://www.Surgeongeneral.Gov/Library/Reports/50-years-of-progress. Drug Alcohol Rev. 2015, 34, 694–695. [Google Scholar]
- Cnattingius, S. The epidemiology of smoking during pregnancy: Smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tobacco Res. 2004, 6, S125–S140. [Google Scholar] [CrossRef]
- Cui, H.; Gong, T.; Liu, C.; Wu, Q. Associations between passive maternal smoking during pregnancy and preterm birth: Evidence from a meta-analysis of observational studies. PLoS ONE 2016, 11, e0147848. [Google Scholar] [CrossRef]
- Sun, X.; Luo, X.; Zhao, C.; Zhang, B.; Tao, J.; Yang, Z.; Ma, W.; Liu, T. The associations between birth weight and exposure to fine particulate matter (PM2.5) and its chemical constituents during pregnancy: A meta-analysis. Environ. Pollut. 2016, 211, 38–47. [Google Scholar] [CrossRef]
- Ye, L.; Ji, Y.; Lv, W.; Zhu, Y.; Lu, C.; Xu, B.; Xia, Y. Associations between maternal exposure to air pollution and birth outcomes: A retrospective cohort study in Taizhou, China. Environ. Sci. Pollut. Res. 2018, 25, 21927–21936. [Google Scholar] [CrossRef]
- Amegah, A.K.; Quansah, R.; Jaakkola, J.J. Household air pollution from solid fuel use and risk of adverse pregnancy outcomes: A systematic review and meta-analysis of the empirical evidence. PLoS ONE 2014, 9, e113920. [Google Scholar] [CrossRef]
- Reid, C.E.; Brauer, M.; Johnston, F.H.; Jerrett, M.; Balmes, J.R.; Elliott, C.T. Critical review of health impacts of wildfire smoke exposure. Environ. Health Perspect. 2016, 124, 1334–1343. [Google Scholar] [CrossRef]
- Chaudhuri, I.; Fruijtier-Pölloth, C.; Ngiewih, Y.; Levy, L. Evaluating the evidence on genotoxicity and reproductive toxicity of carbon black: A critical review. Crit. Rev. Toxicol. 2018, 48, 143–169. [Google Scholar] [CrossRef] [PubMed]
- Ema, M.; Naya, M.; Horimoto, M.; Kato, H. Developmental toxicity of diesel exhaust: A review of studies in experimental animals. Reprod. Toxicol. 2013, 42, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Morales-Rubio, R.A.; Alvarado-Cruz, I.; Manzano-León, N.; Uribe-Ramirez, M.; Quintanilla-Vega, B.; Osornio-Vargas, A.; De Vizcaya-Ruiz, A. In utero exposure to ultrafine particles promotes placental stress-induced programming of renin-angiotensin system-related elements in the offspring results in altered blood pressure in adult mice. Part. Fibre Toxicol. 2019, 16, 7. [Google Scholar] [CrossRef]
- Hougaard, K.S.; Campagnolo, L.; Chavatte-Palmer, P.; Tarrade, A.; Rousseau-Ralliard, D.; Valentino, S.; Park, M.V.; de Jong, W.H.; Wolterink, G.; Piersma, A.H. A perspective on the developmental toxicity of inhaled nanoparticles. Reprod. Toxicol. 2015, 56, 118–140. [Google Scholar] [CrossRef] [PubMed]
- Kannan, S.; Misra, D.P.; Dvonch, J.T.; Krishnakumar, A. Exposures to airborne particulate matter and adverse perinatal outcomes: A biologically plausible mechanistic framework for exploring potential effect modification by nutrition. Environ. Health Perspect. 2006, 114, 1636–1642. [Google Scholar] [CrossRef]
- Cai, Y.; Hansell, A.L.; Granell, R.; Blangiardo, M.; Zottoli, M.; Fecht, D.; Gulliver, J.; Henderson, A.J.; Elliott, P. Prenatal, early-life and childhood exposure to air pollution and lung function: The ALSPAC cohort. Am. J. Respir. Crit. Care Med. 2020. [Google Scholar] [CrossRef]
