Mental Health Literacy Intervention on Help-Seeking in Athletes: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria
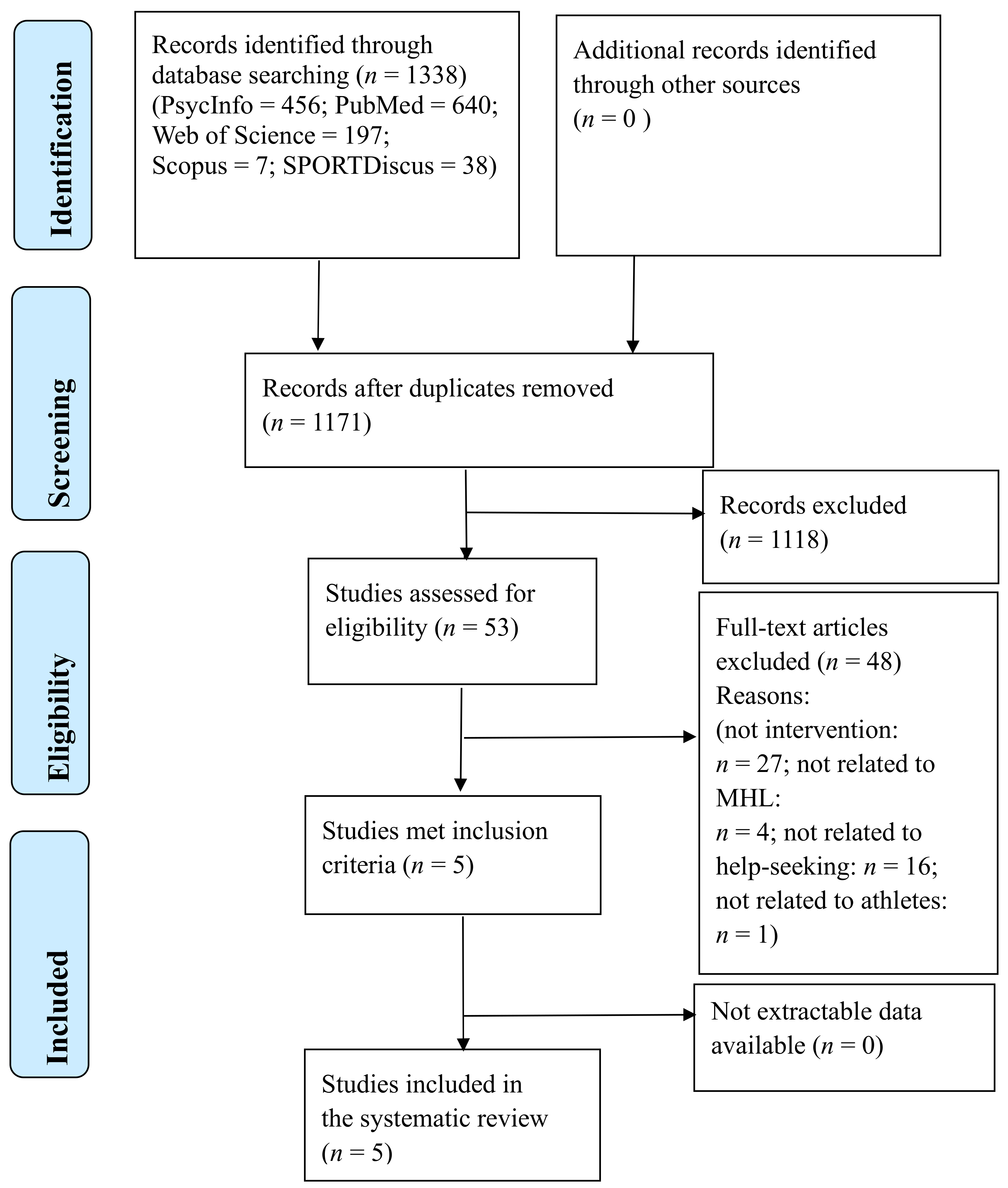
2.3. Study Selection
2.4. Data Collection Process and Data Items
2.5. Risk of Bias Assessment
2.6. Outcome Categories
2.7. Analysis
3. Results
3.1. Characteristics of the Included Programmes and Their Studies
3.2. Study Content of the Included Programmes and their Studies
3.3. Study Results of Included Programs and Their Studies
3.3.1. Effects on Mental Health Knowledge
3.3.2. Effects on Help-Seeking
3.3.3. Effects on Stigma
3.3.4. Effects on Additional Outcomes
3.4. Risk of Bias in Included Studies
3.5. Outcome Measure Validity Assessment
4. Discussion
4.1. Effects of Studies on Mental Health Knowledge Outcomes
4.2. Effects of the Studies on Help-Seeking Outcomes
4.3. Effects of the Studies on Stigma Outcomes
4.4. Effects of the Studies on Additional Outcomes
4.5. Improving the Methodological Quality of Studies
4.6. Consideration for Intervention Delivery Methods
4.7. Limitations and Recommendations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Reardon, C.L.; Hainline, B.; Aron, C.M.; Baron, D.; Baum, A.L.; Bindra, A.; Budgett, R.; Campriani, N.; Castaldelli-Maia, J.M.; Currie, A.; et al. Mental Health in Elite Athletes: International Olympic Committee Consensus Statement (2019). Br. J. Sports Med. 2019, 53, 667–699. [Google Scholar] [CrossRef]
- Schinke, R.J.; Stambulova, N.B.; Si, G.; Moore, Z. International Society of Sport Psychology Position Stand: Athletes’ Mental Health, Performance, and Development. Int. J. Sport Exerc. Psychol. 2018, 16, 622–639. [Google Scholar] [CrossRef]
- Gulliver, A.; Griffiths, K.M.; Mackinnon, A.; Batterham, P.J.; Stanimirovic, R. The Mental Health of Australian Elite Athletes. J. Sci. Med. Sport 2015, 18, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Gouttebarge, V.; Jonkers, R.; Moen, M.; Verhagen, E.; Wylleman, P.; Kerkhoffs, G. The Prevalence and Risk Indicators of Symptoms of Common Mental Disorders among Current and Former Dutch Elite Athletes. J. Sports Sci. 2017, 35, 2148–2156. [Google Scholar] [CrossRef] [PubMed]
- Stillman, M.A.; Glick, I.D.; McDuff, D.; Reardon, C.L.; Hitchcock, M.E.; Fitch, V.M.; Hainline, B. Psychotherapy for Mental Health Symptoms and Disorders in Elite Athletes: A Narrative Review. Br. J. Sports Med. 2019, 53, 767–771. [Google Scholar] [CrossRef] [PubMed]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Barriers and Facilitators to Mental Health Help-Seeking for Young Elite Athletes: A Qualitative Study. BMC Psychiatry 2012, 12, 157. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y. Anaysis of Relevant Factors to Excellent Sportsmen’s Mental Health. Master’s Thesis, Zhengzhou University, Zhengzhou, China, 2008. [Google Scholar]
