Abstract
Background: The traditional home care model entails caring “for” people with disabilities, not “with” them. Reablement care has been applied to long-term care, but the evidence for care attendants, home care recipients, and family caregivers simultaneously is limited. Methods: First, a survey was conducted to explore the needs of home care recipients and family caregivers to achieve independence at home to develop the reablement home care model for home care. Then, an intervention with two groups was implemented. The experimental group included a total of 86 people who participated in the reablement home care model. The control group included 100 people and received usual home care. The self-reliance concept, job satisfaction, and sense of achievement for care attendants; quality of life for home care users; and caregiving burden for family caregivers were assessed. Results: The reablement home care model improved the job satisfaction and achievement of home care attendants, improved mutual support and independence in the self-reliance concept and quality of life among the users, and reduced the stress of the users and family caregivers. Conclusion: The reablement home care model improved the outcomes for providers, care recipients, and family caregivers. Reablement home care is suggested in long-term care policies.
1. Introduction
Home care (HC) aims to provide intermittent care for people with disabilities living in the community to advocate aging in place. The broad definition of HC usually includes medical, home medical, or nursing care, as well as home services that provide personal care and assistance with housework for people with disability at their homes [1]. Due to various complicated care needs and differences in home settings, HC can be both helpful and challenging. Past studies have already provided evidence that HC services can improve the physical function and quality of life of people with disabilities and reduce the burden on family caregivers [2,3]. However, HC is not a panacea. HC recipients may depend on home help too much and hesitate to do the housework that they are capable of doing by themselves [4]. In such cases, the potential of HC recipients to recover their physical function is not optimized. At times, care recipients or family caregivers might abuse HC attendants by having them perform house chores that are unrelated to the care itself and are usually performed as a system of uniform care. Person-centered care should emphasize autonomy and choice for health care recipients [5,6]. Thus, the home care that is provided to each person with a disability should be tailored to his or her own needs, preferences, and choices [7,8]. Furthermore, despite the increased expenditure associated with HC services, the independence of people with disabilities has not improved, and their quality of life worsens as their physical function declines [9]. The ability people with disabilities have to fit their home environment may be reduced due to their disabilities, and thus person–environment fit may also influence the effects of HC services. The provision of home care that fits the home environment of people with disabilities should be personalized. Therefore, a new care model called reablement care has been developed and implemented in long-term care institutions and HC settings. In this study, we aimed to establish a reablement model for HC services and to evaluate the effectiveness of this model for care attendants, care recipients, and family caregivers. The term “home care” (HC) in this study refers to personal care and housework provided for people with disabilities at home in the community and does not include medical and nursing care, and we use the term “RHC” for the reablement model of home care. In Taiwan, the requirement for people with disabilities to receive HC is a disability lasting for more than 6 months. Thus, home care is primarily provided as long-term care rather than subacute care.
The traditional HC model entails caring “for” a person with a disability and not “with” them. This care model was suggested to cause dependency and further loss of function for care recipients [4]. A new concept, i.e., reablement, aims to help people with disabilities recover their physical function through performing activities of daily living rather than having formal or informal caregivers perform these activities for them [10], focusing on supporting independence [11]. Reablement and rehabilitation are different: Reablement aims to reduce the need for long-term care by helping recipients regain confidence and learn the skills needed to maximize their independence, whereas rehabilitation aims to restore physical function to achieve the highest level [12]. Rehabilitation is a part of medical care and is often applied at the subacute care stage for persons who have a good chance of recovering completely. Although home-based rehabilitation is also available in some home care services in Taiwan, the traditional HC model used in this study did not cover home-based medical care, nursing care, or rehabilitation. In contrast, long-term care recipients with disabilities are usually unable to completely recover. In other words, rehabilitation aims to cure, but reablement aims to improve or maintain independence. Reablement often assists people with disabilities in setting their own goals to achieve independence not only by health care professionals but also by care attendants and family caregivers. Therefore, the reablement model is person-centered, preference-based care and emphasizes self-determination. The home care model in this study does not include medical care. Home care attendants can assist personal care-oriented home care for reablement.
