Association between Migrant Women’s Legal Status and Prenatal Care Utilization in the PreCARE Cohort
Abstract
1. Introduction
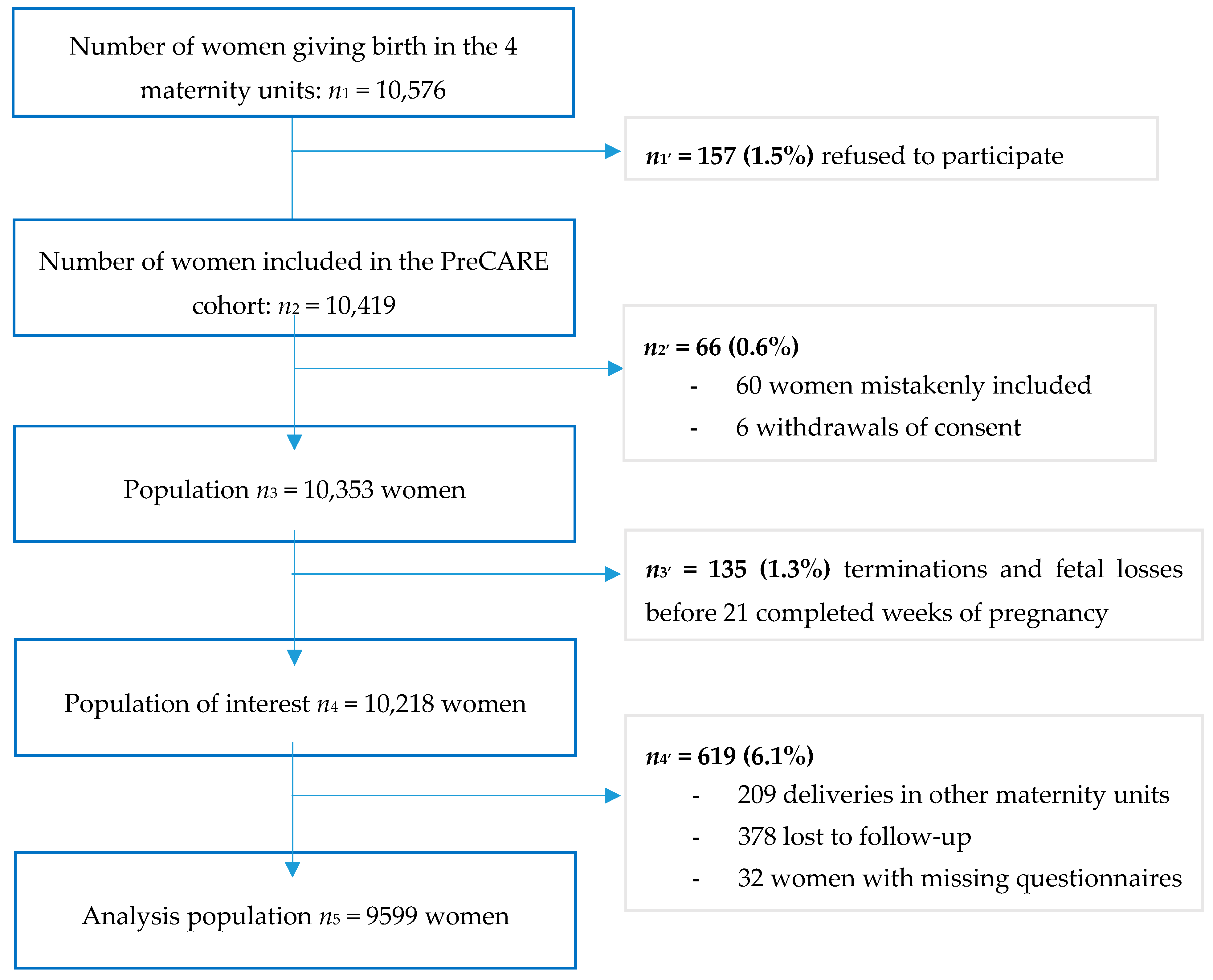
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Inadequate Prenatal Care * | |||
|---|---|---|---|
| n | % | p ** | |
| Migrants with French or European nationality not born in SSA (n = 1174) | 360 | 30.7 | 0.2 |
| Migrants with French or European nationality born in SSA (n = 381) | 131 | 34.4 | |
| Other legal migrants not born in SSA (n = 1929) | 740 | 38.4 | 0.002 |
| Legal migrants born in SSA (n = 877) | 391 | 44.6 | |
| Undocumented migrants not born in SSA (n = 407) | 198 | 48.6 | 0.04 |
| Undocumented migrants born in SSA (n = 308) | 174 | 56.5 | |
| Inadequate Prenatal Care * | ||
|---|---|---|
| Complete cases (n = 8869) | Multiple imputations (n = 9599) | |
| aOR [95% CI] 1 | aOR [95% CI] 1 | |
| Nonmigrants (n = 4523) | 1 | 1 |
| Migrants with French or European nationality (n = 1555) | 1.17 [1.02–1.33] | 1.17 [1.03–1.33] |
| Other legal migrants (n = 2806) | 1.61 [1.44–1.80] | 1.60 [1.43–1.78] |
| Undocumented migrants (n = 715) | 2.58 [2.16–3.09] | 2.58 [2.16–3.07] |
| Inadequate Prenatal Care * | ||
|---|---|---|
| OR [95% CI] | aOR [95% CI] 1 | |
| Nonmigrants (n = 4511) | 1 | 1 |
| Migrants with French or European nationality (n = 1508) | 1.24 [1.09–1.42] | 1.09 [0.95–1.26] |
| Legal migrants (n = 2527) | 1.79 [1.61–1.99] | 1.49 [1.32–1.67] |
| Undocumented migrants (n = 569) | 2.65 [2.21–3.18] | 2.19 [1.80–2.67] |
| Study Population (n = 9599) | Women Excluded (n = 619) | ||||
|---|---|---|---|---|---|
| n | % | n | % | p | |
| Legal status | 0.3 | ||||
| Nonmigrants | 4523 | 47.1 | 277 | 44.7 | |
| Migrants with French or European nationality | 1555 | 16.2 | 93 | 15.0 | |
| Other legal migrants | 2806 | 29.2 | 154 | 24.9 | |
| Undocumented migrants | 715 | 7.4 | 54 | 8.7 | |