- Rickwood, D.; Thomas, K. Conceptual Measurement Framework for Help-Seeking for Mental Health Problems. Psychol. Res. Behav. Manag. 2012, 5, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Rickwood, D.; Deane, F.P.; Wilson, C.J.; Ciarrochi, J. Young People’s Help-Seeking for Mental Health Problems. Aust. E-J. Adv. Ment. Health 2005, 4, 218–251. [Google Scholar] [CrossRef]
- Ajzen, I. From Intentions to Actions: A Theory of Planned Behavior. In Action Control: From Cognition to Behaviour; Springer: New York, NY, USA, 1985; pp. 11–39. [Google Scholar]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Perceived Barriers and Facilitators to Mental Health Help-Seeking in Young People: A Systematic Review. BMC Psychiatry 2010, 113. [Google Scholar] [CrossRef]
- Jorm, A.F.; Korten, A.E.; Jacomb, P.A.; Christensen, H.; Rodgers, B.; Pollitt, P. “Mental Health Literacy”: A Survey of the Public’s Ability to Recognise Mental Disorders and Their Beliefs about the Effectiveness of Treatment. Med. J. Aust. 1997, 166, 182–186. [Google Scholar] [CrossRef]
- Jorm, A.F.; Barney, L.J.; Christensen, H.; Highet, N.J.; Kelly, C.M.; Kitchener, B.A. Research on Mental Health Literacy: What We Know and What We Still Need to Know. Aust. N. Z. J. Psychiatry 2006, 40, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Jorm, A.F. Mental Health Literacy: Empowering the Community to Take Action for Better Mental Health. Am. Psychol. 2012, 67, 231–243. [Google Scholar] [CrossRef] [PubMed]
- Breslin, G.; Haughey, T.; O’Brien, W.; Robertson, A.; Caulfield, L.; Lawlor, M. Increasing Athlete Knowledge of Mental Health and Intentions to Seek Help: The State of Mind Ireland (SOMI) Pilot Program. J. Clin. Sport Psychol. 2018, 12, 39–56. [Google Scholar] [CrossRef]
- Han, Z.; Wang, D.; Ouyang, L.; Niu, P.; Yun, Z. Adaptation and Psychometric Properties of Mental Health Literacy Scale in Chinese Elite Athletes. Hubei Sport Sci. 2019, 38, 226–229. [Google Scholar]
- Kern, A.; Heininger, W.; Klueh, E.; Salazar, S.; Hansen, B.; Meyer, T.; Eisenberg, D. Athletes Connected: Results from a Pilot Project to Address Knowledge and Attitudes about Mental Health among College Student-Athletes. J. Clin. Sport Psychol. 2017, 11, 324–336. [Google Scholar] [CrossRef]
- Kutcher, S.; Wei, Y.; Coniglio, C. Mental Health Literacy: Past, Present, and Future. Can. J. Psychiatry 2016, 61, 154–158. [Google Scholar] [CrossRef] [PubMed]
- Wahto, R.S.; Swift, J.K.; Whipple, J.L. The Role of Stigma and Referral Source in Predicting College Student-Athletes’ Attitudes toward Psychological Help-Seeking. J. Clin. Sport Psychol. 2016, 10, 85–98. [Google Scholar] [CrossRef]
- Watson, J.C. College Student-Athletes’ Attitudes toward Help-Seeking Behavior and Expectations of Counseling Services. J. Coll. Stud. Dev. 2005, 46, 442–449. [Google Scholar] [CrossRef]
- Bauman, N.J. The Stigma of Mental Health in Athletes: Are Mental Toughness and Mental Health Seen as Contradictory in Elite Sport? Br. J. Sports Med. 2016, 50, 135–136. [Google Scholar] [CrossRef]
