The Effects of Circadian Rhythm Disruption on Mental Health and Physiological Responses among Shift Workers and General Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Measures
2.3.1. Polysomnography
2.3.2. Abbreviated Profile of Mood States
2.3.3. General Health Questionnaire-28 (GHQ-28)
2.3.4. Working Memory and Processing Speed Indexes of the Wechsler Adult Intelligent Scale (WAIS-IV)
2.3.5. Blood Test
2.4. Experimental Procedure
2.4.1. Normal Condition
2.4.2. Disrupted Condition
2.4.3. General Population
2.4.4. Shift Worker
2.5. Statistical Analysis
3. Result
3.1. The Relationship between Circadian Rhythm and Mental Health (Mood, Psychological Wellbeing, Working Memory, and Processing Speed)
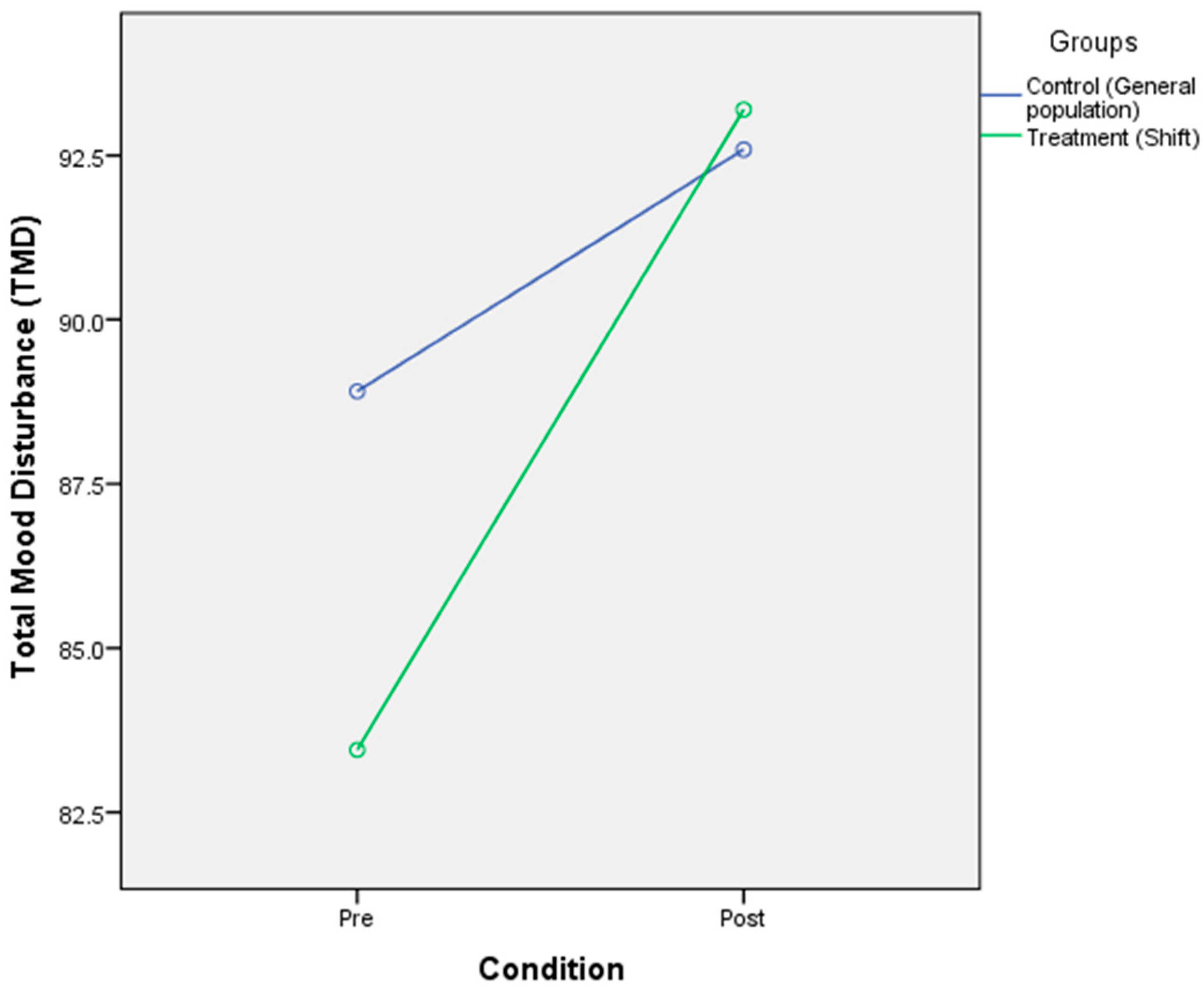
3.2. The Effect of Circadian Rhythm Disruption on Mood
3.3. The Effect of Circadian Rhythm Disruption on Psychological Wellbeing