| Missing | 0 | 0.0 | 41 | 6.6 | |
| Maternal birthplace | <0.001 | ||||
| Metropolitan France | 4363 | 45.5 | 262 | 42.4 | |
| Oversea French territories | 166 | 1.7 | 15 | 2.4 | |
| Europe (other) | 467 | 4.9 | 38 | 6.1 | |
| North Africa | 2116 | 22.0 | 103 | 16.6 | |
| Sub-Saharan Africa | 1566 | 16.3 | 115 | 18.6 | |
| Asia–Middle East | 626 | 6.5 | 27 | 4.4 | |
| Others | 295 | 3.1 | 59 | 9.5 | |
| Missing | 0 | 0.0 | 0 | 0.0 | |
| Maternal age (years) | <0.001 | ||||
| <20 | 128 | 1.3 | 19 | 3.1 | |
| [20,21,22,23,24,25] | 1303 | 13.6 | 99 | 16.0 | |
| [25,26,27,28,29,30] | 2912 | 30.3 | 184 | 29.7 | |
| [30,31,32,33,34,35,36,37,38,39,40] | 4793 | 49.9 | 271 | 43.8 | |
| ≥40 | 463 | 4.8 | 46 | 7.4 | |
| Missing | 0 | 0.0 | 0 | 0.0 | |
| Living alone | 1409 | 14.7 | 130 | 21.0 | <0.001 |
| Missing | 27 | 0.3 | 41 | 6.6 | |
| Deprivation index * | <0.001 | ||||
| 0 criterion | 6322 | 65.9 | 340 | 54.9 | |
| 1 criterion | 1681 | 17.5 | 97 | 15.7 | |
| 2 criteria | 839 | 8.7 | 66 | 10.7 | |
| 3 or 4 criteria | 660 | 6.9 | 67 | 10.8 | |
| Missing | 97 | 1.0 | 49 | 7.9 | |
| Schooling level | 0.2 | ||||
| ≤Primary school | 667 | 6.9 | 37 | 6.0 | |
| Middle school | 1746 | 18.2 | 98 | 15.8 | |
| High school | 2299 | 24.0 | 124 | 20.0 | |
| University | 4792 | 49.9 | 318 | 51.4 | |
| Missing | 95 | 1.0 | 42 | 6.8 | |
| Social welfare coverage | 0.02 | ||||
| Standard health insurance | 1368 | 14.3 | 86 | 13.9 | |
| Complementary health insurance | 6001 | 62.5 | 338 | 54.6 | |
| Universal health coverage | 1191 | 12.4 | 69 | 11.1 | |
| State medical assistance | 586 | 6.1 | 38 | 6.1 | |
| No healthcare insurance | 367 | 3.8 | 38 | 6.1 | |
| Missing | 86 | 0.9 | 50 | 8.1 | |
References
- Les Immigrés Récemment Arrivés en France-Insee Première-1524. Available online: https://www.insee.fr/fr/statistiques/1281393 (accessed on 29 July 2020).