- Gulliver, A.; Griffiths, K.M.; Christensen, H.; Mackinnon, A.; Calear, A.L.; Parsons, A.; Bennett, K.; Batterham, P.J.; Stanimirovic, R. Internet-Based Interventions to Promote Mental Health Help-Seeking in Elite Athletes: An Exploratory Randomized Controlled Trial. J. Med. Internet Res. 2012, 14, e69. [Google Scholar] [CrossRef]
- Breslin, G.; Shannon, S.; Haughey, T.; Donnelly, P.; Leavey, G. A Systematic Review of Interventions to Increase Awareness of Mental Health and Well-Being in Athletes, Coaches and Officials. Syst. Rev. 2017, 6, 117. [Google Scholar] [CrossRef]
- Mallett, R.; Hagen-Zanker, J.; Slater, R.; Duvendack, M. The Benefits and Challenges of Using Systematic Reviews in International Development Research. J. Dev. Eff. 2012, 4, 445–455. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. J. Clin. Epidemiol. 2009, 62, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Libr. 2008, 4, 265. [Google Scholar] [CrossRef]
- Morgan, A.J.; Ross, A.; Reavley, N.J. Systematic Review and Meta-Analysis of Mental Health First Aid Training: Effects on Knowledge, Stigma, and Helping Behaviour. PLoS ONE 2018, 13, e0197102. [Google Scholar] [CrossRef]
- Stang, A. Critical Evaluation of the Newcastle-Ottawa Scale for the Assessment of the Quality of Nonrandomized Studies in Meta-Analyses. Eur. J. Epidemiol. 2010, 603–605. [Google Scholar] [CrossRef]
- Knight, E.L. Self-Help and Serious Mental Illness.Pdf. Medscape Gen. Med. 2006, 8, 68. [Google Scholar]
- Cohen, J. A Power Primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Pierce, D.; Pierce, D.; Liaw, S.; Dobell, J.; Anderson, R. Australian Rural Football Club Leaders as Mental Health Advocates: An Investigation of the Impact of the Coach the Coach Project. Int. J. Ment. Health Syst. 2010, 4, 10. [Google Scholar] [CrossRef] [PubMed]
- Van Raalte, J.L.; Cornelius, A.E.; Andrews, S.; Diehl, N.S.; Brewer, B.W. Mental Health Referral for Student-Athletes: Web-Based Education and Training. J. Clin. Sport Psychol. 2015, 9, 197–212. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; Robertson, J.; Peterson, J.; Welch, V.; Losos, M. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta- Analysis Bias and Confounding Newcastle-Ottowa Scale; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2011; Available online: http://www.ohri.ca/programs/clinicalepidemiology/oxford.htm (accessed on 30 September 2020).
- Xu, Z.; Huang, F.; Kösters, M.; Staiger, T.; Becker, T.; Thornicroft, G.; Rüsch, N. Effectiveness of Interventions to Promote Help-Seeking for Mental Health Problems: Systematic Review and Meta-Analysis. Psychol. Med. 2018, 48, 2658–2667. [Google Scholar] [CrossRef] [PubMed]
