Abstract
With increasing girls’ enrolment in schools, school preparedness to ensure a menstrual friendly environment is crucial. The study aimed to conduct a systematic review regarding the existing evidence on menstrual hygiene management (MHM) across schools in India. It further aimed to highlight the actions that have been taken by the government to improve the MHM situation in India. We conducted the systematic literature search using PubMed, EMBASE, and Web of Science for searching the peer-reviewed articles and Google Scholar for anecdotal reports published from inception until 30 October 2019. Of 1125 publications retrieved through the search, 183 papers were included in this review, using a priori created data-extraction form. Meta-analysis was used to estimate the pooled prevalence (PP) of MHM practices in schools. Less than half of the girls were aware of menstruation before menarche (PP 0.45, 0.39 to 0.51, I2 = 100.0%, n = 122). Teachers were a less common source of information about menstruation to girls (PP 0.07, 0.05 to 0.08, I2 = 100.0%, n = 86). Separate toilets for girls were present in around half of the schools (PP 0.56, 0.42 to 0.75, I2 100.0%, n = 11). MHM in schools should be strengthened with convergence between various departments for explicit implementation of guidelines.
1. Introduction
Inadequate menstrual hygiene management (MHM) among adolescent girls (15–19 years) is a public health problem, mainly in low and middle-income countries []. With over 0.6 billion adolescent girls (8% of the world’s population), the issue of menstrual hygiene by virtue of its magnitude is an issue of global concern. More than 80 percent of these adolescents reside in the Asian and African continents []. India is home to 243 million adolescents, which accounts for a quarter of the country’s total population []. India has over 355 million menstruating women and girls, but millions of women across the country face uncomfortable and undignified experience with MHM [].
Menstrual hygiene is often regarded as a multi-sectoral issue that requires an integrated action from the Department of Education, Health, Women, and Child Development and Water Sanitation Hygiene (WASH) []. In recent years, we have witnessed a strengthened move by the government towards addressing this public health issue. With the launch of the National Rural Health Mission in 2005, menstrual hygiene promotion was formally included as a key responsibility of the community health workers (Accredited Social Health Activist; ASHA) followed by the implementation of menstrual hygiene promotion scheme for girls in rural areas in 2011 []. In 2015, another milestone was achieved when the Ministry of Drinking Water and Sanitation published guidelines on MHM []. There has been a lot of national and international level push to address this issue through various social media platforms including the making of a film called Padman [], roll out of menstrual hygiene campaigns, performing trials on eco-friendly or biodegradable menstrual products, implementing comprehensive sexuality education in schools, etc. [].
Menstruation among school-age girls is a neglected issue on the implementation front despite the formal inclusion of a menstrual hygiene scheme under the reproductive and child health program by the government of India (in 2011) []. This issue still lacks educational support from health workers, pragmatic guidelines to operationalize MHM in schools, and adequate monetary resources to implement the needed actions. Fear, shame, ongoing social taboos, ignorant unsupportive teachers, lack of water, sanitation, disposal facilities, and privacy, are some of the barriers in building an enabling environment for safe and hygienic menstrual practices within the school premises [,,]. These system-level challenges, in conjunction, not only negatively impact sexual and reproductive health outcomes of adolescent girls but also affects their self-confidence and agency (ability to make a decision and take actions for self) []. The increasing enrolment of girls in secondary and senior secondary schools demands a more comprehensive approach to make schools menstrual hygiene friendly and prevent school dropouts or absenteeism [].
Given that a comprehensive approach to study MHM among schools in India was not made in previous reviews, we chose to conduct a systematic review. The review aimed to objectively summarize the evidence on the actions taken at the school (system)- and policy-level to make schools a menstrual hygiene friendly place for adolescent girls in India.
Research Question
The research question was defined as “Are schools in India menstrual hygiene friendly, and what are the policy-level actions taken by the government of India to make our schools menstrual hygiene friendly?”
2. Materials and Methods
2.1. Literature Search
We used the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) framework for systematic reviews to identify the published and grey literature on school (system-) and policy-level actions []. A systematic literature search was undertaken to identify the evidence using the online databases of MEDLINE (PubMed), EMBASE, and Web of Science, from inception until 30 October 2019. In addition, for the policy-level actions, we did a manual search for the relevant documents through the government of India’s website and Google Scholar. We searched the websites of the four concerned ministries related to MHM, including the Ministry of Health and Family Welfare, Ministry of Women and Child Development, Ministry of Drinking Water and Sanitation, and Ministry of Human Resource Development. Since many papers, project reports, documents, or guidelines are not published in peer-reviewed journals, the Google Scholar search was extended to include the grey literature.
Keywords used for the search across three databases were: (‘Menstruation OR Menstrual OR Menses OR Periods OR Hygien* OR Sanitation OR Sanitary OR Hygiene’) AND (‘School OR Adolescent OR Adolescen* OR Pubescence’ AND ‘Girl OR Women OR female’) AND India. Cross-referencing (screening reference list of included studies) was also used to add other studies of relevance to our review. We did not consider abstracts from conference books, manuscripts, or reports published in any language other than English. Endnote X.8.0.1 (Clarivate Analytics, Philadelphia, US) was used to manage all references identified in the search. All the search results were imported in endnote and duplicates if any were removed.
2.2. Inclusion and Exclusion Criteria
For the purpose of this review, a ‘menstrual hygiene friendly school’ was defined as schools where (1) teachers had adequate knowledge about MHM or teacher was a source of information for MHM (before or after menarche) to girls, (2) school management committees took menstrual health-promoting actions, and (3) there were facilities of clean, separate girls’ toilets, changing rooms, water, soap, safe disposal of used pads, and emergency sanitary pads (sanitation facilities). Furthermore, (4) male sensitization on MHM, (5) girls’ awareness on menstruation before menarche, (6) availability of education material on menstrual hygiene promotion, (7) waste management facilities in school premises, and (8) regular monitoring of the schools for rolling out MHM, were added dimensions of menstrual hygiene friendly schools []. We established inclusion criteria as any publication that described any of the above-said components of menstrual hygiene friendly schools in India for school-level actions (Figure 1). Any study not reporting on any of these eight dimensions was excluded during the screening process. Studies that included girls’ awareness of MHM in their findings but did not mention that they were school-going girls were also excluded from the analysis. For policy-level actions, guidelines, or reports that have specified about the government of India’s actions on MHM promotion in schools were included.
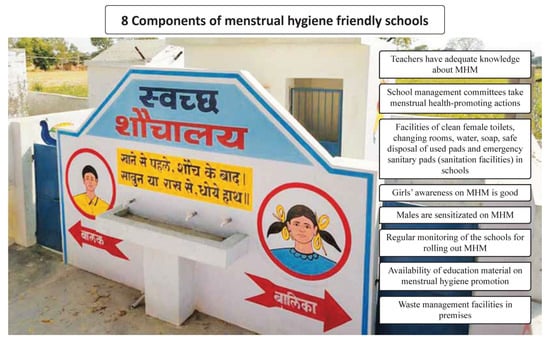
Figure 1.
The figure depicts the photo of a well-designed toilet infrastructure in one of the States in India. Moreover, the figure depicts the eight components of menstrual hygiene friendly schools, which were used as the inclusion criteria for studies in this review. (MHM: Menstrual Hygiene Management).
2.3. Data Analysis
Quality assessment of included studies was performed based on seven criteria as specified in another review []. Each criterion had a value of one or zero. For each study, the results of all the seven criteria were summed to obtain a quality score ranging from 0 to 7. However, studies were not excluded on the basis of a quality score. The quality assessment sheet of the includes studies is provided as Supplementary Table S1. We did not contact the authors of the studies or reports for further information. Two authors (Shantanu Sharma and Devika Mehra) independently reviewed all the titles and abstracts to select the relevant studies. The data on the above-said dimensions, as specified previously, were extracted from the included studies according to a standard form created a priori. Discordance between the two authors was resolved by consensus. The results are presented based on the eight components of menstrual hygiene friendly schools.
Meta-analysis was performed on four out of the eight components of school-level actions as quantitative data were available for only four of them. These four components included teacher as a source of information about MHM (before or after menarche) to girls, separate toilet facilities for girls in schools, awareness of girls on menstruation before menarche, and good disposal facility for sanitary pads in schools. Pooled prevalence (PP) was estimated in a random-effects model using the RevMan version.5.3 software (Cochrane Collaboration, London, UK). Forest plots were generated to display the overall random-effects pooled estimates with 95% confidence intervals. The heterogeneity was quantified using the I2 measure and its confidence interval. We used generic inverse variance method and computation of the standard error was done using the formula: Square Root [(proportion*(1-proportion))/sample size].
3. Results
Of 1125 papers and reports (of which 152 retrieved through cross-referencing and grey literature), 183 were considered eligible (Figure 2). Furthermore, 153 out of 183 were used for the quantitative synthesis of meta-analysis. Most of the studies were of low-to-moderate quality with the combined average score of 2.6. The characteristics of the included papers have been shown in Table 1. The PRISMA framework checklist is provided as Supplementary Table S2. The findings from included papers were presented under two broad themes, namely, school-level (system) actions, and policy-level actions. Under the system-level (school) actions, eight components were included, as defined previously.
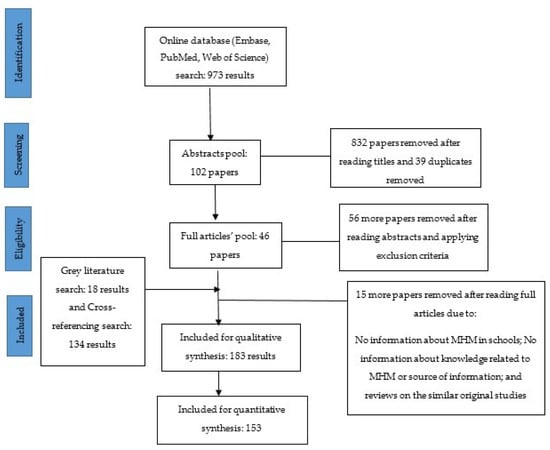
Figure 2.
Search and exclusion criteria for literature review.

Table 1.
Characteristics of included studies related to menstrual hygiene friendly schools published until October 2019.
3.1. School-Level Actions (System)
3.1.1. Menstrual Hygiene Knowledge Among School Teachers
According to our literature review, there was no peer-reviewed publication or anecdotal reports on the knowledge of school teachers regarding menstruation issues in India. The programs that included reproductive health education as a means to disseminate MHM information in schools did not measure or mention this. Moreover, school teachers were reported as the less common source of MHM information among adolescent girls in 74 studies [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,], yet in 12 studies, a large proportion of girls (more than one-fourth) reported that teachers were a common source of information about MHM (Table 2) [,,,,,,,,,,,]. The teachers in those schools were reported to have been supportive []. In addition to these challenges, non-availability or limited availability of female teachers in schools was a serious issue. Despite schools running health programs, teachers found discussing menstruation embarrassing and instruct the students to read that chapter in the textbook at home. As English was not taught in some schools, the use of vernacular terms for human reproductive organs in the local language became very embarrassing for teachers as well as students []. It has been reported that many teachers were insensitive to the physical and mental state of girls during their periods []. Moreover, a study from Tamil Nadu reported that 1.3% of the schoolgirls were scolded by teachers for menstrual problems []. Teachers felt the need to do games and activities to share information about various menstruation-related issues with girls. However, they could not conduct such activities in school because they were pre-occupied with routine duties and curriculum targets []. Teachers were a source of information among 7% girls (PP 7.0%, 95% Confidence Interval (CI) 5.0% to 8.0%, I2 = 100%, n = 86) (Figure 3).