- Institut National de la Statistique et des Etudes Economiques. Les Naissances en 2018. 2019. Available online: https://www.insee.fr/fr/statistiques/4190314?sommaire=4190525 (accessed on 29 July 2020).
- Pedersen, G.S.; Grøntved, A.; Mortensen, L.H.; Andersen, A.-M.N.; Rich-Edwards, J. Maternal Mortality Among Migrants in Western Europe: A Meta-Analysis. Matern. Child Health J. 2013, 18, 1628–1638. [Google Scholar] [CrossRef] [PubMed]
- Akker, T.V.D.; Van Roosmalen, J. Maternal mortality and severe morbidity in a migration perspective. Best Pr. Res. Clin. Obstet. Gynaecol. 2016, 32, 26–38. [Google Scholar] [CrossRef] [PubMed]
- Sauvegrain, P.; Stewart, Z.; Gonthier, C.; Saurel-Cubizolles, M.J.; Saucedo, M.; Azria, E. Access to prenatal care and maternal health of immigrant women in France. Bull. Epidémiol. Hebd. 2017, 19–20, 389–395. [Google Scholar]
- Almeida, L.; Santos, C.C.; Caldas, J.M.P.; Ayres-De-Campos, D.; Dias, S.F. Obstetric care in a migrant population with free access to health care. Int. J. Gynecol. Obstet. 2014, 126, 244–247. [Google Scholar] [CrossRef] [PubMed]
- Zeitlin, J.; Combier, E.; Levaillant, M.; Lasbeur, L.; Pilkington, H.; Charreire, H.; Rivera, L. Neighbourhood socio-economic characteristics and the risk of preterm birth for migrant and non-migrant women: A study in a French district. Paediatr. Périnat. Epidemiol. 2011, 25, 347–356. [Google Scholar] [CrossRef]
- Zeitlin, J.; Bucourt, M.; Rivera, L.; Topuz, B.; Papiernik, E. Preterm birth and maternal country of birth in a French district with a multiethnic population. BJOG Int. J. Obstet. Gynaecol. 2004, 111, 849–855. [Google Scholar] [CrossRef]
- De Jong, L.; Pavlova, M.; Winters, M.; Rechel, B. A systematic literature review on the use and outcomes of maternal and child healthcare services by undocumented migrants in Europe. Eur. J. Public Health 2017, 27, 990–997. [Google Scholar] [CrossRef]
- Saurel-Cubizolles, M.-J.; Saucedo, M.; Drewniak, N.; Blondel, B.; Bouvier-Colle, M.-H. Santé périnatale des femmes étrangères en France. Bull Épidémiol. Hebd. 2012, 2, 3–4. [Google Scholar]
- Gagnon, A.J.; Zimbeck, M.; Zeitlin, J. Migration to western industrialised countries and perinatal health: A systematic review. Soc. Sci. Med. 2009, 69, 934–946. [Google Scholar] [CrossRef]
- Kandasamy, T.; Cherniak, R.; Shah, R.; Yudin, M.H.; Spitzer, R. Obstetric Risks and Outcomes of Refugee Women at a Single Centre in Toronto. J. Obstet. Gynaecol. Can. 2014, 36, 296–302. [Google Scholar] [CrossRef]
- Philibert, M.; Deneux-Tharaux, C.; Bouvier-Colle, M. Can excess maternal mortality among women of foreign nationality be explained by suboptimal obstetric care? BJOG Int. J. Obstet. Gynaecol. 2008, 115, 1411–1418. [Google Scholar] [CrossRef] [PubMed]
- Deneux-Tharaux, C.; Saucedo, M. Epidemiology of maternal mortality in France, 2010–2012. Gynécol. Obs. Fertil. Sénol. 2017, 45, S8–S21. [Google Scholar] [CrossRef] [PubMed]
- Boulkedid, R.; Sibony, O.; Bossu-Salvador, C.; Oury, J.; Alberti, C. Monitoring healthcare quality in an obstetrics and gynaecology department using a CUSUM chart. BJOG Int. J. Obstet. Gynaecol. 2010, 117, 1225–1235. [Google Scholar] [CrossRef] [PubMed]