The reablement concept is practiced at home [13]. The priority for daily activities is determined by the individuals so that timely rehabilitation and practice of daily activities can be designed and provided [14]. Lewin [15] suggests the following principles for the practice of reablement: real needs in formal care, time limit on the intervention (usually 6–12 weeks), intense intervention provided at the care recipient’s home, maximizing independence, person-centered, and goal-oriented.
This type of model has been applied for the care of people with disabilities. In the United Kingdom, Australia, and Scandinavian countries, this model has been applied in community-based care [12,16,17], whereas in New Zealand, Japan, and Taiwan, similar models, usually called self-reliance or self-support models, are applied in long-term care institutions [18,19,20]. Some empirical evidence shows that such reablement or restorative care models may improve physical function [16,18,21]. Client-centered home care may be responsive in time, safe, and improve the continuity of care [22]. By strengthening intrinsic motivation via the participant’s willpower, responsibility, and confidence, the skills needed to perform daily activities can be improved and maintained [13]. Most importantly, client-centered home care emphasizes the need for personalized customization [23]. The cost of care can be reduced by improving physical independence [24]. However, the effects of such reablement programs on care recipients’ autonomy and willpower have not been assessed. The effects of these programs on physical function or mortality are unconfirmed [17,18,25]. The effectiveness of such reablement projects on care attendants and family caregivers has only been assessed by limited research. Restorative care may improve family caregivers’ health-related quality of life [18], and family caregivers can gain more free time when reablement helps to improve the patient’s physical functions [26].
The HC model in Taiwan is primarily conducted in the traditional way. In this study, we aim to develop an RHC model for older adults with disabilities in the community through a quasi-experimental design to compare the effects of the RHC model and the traditional HC model on care attendants, care recipients, and their family caregivers.
2. Materials and Methods
This study consisted of two stages. First, a survey was conducted to determine the most important independence needs when designing an RHC model. Then, an experimental design was implemented to compare the effects of RHC and traditional HC on care attendants. The study gained approval from the relevant medical research ethical committees before conduction (JEN-AI IRB106-07).
2.1. Needs Assessment for Setting Priorities to Establish the RHC Model
We used a survey to explore participants’ needs in HC. In total, 210 care attendants, 55 HC recipients, and 65 family caregivers from two home care agencies participated in the survey. The recipients and their family caregivers were asked about their disability level and the daily activities they hoped to improve. The care attendants were asked about their needs when providing HC and rated their own professional knowledge and skills (Table 1). The most prevalent functional impairments in activities of daily living (ADLs) were taking baths, dressing, and transferring, and the most prevalent functional limitations in instrumental activities of daily living (IADLs) were heavy housework, going out by taking a car or train alone, and light housework. We also listed the expectations of the daily activities to be improved from the home care recipients and family caregivers and the most needed skills in home care from care attendants. The priority needs in home care for people with disabilities were bathing, taking a car or train alone, housework, and dressing; the priority needs in home care for family caregivers were bathing, walking, and going outside. The priority needs for care attendants to learn in home care skills were transferring, passive motion exercise, and using assistive devices. The common priorities for RHC by HC recipients, family caregivers, and care attendants were transferring and mobility as well as personal hygiene, and bathing knowledge and skills related to other care needs were provided as well. Thus, these items were set as the priority to be included in the RHC program.

Table 1.
Needs assessment of the reablement home care items reported by care recipients, family caregivers, and care attendants.
The RHC program was developed by a team that was led by the researcher, who has degrees in both nursing and social work and familiarity with RHC, and consisted of a physical therapist, a nurse, a social worker, and the related staff in the home care agencies. Before the program started, the researchers communicated with the professionals about the concept of reablement and the way to deliver training for care attendants. The structure of the program to empower the care attendants was designed according to the independent care plan guide [27] (Supplemental Table S1). The training course for developing the RHC program included the concepts and skills needed for reablement in home care, and the advanced skills from the expectations based on the needs assessment survey were strengthened in the course. The main priorities for RHC were the core skills needed to empower care attendants. For example, if the most necessary skill was about transferring care, then the skill was taught by a physical therapist in the training program for care attendants. When the RHC program started, the participants (both home care recipients and their family caregivers) were asked about their special needs for their functional improvement (one or two items), and then, the care attendants developed their personalized care plan for RHC. If the care attendants needed extra mentoring regarding the care skills needed to meet the special needs of the participants, then they were able to participate in periodic meetings to consult with cross-disciplinary professionals to receive advice or further training.