Table 2.
Characteristics of the included studies for teachers as a source of information about menstruation and girls’ pre-menarche awareness.
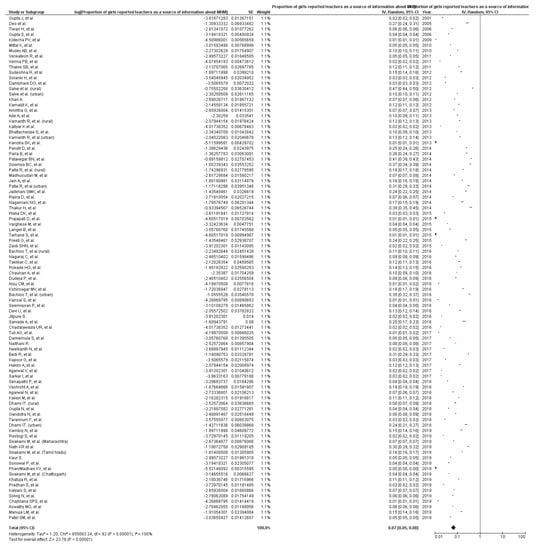
Figure 3.
Pooled prevalence of teachers as a source of information about menstruation to girls in India, from the included studies published until October 2019 (n = 86 studies). CI: Confidence Interval; SE = Standard error. I2: Heterogeneity; Squares represent proportions or prevalence. Lines represent 95% CI. Diamonds represent pooled prevalence.
3.1.2. School Management Committee Taking Menstrual Health-Promoting Actions
The World Health Organization proposed the concept of Health Promoting Schools (HPS) in 1995, which advocated for the total life approach to school-based health promotion while focusing on the curriculum, the school’s ethos, and the environment. The HPS framework emphasized creating a management committee as a support structure for schools to help in planning, designing policies, strategies, and procedures towards health promotion []. Menstrual hygiene promotion could be one of the outcomes of the actions of this committee. However, evidence on the existence of such committees and their commitment to health promotion was limited []. In two intervention studies from Bihar and Chandigarh, the school management committee under the HPS framework was established as an effective means towards promoting health [,]. School management committees were non-functional and completely unaware of their roles and responsibilities [,].
3.1.3. Sanitation Facilities in Schools
Unavailability of disposal mechanisms for pads, poor water supply for washing or flushing, poor hygienic conditions of the toilets, lack of soap, washbasins, mugs for washing in the toilets, and no separate toilets for girls were major WASH challenges girls faced during menstruation. Broken lock/doors of the toilets were a matter of concern for the security of the girls in schools. These findings have been reported in 30 studies [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,]. There were gaps with respect to the non-availability of emergency supplies of sanitary materials in schools [,,,,]. The girls in schools threw away sanitary pads or other menstrual articles in toilets or left the soiled wrapped pads at toilet corners due to lack of dustbins or separate place for disposal. As a result, the sewage system was blocked, or toilets became dirty, a breeding place for flies and mosquitoes, and unhygienic for other toilet users and cleaners [,,]. Less than two-thirds of schools in India had dustbins with a lid for disposing of pads. The proportion of schools with bins having lids for the disposal of sanitary materials was 62%. []. Moreover, only 21% of girls could get pain relievers for menstrual cramps, and 37% told that absorbents were available in schools when needed []. Only 56% (PP 56%) schools in India had separate toilets for girls (95% CI 42% to 75%, I2 = 100%, n = 11) (Figure 4). Table 3 shows the characteristics of some of the studies that reported on the presence of separate toilets for girls in schools.
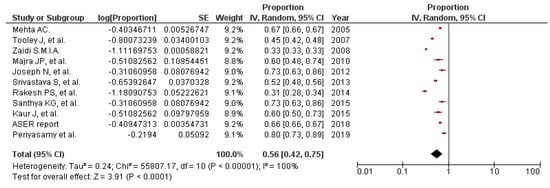
Figure 4.
Pooled prevalence of schools with separate toilets for girls in India, from studies published until Oct 2019 (n = 11). CI: Confidence Interval; SE = Standard error; ASER: Annual Status of Education Report Centre. I2: Heterogeneity. Squares represent proportions or prevalence. Lines represent 95% CI. Diamonds represent pooled prevalence.

Table 3.
Characteristics of the included studies for separate toilet for girls and good disposal facilities for sanitary products.
3.1.4. Sensitization of Boys and Male Teachers on MHM
In 2014, UNESCO, in its technical note, emphasized that male teachers in the schools might not be sensitized to the needs of girls, and hence, did not allow them to visit the toilet during their lecture. Male teachers perceived that girls were not interested in studies []. In other studies, it was reported that teasing by male teachers was common. This insensitive behavior might be fueled by ignorance, prevailing local myths, and cultural taboos related to menstrual blood among men [,]. As a result, topics such as puberty and menstruation were not included in the curriculum due to the predominance of male teachers in most of the schools [,]. There was a higher predominance of male teachers or administrators in schools, and they were hesitant to talk about MHM due to the gendered rooting of menstruation and cultural taboos related to it. It was reported that girls were often teased and subjected to embarrassment by boys and male teachers in schools due to the staining of their clothes during periods []. Moreover, because of the lack of knowledge about menstruation, boys displayed a negative attitude towards menstruation [].
3.1.5. Girls’ Awareness of MHM
Another barrier to a comfortable and dignified experience of MHM among girls was the lack of or limited awareness as reported in 92 studies (Table 2) [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,]. The lack of awareness led girls to think menstruation as a representation of sin, and menstrual blood as an impure entity. Schools were not reported often as a source of menstrual hygiene education []. On the contrary, 34 studies documented that a large proportion of girls (more than two-third) had high knowledge about menstruation [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,]. Among 122 studies with available information, the pooled prevalence of awareness about menstruation before menarche was 45% (95% CI 39% to 51%, I2 = 100%) (Figure 5). There was not much difference in the proportion of girls who were aware about menstruation before menarche between rural and urban areas (around 2%, not shown in the data).
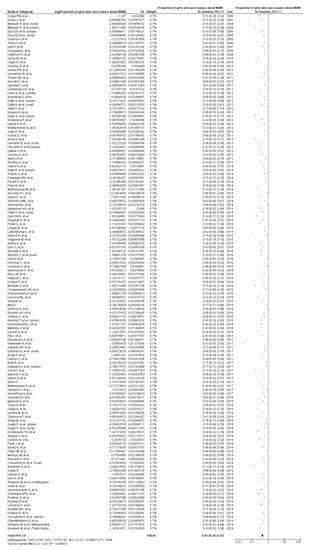
Figure 5.
Pooled prevalence of girls’ awareness about menstruation prior to menarche in India, from studies published until Oct 2019 (n = 122). CI: Confidence Interval; SE = Standard error; I2: Heterogeneity. Squares represent proportions or prevalence. Lines represent 95% CI. Diamonds represent pooled prevalence
3.1.6. Education Material for Menstrual Hygiene Promotion in Schools
Limited data were available related to this component of MHM in schools. The study among schools across three states of India (Chhattisgarh, Maharashtra, and Tamil Nadu) reported that written materials about menstruation were infrequently available (19%) in schools []. In the global baseline report 2018, it was reported that around 64% of schools in India were providing menstrual hygiene education to female students [].
3.1.7. Facilities for Waste Management in Schools
Safe waste management of used sanitary pads in schools was another major issue. Most of the schools lacked any such facility. The lack of facilities discouraged girls from using sanitary pads in schools or attending schools during menstruation [,,,,,]. School sanitation and hygiene education under the total sanitation campaign in Uttar Pradesh, the largest state in India, had the provision of installing incinerators in toilets of secondary schools, but none of the schools implemented the same []. It was reported in a study that only 27% of schools had good disposal facilities for menstrual waste on their premises (Table 3). The most frequently mentioned option for disposal was taking the soiled item home (21%) followed by burn pits (20%), rubbish pits (17%), bins (16%), and incinerator (7%). Incinerators were common in selected states and certain grades of schools []. It has been reported that some schools used incinerators or “feminine hygiene bins” for disposing menstrual waste material, but due to shyness or fear of being seen by others, they were not used. Sanitary napkin vending machines have been installed in toilets of some schools in Kerala, which are semiautomatic and operated by inserting a coin in it. It contained 30–50 sanitary napkins to meet the emergency needs of the girls/women in schools []. In the joint WHO-UNICEF baseline report 2018, it was reported that only 36% of schools in India had functional incinerators for disposal of sanitary wastes. Mizoram is the only state where more than 50% of schools have a functional incinerator for the disposal of sanitary waste. []. Thirty percent of the schools had good disposal facilities for sanitary products (PP 30%, 95% CI 13% to 69%, I2 = 100%, n = 2) (Figure 6).
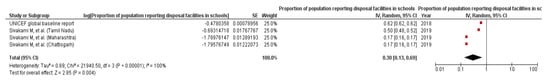
Figure 6.
Pooled prevalence of proportion of girls/student populations reported that schools had good disposal facilities for sanitary products, from studies published until Oct 2019 (n = 2). CI: Confidence Interval; SE = Standard error; I2: Heterogeneity. Squares represent proportions or prevalence. Lines represent 95% CI. Diamonds represent pooled prevalence.
3.1.8. Monitoring of Schools for MHM Friendly Services
The concept of periodic monitoring of the data related to MHM practices in schools was in its nascence, and a key focus on measuring outcome indicators needs to be levied. To our knowledge, there was no school-based data on such measures.
Policy-Level Actions to Address MHM in Schools
The first in the series of national-level directions on MHM for schools was the operational guidelines for the promotion of menstrual hygiene (2012) in rural areas []. The guidelines outlined the strategy to reach school girls through the adolescent education program. The key components of the school-based program were the provision of sanitary napkin distribution, health education, and incinerator for safe disposal. In 2014, the Ministry of health and family program launched the National Adolescent Health Programme known as Rashtriya Kishore Swasthya Karyakaram (RKSK), which levied clear guidelines for providing education, awareness, and support for better MHM using the peer education model. This national program worked at building protective factors that could help adolescents developing ‘resilience’ through both community and school-based interventions []. In the recent five years, sanitation and hygiene received a much-needed impetus from stakeholders of all spheres. With the launch of menstrual hygiene management guidelines in 2015 [], the issue was streamlined into a formal agenda. The action guide laid down the suggestive measures to ensure menstrual hygiene friendly schools. The guidelines addressed the performance measurement with six indicators dedicated to assessing school performance based on MHM. However, there was a lack of detailing on the process and activity-oriented charting of the MHM framework, which schools would follow.