- Azria, E.; Stewart, Z.; Gonthier, C.; Estellat, C.; Deneux-Tharaux, C. Social inequalities in maternal health. Gynecol. Obstet. Fertil. 2015, 43, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Linard, M.; Blondel, B.; Estellat, C.; Deneux-Tharaux, C.; Luton, D.; Oury, J. Association between inadequate antenatal care utilisation and severe perinatal and maternal morbidity: An analysis in the PreCARE cohort. BJOG Int. J. Obstet. Gynaecol. 2018, 125, 587–595. [Google Scholar] [CrossRef]
- Heaman, M.; Bayrampour, H.; Kingston, D.; Blondel, B.; Gissler, M.; Roth, C.; Alexander, S.; Gagnon, A.J. Migrant Women’s Utilization of Prenatal Care: A Systematic Review. Matern. Child Health J. 2012, 17, 816–836. [Google Scholar] [CrossRef]
- Gonthier, C.; Estellat, C.; Deneux-Tharaux, C.; Blondel, B.; Alfaiate, T.; Schmitz, T.; Oury, J.-F.; Mandelbrot, L.; Luton, D.; Ravaud, P.; et al. Association between maternal social deprivation and prenatal care utilization: The PreCARE cohort study. BMC Pregnancy Childbirth 2017, 17, 126. [Google Scholar] [CrossRef]
- Gieles, N.C.; Tankink, J.B.; Van Midde, M.; Düker, J.; Van Der Lans, P.; Wessels, C.M.; Bloemenkamp, K.W.M.; Bonsel, G.; Akker, T.V.D.; Goosen, S.; et al. Maternal and perinatal outcomes of asylum seekers and undocumented migrants in Europe: A systematic review. Eur. J. Public Health 2019, 29, 714–723. [Google Scholar] [CrossRef]
- Nay, O.; Béjean, S.; Benamouzig, D.; Bergeron, H.; Castel, P.; Ventelou, B. Achieving universal health coverage in France: Policy reforms and the challenge of inequalities. Lancet 2016, 387, 2236–2249. [Google Scholar] [CrossRef]
- Kotelchuck, M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. Am. J. Public Health 1994, 84, 1414–1420. [Google Scholar] [CrossRef]
- Alexander, G.R.; Kotelchuck, M. Quantifying the adequacy of prenatal care: A comparison of indices. Public Health Rep. 1996, 111, 408–419. [Google Scholar] [PubMed]
- Ananth, C.V.; Schisterman, E.F. Confounding, causality, and confusion: The role of intermediate variables in interpreting observational studies in obstetrics. Am. J. Obstet. Gynecol. 2017, 217, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Little, R.; Rubin, D. Statistical Analysis with Missing Data, 3rd ed.; Wiley: Hoboken, NJ, USA, 2019. [Google Scholar]
- Korinek, K.; Smith, K.R. Prenatal care among immigrant and racial-ethnic minority women in a new immigrant destination: Exploring the impact of immigrant legal status. Soc. Sci. Med. 2011, 72, 1695–1703. [Google Scholar] [CrossRef]
- Wolff, H.; Stalder, H.; Epiney, M.; Walder, A.; Irion, O.; Morabia, A. Health care and illegality: A survey of undocumented pregnant immigrants in Geneva. Soc. Sci. Med. 2005, 60, 2149–2154. [Google Scholar] [CrossRef]
- Kentoffio, K.; Berkowitz, S.A.; Atlas, S.J.; Oo, S.A.; Percac-Lima, S. Use of maternal health services: Comparing refugee, immigrant and US-born populations. Matern. Child Health J. 2016, 20, 2494–2501. [Google Scholar] [CrossRef] [PubMed]