2.2. Recruitment, Implementation, and Evaluation of the Intervention
Two HC agencies participated in this survey. One home care agency was recruited as the experimental group and implemented the RHC program; the other agency was invited as the control group and implemented traditional HC service. The inclusion criteria for the participants in the two groups were older adults aged 65 years and above with a disability who were able to communicate, intact cognitive function (records from the agencies), and willing to participate in the program. The existing home care recipients and their family caregivers in these two agencies were approached and invited to participate in this study. When they understood the whole program and agreed to participate in the program, consent was provided, and the process was assessed every month during the study. The RHC group consisted of 33 pairs of care recipients and family caregivers with 20 care attendants, whereas the traditional HC (control) group consisted of 40 pairs of care recipients and family caregivers with 20 care attendants (see Figure 1). The intervention was conducted for 3 months.
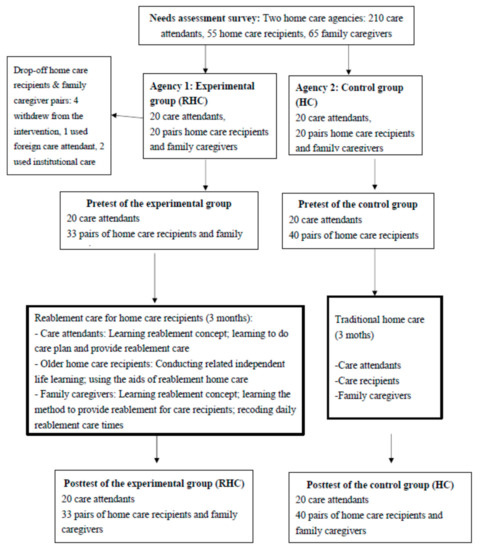
Figure 1.
Flow chart of the intervention of the reablement home care model.
The care attendants in the experimental group participated in the empowerment training program. The knowledge and skills learned by the care attendants were assessed by testing their knowledge and skills after the training and during three meetings hosted by the researcher and the care attendants during the program to solve the challenges of the RHC model.
Both the RHC recipients and their family caregivers in the experimental group were introduced to the new care model and agreed to participate in the study. In the RHC model, not only were new methods of care given to them but they also learned how to use assistive devices to improve home care recipients’ independence, and the family caregivers learned how to assist the care recipients in achieving the goal of self-reliance. The care attendants needed to work with the family caregivers to identify the most needed care items through communication, set care goals together, and help family caregivers provide RHC for the care recipients with disabilities that would encourage the care recipients’ willingness to be self-reliant and independent.
During the intervention, periodic meetings were conducted each month, not only to provide consultations with cross-disciplinary professionals to give advice or further training but also to collect qualitative observations and opinions from the care attendants during the program. The observations from the care attendants were recorded to improve the care delivery or to modify the care plan for process evaluation.
2.3. Measures
2.3.1. Main Dependent Variable: The Self-Reliance Concept on the HC Scale
The self-reliance concept on the HC scale was based on the dynamic self-determination model [28] and modified (see Supplemental Table S2). The scale was validated by three experts in the fields of nursing, social work, and long-term care policy. The scale was tested and modified before formal application. Dependence was defined as the extent to which home attendants, home care recipients, and family caregivers depended on HC services to address their functional limitations. Mutual support was defined as the knowledge and skills that the family caregivers perceived themselves as having regarding assistance with care needs and their willingness to collaborate with the HC attendant to provide care by setting appropriate goals and learning care skills. There were 11 items in this domain for the HC attendants and care recipients and 10 items for the family caregivers. Independence was defined as the belief, willingness, and ability to help the care recipients with self-care activities to maximize their independence in HC. Each item was scored from 1 to 5. The Cronbach’s α of the scale ranged from 0.71 to 0.78, indicating satisfactory internal consistency. The development of the scale was reported previously [29].