Another milestone in this realm towards filling MHM gaps in schools was a comprehensive WASH assessment tool. It was operationalized in a three-year project led by the Urban Management center and supported by the government of Gujarat []. The tool underscored the need for MHM facilities and IEC across schools besides key components of WASH infrastructure assessment. The initiative (2014–2017) envisaged innovative approaches such as mobile application-based data collection for school sanitation surveys, competition-based approach to WASH improvement named as school swachh survekshan (cleaniness assessment), the concept of creating ‘model school’ based on Indian standard codes and Sarva Shiksha Abhiyan (a program for universal elementary education) standards with a positive environment for integrated learning, sports, recreation, and good access to WASH facilities. This joint action research program involved behavior change approaches such as IEC campaigns, school sanitation clubs, self-assessment tools for monitoring sanitation index, etc. [].
The push for MHM at an international level contributed towards sailing the agenda across nations, including India. Understanding the importance and growing interest in transforming the school environment for menstruating girls and female teachers, the “MHM in ten” members put forward a 10-year agenda (2014–2024). The five key action priorities of the plan revolved around building a strong cross-sector evidence base for MHM in schools, around developing and disseminate guidelines, do evidence-based advocacy, delegate responsibility, and integration with the education system []. The recently released Clean India: Clean Schools handbook underpinned the theme of securing a healthy school environment []. Installation of the napkin-vending machines and environmentally safe disposal mechanisms such as low-cost incinerators attached to the girls’ toilets in schools for disposal of used MHM products were major efforts in this direction. The government launched 100 percent oxy-biodegradable sanitary napkins under the name “Suvidha (facility)”. These sanitary pads were available under the scheme, entitled “Pradhan Mantri Bhartiya Janaushadhi Pariyojana” (Prime Minister Indian People Drug Scheme). The sanitary pads were made available at INR 1 in the drug dispensing stores created under the scheme. These napkins biodegrade automatically when it comes in contact with oxygen after being discarded [].
4. Discussion
Menstrual health promotion in schools remains an issue of concern in India. Limited evidence was available on the different components of menstrual hygiene friendly school. Most of the evidence was available on two components, primarily girls’ awareness about MHM, and sanitation facilities in schools, leaving other components unaddressed. MHM in schools, although it was conceptualized comprehensively with different components as documented in guidelines, the data on its implementation was limited. There was a dearth of literature on education programs focusing on MHM in schools and knowledge, attitude, practices of mentors (teachers) who acted as an immediate source of information to girls. Although the data were available for the source of information about MHM (teachers), the studies on whether teachers as a source of information to girls had adequate knowledge about MHM were not available. We estimated that more than half of the girls did not have information about menstruation prior to menarche. Only 7% of girls reported teachers as a source of information for MHM. Menstruation hygiene education in school has most often being outsourced to non-governmental agencies [,]. Discrimination against female teachers to continue teaching in schools during periods was another example of a social barrier against menstruation. Not only did this practice disrupt the learning process, but it also perpetuated negative images among young minds and society [].
Research evidence revealed that lack of sanitation facilities in schools hindered the ability of girls to manage menstruation healthily, safely, and with dignity. Evidence showed how this aspect affected coping strategies of girls during menstruation []. Only 56% of schools had the facility of a separate toilet for girls. Appropriate menstrual waste disposal facilities were still lacking in the majority of the schools in the country. Studies reported that because of a lack of awareness and sanitation facilities, most of the girls did not change pads in schools [,,]. Despite being emphasized in the education policies, display of MHM messages through information, education, and communication (IEC) materials were not routinely practiced in schools []. IEC materials such as posters, leaflets helped to reinforce the health promotion messages and supporting behavior change at large []. Although online monitoring of some of the WASH indicators in schools was done, MHM components were not included []. A lack of evidence on MHM management information system (MIS) data takes away the system of their efficacy in dealing with this social health problem at a large scale []. Other reviews have reported similar findings on one or more of the eight components of MHM friendly schools in India [,,].
Our review highlighted minimal rural-urban differences in menstrual hygiene practices in schools. However, in the national-level survey, it was reported that more than 50% of the rural girls did not use hygienic methods of menstrual protection (girls who use locally prepared napkins, sanitary napkins, or tampons during their menstrual period) compared to 23% in urban areas []. The plausible explanation for this could be the heterogeneity in the included studies in our review. Furthermore, most of the studies had low quality scores.
It is imperative to emphasize the four primary considerations to build effective evidence on MHM friendly school aspect. These are discussed further, below.
Firstly, pre-service training of teachers on MHM with knowledge assessment at regular intervals is a crucial step in this regard since teachers are viewed as health promoters [,]. Teachers’ knowledge assessment can be a part of the regular school education surveys []. Furthermore, the sensitization of male teachers and boys on MHM is equally important. The provision of MHM-related education materials in schools such as booklets, flipcharts, and modules can be the cornerstone in enhancing the knowledge of teachers and girls [].
The second major issue is the urgent need for improvement in the sanitary facilities at schools. MHM was missing in the majority of the schools []. We found data that highlighted the poor sanitation facilities across the school, and effective implementation and monitoring on this aspect were awaited. Previously published meta-synthesis highlighted that the poorly supportive physical infrastructure, such as a lack of water and sanitation facilities, made it difficult for girls to practice MHM safely []. Waste disposal is of equal concern to make the school environment clean and healthy. The widespread reality of poor sanitary facilities and ignorance about menstruating girls’ needs in schools can make its experience a negative one resulting in increased dropout rates among girls [].
The third major area is the efficient working of the school management committee with an emphasis on MHM services in schools. Regular monitoring and timely actions are crucial to transform poor MHM practices in schools. Lastly, an efficient MIS is paramount in constructing evidence-based planning for the policymakers and the education leaders. Improved management of supplies and data generation demands an MIS software to update school authorities and concerned departments in the government at regular intervals. The MIS software may generate monthly data regarding the menstrual supplies stock, availability of sanitation facilities across schools, count of the menstruating adolescent girls, and school preparedness towards maintaining sanitation friendly status []. The Education MIS under UNICEF’s WASH programs (Wins) in schools across 194 countries provides a classic example of robustness and usefulness of data monitoring [].
The multi-sectoral approach to MHM gaps in schools calls for convergence among various Departments such as Health and Family Welfare, Human Resource Development, Tribal Affairs, Woman and Child Development beyond the Department of Drinking Water and Sanitation. We need to leverage the use of resources and concentrated efforts to support school-based interventions for MHM. The different components to make schools menstrual hygiene friendly have been prioritized in other resources [].
The ad-hoc grant-based projects or pilot initiatives by external agencies on MHM in schools are essential for evidence generation, which can be scaled-up as cost-effectiveness solutions at the national or state level. WaterAid India and Vatsalya (Breaking the Silence program) in Uttar Pradesh were working with the schools and service providers to change the perception around MHM []. The program proactively engaged with boys, school teachers, and management committees. Another intervention called ‘the MHM curriculum’, implemented by WASH United India, adopted game-based approaches across schools to empower girls in overcoming the stigma around menstruation []. Under the broad school health-promoting framework, knowledge and perceptions around menstruation were addressed with the support of lay counsellors in the SEHER (Strengthening Evidence base on scHool-based intErventions for pRomoting adolescent health) project from Bihar. This randomized control trial advocated for the involvement of lay counsellors in transforming the school climate and improving adolescent health outcomes [].
Multiple non-peer reviewed anecdotal evaluation reports and articles documented that the implementation of such school-based MHM interventions was imperative to construct evidence. One such evidence was from a large-scale study covering 15 districts in India, called project JAGRITI, with menstrual hygiene promotion among adolescent girls as one of the components []. The program, run by the MAMTA-health Institute for Mother and Child, made a 10-step pragmatic guideline towards transforming schools into menstrual hygiene friendly with essential and desirable components (adapted from the National guidelines). Other national and state-level menstrual health players active in India are contributing to the availability of low-cost disposable sanitary material, MHM education to girls through comic books, training of facilitators, and researching on MHM behavior and practices [].
Poor menstrual hygiene practices can lead to potential long-term consequences such as dropping out of school, early marriage, restriction of mobility, agency development (capacity to act independently), menstrual irregularities, and other reproductive and mental health problems. Moreover, menstrual irregularities during reproductive age group are common in many gynecological diseases, such as endometriosis, which may affect mental and psychological well-being in long-term []. There are multiple challenges girls face in managing menstruation due to poor awareness about safe practices, limited access to sanitary products, sanitation, and lack of support from teachers or family members. Schools have emerged as an important delivery platform for health promotion interventions, which needs more consistent efforts to improve the health outcomes of young girls.
Limitations of the Study
The results of the review should be interpreted in view of some limitations. This review aimed to provide an overview of menstrual hygiene practices in schools. We could not produce a critically appraised and synthesized results for all the components of menstrual hygiene friendly schools. Heterogeneity between the included studies was very high, which might affect the validity of the pooled results. Most of the included studies were of low quality. The reports and peer-reviewed journal articles, which were publicly available, were included in our study. This limits our access to published literature in the public domain only. The study results might be considered in lieu of publication bias for positive findings because negative findings might not have been placed in the included reports and papers or papers and reports with negative findings may not have been published or made publicly available.
5. Conclusions
MHM practices in schools are poor in India. Furthermore, we lack sufficient data to conclude the MHM situation in schools. The government has developed national level guidelines on all the aspects of MHM friendly school. However, its effective implementation on the ground is lacking. Still, MHM in schools is largely supported by outside agencies. Research on MHM in schools is mainly focused on observational studies to assess the knowledge and practices of girls regarding MHM. Moreover, research on the other aspects, such as waste management, teacher’s knowledge assessment, and management information, is limited.
There is a wide scope of integrating various curriculum or non-curriculum-based actions on menstrual health education and establish schools as an ideal forum to disseminate MHM information. There is a need for transforming the existing infrastructure into menstrual hygiene friendly, which needs to be the priority area for all the schools (government or private). Simplifying the elaborated guidelines into pragmatic action points would help authorities and management committees to implement the program easily in all the schools. The increased momentum from international donors, small and medium-sized enterprises, and non-governmental organizations could be synergized and channeled into constructive outcomes for attaining improved menstrual health outcomes. The emerging scientific and innovative solutions from MHM projects could help policymakers in strategizing concentrated efforts in this direction. Moreover, expanding MHM accountability from sanitation and health ministries to other departments will help to improve menstrual hygiene conditions in the country multilaterally. To better understand the problems surrounding MHM for adolescent girls in school, the impact of MHM interventions, we need new research studies with expanded range of methodologies.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/17/2/647/s1, Table S1: Description of the qualitative assessment of the studies included in the review, Table S2: PRISMA checklist.