- Stewart, E.W.; De Souza, L.R.; Yudin, M.H. Access to Prenatal Care for Pregnant Refugee Women in Toronto, Ontario, Canada: An Audit Study. J. Health Care Poor Underserved 2018, 29, 687–700. [Google Scholar] [CrossRef] [PubMed]
- Malebranche, M.; Norrie, E.; Hao, S.; Brown, G.; Talavlikar, R.; Hull, A.; De Vetten, G.; Nerenberg, K.A.; Metcalfe, A.; Fabreau, G. Antenatal Care Utilization and Obstetric and Newborn Outcomes Among Pregnant Refugees Attending a Specialized Refugee Clinic. J. Immigr. Minor. Health 2019, 22, 467–475. [Google Scholar] [CrossRef]
- Vignier, N.; Dray-Spira, R.; Bouchaud, O.; Du Loû, A.D.; Chauvin, P. Refusal to provide health care to sub-Saharan African migrants in France. Lancet Public Health 2018, 3, e12. [Google Scholar] [CrossRef]
- Atkins, D.N.; Held, M.L.; Lindley, L.C. The impact of expanded health insurance coverage for unauthorized pregnant women on prenatal care utilization. Public Health Nurs. 2018, 35, 459–465. [Google Scholar] [CrossRef]
- Almeida, L.; Caldas, J.M.P.; Ayres-De-Campos, D.; Barrientos, D.M.S.; Dias, S.F. Maternal Healthcare in Migrants: A Systematic Review. Matern. Child Health J. 2013, 17, 1346–1354. [Google Scholar] [CrossRef]
- Van Hanegem, N.; Miltenburg, A.S.; Zwart, J.J.; Bloemenkamp, K.W.M.; Van Roosmalen, J. Severe acute maternal morbidity in asylum seekers: A two-year nationwide cohort study in the Netherlands. Acta Obstet. Gynecol. Scand. 2011, 90, 1010–1016. [Google Scholar] [CrossRef] [PubMed]
- Choté, A.A.; Koopmans, G.T.; Redekop, W.K.; De Groot, C.J.M.; Hoefman, R.J.; Jaddoe, V.W.V.; Hofman, A.; Steegers, E.A.P.; MacKenbach, J.P.; Trappenburg, M.; et al. Explaining Ethnic Differences in Late Antenatal Care Entry by Predisposing, Enabling and Need Factors in the Netherlands. The Generation R Study. Matern. Child Health J. 2010, 15, 689–699. [Google Scholar] [CrossRef] [PubMed]
- Colón-Burgos, J.F.; Colón-Jordan, H.M.; Reyes-Ortiz, V.E.; Marin-Centeno, H.A.; Rios-Mota, R. Disparities and Barriers Encountered by Immigrant Dominican Mothers Accessing Prenatal Care Services in Puerto Rico. J. Immigr. Minor. Health 2013, 16, 646–651. [Google Scholar] [CrossRef] [PubMed]
- Geltman, P.L.; Meyers, A. Immigration Legal Status and Use of Public Programs and Prenatal Care. J. Immigr. Health 1999, 1, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Herbst, M.A.; Mercer, B.M.; Beazley, D.; Meyer, N.; Carr, T.; Herbst, M. Relationship of prenatal care and perinatal morbidity in low-birth-weight infants. Am. J. Obstet. Gynecol. 2003, 189, 930–933. [Google Scholar] [CrossRef]
- Partridge, S.; Balayla, J.; Holcroft, C.A.; Abenhaim, H.A. Inadequate Prenatal Care Utilization and Risks of Infant Mortality and Poor Birth Outcome: A Retrospective Analysis of 28,729,765 U.S. Deliveries over 8 Years. Am. J. Perinatol. 2012, 29, 787–794. [Google Scholar] [CrossRef]
- Huddleston, T.; Bilgili, O.; Joki, A.L.; Vankova, Z. Migrant Integration Policy Index 2015: MIPEX 2015. Barcelona; CIDOB Migration Policy Group: Brussels, Belgium, 2015; Available online: http://www.mipex.eu/sites/default/files/downloads/pdf/files/custom/a4/2019.08.21-11.25.18-mipex-2015-custom-book-a4.pdf (accessed on 29 July 2020).