- WHO. Improving Health Systems and Services for Mental Health; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Wei, S.; Zhuozhuo, S.; Wang, S.; Hall, B.J. Barriers to Professional Mental Health Help-Seeking Among Chinese Adults: A Systematic Review. Front. Psychiatry 2020, 11, 442. [Google Scholar] [CrossRef]
- Scott, A.J.; Webb, T.L.; Rowse, G. Self-Help Interventions for Psychosis: A Meta-Analysis. Clin. Psychol. Rev. 2015, 39, 96–112. [Google Scholar] [CrossRef] [PubMed]
- Rickwood, D.; Bradford, S. The Role of Self-Help in the Treatment of Mild Anxiety Disorders in Young People: An Evidence-Based Review. Psychol. Res. Behav. Manag. 2012, 5, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Schnyder, N.; Panczak, R.; Groth, N.; Schultze-Lutter, F. Association between Mental Health-Related Stigma and Active Help-Seeking: Systematic Review and Meta-Analysis. Br. J. Psychiatry 2017, 210, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Mojtabai, R.; Olfson, M.; Sampson, N.A.; Jin, R.; Druss, B.; Wang, P.S.; Wells, K.B.; Pincus, H.A.; Kessler, R.C. Barriers to Mental Health Treatment: Results from the National Comorbidity Survey Replication. Psychol. Med. 2011, 41, 1751–1761. [Google Scholar] [CrossRef] [PubMed]
- Bonabi, H.; Müller, M.; Ajdacic-Gross, V.; Eisele, J.; Rodgers, S.; Seifritz, E.; Rössler, W.; Rüsch, N. Mental Health Literacy, Attitudes to Help Seeking, and Perceived Need as Predictors of Mental Health Service Use: A Longitudinal Study. J. Nerv. Ment. Dis. 2016, 204, 321–324. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Hayden, J.A.; Kutcher, S.; Zygmunt, A.; McGrath, P. The Effectiveness of School Mental Health Literacy Programs to Address Knowledge, Attitudes and Help Seeking among Youth. Early Interv. Psychiatry 2013, 7, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, S.; Foo, J.C.; Nishida, A.; Ogawa, S.; Togo, F.; Sasaki, T. Mental Health Literacy Programs for School Teachers: A Systematic Review and Narrative Synthesis. Early Interv. Psychiatry 2020, 14, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Kutcher, S.; Wei, Y.; Gilberds, H.; Ubuguyu, O.; Njau, T.; Brown, A.; Sabuni, N.; Magimba, A.; Perkins, K. A School Mental Health Literacy Curriculum Resource Training Approach: Effects on Tanzanian Teachers’ Mental Health Knowledge, Stigma and Help-Seeking Efficacy. Int. J. Ment. Health Syst. 2016, 10, 50. [Google Scholar] [CrossRef] [PubMed]
- Kidger, J.; Stone, T.; Tilling, K.; Brockman, R.; Campbell, R.; Ford, T.; Hollingworth, W.; King, M.; Araya, R.; Gunnell, D. A Pilot Cluster Randomised Controlled Trial of a Support and Training Intervention to Improve the Mental Health of Secondary School Teachers and Students—The WISE (Wellbeing in Secondary Education) Study. BMC Public Health 2016, 16, 1–14. [Google Scholar] [CrossRef]
- Jorm, A.F.; Kitchener, B.A.; Sawyer, M.G.; Scales, H.; Cvetkovski, S. Mental Health First Aid Training for High School Teachers: A Cluster Randomized Trial. BMC Psychiatry 2010, 10. [Google Scholar] [CrossRef] [PubMed]