Author Contributions
S.S. conceived and designed the study. S.S. and D.M. performed the literature search, and extraction and analysis of the data. N.B. supported in designing the search strategy. S.S. wrote the first draft of the paper, which was critically revised by N.B., D.M., and S.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sommer, M.; Sahin, M. Overcoming the taboo: Advancing the global agenda for menstrual hygiene management for schoolgirls. Am. J. Public Health 2013, 103, 1556–1559. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. Demographics. Available online: https://data.unicef.org/topic/adolescents/demographics/ (accessed on 20 September 2018).
- Government of India. Census 2011. Available online: http://censusindia.gov.in/Census_And_You/age_structure_and_marital_status.aspx (accessed on 5 August 2018).
- Geertz, A.; Iyer, L.; Kasen, P.; Mazzola, F.; Peterson, K. Menstrual health in India: Country’s Landscape Analysis. Available online: http://menstrualhygieneday.org/wp-content/uploads/2016/04/FSG-Menstrual-Health-Landscape_India.pdf (accessed on 6 June 2018).
- Keatman, T.; Cavill, S.; Mahon, T. Menstrual Hygiene Management in Schools in South Asia, Synthesis Report; Water Aid: New Delhi, India, 2018. [Google Scholar]
- National Rural Health Mission. Training Module for ASHA on Menstrual Hygiene; National Rural Health Mission: New Delhi, India, 2011.
- Ministry of Drinking Water and Sanitation. Menstrual Hygiene Management, National Guidelines; Ministry of Drinking Water and Sanitation: New Delhi, India, 2015.
- Priyadarshani, S. Bollywood Takes on Menstrual Hygiene. Available online: https://www.nature.com/articles/d41586-018-02515-y (accessed on 10 August 2018).
- Government of India. Operational Guidelines for Menstrual Hygiene Promotion among Adolescent Girls (10–19 Years) in Rural Areas; Government of India: New Delhi, India, 2011.
- Mahon, T.; Fernandes, M. Menstrual hygiene in South Asia: A neglected issue for WASH (water, sanitation and hygiene) programmes. Gend. Dev. 2010, 18, 99–113. [Google Scholar] [CrossRef]
- Sommer, M.; Sutherland, C.; Chandra-Mouli, V. Putting menarche and girls into the global population health agenda. Reprod. Health 2015, 12, 24. [Google Scholar] [CrossRef] [PubMed]
- Kirk, J.; Sommer, M. Menstruation and body awareness: Linking girls’ health with girls’ education. In Special on Gender and Health; Royal Tropical Institute (KIT): Amsterdam, The Netherlands, 2006; pp. 1–22. [Google Scholar]
- National Council of Education Research Training. 8th All India School Education Surveys: A Concised Report, 1st ed.; NCEET Publications: New Delhi, India, 2016.
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Van Eijk, A.M.; Sivakami, M.; Thakkar, M.B.; Bauman, A.; Laserson, K.F.; Coates, S.; Phillips-Howard, P.A. Menstrual hygiene management among adolescent girls in India: A systematic review and meta-analysis. BMJ Open 2016, 6, e010290. [Google Scholar] [CrossRef]
- Gupta, J.; Gupta, H. Adolescents and Menstruation. J. Fam. Welf. 2001, 47, 1–13. [Google Scholar]
- Gupta, S.; Sinha, A. Awareness about reproduction and adolescent changes among school girls of different socioeconomic status. J. Obstet. Gynecol. India 2006, 56, 324–328. [Google Scholar]
- Tiwari, H.; Oza, U.N.; Tiwari, R. Knowledge, attitudes and beliefs about menarche of adolescent girls in Anand district, Gujarat. East. Mediterr. Health J. 2006, 12, 428–433. [Google Scholar]
- Kotecha, P.V.; Patel, S.; Baxi, R.K.; Mazumdar, V.S.; Misra, S.; Modi, E.; Diwanji, M. Reproductive health awareness among rural school going adolescents of Vadodara district. Indian J. Sex. Transm. Dis. AIDS 2009, 30, 94. [Google Scholar]
- Mittal, K.; Goel, M.K. Knowledge regarding reproductive health among urban adolescent girls of Haryana. Indian J. Community Med. 2010, 35, 529–530. [Google Scholar]
- Mudey, A.; Kesharwani, N.; Mudey, G.A.; Goyal, R.C. A cross-sectional study on awareness regarding safe and hygienic practices amongst school going adolescent girls in rural area of Wardha District, India. Glob. J. Health Sci. 2010, 2, 225–231. [Google Scholar] [CrossRef]
- Verma, P.B.; Pandya, C.M.; Ramanuj, V.A.; Singh, M.P. Menstrual pattern of adolescent school girls of Bhavnagar (Gujarat). Natl. J. Integr. Res. Med. 2011, 2, 38–40. [Google Scholar]
- Thakre, S.B.; Thakre, S.S.; Reddy, M.; Rathi, N.; Pathak, K.; Ughade, S. Menstrual hygiene: Knowledge and practice among adolescent school girls of Saoner, Nagpur District. J. Clin. Diagn. Res. 2011, 5, 1027–1033. [Google Scholar]
- Venkatesh, R.; Dhoundiyal, M. Perceptions and practices during menstruation among adolescent girls in and around Bangalore city. Indian J. Matern. Child Health 2011, 13, 1–7. [Google Scholar]
- Kamaljit, K.; Balwinder, A.; Singh, G.K.; Neki, N.S. Social beliefs and practices associated with menstrual hygiene among adolescent girls of Amritsar, Punjab, India. J. Int. Med. Sci. Acad. 2012, 25, 69–70. [Google Scholar]
- Sudeshna, R.; Aparajita, D. Determinants of menstrual hygiene among adolescent girls: A multivariate analysis. Natl. J. Community Med. 2012, 3, 294–301. [Google Scholar]
- Khan, A. Perceptions and practices about menstrual hygiene among adolescent girls in a rural area-a cross-sectional study. Int. J. Health Sci. Res. 2012, 2, 29–34. [Google Scholar]
- Solanki, H.; Gosalia, V.; Patel, H.; Vora, F.; Singh, M.P. A study of menstrual problems and practices among girls of Mahila College. Natl. J. Integr. Res. Med. 2012, 3, 24–27. [Google Scholar]
- Dambhare, D.G.; Wagh, S.V.; Dudhe, J.Y. Age at menarche and menstrual cycle pattern among school adolescent girls in Central India. Glob. J. Health Sci. 2012, 4, 105. [Google Scholar] [CrossRef]
- Ade, A.; Patil, R. Menstrual hygiene and practices of rural adolescent girls of Raichur. Int. J. Biol. Med. Res. 2013, 42, 3014–3017. [Google Scholar]
- Bhattacherjee, S.; Ray, K.; Biswas, R.; Chakraborty, M. Menstruation: Experiences of adolescent slum dwelling girls of Siliguri City, West Bengal, India. J. Basic Clin. Reprod. Sci. 2013, 2, 85–91. [Google Scholar] [CrossRef]
- Kanotra, S.K.; Bangal, V.B.; Bhavthankar, D.P. Menstrual pattern and problems among rural adolescent girls. Int. J. Biomed. Adv. Res. 2013, 4, 551–554. [Google Scholar] [CrossRef]
- Kamanth, R.; Ghosh, D.; Lena, A.; Chandrasekaran, V. A study on knowledge and practices regarding menstrual hygiene among rural and urban adolescent girls in Udipi Taluk, Manipal, India. Glob. J. Med. Public Health 2013, 2, 1–9. [Google Scholar]
- Amirtha, G.; Premarajan, K.C.; Sarkar, S.; Lakshminarayanan, S. Menstrual health-Knowledge, practices and needs of adolescent school girls in Pondicherry. Indian J. Matern. Child Health 2013, 15, 2–5. [Google Scholar]
- Katiyar, K.; Chopra, H.; Garg, S.K.; Bajpai, S.K.; Bano, T.; Jain, S.; Kumar, A. KAP study of menstrual problems in adolescent females in an urban area of Meerut. Indian J. Community Health 2013, 25, 217–220. [Google Scholar]
- Nagamani, N.G.; Krishnaveni, A.; Naidu, S.; Sreegiri, S. A study on menstrual practices among adolescent girls residing in urban slums of Visakhapatnam city of Andhra Pradesh State. Int. J. Res. Med. 2014, 3, 62–64. [Google Scholar]
- Raina, D.; Balodi, G. Menstrual hygiene: Knowledge, practise and restrictions amongst girls of Dehradun, Uttarakhand, India. Glob. J. Interdiscip. Soc. Sci. 2014, 3, 156–162. [Google Scholar]
- Jain, A.; Aswar, N.R.; Domple, V.K.; Doibale Mohan, K.; Barure Balaji, S. Menstrual hygiene awareness among rural unmarried girls. J. Evol. Med. Dent Sci. 2014, 3, 1413–1419. [Google Scholar]
- Madhusudan, M.; Chaluvaraj, T.S.; Chaitra, M.M.; Ankitha, S.; Pavithra, M.S.; Mahadeva Urthy, T.S. Menstrual hygiene: Knowledge and practice among secondary school girls of Hosakote, rural Bangalore. Int. J. Basic Appl. Med. Sci. 2014, 4, 313–320. [Google Scholar]
- Prajapati, D.J.; Shah, J.P.; Khedia, G. Menstrual hygiene: Knowledge and practice among adolescent girls of rural Kheda. Natl. J. Community Med. 2015, 6, 349–353. [Google Scholar]
- Zaidi, S.H.N.; Sivakami, A.; Ramasamy, J. Menstrual hygiene and sanitation practices among adolescent school going girls: A study from a South Indian town. Int. J. Community Med. Public Health 2015, 2, 189–194. [Google Scholar] [CrossRef]
- Langer, B.; Mahajan, R.; Gupta, R.K.; Kumari, R.; Jan, R.; Mahajan, R. Impact of menstrual awareness and knowledge among adolescents in a rural area. Indian J. Community Health 2015, 27, 456–461. [Google Scholar]
- Preeti, G.; Amaresh, B.; Singh, H.; Lakshmi, A.; Srinivas, K.; Singh, G. A cross sectional study of knowledge, attitude and practices regarding menstrual pattern in adolescent girl. J. Evid. Based Med. Healthc. 2015, 2, 3933–3939. [Google Scholar]
- Varghese, M.; Ravichandran, M.; Karunai Anandhan, A. Knowledge and practice of menstrual hygiene among adolescent girls. Ind. J. Youth Adol. Health 2015, 2, 35–43. [Google Scholar]
- Walia, D.K.; Yadav, R.J.; Pandey, A.; Bakshi, R.K. Menstrual patterns among school going adolescent girls in Chandigarh and rural areas of Himachal Pradesh, North India. Natl. J. Community Med. 2015, 6, 583–586. [Google Scholar]
- Tarhane, S.; Kasulkar, A. Awareness of adolescent girls regarding menstruation and practices during menstrual cycle. Panacea J. Med. Sci. 2015, 5, 29–32. [Google Scholar]
- Chadalawada, U.R.; Kala, S. Assessment of menstrual hygiene practices among adolescent girls. Stanley Med. J. 2016, 3, 13–16. [Google Scholar]
- Kansal, S.; Singh, S.; Kumar, A. Menstrual hygiene practices in context of schooling: A community study among rural adolescent girls in Varanasi. Indian J. Community Med. 2016, 41, 39–44. [Google Scholar]