| Nonmigrants (n = 4523) | Migrants with French or European Nationality (n = 1555) | Other Legal Migrants (n = 2806) | Undocumented Migrants (n = 715) | p **** | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Age (years) (n = 9599) | <0.001 | ||||||||
| <20 | 76 | 1.7 | 13 | 0.8 | 26 | 0.9 | 13 | 1.8 | |
| [20,21,22,23,24,25] | 606 | 13.4 | 188 | 12.1 | 375 | 13.4 | 134 | 18.7 | |
| [25,26,27,28,29,30] | 1428 | 31.6 | 362 | 23.3 | 871 | 31.0 | 251 | 35.1 | |
| [30,31,32,33,34,35,36,37,38,39,40] | 2255 | 49.9 | 864 | 55.6 | 1379 | 49.1 | 295 | 41.3 | |
| ≥40 | 158 | 3.5 | 128 | 8.2 | 155 | 5.5 | 22 | 3.1 | |
| Social isolation (n = 9596) | 77 | 1.7 | 55 | 3.5 | 172 | 6.1 | 123 | 17.2 | <0.001 |
| Poor or insecure housing conditions (n = 9596) | 412 | 9.1 | 175 | 11.3 | 510 | 18.2 | 406 | 56.8 | <0.001 |
| No standard healthcare insurance (n = 9585) | 396 | 8.8 | 276 | 17.7 | 833 | 29.7 | 639 | 89.4 | <0.001 |
| No work-related household income (n = 9593) | 435 | 9.6 | 194 | 12.5 | 520 | 18.5 | 335 | 46.9 | <0.001 |
| Deprivation index * (n = 9502) | <0.001 | ||||||||
| 0 criterion | 3661 | 80.9 | 1087 | 69.9 | 1574 | 56.1 | 0 | 0.0 | |
| 1 criterion | 515 | 11.4 | 293 | 18.8 | 667 | 23.8 | 206 | 28.8 | |
| 2 criteria | 240 | 5.3 | 117 | 7.5 | 337 | 12.0 | 145 | 20.3 | |
| 3 or 4 criteria | 103 | 2.3 | 55 | 3.5 | 216 | 7.7 | 286 | 40.0 | |
| Schooling level (n = 9504) | <0.001 | ||||||||
| ≤Primary school | 32 | 0.7 | 88 | 5.7 | 391 | 13.9 | 156 | 21.8 | |
| Middle school | 643 | 14.2 | 297 | 19.1 | 633 | 22.6 | 173 | 24.2 | |
| High school | 892 | 19.7 | 419 | 26.9 | 793 | 28.3 | 195 | 27.3 | |
| University | 2943 | 65.1 | 736 | 47.3 | 943 | 33.6 | 170 | 23.8 | |
| Social welfare coverage at inclusion (n = 9513) | <0.001 | ||||||||
| Standard health insurance (SHI) | 429 | 9.5 | 264 | 17.0 | 675 | 24.1 | 0 | 0.0 | |
| SHI + Complementary health insurance | 3695 | 81.7 | 1013 | 65.1 | 1293 | 46.1 | 0 | 0.0 | |
| Universal health coverage (CMU) | 366 | 8.1 | 218 | 14.0 | 607 | 21.6 | 0 | 0.0 | |
| State medical assistance (AME) | 1 | 0.0 | 22 | 1.4 | 90 | 3.2 | 473 | 66.2 | |
| No healthcare insurance | 29 | 0.6 | 36 | 2.3 | 136 | 4.8 | 166 | 23.2 | |
| Maternal birthplace (n = 9583) | <0.001 | ||||||||
| Metropolitan France | 4357 | 96.3 | 0 | 0.0 | 0 | 0.0 | 6 | 0.8 | |
| Overseas French territory | 166 | 3.7 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |
| Europe (other) | 0 | 0.0 | 339 | 21.8 | 77 | 2.7 | 51 | 7.1 | |
| North Africa | 0 | 0.0 | 611 | 39.3 | 1314 | 46.8 | 191 | 26.7 | |
| Sub-Saharan Africa | 0 | 0.0 | 381 | 24.5 | 877 | 31.3 | 308 | 43.1 | |
| Asia–Middle East | 0 | 0.0 | 128 | 8.8 | 379 | 13.6 | 109 | 15.2 | |
| Other | 0 | 0.0 | 86 | 5.5 | 159 | 5.7 | 50 | 7.0 | |
| Length of residency (median in months) ** (n = 8687) IQR 25/75 | 141.4 82.7 | 250.6 | 71.9 26.0 | 118.8 | 31.6 9.4 | 73.4 | <0.001 | ||
| Language barrier (n = 9322) | 41 | 0.9 | 150 | 9.6 | 575 | 20.5 | 241 | 33.7 | <0.001 |