2.3.2. Variables for the Care Attendants
The HC competency test included a knowledge test of RHC and a practical skills test with scores ranging from 0 to 100. The control group was only tested on the concept of self-reliant support HC because there was no training intervention. Job satisfaction of the HC attendants included 11 items, and each item was scored from 1 to 5. The sense of accomplishment scale described the perceived achievements of the HC attendants in their job. There were 10 items on this scale, scored from 1 to 5 for each item. Demographics included gender, age, education level (elementary school or lower, junior high school, senior high school, college, university and above), marital status (having spouse or having no spouse), ethnic group, religious beliefs, work experience (years), and work hours per month.
2.3.3. Variables for the Care Recipients
Disability level was measured by the Barthel Index [30], which categorizes the disability level into mild (score 91–99), moderate (score 60–90), and severe (score < 60). Cronbach’s α was 0.89, with a measurement of 10 items scored on scales of 0, 5, or 10 points. The total scores were categorized as follows: completely dependent (0~20), heavily dependent (21~61), moderately dependent (62~90), and independent (91~99). The self-care difficulty for 10 daily living activities was self-rated, including dressing and undressing, bathing, dining, taking medication, personal hygiene, transferring, bowel control, bladder control, ability to use assistive devices, and ability to perform general daily activities. Each item was rated as no difficulty, slightly difficult, very difficult, or not possible at all (scored 0 to 3); the total score ranged from 0 to 30. The WHO Quality of Life-BREF [31] was used to measure the care recipients’ health-related quality of life. There were 28 items on this scale, and each item was scored from 1 to 5. Demographics included age, gender, education, marital status, ethnic group, religious beliefs, and disability level (mild/moderate/severe).
2.3.4. Variables for the Family Caregivers
The level of difficulty of caring for the care recipients was assessed for the following 10 items: dressing and undressing, bathing, eating, taking medication, personal hygiene, transferring, bowel control, bladder control, ability to use assistive devices, and ability to perform general daily activities. Each item was rated as presenting no difficulty, a slight difficulty, a great deal of difficulty, or not possible at all (scored 0 to 3). The total score ranged from 0 to 30. The family caregiving burden was measured by the 14-item Family Caregiving Burden scale [32], and each item was scored from 0 to 3. Demographics included age, gender, education, marital status, caregiving experience (years), and the relationship to the care recipients.
2.4. Analysis
Descriptive analysis was conducted, and the chi-square test, paired t-test, and one-way ANOVA were performed. The generalized estimation equation (GEE) [33] was used to examine the effect of the interventions by controlling for covariates. IBM SPSS 22.0 software (IBM, Armonk, NY, USA) was used for the analyses.
3. Results
Table 2 shows the descriptive data for the care attendants in the experimental group and the control group. The characteristics of the two groups were generally similar, except the characteristics of the care attendants at baseline.

Table 2.
Description of the sample: care attendants.
Table 3 shows the descriptive characteristics of the care recipients and their family caregivers in the two groups at baseline. The HC users in the experimental group were younger and more likely to be male than those in the control group. The caregiving burden was higher in the experimental group at baseline.

Table 3.
Description of the sample: home care users and family caregivers.
Table 4 shows the results of pretest and post-test scores on the self-reliance HC scale. The RHC care attendants’ dependence was reduced and mutual support and independence were increased after the intervention. Both the care recipients and family caregivers reported a significant decrease in their dependence after the intervention. The RHC care attendants reported lower dependence but higher mutual support than the care recipients and family caregivers after the intervention. The self-reliance concept for the care attendants or the care recipients in the control group did not change. However, the family caregivers of the control group indicated that mutual support and independence increased over time.

Table 4.
Pretest and post-test of the self-reliance home care scale rated by the care attendants, home care recipients, and family caregivers.