- Seenivasan, P.; Priya, K.C.; Rajeswari, C.; Akshaya, C.C.; Sabharritha, G.; Sowmya, K.R.; Banu, S. Knowledge, attitude and practices related to menstruation among adolescent girls in Chennai. J. Clin. Sci. Res. 2016, 5, 164–170. [Google Scholar] [CrossRef]
- Kshirsagar, M.V.; Mhaske, M.; Ashturkar, M.D.; Fernandez, K. Study of menstrual hygienic practices among the adolescent girls in rural area. Natl. J. Community Med. 2016, 7, 241–244. [Google Scholar]
- Dudeja, P.; Sindhu, A.; Shankar, P.; Gadekar, T. A cross-sectional study to assess awareness about menstruation in adolescent girls of an urban slum in western Maharashtra. Int. J. Adolesc. Med. Health 2016, 30, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Anju, C.M.; Jesha, M.M.; Sebastian, N.M.; Haveri, S.P. Menstrual hygiene practices in a rural area of north Kerala. Int. J. Prev. Curative Community Med. 2016, 21, 64–70. [Google Scholar]
- Devi, R.U.; Sivagurunathan, C.; Kumar, P.M. Awareness about menstrual hygiene among adolescent girls in rural area of Kancheepuram District-Tamil Nadu. Int. J. Pharm. Biol. Sci. 2016, 7, 267–269. [Google Scholar]
- Taklikar, C.; Dobe, M.; Mandal, R.M. Menstrual Hygiene Knowledge and Practice among Adolescent School Girls of Urban Slum of Chetla, Kolkata. Indian J. Hyg. Public Health 2016, 2, 57–67. [Google Scholar]
- Nagaraj, C.; Konapur, K.S. Effect of health education on awareness and practices related to menstruation among rural adolescent school girls in Bengaluru, Karnataka. Int. J. Prevent. Public Health Sci. 2016, 2, 18–21. [Google Scholar]
- Chauhan, A.; Chauhan, S.K.; Bala, D.V. Menstruation and menstrual hygiene among adolescent girls of Ahmadabad city: A descriptive analysis. Int. Multispecialty J. Health 2016, 2, 7–12. [Google Scholar]
- Sarvade, A.; Nile, R.G. Menstrual hygiene: Awareness and practices amongst adolescent girls attended school health camp in Mumbai, Maharashtra, India. Int. J. Community Med. Public Health 2016, 3, 3022–3025. [Google Scholar] [CrossRef]
- Rokade, H.G.; Kumavat, A.P. Study of menstrual pattern and menstrual hygiene practices among adolescent girls. Natl. J. Community Med. 2016, 7, 398–403. [Google Scholar]
- Jitpure, S. Assessment of menstrual hygiene, menstrual practices and menstrual problems among adolescent girls living in urban slums of Bilaspur (Chhattisgarh). IOSR J. Dent. Med. Sci. 2016, 15, 16–20. [Google Scholar]
- Darivemula, S.; Nagoor, K.; Reddy, B.; Kahn, S.; Sekhar, C.; Basha, J. A community based study on knowledge and practices of menstrual hygiene among the adolescent girls in rural south India. J. Int. J. Curr. Adv. Res. 2017, 6, 4749–4752. [Google Scholar]
- Sarkar, I.; Dobe, M.; Dasgupta, A.; Basu, R.; Shahbabu, B. Determinants of menstrual hygiene among school going adolescent girls in a rural area of West Bengal. J. Fam. Med. Prim. Care 2017, 6, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Tuli, A.G.; Dhar, T.; Garg, J.; Garg, N. Menstrual hygiene-knowledge and practice among adolescent school girls in rural areas of Punjab. J. Evol. Med. Dent. Sci. 2017, 6, 5793–5796. [Google Scholar] [CrossRef]
- Hakim, A.; Rizwana, S.; Manisha; Tak, H. A cross sectional study on the knowledge, attitudes and practices towards menstrual cycle and its problems: A comparative study of government and non-government adolescent school girls. Int. J. Community Med. Public Health 2017, 4, 973–981. [Google Scholar] [CrossRef][Green Version]
- Agarwal, V.; Fancy, M.J.; Shah, H.; Agarwal, A.S.; Shah, J.H.; Singh, S. Menstrual hygiene: Knowledge and practice among adolescent girls of rural Sabarkantha district. Natl. J. Community Med. 2017, 8, 597–601. [Google Scholar]
- Neelkanth, N.; Singh, D.; Bhatia, P. A study to assess the knowledge regarding practices of menstrual hygiene and RTI among high and higher secondary school girls: An educational interventional study. Int. J. Community Med. Public Health 2017, 4, 4520–4526. [Google Scholar] [CrossRef][Green Version]
- Naithani, R. A study on knowledge and practices regarding menstrual hygiene among adolescent girls in Pauri, Uttarakhand. J. Mt. Res. 2017, 12, 25–29. [Google Scholar]
- Kapoor, G.; Kumar, D. Menstrual hygiene: Knowledge and practice among adolescent school girls in rural settings. Int. J. Reprod. Contracept. Obstet. Gynecol. 2017, 6, 959–962. [Google Scholar] [CrossRef]
- Gandotra, N.; Pal, R.; Maheshwari, S. Assessment of knowledge and practices of menstrual hygiene among urban adolescent girls in North India. Int. J. Reprod. Contracept. Obstet. Gynecol. 2018, 7, 2825–2828. [Google Scholar] [CrossRef][Green Version]
- Gupta, N.; Kariwala, P.; Dixit, A.M.; Govil, P.; Jain, P.K. A cross-sectional study on menstrual hygiene practices among school going adolescent girls (10–19 years) of Government Girls Inter College, Saifai, Etawah. Int. J. Community Med. Public Health 2018, 5, 4560–4565. [Google Scholar] [CrossRef]
- Agarwal, N.; Soni, N.; Singh, S.P.; Soni, G.P. Knowledge and Practice Regarding Menstrual Hygiene Among Adolescent Girls of Rural Field Practice Area of RIMS, Raipur (CG), India. Int. J. Reprod. Contracept. Obstet. Gynecol. 2018, 7, 2317–2321. [Google Scholar] [CrossRef][Green Version]
- Tarannum, F.; Khalique, N.; Eram, U. A community based study on age of menarche among adolescent girls in Aligarh. Int. J. Community Med. Public Health 2018, 5, 395–400. [Google Scholar] [CrossRef]
- Vashisht, A.; Pathak, R.; Agarwalla, R.; Patavegar, B.N.; Panda, M. School absenteeism during menstruation amongst adolescent girls in Delhi, India. J. Fam. Community Med. 2018, 25, 163. [Google Scholar]
- Kakeri, M.; Patil, S.B.; Waghmare, R. Knowledge and practice gap for menstrual hygiene among adolescent school girls of tribal district of Maharashtra, India: A cross sectional study. Indian J. Youth Adol. Health 2018, 5, 23–27. [Google Scholar]
- Dharni, I.T. A comparative study to assess the menstrual hygiene practices among adolescent girls of urban and rural schools of Ludhiana, Punjab. Int. J. Adv. Res. 2018, 6, 586–600. [Google Scholar] [CrossRef]
- Senapathi, P.; Kumar, H. A comparative study of menstrual hygiene management among rural and urban adolescent girls in Mangaluru, Karnataka. Int. J. Community Med. Public Health 2018, 5, 2548–2556. [Google Scholar] [CrossRef]
- Aswathy, M.G.; Saju, C.R.; Mundodan, J.M. Awareness and practices regarding menarche in adolescent school going girls of Thrissur educational district. Int. J. Community Med. Public Health 2019, 6, 755–758. [Google Scholar] [CrossRef]
- Rastogi, S.; Khanna, A.; Mathur, P. Uncovering the challenges to menstrual health: Knowledge, attitudes and practices of adolescent girls in government schools of Delhi. Health Educ. J. 2019, 78, 839–850. [Google Scholar] [CrossRef]
- Sivakami, M.; Ejik, A.M.V.; Thakur, H.; Kakade, N.; Patil, C.; Shinde, S.; Surani, N.; Bauman, A.; Zulaika, G.; Kabir, Y.; et al. Effect of menstruation on girls and their schooling, and facilitators of menstrual hygiene management in schools: Surveys in government schools in three states in India, 2015. J. Glob. Health 2019, 9, e010408. [Google Scholar] [CrossRef]
- Patel, S.; Vernekar, S.P.; Desai, A.M. A study on the knowledge, attitude and practices regarding menstrual hygiene among adolescent girls in schools in a rural area of Goa. J. Clin. Diagn. Res. 2019, 13, 7–10. [Google Scholar] [CrossRef]
- Khatuja, R.; Mehta, S.; Dinani, B.; Chawla, D.; Mehta, S. Menstrual health management: Knowledge and practices among adolescent girls. Trop. J. Obstet. Gynaecol. 2019, 36, 283–286. [Google Scholar]
- Pradhan, S.; Kar, K.; Samal, B.P.; Pradhan, J. Assessment of knowledge and practice of menstrual hygiene among school going adolescent girls in an urban area of Odisha: A cross sectional study. Int. J. Community Med. Public Health 2019, 6, 3979–3983. [Google Scholar] [CrossRef]
- Phani Madhavi, K.V.; Paruvu, K. Menstrual hygiene and practices among adolescent girls in rural Visakhapatnam: A cross-sectional study. Int. J. Community Med. Public Health 2019, 6, 432–436. [Google Scholar] [CrossRef]
- Chajhlana, S.P.S.; Amaravadhi, S.R.; Mazodi, S.D.; Kolusu, V.S. Determinants of menstrual hygiene among school going adolescent girls in urban areas of Hyderabad. Int. J. Community Med. Public Health 2019, 6, 2211–2215. [Google Scholar] [CrossRef]
- Sonowal, P.; Talukdar, K. Menstrual hygiene knowledge and practices amongst adolescent girls in urban slums of Dibrugarh town- a cross sectional study. Galore Int. J. Health Sci. Res. 2019, 4, 44–51. [Google Scholar]
- Kamboj, N.; Chandiok, K. Knowledge and practices regarding menstrual hygiene among school going adolescent girls. J. Curr. Sci. 2019, 20, 1–8. [Google Scholar]
- Kaur, S. Knowledge and attitude on menstrual hygiene among adolescent girls in Kapurthala district of Punjab. Int. J. Sci. Res. Rev. 2019, 7, 3374–3379. [Google Scholar]
- Solvig, N.; Raja, L.; George, C.E.; O’Connell, B.; Gangadharan, P.; Norman, G. Analysis of knowledge of menstruation, hygiene practices, and perceptions in adolescent girls in India. Mod. Health Sci. 2019, 2, 16–21. [Google Scholar] [CrossRef]
- Manuja, L.M.; Raghavendra, S.K.; Shashikiran, M. Menstrual hygiene among adolescent girls in the rural field practice area of medical college in Mandya. Natl. J. Res. Community Med. 2019, 8, 236–239. [Google Scholar]
- Kalyani, S.; Bicholkar, A.; Cacodcar, J.A. A study of knowledge, attitude and practices regarding menstrual health among adolescent girls in North Goa. Epidem. Int. 2019, 4, 1–5. [Google Scholar]