- Yang, S.; Kim, H.; Kim, H.; Lee, S.; Kang, M.; Cho, H.; Yoon, J.; Jung, S.; Lee, E.; Yang, H. Particulate matter at third trimester and respiratory infection in infants, modified by GSTM1. Pediatr. Pulmonol. 2020, 55, 245–253. [Google Scholar] [CrossRef]
- Guxens, M.; Lubczyńska, M.J.; Muetzel, R.L.; Dalmau-Bueno, A.; Jaddoe, V.W.; Hoek, G.; van der Lugt, A.; Verhulst, F.C.; White, T.; Brunekreef, B. Air pollution exposure during fetal life, brain morphology, and cognitive function in school-age children. Biol. Psychiatry 2018, 84, 295–303. [Google Scholar] [CrossRef]
- Rosa, M.J.; Hair, G.M.; Just, A.C.; Kloog, I.; Svensson, K.; Pizano-Zárate, M.L.; Pantic, I.; Schnaas, L.; Tamayo-Ortiz, M.; Baccarelli, A.A. Identifying critical windows of prenatal particulate matter (PM2.5) exposure and early childhood blood pressure. Environ. Res. 2020, 182, 109073. [Google Scholar] [CrossRef]
- Breton, C.V.; Mack, W.J.; Yao, J.; Berhane, K.; Amadeus, M.; Lurmann, F.; Gilliland, F.; McConnell, R.; Hodis, H.N.; Künzli, N. Prenatal air pollution exposure and early cardiovascular phenotypes in young adults. PLoS ONE 2016, 11, e0150825. [Google Scholar] [CrossRef]
- Cohen, A.J.; Brauer, M.; Burnett, R.; Anderson, H.R.; Frostad, J.; Estep, K.; Balakrishnan, K.; Brunekreef, B.; Dandona, L.; Dandona, R. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the global burden of diseases study 2015. Lancet 2017, 389, 1907–1918. [Google Scholar] [CrossRef]
- Velazquez, M.A.; Fleming, T.P.; Watkins, A.J. Periconceptional environment and the developmental origins of disease. J. Endocrinol. 2019, 242, T33–T49. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rodríguez, P.; Ramiro-Cortijo, D.; Reyes-Hernández, C.G.; de Pablo, L.A.L.; González, M.C.; Arribas, S.M. Implication of oxidative stress in fetal programming of cardiovascular disease. Front. Physiol. 2018, 9, 602. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Huang, S.; Jiao, A.; Yang, X.; Yun, J.; Wang, Y.; Xue, X.; Chu, Y.; Liu, F.; Liu, Y. Association between ambient fine particulate matter and preterm birth or term low birth weight: An updated systematic review and meta-analysis. Environ. Pollut. 2017, 227, 596–605. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M.; Higgins, J.P.; Hedges, L.V.; Rothstein, H.R. Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Res. Synth. Methods 2017, 8, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Belbasis, L.; Savvidou, M.D.; Kanu, C.; Evangelou, E.; Tzoulaki, I. Birth weight in relation to health and disease in later life: An umbrella review of systematic reviews and meta-analyses. BMC Med. 2016, 14, 147. [Google Scholar] [CrossRef]
- Dadvand, P.; Parker, J.; Bell, M.L.; Bonzini, M.; Brauer, M.; Darrow, L.A.; Gehring, U.; Glinianaia, S.V.; Gouveia, N.; Ha, E.H.; et al. Maternal exposure to particulate air pollution and term birth weight: A multi-country evaluation of effect and heterogeneity. Environ. Health Perspect. 2013, 121, 267–373. [Google Scholar] [CrossRef]
- Sapkota, A.; Chelikowsky, A.P.; Nachman, K.E.; Cohen, A.J.; Ritz, B. Exposure to particulate matter and adverse birth outcomes: A comprehensive review and meta-analysis. Air Qual. Atmos. Health 2012, 5, 369–381. [Google Scholar] [CrossRef]