Table 5 shows the results of the GEE analysis of the effects of the self-reliance HC program by comparing the experimental group and the control group. The term “group* time” indicates the effect of the self-reliance HC intervention on the experimental group compared with the effect of traditional HC on the control group. Due to the limited number of cases, only covariates that were significant in the bivariate analysis were included in the models.

Table 5.
Effects of self-reliance support intervention on the care attendants, care recipients, and family caregivers by the generalized estimating equation.
After the intervention, compared with the control group, the care attendants in the experimental group who had received the self-reliance HC training had a higher training score (β = 14.66), higher job satisfaction (β = 3.35), and higher sense of achievement (β = 5.10) and rated the care recipients as having lower dependence (β = −0.505), higher mutual support (β = 11.70), and higher independence (β = 6.75) after the intervention. Regarding the care recipients, satisfaction with the HC agency increased (β = 2.79) and quality of life improved (β = 7.77). Family caregivers indicated an increased self-reliance independence level (β = 6.44) and a reduced caregiving burden (β = −2.79) after the intervention.
4. Discussion
This quasi-experimental study established a new RHC model and evaluated its effects on care attendants, care recipients, and family caregivers. The intervention was found to be beneficial for the care attendants’ perception of their self-reliance HC skills, job satisfaction, and sense of achievement at work and led to higher mutual support and independence among their care recipients. The RHC recipients indicated that the new care model improved their quality of life and reported higher satisfaction with the HC provider. The RHC model increased the perceived independence of the family caregivers and reduced their caregiving burden.
4.1. Effects for Home Care Recipients
The reablement intervention was shown to improve quality of life; although the difficulty with self-care did not change significantly, in contrast with the improvement in physical function reported in previous studies [16,19,21]. However, the intervention helped to reduce the care recipients’ perceived dependence and increase mutual support, although the change was not significant. Because the disability level is often unable to be recovered completely, maintaining current physical function for as long as possible should be the goal. In addition, it is possible that physical function was not sensitive enough to such a short-term intervention and required more time to change participants’ mindset and behaviors from mutual support to independence. In this study, the duration of the program was set to 3 months according to the existing literature [15]. The item number for developing care plans in RHC was set to 1 or 2. Under this short-term period and with limited items for functional reablement, it was easier and practical for home care recipients and care attendants to perform such an RHC care plan.
4.2. Effects for Family Caregivers
Previous research has indicated that reablement care may improve family caregivers’ quality of life [18] and provide some relief from care [26]. In the current study, the RHC model reduced the caregiving burden and significantly increased the independence concept in caregiving. The involvement and responsibility of the care recipients in the process made them willing to try, and at best, their function could be improved. The change in the mutual support and independence of people with disabilities could help family caregivers feel supported as part of a team with the care recipient and the care attendant. Such support would mean that family caregivers would not need to feel responsible for caring for the person with a disability alone. The increase in the independence concept of family caregivers may also change their expectations of care and ways to care for adults with disabilities. Traditional culture in Taiwan expects family members to care for older adults with disabilities to show their filial piety or ask care attendants to do most of the work, even though adults with disabilities may still have some degree of function. The reablement concept of family caregivers would help them build appropriate expectations in home care and encourage adults with disabilities to improve their physical function as much as possible.
4.3. Effects for Care Attendants
The self-reliance concept of the reablement program affected care attendants by reducing their expectations of care recipients’ dependence while increasing their emphasis on mutual support and independence through HC. The care attendants in the experimental group increased their competency, job satisfaction, and sense of achievement after the intervention. Care attendants are often viewed as semiprofessionals, and their sense of achievement and dignity have usually been neglected. Through the empowerment process, the reablement process gives care attendants more autonomy and a greater sense of achievement in their work [34].