| Smoked before pregnancy (n = 9507) | 1237 | 27.3 | 206 | 13.2 | 138 | 4.9 | 45 | 6.3 | <0.001 |
| Smoked during pregnancy (n = 9455) | 644 | 14.2 | 113 | 7.3 | 66 | 2.4 | 21 | 2.9 | <0.001 |
| Alcohol during pregnancy (n = 9471) | 372 | 8.2 | 96 | 6.2 | 134 | 4.8 | 61 | 8.5 | <0.001 |
| Drugs during pregnancy (n = 9594) | 39 | 0.9 | 5 | 0.3 | 6 | 0.2 | 1 | 0.1 | <0.001 |
| Prepregnancy BMI (kg/m2) (n = 9599) | <0.001 | ||||||||
| <18.5 | 303 | 6.7 | 76 | 4.9 | 122 | 4.3 | 46 | 6.4 | |
| 18.5–24.9 | 2844 | 62.9 | 864 | 55.6 | 1361 | 48.5 | 318 | 44.5 | |
| 25–29.9 | 767 | 17.0 | 366 | 23.5 | 733 | 26.1 | 167 | 23.4 | |
| ≥30 | 505 | 11.2 | 187 | 12.0 | 376 | 13.4 | 80 | 11.2 | |
| Nulliparous (n = 9587) High risk at the beginning of pregnancy *** (n = 9550) | 2302 925 | 50.9 20.5 | 520 297 | 33.4 19.1 | 963 521 | 34.3 18.6 | 332 124 | 46.4 17.3 | <0.001 0.1 |
| Nonmigrants (n = 4523) | Migrants with French or European Nationality (n = 1555) | Other Legal Migrants (n = 2806) | Undocumented Migrants (n = 715) | p *** | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Initiation of care ≥14 GW (n = 9586) | 641 | 14.2 | 238 | 15.3 | 524 | 18.7 | 214 | 29.9 | <0.001 |
| Percentage of recommended prenatal visits <50% * (n = 9566) | 118 | 2.6 | 35 | 2.3 | 85 | 3.0 | 43 | 6.0 | <0.001 |
| First trimester ultrasound not performed between 11 and 14 GW (n = 9256) | 781 | 17.3 | 349 | 22.4 | 857 | 30.5 | 304 | 42.5 | <0.001 |
| Second trimester ultrasound not performed between 21 and 24 GW (n = 9391) | 689 | 15.2 | 312 | 20.1 | 606 | 21.6 | 204 | 28.5 | <0.001 |
| Third trimester ultrasound not performed between 31 and 34 GW (n = 9433) | 753 | 16.6 | 278 | 17.9 | 584 | 20.8 | 160 | 22.4 | <0.001 |
| Inadequate prenatal care according to mAPNCU index ** | 1196 | 26.4 | 491 | 31.6 | 1131 | 40.3 | 372 | 52.0 | <0.001 |
| Missing data for an item of the index | 307 | 6.8 | 121 | 7.8 | 171 | 6.1 | 43 | 6.0 | |
| Indirect indicators of prenatal care | |||||||||
| Pre-anesthesia evaluation ≥37 GW (n = 9061) | 438 | 9.7 | 160 | 10.3 | 347 | 12.4 | 91 | 12.7 | 0.001 |
| No determination of Rhesus group before entering the delivery room (n = 9531) | 23 | 0.5 | 7 | 0.5 | 15 | 0.5 | 4 | 0.6 | 0.9 |
| No hepatitis B serology determination before entering the delivery room (n = 9550) | 33 | 0.7 | 6 | 0.4 | 15 | 0.5 | 3 | 0.4 | 0.4 |
| No predelivery identification of estimated fetal weight >95th percentile (among 479 women with birth weight >95th percentile, n = 9506) | 71 | 39.0 | 32 | 32.7 | 65 | 38.0 | 13 | 46.4 | 0.6 |
| No predelivery identification of estimated fetal weight <3rd percentile (among 343 women with birth weight <3rd percentile, n = 9439) | 58 | 34.9 | 25 | 44.6 | 41 | 50.0 | 8 | 20.5 | 0.007 |
| No predelivery identification of placenta previa (among 124 women with placenta previa, n = 9422) | 5 | 9.1 | 3 | 15.0 | 3 | 8.6 | 0 | 0 | 0.5 |