- Lamichhane, D.K.; Leem, J.H.; Lee, J.Y.; Kim, H.C. A meta-analysis of exposure to particulate matter and adverse birth outcomes. Environ. Health. Toxicol. 2015, 30, e2015011. [Google Scholar] [CrossRef]
- Stieb, D.M.; Chen, L.; Eshoul, M.; Judek, S. Ambient air pollution, birth weight and preterm birth: A systematic review and meta-analysis. Environ. Res. 2012, 117, 100–111. [Google Scholar] [CrossRef]
- Zhu, X.; Liu, Y.; Chen, Y.; Yao, C.; Che, Z.; Cao, J. Maternal exposure to fine particulate matter (PM 2.5) and pregnancy outcomes: A meta-analysis. Environ. Sci. Pollut. Res. 2015, 22, 3383–3396. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Yang, M.; Zhu, Z.; Sun, S.; Zhang, Q.; Cao, J.; Ding, R. Maternal exposure to air pollution and the risk of low birth weight: A meta-analysis of cohort studies. Environ. Res. 2020, 190, 109970. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Chen, Y.; Mi, B.; Dang, S.; Zhao, D.; Liu, R.; Wang, H.; Yan, H. Ambient air pollution and adverse birth outcomes: A systematic review and meta-analysis. J. Zhejiang Univ. Sci. B 2019, 20, 238–252. [Google Scholar] [CrossRef] [PubMed]
- Ji, Y.; Song, F.; Xu, B.; Zhu, Y.; Lu, C.; Xia, Y. Association between exposure to particulate matter during pregnancy and birthweight: A systematic review and a meta-analysis of birth cohort studies. J. Biomed. Res. 2019, 33, 56–68. [Google Scholar]
- Fleischer, N.L.; Merialdi, M.; van Donkelaar, A.; Vadillo-Ortega, F.; Martin, R.V.; Betran, A.P.; Souza, J.P.; O’Neill, M.S. Outdoor air pollution, preterm birth, and low birth weight: Analysis of the world health organization global survey on maternal and perinatal health. Environ. Health Perspect. 2014, 122, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Shu, L.; Sheng, J.; Mu, M.; Wang, S.; Tao, X.; Xu, S.; Tao, F. Birth weight and risk of coronary heart disease in adults: A meta-analysis of prospective cohort studies. J. Dev. Orig. Health Dis. 2014, 5, 408–419. [Google Scholar] [CrossRef] [PubMed]
- Knop, M.R.; Geng, T.; Gorny, A.W.; Ding, R.; Li, C.; Ley, S.H.; Huang, T. Birth weight and risk of Type 2 diabetes mellitus, cardiovascular disease, and hypertension in adults: A meta-analysis of 7,646,267 participants from 135 studies. J. Am. Heart Assoc. 2018, 7, e008870. [Google Scholar] [CrossRef]
- Mohseni, R.; Mohammed, S.H.; Safabakhsh, M.; Mohseni, F.; Monfared, Z.S.; Seyyedi, J.; Mejareh, Z.N.; Alizadeh, S. Birth weight and risk of cardiovascular disease incidence in adulthood: A dose-response meta-analysis. Curr. Atheroscler. Rep. 2020, 22, 1–13. [Google Scholar] [CrossRef]
- Woodruff, T.J.; Parker, J.D.; Darrow, L.A.; Slama, R.; Bell, M.L.; Choi, H.; Glinianaia, S.; Hoggatt, K.J.; Karr, C.J.; Lobdell, D.T.; et al. Methodological issues in studies of air pollution and reproductive health. Environ. Res. 2009, 109, 311–320. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, M.J.; Dadvand, P.; Grellier, J.; Martinez, D.; Vrijheid, M. Environmental risk factors of pregnancy outcomes: A summary of recent meta-analyses of epidemiological studies. Environ. Health 2013, 12, 6. [Google Scholar] [CrossRef]
- Johnston, H.J.; Mueller, W.; Steinle, S.; Vardoulakis, S.; Tantrakarnapa, K.; Loh, M.; Cherrie, J.W. How harmful is particulate matter emitted from biomass burning? A Thailand perspective. Curr. Pollut. Rep. 2019, 5, 353–377. [Google Scholar] [CrossRef]