4.4. Process Evaluation
Reablement constitutes a paradigm shift in community medical services from a traditional model that focuses on alternative functions to a supplemented a model centered on activities and independence [35]. The development of the individualized RHC program was challenging for the HC attendants, despite support and assistance from the researchers and professionals in the HC agency. According to the opinions collected during the program, the RHC care attendants reported that it was hard to change the HC method at the beginning. They found that using an authoritative attitude to require care recipients’ cooperation did not help. In contrast, if they acted like a partner and asked the care recipient to be their partner in the reablement activities, the effect was much better. Family caregivers’ attitudes and cooperation were very important to assure the efficacy of the program when the care attendants were not there. Communication skills, such as empathy, listening, and the ability to let the participant be an expert in his or her life situation, are prerequisites for allowing the participants to set their own goals [36]. Some of the care recipients reported that “they feel alive” because they were doing something for themselves, similar to previous findings [26]. Reablement care also increased the interaction between the care recipients and both the care attendants and family caregivers. Trust in the care attendants and the relationship with family caregivers were built through the reablement process.
4.5. Strengths and Limitations
This study has strengths. To the best of our knowledge, this is the first reablement intervention program to consider the effect not only on care recipients but also on caregivers, both formal care attendants and family caregivers. The reablement concept was proven to be feasible in the HC setting and not only in institutions.
This study has limitations. First, the study was conducted in only two HC agencies. The results may not be generalized to other agencies, care recipients, or family caregivers. Second, the sample size was not large, and the study was not a randomized trial due to limitations. It was not possible to use a double-blind design for this study. Third, more time may be needed to show more significant effects of RHC. Fourth, it was not feasible to conduct a randomization intervention because we needed to obtain agreement from the home care agency and the care recipients. Thus, only a quasi-experimental design was conducted. In addition, the competency of care attendants of the RHC program was better than that of the control group, and their working tenure was also longer than that of the control group. RHC care attendants may be more capable of delivering advanced home care skills at baseline. Thus, an advanced statistics method (GEE) was applied. The group difference was controlled in the GEE analysis, and the intervention effect (the time*group term) was still significant, which means that the RHC program did show a significant effect when controlling for group (agency) differences. Fifth, the participants who agreed to participate in the RHC program may have had higher motivation to improve their physical function, and thus the effect for them may have also been better. There may have been a self-selection bias in the participants. Sixth, the study focused on the quantitative outcomes of the program, and only limited qualitative findings were observed in the process. A mixed methodology for evaluating the program is suggested in future research.
5. Conclusions
This study provides evidence regarding the establishment and evaluation of an RHC model for older adults with disabilities. We suggest that additional research on the reablement care model should be developed to further support its effects. If additional evidence in support of reablement care is accumulated, then the RHC model could be incentivized in the payment system to encourage the provision of HC quality in long-term care policy.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/17/23/8784/s1, Table S1. The content of the reablement home care model for empowering the care attendants; Table S2. The self-reliance home care scale.