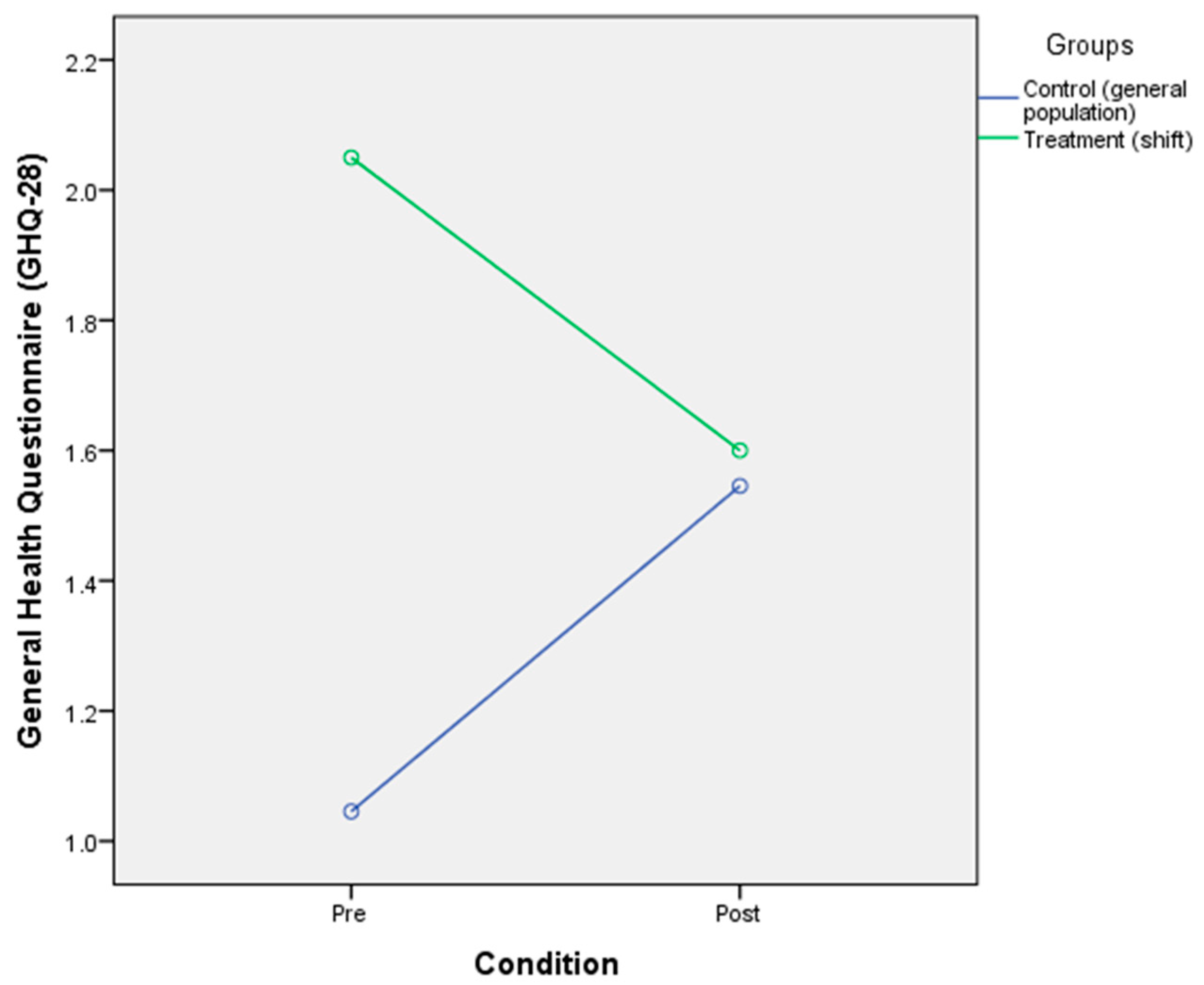
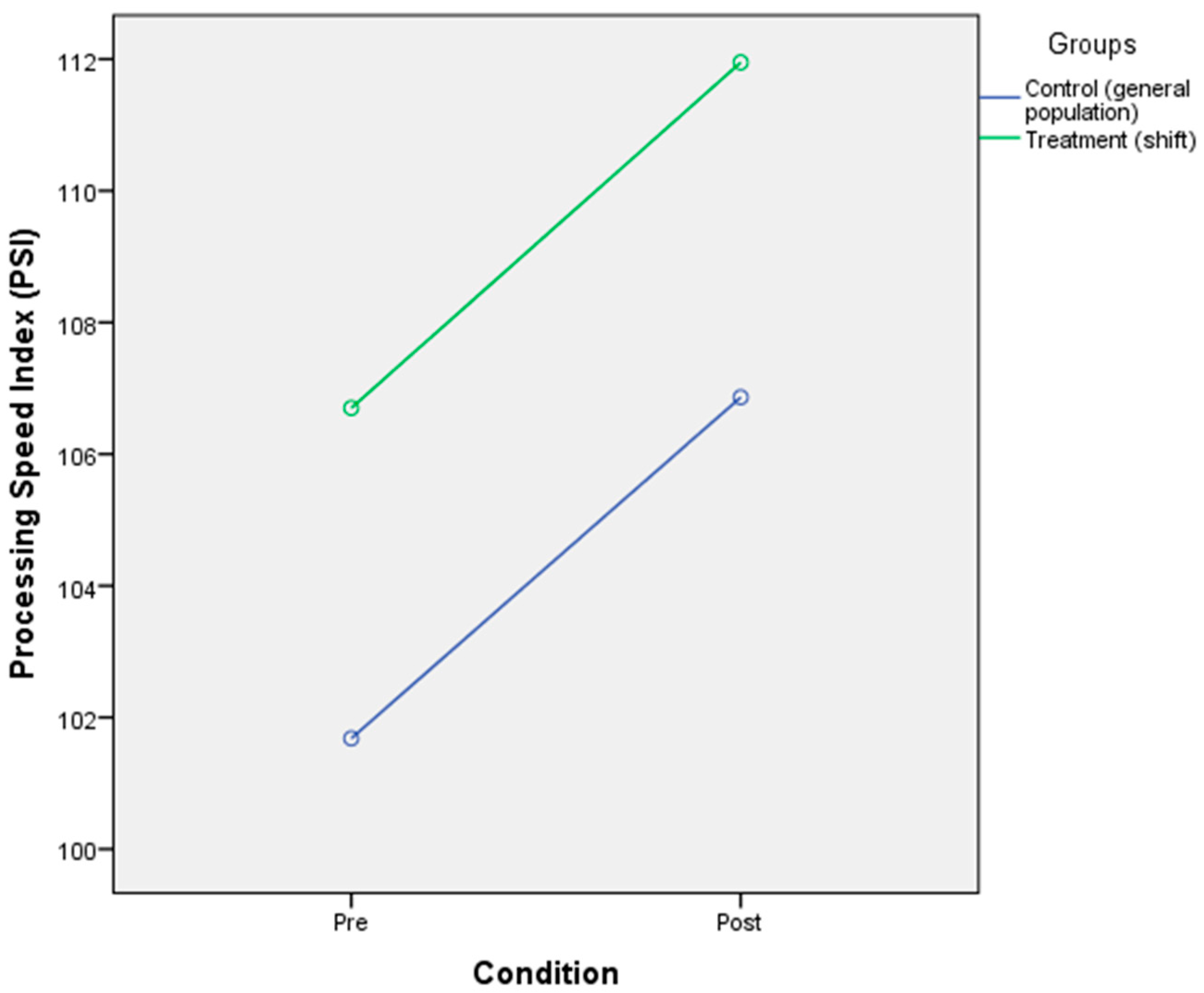
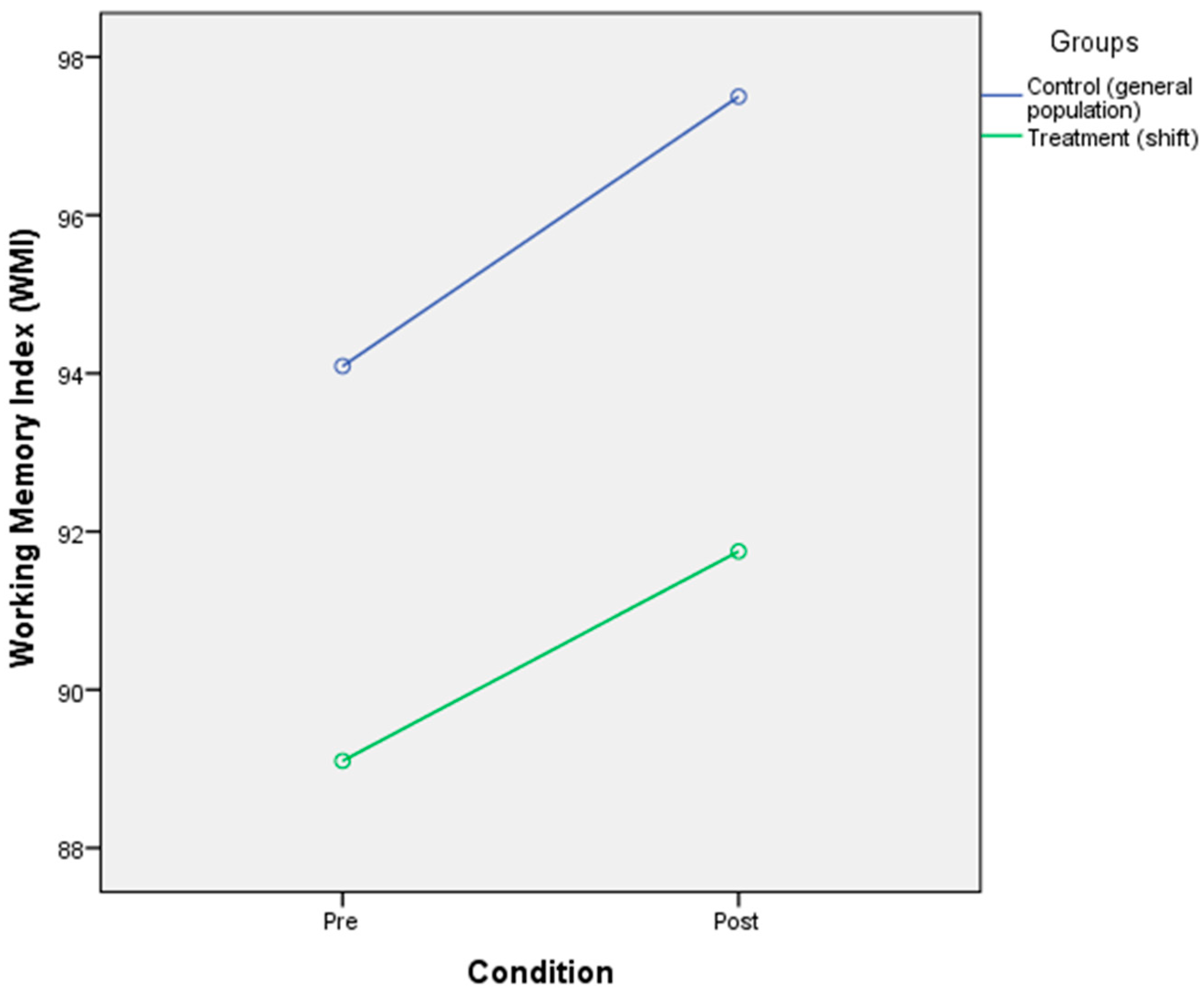
3.4. The Effect of Circadian Rhythm Disruption on Cognitive Performance (Processing Speed and Working Memory)
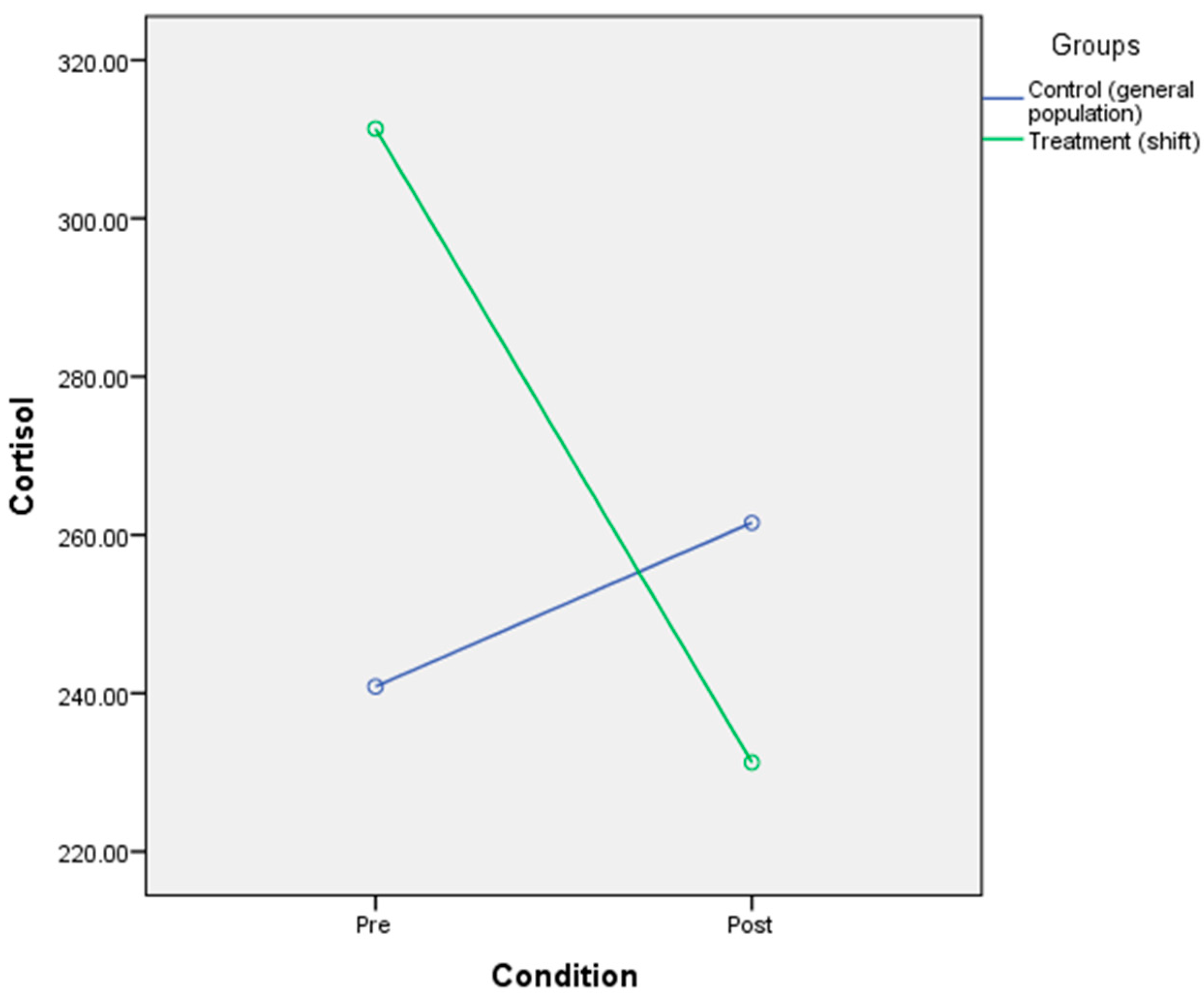
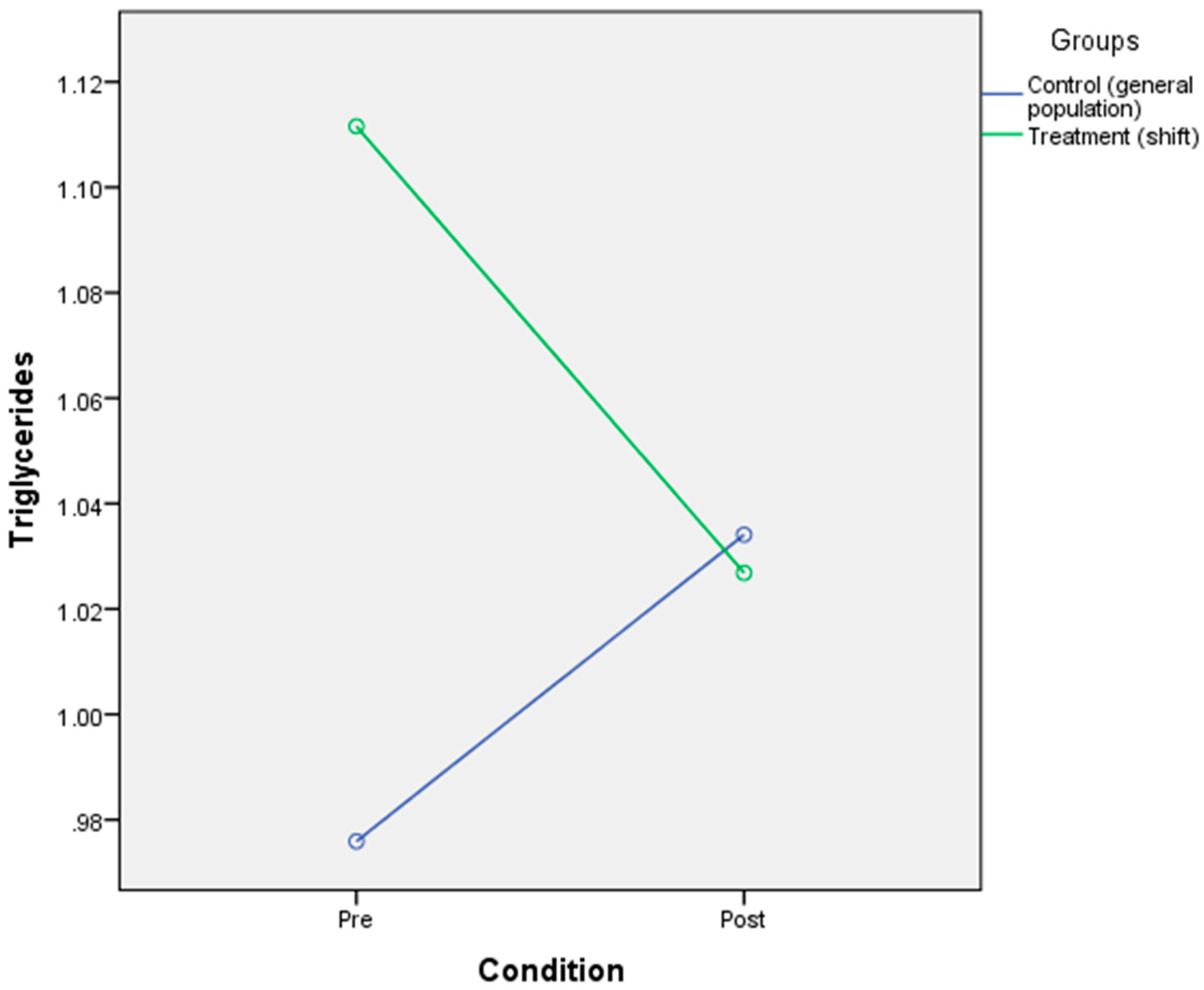