- Burnett, R.; Chen, H.; Szyszkowicz, M.; Fann, N.; Hubbell, B.; Pope, C.A., 3rd; Apte, J.S.; Brauer, M.; Cohen, A.; Weichenthal, S.; et al. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl. Acad. Sci. USA 2018, 115, 9592–9597. [Google Scholar] [CrossRef] [PubMed]
| Descriptive Information on Meta-Study and All Input Studies | Meta-Risk Estimates for Specific Analyses | ||||||
|---|---|---|---|---|---|---|---|
| Reference | Country/Region | Range of Participants/Births | Exposure Range (Using Study Metrics) | Adjusted for/Subgroup | Studies Included in Risk Estimate Analysis (n) | OR/RR (95% CI), PM2.5 per 10 µg/m3 Increment | Heterogeneity (I2) |
| Sapkota et al. 2012 (*) [28] | USA (n = 9), Canada and Taiwan (n = 2 each), Germany, Brazil, Korea and (n = 1 each) | Participants: 128 to 374,167; Cases: 69 to 21,450 | Range of PM2.5 means (where reported): 5.1–11.9 µg/m3; Range of PM2.5 medians (where reported): 13.5–14.4 µg/m3 | NA | 4 | 1.09 [0.90, 1.32] | 57.4% |
| Stieb et al. 2012 [30] | North America (n = 27), Europe (n = 18), Asia (n = 10), Australia (n = 4), South America (n = 3) | Births: 153 to 3,303,834 | PM2.5 Min./Max. average 24 h concentrations (µg/m3) among all studies: Min. 1.8 Max. 44.2 | NA | 6 | 1.05 [0.99, 1.12] | 85.5% |
| Dadvand et al. 2013 (*) [27] | North America (6), Europe (5), South America (1), Asia (1), Oceania (1) | Births: ~1000 to ~2 m | Range of PM2.5 medians (where reported): 3.98–20.3 µg/m3 | NA | 7 | 1.17 [1.08, 1.26] | 92.3% |
| Adjusted for maternal SES | 1.10 [1.03, 1.18] | 89.7% | |||||
| Adjusted for maternal SES and centre specific covariates ** | 1.04 [0.99, 1.09] | 68.5% | |||||
| Zhu et al. 2015 [31] | USA (n = 17), Canada (n = 2), Australia (n = 2), Netherlands, UK, Poland and Norway (n = 1 each) | Study population: 481 to 1,5480,904 | NA | NA | 6 | 1.05 [1.02, 1.07] | 39.70% |
| Sun et al. 2016 [7] | USA (n = 23), Multi-country (n = 2), Canada, Spain, Netherlands, UK, Poland, Norway, Australia (n = 1 each) | Participants: 481 to 3,545,177 | Range of PM2.5 (where reported): 5.1–43.8 µg/m3; Except (Fleischer et al., 2014 [35]): 1.4–98.1 µg/m3 | 19 | 1.09 [1.03, 1.15] | 92.6% | |
| USA | 14 | 1.08 [1.02, 1.14] | 94.3% | ||||
| Other setting | 5 | 1.14 [1.04, 1.25] | 36.1% | ||||
| Li et al. 2017 (*) [24] | USA n = 17, Canada n = 2, Europe n = 3, other n =1 | Births: 3853 to 3,545,177 | Range of PM2.5 means (where reported) 1.82–22.11 µg/m3 | NA | 4 | 1.05 [0.98, 1.12] | 85.0% |
| Guo et al. 2019 [33] | USA (n = 17), Canada (n = 4), Brazil and China (n = 3 each), Spain, Australia, South Korea, and multi-country (n = 2 each), Iran, UK, Taiwan, Norway, Sweden, and Japan (n = 1 each) | Births: 225 to 2,402,545 | NA | NA | 6 | 1.00 [0.98, 1.03] | 73.3% |
| Ji et al. 2019 [34] | USA and Canada (n = 3 each), Iran, Korea, Netherlands, Taiwan, Brazil, UK, Spain, multi-country (n = 1 each) | Births: 225 to 423,719 | NA | NA | 6 | 1.04 [0.99, 1.09] | 67.4% |
| Li et al. 2020 *** [32] | USA (n = 20), China (n = 9), Korea (n = 5), Canada (n = 4), Japan, Lithuania, Spain, UK (n = 2 each), Australia, Czech republic, India, Iran, Peru, Poland, Puerto Rico, multi-country (n = 1 each) | 225 to 3,545,177 | NA | 29 | 1.08 [1.04, 1.12] | 86.0% | |