- Moor, S.; Ann, M.; Hester, M.; Elisabeth, W.J.; Robert, E.; Robert, W.; Caroline, B. Improving the Recognition of Depression in Adolescence: Can We Teach the Teachers? J. Adolesc. 2007, 30, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Rossetto, A.; Jorm, A.F.; Reavley, N.J. Predictors of Adults’ Helping Intentions and Behaviours towards a Person with a Mental Illness: A Six-Month Follow-up Study. Psychiatry Res. 2016, 240, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. BMC Med. 2010, 8, 18. [Google Scholar] [CrossRef] [PubMed]
- Seidler, Z.E.; Dawes, A.J.; Rice, S.M.; Oliffe, J.L.; Dhillon, H.M. The Role of Masculinity in Men’s Help-Seeking for Depression: A Systematic Review. Clin. Psychol. Rev. 2016, 49, 106–118. [Google Scholar] [CrossRef] [PubMed]
- Swann, C.; Telenta, J.; Draper, G.; Liddle, S.; Fogarty, A.; Hurley, D.; Vella, S. Youth Sport as a Context for Supporting Mental Health: Adolescent Male Perspectives. Psychol. Sport Exerc. 2018, 35, 55–64. [Google Scholar] [CrossRef]
- Reeves, B.C.; Deeks, J.J.; Higgins, J.P.T.; Wells, G.A. Including Non-Randomized Studies. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J.P.T., Green, S., Eds.; John Wiley & Sons: Chichester, UK, 2008. [Google Scholar]
- O’Connor, M.; Casey, L. The Mental Health Literacy Scale (MHLS): A New Scale-Based Measure of Mental Health Literacy. Psychiatry Res. 2015, 229, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.; von Sternberg, K.; Davis, K. Expanding a Measure of Mental Health Literacy: Development and Validation of a Multicomponent Mental Health Literacy Measure. Psychiatry Res. 2016, 243, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Dias, P.; Campos, L.; Almeida, H.; Palha, F. Mental Health Literacy in Young Adults: Adaptation and Psychometric Properties of the Mental Health Literacy Questionnaire. Int. J. Environ. Res. Public Health 2018, 15, 1318. [Google Scholar] [CrossRef]
- Wantland, D.J.; Portillo, C.J.; Holzemer, W.L.; Slaughter, R.; McGhee, E.M. The Effectiveness of Web-Based vs. Non-Web-Based Interventions: A Meta-Analysis of Behavioral Change Outcomes. J. Med. Internet Res. 2004, 6. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Breslin, G.; Haughey, T.J.; Donnelly, P.; Kearney, C.; Prentice, G. Promoting Mental Health Awareness in Sport Clubs. J. Public Ment. Health 2017, 16, 55–62. [Google Scholar] [CrossRef]
- Maiman, L.A.; Becker, M.H. The Health Belief Model: Origins and Correlates in Psychological Theory. Health Educ. Behav. 1977, 2, 336–353. [Google Scholar] [CrossRef]
- Bird, M.D.; Chow, G.M.; Cooper, B.T. Student-Athletes’ Mental Health Help-Seeking Experiences: A Mixed Methodological Approach. J. Coll. Stud. Psychother. 2020, 34, 59–77. [Google Scholar] [CrossRef]
| First Author (Year) | Country | Athlete Type | Participants (n) | % Female | Mean Age (SD), Range | Type of Sport |