Author Contributions
Conceptualization, Y.-H.C., H.-C.H., C.-L.C., and C.-F.C.; methodology, Y.-H.C., H.-C.H., C.-F.C., and S.-N.C.-L.; supervision, H.-C.H. and S.-W.H.; validation, C.-L.C., C.-F.C., S.-N.C.-L., Y.-M.C., and S.-W.H.; formal analysis, Y.-H.C. and H.-C.H.; investigation, Y.-H.C.; resources, Y.-H.C. and H.-C.H.; data curation, Y.-H.C.; original draft preparation, Y.-H.C. and H.-C.H.; review and editing, H.-C.H., C.-L.C., C.-F.C., S.-N.C.-L.,Y.-M.C., and S.-W.H.; visualization, C.-L.C., C.-F.C., S.-N.C.-L., Y.-M.C., and S.-W.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
We appreciate the participation of the home care recipients, family caregivers, and the care attendants and staff from two home care agencies.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kane, R.A.; Kane, R.L. Long-Term Care: Principle, Programs, and Policies; Springer: New York, NY, USA, 1987; p. 422. [Google Scholar]
- Bookwala, J.; Zdaniuk, B.; Burton, L.; Lind, B.; Jackson, S.; Schulz, R. Concurrent and long-term predictors of older adults’ use of community-based long-term care services: The caregiver health effects study. J. Aging Health 2004, 16, 88–115. [Google Scholar] [CrossRef] [PubMed]
- Naoki, Y.; Matsuda, Y.; Maeda, I.; Kamino, H.; Kozaki, Y.; Tokoro, A.; Maki, N.; Takada, M. Association between family satisfaction and caregiver burden in cancer patients receiving outreach palliative care at home. Palliat. Support. Care 2018, 16, 260. [Google Scholar] [CrossRef] [PubMed]
- Parsons, J.G.M.; Sheridan, N.; Rouse, P.; Robinson, E.; Connolly, M. A randomized controlled trial to determine the effect of a model of restorative home care on physical function and social support among older people. Arch. Phys. Med. Rehabil. 2013, 94, 1015–1022. [Google Scholar] [CrossRef] [PubMed]
- Kogan, A.C.; Wilber, K.; Mosqueda, L. Person-centered care for older adults with chronic conditions and functional impairment: A systematic literature review. J. Am. Geriatr. Soc. 2016, 64, e1–e7. [Google Scholar] [CrossRef]
- Black, K.; Hyer, K. Person-centered considerations in practice for persons with dementia and their caregivers across the continuum of care. Best Pract. Ment. Health 2010, 6, 33–46. [Google Scholar]
- Jokstad, K.; Skovdahl, K.; Landmark, B.T.; Haukelien, H. Ideal and reality; Community healthcare professionals’ experiences of user-involvement in reablement. Health Soc. Care Community 2019, 27, 907–916. [Google Scholar] [CrossRef]
- Wellin, C.; Jaffe, D.J. In search of “personal care”: Challenges to identity support in residential care for elders with cognitive illness. J. Aging Stud. 2004, 18, 275–295. [Google Scholar] [CrossRef]
- Tessier, A.; Beaulieu, M.D.; Mcginn, C.A.; Latulippe, R. Effectiveness of reablement: A systematic review. Healthc. Policy 2016, 11, 49. [Google Scholar] [CrossRef]
- Cochrane, A.; McGilloway, S.; Furlong, M.; Molloy, D.W.; Stevenson, M.; Donnelly, M. Home-care’re-ablement’services for maintaining and improving older adults’ functional independence (Protocol). Cochrane Libr. 2013, 11, 1–12. [Google Scholar] [CrossRef]
- Langeland, E.; Tuntland, H.; Folkestad, B.; Førland, O.; Jacobsen, F.F.; Kjeken, I. A multicenter investigation of reablement in Norway: A clinical controlled trial. BMC Geriatr. 2019, 19, 29. [Google Scholar] [CrossRef]
- Sims-Gould, J.; Tong, C.E.; Wallis-Mayer, L.; Ashe, M.C. Reablement, reactivation, rehabilitation and restorative interventions with odler adults in receipt of home care: A systematic review. J. Am. Med. Dir. Assoc. 2017, 18, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Hjelle, K.M.; Tuntland, H.; Førland, O.; Alvsvåg, H. Driving forces for home-based reablement; a qualitative study of older adults’ experiences. Health Soc. Care Community 2017, 25, 1581–1589. [Google Scholar] [CrossRef] [PubMed]
- Aspinal, F.; Glasby, J.; Rostgaard, T.; Tuntland, H.; Westendorn, R.G.J. New horizons: Reablement-supporting older people towards independence. Age Ageing 2016, 45, 574–578. [Google Scholar] [CrossRef] [PubMed]
- Lewin, G.; Concanen, K.; Youens, D. The Home Independence Program with non-health professionals as care managers: An evaluation. Clin. Interv. Aging 2016, 11, 807. [Google Scholar] [CrossRef] [PubMed]