| The Americas | 18 | 1.07 [1.02, 1.12] | >50% | ||||
| Asia | 7 | 1.04 [0.99,1.10] | >50% | ||||
| Europe | 4 | 1.38 [1.19, 1.59] | <50% | ||||
| Descriptive Information on Meta-Study and All Input Studies | Meta-Risk Estimates for Specific Analyses | ||||||
|---|---|---|---|---|---|---|---|
| Reference | Country/Region | Range of Participants/Births | Exposure Range (using Study Metrics) | Adjusted for/Subgroup | Studies Included in Risk Estimate Analysis (n) | Change in BW (g) (95% CI), PM2.5 per 10 µg/m3 Increment | Heterogeneity (I2) |
| Stieb et al. 2012 [30] | North America (n = 27), Europe (n = 18), Asia (n = 10), Australia (n = 4), South America (n = 3) | Births: 153 to 3,303,834 | PM2.5 Min./Max. average 24-hour concentrations (µg/m3) among all studies: Min. 1.8 Max. 44.2 | 7 | −23.4 [−45.5, −1.4] | 94.7% | |
| Lamichhane et al. 2015 [29] | North America (n = 25), Asia (n = 7), Europe (n = 6), Australia (n = 4), and South America (n = 2) | Births: 235 to 3,303,834 | Range of PM2.5 means (where reported): 9.4–21.3 µg/m3 | Combined studies * | 8 | −13.88 [−15.7, −12.06] | 47.5% |
| Adjusted for maternal smoking | 7 | −22.17 [−37.93, −6.41] | 92.3% | ||||
| Zhu et al. 2015 [31] | USA (n = 17), Canada (n = 2), Australia (n = 2), Netherlands, UK, Poland and Norway (n = 1 each) | Population: 481 to 1,548,904 | NA | 12 | −14.58 [−19.31, −9.86] | 86.8% | |
| Sun et al. 2016 [7] | USA (n = 23), Multi-country (n = 2), Canada, Spain, Netherlands, UK, Poland, Norway, Australia (n = 1 each) | Participants: 481 to 3,545,177 | Range of PM2.5 means (where reported): 5.1–43.8 µg/m3; Except (Fleischer et al., 2014 [35]): 1.4–98.1 µg/m3 | 17 | −15.9 [−26.8, −5.0] | 98.5% | |
| USA | 13 | −18.8 [−31.4, −6.3] | 99.0% | ||||
| Other settings | 4 | −1.8 [−12.2, 8.7] | 26.2% | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steinle, S.; Johnston, H.J.; Loh, M.; Mueller, W.; Vardoulakis, S.; Tantrakarnapa, K.; Cherrie, J.W. In Utero Exposure to Particulate Air Pollution during Pregnancy: Impact on Birth Weight and Health through the Life Course. Int. J. Environ. Res. Public Health 2020, 17, 8948. https://doi.org/10.3390/ijerph17238948
Steinle S, Johnston HJ, Loh M, Mueller W, Vardoulakis S, Tantrakarnapa K, Cherrie JW. In Utero Exposure to Particulate Air Pollution during Pregnancy: Impact on Birth Weight and Health through the Life Course. International Journal of Environmental Research and Public Health. 2020; 17(23):8948. https://doi.org/10.3390/ijerph17238948
Chicago/Turabian StyleSteinle, Susanne, Helinor J. Johnston, Miranda Loh, William Mueller, Sotiris Vardoulakis, Kraichat Tantrakarnapa, and John W. Cherrie. 2020. "In Utero Exposure to Particulate Air Pollution during Pregnancy: Impact on Birth Weight and Health through the Life Course" International Journal of Environmental Research and Public Health 17, no. 23: 8948. https://doi.org/10.3390/ijerph17238948
APA StyleSteinle, S., Johnston, H. J., Loh, M., Mueller, W., Vardoulakis, S., Tantrakarnapa, K., & Cherrie, J. W. (2020). In Utero Exposure to Particulate Air Pollution during Pregnancy: Impact on Birth Weight and Health through the Life Course. International Journal of Environmental Research and Public Health, 17(23), 8948. https://doi.org/10.3390/ijerph17238948