- Deo, D.S.; Ghattargi, C.H. Perceptions and practices regarding menstruation: A comparative study in urban and rural adolescent girls. Indian J. Community Med. 2005, 30, 33–34. [Google Scholar]
- Salve, S.B.; Dase, R.K.; Mahajan, S.M.; Adchitre, S.A. Assessment of knowledge and practices about menstrual hygiene amongst rural and urban adolescent girls–A comparative study. Int. J. Recent Trends Sci. Technol. 2012, 3, 65–70. [Google Scholar]
- Paria, B.; Bhattacharyya, P.K.; Das, S. A comparative study on menstrual hygiene among urban and rural adolescent girls of West Bengal. J. Fam. Med. Prim. Care 2014, 3, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Patle, R.; Kubde, S. Comparative study on menstrual hygiene in rural and urban adolescent girls. Indian J. Med. Sci. Public Health 2014, 3, 129–132. [Google Scholar] [CrossRef]
- Pandit, D.; Bhattacharyya, P.; Bhattacharya, R. Menstrual hygiene: Knowledge and practice among adolescent school girls in rural areas of West Bengal. IOSR J. Dent. Med. Sci. 2014, 13, 19–24. [Google Scholar] [CrossRef]
- Thakur, H.; Aronsson, A.; Bansode, S.; Stalsby Lundborg, C.; Dalvie, S.; Faxelid, E. Knowledge, practices, and restrictions related to menstruation among young women from low socioeconomic community in Mumbai, India. Front. Public Health 2014, 2, 72. [Google Scholar] [CrossRef]
- Patavegar, B.N.; Kapilashrami, M.C.; Rasheed, N.; Pathak, R. Menstrual hygiene among adolescent school girls: An in-depth cross-sectional study in an urban community. Int. J. Health Sci. Res. 2014, 4, 15–21. [Google Scholar]
- Jailkhani, S.M.K.; Naik, J.D.; Thakur, M.S.; Langre, S.D.; Pandey, V.O. Patterns & problems of menstruation amongst the adolescent girls residing in the urban slum. Sch. J. Appl. Med. Sci. 2014, 2, 529–534. [Google Scholar]
- Sowmya, B.C.; Manjunatha, S.; Kumar, J. Menstrual hygiene practices among adolescent girls: A cross sectional study. J. Evol. Med. Dent. Sci. 2014, 3, 7955–7961. [Google Scholar] [CrossRef]
- Bachloo, T.; Kumar, R.; Goyal, A.; Singh, P.; Yadav, S.S.; Bhardwaj, A.; Mittal, A. A study on perception and practice of menstruation among school going adolescent girls in district Ambala Haryana, India. Int. J. Community Med. Public Health 2016, 3, 931–937. [Google Scholar] [CrossRef]
- Bedi, R.; Choudhary, P.K.; Sharma, S.K.; Meharda, B.; Singh, D.; Sharma, R.K. Impact of health education on knowledge and practices about menstrual hygeine among rural adolescent school going girls at RHTC Srinagar, Ajmer, Rajasthan, India. IOSR J. Dent. Med. Sci. 2017, 16, 1–7. [Google Scholar]
- Nath, K.R.; John, J. Menstrual Hygiene Practices among adolescent girls in a rural area of Kanyakumari District of Tamilnadu. Indian J. Youth Adolesc. Health 2019, 6, 8–14. [Google Scholar]
- Garg, R.; Goyal, S.; Gupta, S. India moves towards menstrual hygiene: Subsidized sanitary napkins for rural adolescent girls—issues and challenges. Matern. Child Health J. 2012, 16, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Ravi, R.; Shah, P.B.; Edward, S.; Gopal, P.; Sathiyasekaran, B.W.C. Social impact of menstrual problems among adolescent school girls in rural Tamil Nadu. Int. J. Adolesc. Med. Health 2018, 30, 1–8. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Promoting Health through Schools. In Report of a WHO Expert Committee on Comprehensive School Health Education and Promotion; World Health Organization Technical Report Series; WHO: Geneva, Switzerland, 1997; pp. 10–12. [Google Scholar]
- Shinde, S.; Pereira, B.; Khandeparkar, P.; Sharma, A.; Patton, G.; Ross, D.A.; Weiss, H.A.; Patel, V. The development and pilot testing of a multicomponent health promotion intervention (SEHER) for secondary schools in Bihar, India. Glob. Health Action 2017, 10, e1385284. [Google Scholar] [CrossRef] [PubMed]
- Thakur, J.S.; Sharma, D.; Jaswal, N.; Bharti, B.; Grover, A.; Thind, P. Developing and implementing an accreditation system for health promoting schools in Northern India: A cross-sectional study. BMC Public Health 2014, 14, 1314. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Thapa, S. How Functional are School Management Committees in the Present Context? CCS Working Paper No. 271. Available online: https://ccs.in/internship_papers/2012/271_how-functional-are-school-management-commitees-in-the-present-context_sijan-thapa.pdf (accessed on 13 February 2019).
- Kumar, S. Roles and functions of school management committees (SMC) of government middle schools in district Kullu of Himachal Pradesh: A case study. Sch. Res. J. Humanit. Sci. Engl. Lang. 2016, 3, 3876–3886. [Google Scholar]
- Kaur, R.; Kaur, K.; Kaur, R. Menstrual Hygiene, Management, and Waste Disposal: Practices and Challenges Faced by Girls/Women of Developing Countries. J. Environ. Public Health. 2018. [Google Scholar] [CrossRef]
- United Nations Children’s Fund (UNICEF); World Health Organization. Drinking Water, Sanitation and Hygiene in Schools: Global Baseline Report 2018; United Nations Children’s Fund (UNICEF); World Health Organization: New York, NY, USA, 2018. [Google Scholar]
- Ganguly, L.; Satpati, L. Sanitation and hygiene status among school students: A micro study on some selective schools of North Dumdum municipality area, West Bengal. Int. Res. J. Public Environ. Health 2019, 6, 127–131. [Google Scholar]
- Bodat, S.; Ghate, M.M.; Majumdar, J.R. School absenteeism during menstruation among rural adolescent girls in Pune. Natl. J. Community Med. 2013, 4, 212–216. [Google Scholar]
- Periyasamy, S.; Krishnappa, P.; Renuka, P. Adherence to components of health promoting schools in schools of Bengaluru, India. Health Promot. Int. 2019, 34, 1167–1178. [Google Scholar] [CrossRef]
- Srivastava, S. Status of Hygiene and Sanitation Conditions in Schools, Uttar Pradesh FANSA U.P; Chapter and Shohratgarh Environmental Society. Available online: http://sesindia.org/pdf/Sanitation%20Status%20in%20Schools%20of%20U.P.pdf (accessed on 10 January 2019).
- Annual Status of Education Report Centre. Annual Status of Education Report (Rural). 2018. Available online: http://img.asercentre.org/docs/ASER%202018/Release%20Material/aserreport2018.pdf (accessed on 5 August 2019).
- Mehta, A.C. Elementary Education in Unrecognised Schools in India; National Institute of Educational Planning and Administration. 2005. Available online: http://dise.in/Downloads/Publications/Publications%202005-06/Ar0506/Introduction.pdf (accessed on 10 October 2019).
- Tooley, J.; Dixon, P. Private schooling for low-income families: A census and comparative survey in East Delhi, India. Int. J. Educ. Dev. 2007, 27, 205–219. [Google Scholar] [CrossRef]
- Zaidi, S.M.I.A. Facilities in Primary and Upper Primary Schools in India: An Analysis of DISE Data of Selected Major States. National Institute of Educational Planning and Administration. 2004. Available online: http://www.dise.in/downloads/use%20of%20dise%20data/zaidi.pdf (accessed on 13 October 2019).
- Majra, J.P.; Gur, A. School environment and sanitation in rural India. J. Glob. Infect. Dis. 2010, 2, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Joseph, N.; Bhaskaran, U.; Saya, G.K.; Kotian, S.M.; Menezes, R.G. Environmental sanitation and health facilities in schools of an urban city of south India. Ann. Trop. Med. Public Health 2012, 5, 431–435. [Google Scholar] [CrossRef]
- UNICEF. An Overview of the Status of Drinking Water and Sanitation in Schools in India. Available online: http://www.dise.in/Downloads/best%20practices/An%20overview%20of%20status%20of%20drinking%20water%20and%20sanitation%20in%20schools%20in%20India.pdf (accessed on 16 October 2019).
- Rakesh, P.S.; Usha, S.; Subhagan, S.; Shaji, M.; Sheeja, A.L.; Subairf, F. Water quality and sanitation at schools: A cross sectional study from Kollam District, Kerala, Southern India. Kerala Med. J. 2014, 7, 62–65. [Google Scholar]
- Devi, U.L.; Kiran, J.K.; Prashanti, B. Girl Child Friendly (NPEGEL) schools and its impact on enrollment and dropout of girl child. Int. J. Sci. Res. 2014, 3, 559–562. [Google Scholar]
- Kaur, J.; Saini, S.K.; Bharti, B.; Kapoor, S. Health Promotion facilities in Schools: WHO Health Promoting Schools Initiative. Nurs. Midwifery Res. J. 2015, 11, 103–111. [Google Scholar]
- Santhya, K.G.; Francis Zavier, A.J.; Jejeebhoy, S.J. School quality and its association with agency and academic achievements in girls and boys in secondary schools: Evidence from Bihar, India. Int. J. Educ. Dev. 2015, 41, 35–46. [Google Scholar] [CrossRef]
- Lahon, S. A study of infrastructure facilities in secondary schools of Assam state with special reference to Sivasagar District. J. Res. 2015, 4, 1–10. [Google Scholar]
- Babu, J.P. Facilities provided by the primary education schools—A study in east Godavari district of Andhra Pradesh. Int. J. Acad. Res. Dev. 2018, 3, 1605–1607. [Google Scholar]
- Padhi, S.; Priyabadini, S.; Pradhan, S.K. An assessment of institutional health for adolescent girls. Indian J. Sci. Technol. 2018, 11, 1–5. [Google Scholar] [CrossRef]
- Kumar, A. An evaluation study of infrastructure facilities in government primary schools in Dehradun district (Uttarakhand). Samwaad eJ. 2018, 7, 75–91. [Google Scholar]
- Mahon, T.; Tripathy, A.; Singh, N. Putting the men into menstruation: The role of men and boys in community menstrual hygiene management. Waterlines 2015, 34, 7–14. [Google Scholar] [CrossRef]
- Kirk, J. The SoE/SBEP Gender Equity Support Program: An Early Impact Assessment. Unpublished Program Document of Sudan Basic Education Program, Nairobi, Kenya. 2005. Available online: https://www.eccnetwork.net/sites/default/files/media/file/doc_1_89_mentors_for_girls.pdf (accessed on 10 September 2018).