- Tuntland, H.; Aaslund, M.K.; Espehaugh, B.; Førland, O.; Kjeken, I. Reablement in community-dwelling older adults: A randomised controlled trial. BMC Geriatr. 2015, 15, 145. [Google Scholar] [CrossRef]
- Legg, L.; Gladman, J.; Drummond, A.; Davidson, A. A systematic review of the evidence on home care reablement services. Clin. Rehabil. 2015, 30, 741–749. [Google Scholar] [CrossRef]
- Parsons, M.; Senior, H.; Kerse, N.; Chen, M.H.; Jacobs, S.; Anderson, C. Randomised trial of restorative home care for frail older people in New Zealand. Nurs. Older People 2017, 29. [Google Scholar] [CrossRef]
- Lin, J.L.; Yu, Y.J. Self-supporting care for Taiwan’s practice. Long-Term Care J. 2017, 21, 15–18. (In Chinese) [Google Scholar] [CrossRef]
- Lin, Y.C.; Huang, L.H. Self-supporting care models for older adults. J. Nurs. 2018, 65, 20–26. (In Chinese) [Google Scholar] [CrossRef]
- Lewin, G.; Miguel, K.D.S.; Knuiman, M.; Alan, J.; Boldy, D.; Hendrie, D.; Vandermeulen, S. A randomized controlled trial of the home independence program, an Australian restorative home-care programme for older adults. Health Soc. Care Community 2013, 21, 69–78. [Google Scholar] [CrossRef]
- Sanerma, P.; Paavilainen, E.; Åstedt-Kurki, P. Home care services for older persons. The views of older persons and family members: A realistic evaluation. Int. J. Older People Nurs. 2020, 15, e12281. [Google Scholar] [CrossRef] [PubMed]
- Tuntland, H.; Kjeken, I.; Folkestad, B.; Førland, O.; Langeland, E. Everyday occupations prioritised by older adults participating in reablement. A cross-sectional study. Scand. J. Occup. Ther. 2020, 27, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Eklund, F.; Treschwo, A.; Ringström, A. Can reablement increase independence and reduce the need for elderly care in a Scandinavian setting? Eur. J. Public Health 2014, 24. [Google Scholar] [CrossRef]
- Cochrane, A.; Furlong, M.; McGilloway, S.; Molloy, D.W.; Stevenson, M.; Donnelly, M. Time-limited home-care reablement services for maintaining and improving the functional independence of older adults. Cochrane Database Syst. Rev. 2016, 10, CD010825. [Google Scholar] [CrossRef] [PubMed]
- Hjelle, K.M.; Alvsvåg, H.; Førland, O. The relatives’ voice: How do relatives experience participation in reablement? A qualitative study. J. Multidiscip. Healthc. 2017, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Goto, J.M. Independence Support Type Care Plan Creation Guide; Gyosei Corporation: Tokyo, Japan, 2016. (In Japanese) [Google Scholar]
- Rice, R. Home Care Nursing Practice: Concepts Application, 4th ed.; Mosby: St. Louis, MO, USA, 2006. [Google Scholar]
- Chiang, Y.H. Self-Reliance Support in Home Care: Model Establishment and Evaluation. Ph.D. Thesis, Department of Healthcare Administration, Asia University, Taichung, Taiwan, January 2019. Available online: https://hdl.handle.net/11296/z6buxu (accessed on 25 November 2020). (In Chinese).
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Yao, G.; Chung, C.W.; Yu, C.F.; Wang, J.D. Development and verification of reliability and validity of the WHOQOL-BREF Taiwan Version. J. Formos. Med. Assoc. 2002, 101, 342–351. [Google Scholar] [PubMed]
- Lin, L.N.; Wu, S.C. Measurement structure of the caregiver burden scale: Findings from a national community survey in Taiwan. Geriatr. Gerontol. Int. 2014, 14, 176–184. [Google Scholar] [CrossRef]
- Liang, K.Y.; Zeger, S.L. Longitudinal data analysis using generalized linear models. Biometrika 1986, 73, 13–22. [Google Scholar] [CrossRef]
- Moe, C.F.; Brinchmann, B.S. Optimising Capasity-A service user and caregiver perspective on reablement. Grounded Theory Rev. 2016, 15, 25–40. [Google Scholar]
- Ryburn, B.; Wells, Y.; Foreman, P. Enabling independence: Restorative approaches to home care provision for frail older adults. Health Soc. Care Community 2009, 17, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Moe, A.; Ingstad, K.; Brataas, H.V. Patient influence in home-based reablement for older persons: Qualitative research. BMC Health Serv. Res. 2017, 17, 736. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).