|---|---|---|---|---|---|---|
| Breslin et al. [15] | IR | Student-athletes | Pre: 100; Post: 100; Follow-up: 15 | 41% | 20.78 ± 2.91 Range: Not reported | Soccer, Gaelic football, rugby, hockey, netball, and golf |
| Gulliver et al. [22] | AU | Elite athletes | Pre:59; Post: 59; Follow-up: 40 | 72.9% | 25.5 (SD: Not reported) (median 24.5) Range = 18–48 | Not reported |
| Kern et al. [17] | US | Student-athletes | Pre:652 *; Post: 626 | 25.1% (unknown: 46.6%) | M (SD): Not reported Ranged = 18–23 | Not reported |
| Pierce et al. [31] | AU | Elite athletes | Pre:275; Post: 96 | Not reported | M (SD): Not reported The median age = 21 Range 15–50 | Football |
| Van Raalte et al. [32] | US | Student-athletes | Pre: 153; Post: 146; | Pre: 70.5%; Post: 67.3% | 19.63 (SD = 1.76) Range: Not reported | Baseball, fencing, football, basketball, soccer, lacrosse, rugby, skiing, softball, squash, gymnastics, track and field, swimming and diving, tennis, golf, and volleyball. |
| First Author (Year) | Intervention Deliverer | Study Design | Control Group | Delivery Method | Follow-Up Points | Duration Length * n Sessions |
|---|---|---|---|---|---|---|
| Breslin et al. [15] | Experienced mental health and well-being tutors | CT | Active | Face-to-face | Post, 3-month * | 1.25 h * 1 |
| Gulliver et al. [22] | N/A | RCT | Active | Online | Post, 3-month | Available 24 h a day, seven days a week |
| Kern et al. [17] | Members of the intervention team | Pre- and post- design | No comparison | Face-to-face | Post | 1 h * 1 |
| Pierce et al. [31] | A MHFA qualified instructor | CT | unknown | Face-to-face | 6-month | 12 h |
| Van Raalte et al. [32] | N/A | RCT | Active | Online | Post | One day (online session lasted at least 10 min) |
| First Author (Year) | Summarize Major Elements |
|---|---|
| Breslin et al. [15] | (1) Mental health information; (2) seeking help; (3) mindfulness practice; and (4) resilience |
| Gulliver et al. [22] | (1) Mental health information; (2) seeking help; (3) stigma; and (4) two effective depression treatments |
| Kern et al. [17] | Mental health information; (2) seeking help; (3) stigma; and (4) supporting friends |
| Pierce et al. [31] | (1) Mental health information; and (2) seeking help; |
| Van Raalte et al. [32] | (1) Mental health information; (2) seeking help; (3) stigma; and (4) information about referral |
| Author (Year) | Effect Size | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Knowledge | Help-Seeking Attitudes | Help-Seeking Intentions | Help-Seeking Behaviours | Stigma | |||||
| Breslin et al. [15] | d a = 0.16 *** | Not reported | d a = 0.06 *** | Not reported | Not reported | ||||
| Gulliver et al. [22] | d1 a = 0.88 ** d1 b = 0.74 ** | d2 a = 0.88 ** d2 b = 0.77 ** | d a = 0.29 d b = −0.14 | d3 a = 0.20 d3 b = 0.05 | d4 a = −0.04 d4 b = −0.36 | OR5 = 57.38, 95% CI5 0.85–3868.09 a OR5 =3.48, 95% CI5 0.10–122.32 b | OR6 = 0.74, 95% CI5 0.03–19.12 a OR6 = 0.21, 95% CI5 0.01–7.79 b | d7 a = 0.25 * d7 b = 0.09 ** | d8 a = 0.03 ** d8 b = 0.53 * |