- Mason, L.; Sivakami, M.; Thakur, H.; Kakade, N.; Beauman, A.; Alexander, K.; Eijke, A.M.V.; Laserson, K.F.; Thakkar, M.B.; Phillips-Howard, P.A. ‘We do not know’: A qualitative study exploring boys’ perceptions of menstruation in India. Reprod. Health 2017, 14, 174. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, P.; Sharma, N. Perceived parental relationship and the awareness level of adolescents regarding menarche. J. Hum. Ecol. 2004, 16, 215–218. [Google Scholar] [CrossRef]
- Khanna, A.; Goyal, R.S.; Bhawsar, R. Menstrual practices and reproductive problems: A study of adolescent girls in Rajasthan. J. Health Manag. 2005, 7, 1. [Google Scholar] [CrossRef]
- Nair, P.; Grover, V.L.; Kannan, A.T. Awareness and practices of menstruation and pubertal changes amongst unmarried female adolescents in a rural area of East Delhi. Indian J. Community Med. 2007, 32, 156–157. [Google Scholar] [CrossRef]
- Udgiri, R.; Angadi, M.M.; Patil, S.; Sorganvi, V. Knowledge and practices regarding menstruation among adolescent girls in an urban slum, Bijapur. J. Indian Med. Assoc. 2010, 108, 514–516. [Google Scholar]
- Omidvar, S.; Begum, K. Factors influencing hygienic practices during menses among girls from south India: A cross sectional study. Int J. Collab. Res. Intern. Med. Public Health 2010, 2, 411–423. [Google Scholar]
- Dorle, A.S.; Hiremath, L.D.; Mannapur, B.S.; Ghattargi, C.H. Awareness regarding puberty changes in secondary school children of Bagalkot, Karnataka—A cross sectional study. J. Clin. Diagn. Res. 2010, 4, 3016–3019. [Google Scholar]
- Dube, S.; Sharma, K. Knowledge, attitude and practice regarding reproductive health among urban and rural girls: A comparative study. Stud. Ethno-Med. 2012, 6, 85–94. [Google Scholar] [CrossRef]
- Shanbhag, D.; Shilpa, R.; D’Souza, N.; Josephine, P.; Singh, J.; Goud, B.R. Perceptions regarding menstruation and practices during menstrual cycles among high school going adolescent girls in resource limited settings around Bangalore city, Karnataka, India. Int. J. Collab. Res. Intern. Med. Public Health 2012, 4, 1353. [Google Scholar]
- Datta, A.; Manna, N.; Datta, M.; Sarkar, J.; Baur, B.; Datta, S. Menstruation and menstrual hygiene among adolescent girls of West Bengal, India: A school based comparative study. Glob. J. Med. Public Health 2012, 1, 50–57. [Google Scholar]
- Verma, P.; Ahmad, S.; Srivastava, R.K. Knowledge and practices about menstrual hygiene among higher secondary school girls. Indian J. Community Health 2013, 25, 265–271. [Google Scholar]
- Yasmin, S.; Manna, N.; Mallik, S.; Ahmed, A.; Paria, B. Menstrual hygiene among adolescent school students: An in-depth cross-sectional study in an urban community of West Bengal, India. IOSR J. Dent Med. Sci. 2013, 5, 22–26. [Google Scholar] [CrossRef]
- Juyal, R.; Kandpal, S.D.; Semwal, J. Social aspects of menstruation related practices in adolescent girls of district Dehradun. Indian J. Community Health 2013, 25, 213–216. [Google Scholar]
- Kumar, D.; Goel, N.K.; Puri, S.; Pathak, R.; Sarpal, S.S.; Gupta, S.; Arora, S. Menstrual pattern among unmarried women from Northern India. J. Clin. Diagn. Res. 2013, 7, 1926–1929. [Google Scholar]
- Arora, A.; Mittal, A.; Pathania, D.; Singh, J.; Mehta, C.; Bunger, R. Impact of health education on knowledge and practices about menstruation among adolescent school girls of rural part of district Ambala, Haryana. Indian J. Community Health 2013, 25, 492–497. [Google Scholar]
- Katkuri, S.; Pisudde, P.; Kumar, N.; Hasan, S.F. A study to assess knowledge, attitude and practices about menstrual hygiene among school going adolescent girl’s in Hyderabad, India. J. Pharm. Biomed. Sci. 2014, 4, 298–302. [Google Scholar]
- Lalbiaknungi, L.; Roy, S.; Paul, A.; Dukpa, R. A study on menstrual hygiene and dysmenorrhea of adolescent girls in a rural population of West Bengal. J. Compr. Health 2015, 3, 33–41. [Google Scholar]
- Anitha, S.; Sinu, E. Menstrual Knowledge and Coping Strategies of Early Adolescent Girls: A School Based Intervention Study. J. Sch. Soc. Work 2015, 11, 10. [Google Scholar]
- Mohanty, S.; Panda, M.; Tripathi, R.M. Assessment of menstrual health among school going adolescent girls of urban slums of Berhampur, Odisha, India: A cross-sectional study. Int. J. Community Med. Public Health 2016, 3, 3440–3444. [Google Scholar] [CrossRef][Green Version]
- Kanchan, C.; Prasad, V.S.V. Menstrual hygiene: Knowledge and practice among adolescent school girls. Panacea J. Med. Sci. 2016, 6, 31–33. [Google Scholar]
- Ramachandra, K.; Gilyaru, S.; Eregowda, A.; Yathiraja, S. A study on knowledge and practices regarding menstrual hygiene among urban adolescent girls. Int. J. Contemp. Pediatr. 2016, 3, 142–145. [Google Scholar] [CrossRef]
- Malhotra, A.; Goli, S.; Cotes, S.; Mosquera-Vasquez, M. Factors associated with knowledge, attitudes, and hygiene practices during menstruation among adolescent girls in Uttar Pradesh. Waterlines 2016, 35, 277–305. [Google Scholar] [CrossRef]
- Krishnamurthy, L.; Ranganath, B.G.; Shruthi, M.N.; Venkatesha, M. Menstrual hygiene practices and knowledge among high school girls of Rural Kolar. Natl. J. Community Med. 2016, 7, 754–758. [Google Scholar]
- Singhal, V.K. Study of menstrual hygiene of school going adolescent girls in Gurgaon, Haryana. Int. J. Sci. Res. 2016, 5, 581–583. [Google Scholar]
- Kusuma, M.L.; Ahmed, M. Awareness, perception and practices of government pre-university adolescent girls regarding menstruation in Mysore city, India. Int. J. Community Med. Public Health 2016, 3, 1593–1599. [Google Scholar]
- Pal, J.; Mullick, T.H. Menstrual hygiene-an unsolved issue: A school-based study among adolescent girls in a slum area of Kolkata. IOSR J. Dent. Med. Sci. 2017, 16, 11–16. [Google Scholar] [CrossRef]
- Singh, P.; Bhardwaj, S.; Singh, S.; Singh, S.; Raghuvanshi, R.S. Study on hygiene and sanitary practices during menstruation among adolescent girls of Udham Singh Nagar district of Uttarakhand. Int. J. Home Sci. 2017, 3, 21–23. [Google Scholar]
- Mathiyalagen, P.; Peramasamy, B.; Vasudevan, K.; Basu, M.; Cherian, J.; Sundar, B. A descriptive cross-sectional study on menstrual hygiene and perceived reproductive morbidity among adolescent girls in a union territory, India. J. Fam. Med. Prim Care 2017, 6, 360–365. [Google Scholar]
- Shoor, P. A study of knowledge, attitude, and practices of menstrual health among adolescent school girls in urban field practice area of medical college, Tumkur. Indian J. Health Sci. Biomed. Res. 2017, 10, 249–255. [Google Scholar] [CrossRef]
- Hema Priya, S.; Nandi, P.; Seetharaman, N.; Ramya, M.R.; Nishanthini, N.; Lokeshmaran, A. A study of menstrual hygiene and related personal hygiene practices among adolescent girls in rural Puducherry. Int. J. Community Med. Public Health 2017, 4, 2348–2355. [Google Scholar] [CrossRef]
- Deshpande, T.N.; Patil, S.S.; Gharai, S.B.; Patil, S.R.; Durgawale, P.M. Menstrual hygiene among adolescent girls – A study from urban slum area. J. Fam. Med. Prim. Care 2018, 7, 1439–1445. [Google Scholar] [PubMed]
- Chauhan, P.; Shaik, R.A.; Anusha, D.V.B.; Sotala, M. A study to assess knowledge, attitude, and practices related to menstrual cycle and management of menstrual hygiene among school-going adolescent girls in a rural area of South India. Int. J. Med. Sci. Public Health. 2019, 8, 114–119. [Google Scholar] [CrossRef]
- Kavitha, M.; Jadhav, J.; Ranganath, T.S.; Vishwanatha. Assessment of knowledge and menstrual hygiene management among adolescent school girls of Nelamangala. Int. J. Community Med. Public Health 2018, 5, 4135–4139. [Google Scholar]
- Sangra, S.; Choudhary, N.; Kouser, W.; Faizal, I. Assessment of knowledge, attitude and practice about menstruation and menstrual hygiene among adolescent girls in rural area of district Kathua, Jammu and Kashmir. Int. J. Community Med. Public Health 2019, 6, 5215–5218. [Google Scholar] [CrossRef]
- Budimelli, S.; Chebrolu, K. Determinants of menstrual hygiene among the adolescent girls in a South Indian village. Int. J. Community Med. Public Health 2019, 6, 3915–3921. [Google Scholar] [CrossRef]
- Das, N.; Tasa, A.S. Menstrual hygiene: Knowledge and practices during menstruation among adolescent girls in urban slums of Jorhat district, Assam, India. Int. J. Community Med. Public Health 2019, 6, 3068–3075. [Google Scholar] [CrossRef]
- Parle, J.; Khatoon, Z. Knowledge, attitude, practice and perception about menstruation and menstrual hygiene among adolescent school girls in rural areas of Raigad district. Int. J. Community Med. Public Health 2019, 6, 2490–2497. [Google Scholar] [CrossRef]
- Vaishampayan, N.; Deshpande, S.R. Awareness of menstruation & related hygiene in adolescent girls—A comparative research study. Int. J. Health Sci. Res. 2019, 9, 65–68. [Google Scholar]
- Dhingra, R.; Kumar, A.; Kour, M. Knowledge and practices related to menstruation among tribal (Gujjar) adolescent girls. Stud. Ethno-Med. 2009, 3, 43–48. [Google Scholar] [CrossRef]
- Nagar, S.; Aimol, K.R. Knowledge of adolescent girls regarding menstruation in tribal areas of Meghalya. Stud. Tribes Tribals 2010, 8, 27–30. [Google Scholar] [CrossRef]