| No predelivery identification of multiple pregnancy (among 141 women with multiple pregnancy, n = 9547) | 13 | 19.4 | 0 | 0 | 6 | 14.3 | 1 | 12.5 | 0.1 |
| No predelivery identification of uterine scar (among 1311 women with a uterine scar, n = 9520) | 27 | 5.7 | 14 | 5.6 | 25 | 5.3 | 8 | 7.2 | 0.9 |
| No predelivery identification of breech presentation (among 392 women with breech delivery, n = 9511) | 22 | 10.9 | 5 | 9.4 | 11 | 10.4 | 2 | 6.5 | 0.9 |
| Inadequate Prenatal Care * | ||
|---|---|---|
| OR [95% CI] | aOR [95% CI] 1 | |
| Nonmigrants (n = 4523) | 1 | 1 |
| Migrants with French or European nationality (n = 1555) | 1.31 [1.16–1.49] | 1.17 [1.03–1.33] |
| Legal migrants (n = 2806) | 1.90 [1.71–2.10] | 1.60 [1.43–1.78] |
| Undocumented migrants (n = 715) | 3.13 [2.65–3.70] | 2.58 [2.16–3.07] |
| Inadequate Prenatal Care * | ||
|---|---|---|
| OR [95% CI] | aOR [95% CI] 1 | |
| Nonmigrants (n = 4523) | 1 | 1 |
| Migrants with French or European nationality not born in SSA (n = 1174) | 1.25 [1.09–1.44] | 1.15 [0.99–1.34] |
| Migrants with French or European nationality born in SSA (n = 381) | 1.52 [1.21–1.91] | 1.22 [0.97–1.55] |
| Other legal migrants not born in SSA (n = 1929) | 1.73 [1.54–1.94] | 1.54 [1.37–1.75] |
| Other legal migrants born in SSA (n = 877) | 2.35 [2.02– 2.73] | 1.80 [1.52–2.12] |
| Undocumented migrants not born in SSA (n = 407) | 2.75 [2.22–3.40] | 2.37 [1.89–2.97] |
| Undocumented migrants born in SSA (n = 308) | 3.72 [2.92–4.75] | 2.95 [2.28–3.82] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eslier, M.; Deneux-Tharaux, C.; Sauvegrain, P.; Schmitz, T.; Luton, D.; Mandelbrot, L.; Estellat, C.; Azria, E. Association between Migrant Women’s Legal Status and Prenatal Care Utilization in the PreCARE Cohort. Int. J. Environ. Res. Public Health 2020, 17, 7174. https://doi.org/10.3390/ijerph17197174
Eslier M, Deneux-Tharaux C, Sauvegrain P, Schmitz T, Luton D, Mandelbrot L, Estellat C, Azria E. Association between Migrant Women’s Legal Status and Prenatal Care Utilization in the PreCARE Cohort. International Journal of Environmental Research and Public Health. 2020; 17(19):7174. https://doi.org/10.3390/ijerph17197174
Chicago/Turabian StyleEslier, Maxime, Catherine Deneux-Tharaux, Priscille Sauvegrain, Thomas Schmitz, Dominique Luton, Laurent Mandelbrot, Candice Estellat, and Elie Azria. 2020. "Association between Migrant Women’s Legal Status and Prenatal Care Utilization in the PreCARE Cohort" International Journal of Environmental Research and Public Health 17, no. 19: 7174. https://doi.org/10.3390/ijerph17197174
APA StyleEslier, M., Deneux-Tharaux, C., Sauvegrain, P., Schmitz, T., Luton, D., Mandelbrot, L., Estellat, C., & Azria, E. (2020). Association between Migrant Women’s Legal Status and Prenatal Care Utilization in the PreCARE Cohort. International Journal of Environmental Research and Public Health, 17(19), 7174. https://doi.org/10.3390/ijerph17197174