| Kern et al. [17] | N/A | d a = 0.44 *** | Not reported | Not reported | d a = 0.20 *** | d a = 0.06 | |||
| Pierce et al. [31] | Not reported | N/A | Not reported | Not reported | N/A | ||||
| Van Raalte et al. [32] | da = 0.24 * | Not reported | Not reported | Not reported | Not reported | ||||
| Author (Year) | Variable | Intervention Group (Mean (SD)) | Control Group [Mean (SD)] | Effect Size | ||
|---|---|---|---|---|---|---|
| Pre-Test | Post-Test/Follow-Up Test | Pre-Test | Post-Test/Follow-Up Test | |||
| Breslin et al. [15] | Resilience | 3.39 (0.60) | 3.37 (0.74) a | 3.66 (0.72) | 3.62 (0.78) a | d a = 0.33 |
| Well-being | 26.49 (3.67) | 27.32 (4.31) a | 26.36 (4.05) | 26.81 (4.85) a | d a = 0.11 | |
| Kern et al. [17] | Supporting teammate: Q1 | 2.79 (1.01) | 3.10 (0.95) a | - | - | d a = 0.30 *** |
| Supporting teammate: Q2 | 2.62 (0.87) | 3.00 (0.72) a | - | - | d a = 0.47 *** | |
| Supporting teammate: Q3 | 2.75 (1.23) | 3.41 (0.73) a | - | - | d a = 0.70 *** | |
| Van Raalte et al. [32] | Self-efficacy | 8.30 (1.94) | 9.03 (1.67) a | 8.15 (1.99) | 7.69 (2.77) a | d a = 0.59 ** |
| Study | Criteria 1 | Criteria 2 | Criteria 3 | Criteria 4 | Criteria 5 | Criteria 6 | Criteria 7 | Classification |
|---|---|---|---|---|---|---|---|---|
| Gulliver et al. [22] | + | + | + | ? | + | + | + | + |
| Van Raalte et al. [32] | ? | ? | ? | ? | + | + | + | ? |
| Study | Selection | Comparability | Exposure (for Study 1 and 3)/Outcome (for Study 2) | Classification |
|---|---|---|---|---|
| Breslin et al. [15] | **** | * | ** | Low risk of bias |
| Kern et al. [17] | ***** | - | * | Low risk of bias |
| Pierce et al. [31] | *** | - | - | High risk of bias |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bu, D.; Chung, P.-K.; Zhang, C.-Q.; Liu, J.; Wang, X. Mental Health Literacy Intervention on Help-Seeking in Athletes: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 7263. https://doi.org/10.3390/ijerph17197263
Bu D, Chung P-K, Zhang C-Q, Liu J, Wang X. Mental Health Literacy Intervention on Help-Seeking in Athletes: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(19):7263. https://doi.org/10.3390/ijerph17197263
Chicago/Turabian StyleBu, Danran, Pak-Kwong Chung, Chun-Qing Zhang, Jingdong Liu, and Xiang Wang. 2020. "Mental Health Literacy Intervention on Help-Seeking in Athletes: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 19: 7263. https://doi.org/10.3390/ijerph17197263
APA StyleBu, D., Chung, P.-K., Zhang, C.-Q., Liu, J., & Wang, X. (2020). Mental Health Literacy Intervention on Help-Seeking in Athletes: A Systematic Review. International Journal of Environmental Research and Public Health, 17(19), 7263. https://doi.org/10.3390/ijerph17197263