- Chothe, V.; Khubchandani, J.; Seabert, D.; Asalkar, M.; Rakshe, S.; Firke, A.; Midha, I.; Simmons, R. Students’ perceptions and doubts about menstruation in developing countries: A case study from India. Health Promot. Pract. 2014, 15, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Durge, P.M.; Varadpande, U. Impact assessment of health education in adolescent girls. J. Obstet. Gynecol. India 1996, 46, 368–372. [Google Scholar]
- Dasgupta, A.; Sarkar, M. Menstrual hygiene: How hygienic is the adolescent girl? Indian J. Community Med. 2008, 33, 77–80. [Google Scholar] [CrossRef]
- Nemade, D.; Anjenaya, S.; Gujar, R. Impact of health education on knowledge and practices about menstruation among adolescent school girls of Kalamboli, Navi-Mumbai. Health Popul. Perspect. Issues 2009, 32, 167–175. [Google Scholar]
- Jothy, K.; Kalaiselvi, S. Is menstrual hygiene and management an issue for the rural adolescent school girls? Elixir Soc Sci. 2012, 44, 7223–7228. [Google Scholar]
- Nair, M.K.C.; Paul, M.K.; Leena, M.; Thankachi, Y.; George, B.; Russell, P.S.; Pillai, H.V. Effectiveness of a reproductive sexual health education package among school going adolescents. Indian J. Pediatr. 2012, 79, S64–S68. [Google Scholar] [CrossRef]
- Anusree, P.C.; Roy, A.; Sara, A.B.; Faseela, V.C.M.; Babu, G.P.; Tamrakar, A. Knowledge regarding menstrual hygiene among adolescent girls in selected school, mangalore with a view to develop an information booklet. IOSR J. Nurs. Health Sci. 2014, 3, 55–60. [Google Scholar]
- Maji, S. A study on menstrual knowledge and practices among rural adolescent girls in Burdwan district, West Bengal. Int. J. Adv. Res. 2016, 4, 896–902. [Google Scholar] [CrossRef]
- Sharma, S.; Choudhary, S.; Saluja, N.; Gaur, D.R.; Kumari, S.; Pandey, S.M. Knowledge and practices about menstrual hygiene among school adolescent girls in Agroha village of Haryana. J. Evolution Med. Dent. Sci. 2016, 5, 389–392. [Google Scholar]
- Chauhan, K.; Mehta, U.; Ranaut, V. Assessment of knowledge and expressed practice regarding menstrual hygiene among the adolescent girls of govt. girls senior secondary school, Lakkar Bazar, Shimla, Himachal Pradesh. Int. J. Obstet. Perinat. Neonatal Nurs. 2016, 2, 19–25. [Google Scholar]
- Dixit, S.; Raghunath, D.; Rokade, R.; Nawaz, S.A.; Nagdeve, T.; Goyal, I. Awareness about Menstruation and Menstrual Hygiene Practices among Adolescent Girls in Central India. Natl. J. Community Med. 2016, 7, 468–473. [Google Scholar]
- Javalkar, S.R.; Akshaya, K.M. Menstrual hygiene practices among adolescent schoolgirls of rural Mangalore, Karnataka. Int. J. Med. Sci. Public Health 2017, 6, 1145–1149. [Google Scholar] [CrossRef]
- Vandana, V.; Simarjeet, K.; Neetu. Menstruation and menstrual hygiene practices of adolescent school going girls: A descriptive study. World J. Pharm. Pharm. Sci. 2017, 6, 2090–2102. [Google Scholar]
- Dabade, K.J.; Dabade, S.K. Comparative study of awareness and practices regarding menstrual hygiene among adolescent girls residing in urban and rural area. Int. J. Community Med. Public Health 2017, 4, 1284–1288. [Google Scholar] [CrossRef]
- Tiwari, A.; Ekka, I.J.; Thakur, R. Assessment of knowledge and practices regarding menstrual hygiene among adolescent girls of Government higher secondary school, station Murhipar, Rajnandgaon (C.G.). Int. J. Community Med. Public Health 2018, 5, 1335–1338. [Google Scholar] [CrossRef][Green Version]
- Gupta, P.; Gupta, J.; Singhal, G.; Meharda, B. Knowledge and practices pertaining to menstruation among the school going adolescent girls of UHTC/RHTC area of Government Medical College, Kota, Rajasthan. Int. J. Community Med. Public Health 2018, 5, 652–656. [Google Scholar] [CrossRef][Green Version]
- Singh, M.; Kundu, M.; Ray, S.; Jain, A. Menstrual hygiene and college absenteeism among medical students, Gurugram. J. Med. Sci. Clin. Res. 2018, 6, 423–427. [Google Scholar]
- Jyothi, B.; Hurakadli, K. Knowledge, practice and attitude of menstrual hygiene among school going adolescent girls: An interventional study in an urban school of Bagalkot city. Med. Innov. 2019, 8, 16–20. [Google Scholar]
- Choudhary, N.; Gupta, M.K. A comparative study of perception and practices regarding menstrual hygiene among adolescent girls in urban and rural areas of Jodhpur district, Rajasthan. J. Fam. Med. Prim. Care 2019, 8, 875–880. [Google Scholar]
- Gupta, S. An empirical study of managing menstrual hygiene in schools (A special reference to Government Upper Primary Schools in District Sambhal (Uttar Pradesh). Integr. J. Soc Sci. 2019, 6, 39–43. [Google Scholar]
- Ministry of Health and Family Welfare (MoHFW). Rashtriya Kishor Swasthya Karyakaram: Operational framework translating strategy into programmes. Government of India: New Delhi, India, 2014. [Google Scholar]
- Urban Management Centre (UMC). The ABC of Water, Sanitation and Hygiene (WASH) Improvement in Schools; ASAL: Gujarat, India, 2017. [Google Scholar]
- Mailman School of Public Health. MHM in TEN: Advancing the MHM Agenda in Teen; Third Annual Meeting; UNICEF; Columbia University: New York, NY, USA, 2016. [Google Scholar]
- Ministry of Human Resource Development (MoHRD). Clean India, Clean Schools: A Handbook; MoHRD: New Delhi, India, 2016.
- Sinha, R.N.; Paul, B. Menstrual hygiene management in India: The concerns. Indian J. Public Health 2018, 62, 71. [Google Scholar] [PubMed]
- DASRA. Spot On! Improving Menstrual Health and Hygiene in India, Report; DASRA: Delhi, India, 2014. [Google Scholar]
- Rose, G. Celebrating Womanhood: How Better Menstrual Hygiene Management Is the Path to Better Health, Dignity and Business; Report; Water Supply & Sanitation Collaborative Council: Geneva, Switzerland, 2013. [Google Scholar]
- World Bank. Toolkit on Hygiene, Sanitation and Water in Schools; World Bank: Washington, DC, USA, 2005. [Google Scholar]
- Sommer, M.; Figueroa, C.; Kwauk, C.; Jones, M.; Fyles, N. Attention to menstrual hygiene management in schools: An analysis of education policy documents in low- and middle-income countries. Int. J. Educ. Dev. 2017, 57, 73–82. [Google Scholar] [CrossRef]
- Marcus, R.; Page, E. Changing Discriminatory Norms Affecting Adolescent Girls through Communication Activities. A Review of Evidence; ODI: London, UK, 2014. [Google Scholar]
- Muralidharan, A.; Patil, H.; Patnaik, S. Unpacking the policy landscape for menstrual hygiene management: Implications for school WASH programmes in India. Waterlines 2015, 34, 79–91. [Google Scholar] [CrossRef]
- Philips-Howard, P.A.; Caruso, B.; Torondel, B.; Zulaika, G.; Sahin, M.; Sommer, M. Menstrual hygiene management among adolescent schoolgirls in low- and middle-income countries: Research priorities. Glob. Health Action 2016, 9, 33032. [Google Scholar] [CrossRef]
- Chandra-Mouli, V.; Patel, S.V. Mapping the knowledge and understanding of menarche, menstrual hygiene and menstrual health among adolescent girls in low- and middle-income countries. Reprod. Health 2017, 14, 30. [Google Scholar] [CrossRef]
- Hennegan, J.; Shannon, A.K.; Rubli, J.; Schwab, K.J.; Melendez-Torres, G.J. Women’s and girls’ experiences of menstruation in low- and middle-income countries: A systematic review and qualitative metasynthesis. PLoS Med. 2019, 16, e1002803. [Google Scholar] [CrossRef]
- International Institute for Population Sciences (IIPS); ICF. National Family Health Survey (NFHS-4), 2015–2016; IIPS: Mumbai, India, 2017. [Google Scholar]
- Byrne, J.; Rietdijk, W.; Pickett, K. Teachers as health promoters: Factors that influence early career teachers to engage with health and wellbeing education. Teach. Teach. Educ. 2019, 69, 289–299. [Google Scholar] [CrossRef]
- Sommers, M.; Mumtaz, Z.; Bhatti, A. Formative Menstrual Hygiene Management Research: Adolescent Girls in Baluchistan; Real Medicine Foundation: Islamabad, Pakistan, 2016. [Google Scholar]
- Bharadwaj, S.; Patkar, A. Menstrual Hygiene and Management in Developing Countries: Taking Stock; Junction Social: Mumbai, India, 2004. [Google Scholar]
- Katti, V.S.; Pimple, Y.; Saraf, A. Menstrual Hygiene in Rural India. Indian J. Public Health Res. Dev. 2017, 8, 978. [Google Scholar] [CrossRef]
- UNICEF. Advancing WASH in Schools Monitoring; Working Paper; UNICEF: New York, NY, USA, 2015. [Google Scholar]
- Sarah, H.; Mahon, T.; Cavill, S. Module six: Menstrual hygiene matters. In A Resource for Improving Menstrual Hygiene around the World, 1st ed.; Water Aid: London, UK, 2012. [Google Scholar]
- Vatsalya. Woman with Wings: Celebrating Womanhood, Menstrual Hygiene Management. Available online: http://vatsalya.org.in/wp-content/uploads/2015/01/Women-with-wings.pdf (accessed on 20 September 2018).
- Ina, J. WASH United‘s Menstrual Hygiene Management Training for Girls, Boys and Teachers Report; WASH United: Berlin, Germany; Available online: http://www.unicef.org/wash/schools/files/3.5_Jurga.pdf (accessed on 8 September 2018).
- Sharma, S.; Arora, K. Menstrual Hygiene Friendly Schools in India: A Need to Translate Research into Actions. Available online: https://mamtahimc.wordpress.com/2018/12/29/menstrual-hygiene-friendly-schools-in-india-a-need-to-translate-research-into-actions/ (accessed on 3 February 2019).
- Laganà, A.S.; La Rosa, V.L.; Rapisarda, A.M.C.; Valenti, G.; Sapia, F.; Chiofalo, B.; Rossetti, D.; Ban Frangež, H.; Vrtačnik Bokal, E.; Vitale, S.G. Anxiety and depression in patients with endometriosis: Impact and management challenges. Int. J. Womens Health 2017, 9, 323–330. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).