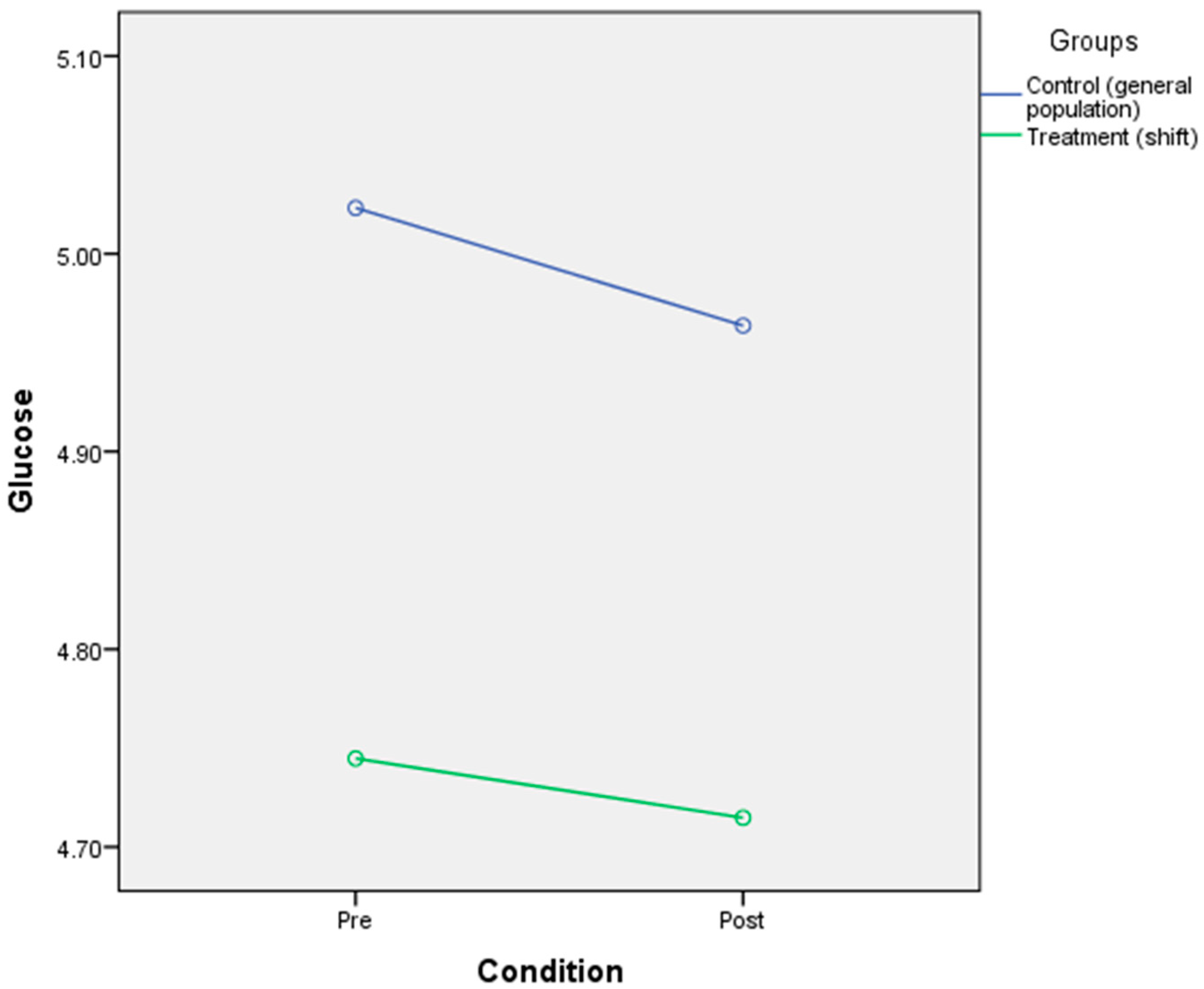
3.5. The Effect of Circadian Rhythm Disruption on Physiological Responses (Glucose, Triglycerides, Cortisol)
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Shanmugam, V.; Wafi, A.; Al-Taweel, N.; Büsselberg, D. Disruption of circadian rhythm increases the risk of cancer, metabolic syndrome and cardiovascular disease. J. Local Glob. Health Sci. 2013, 3. [Google Scholar] [CrossRef]
- Walker, M. Why We Sleep: The New Science of Sleep and Dreams; Penguin: Westminster, UK, 2017. [Google Scholar]
- McClung, C.R. CIRCADIAN RHYTHMS: Linking the Loops. Science 2009, 323, 1440–1441. [Google Scholar] [CrossRef]
- Zheng, G.; Li, K.; Bu, W.; Wang, Y. The Effects of Indoor High Temperature on Circadian Rhythms of Human Work Efficiency. Int. J. Environ. Res. Public Health 2019, 16, 759. [Google Scholar] [CrossRef]
- Salgado-Delgado, R.; Osorio, A.T.; Saderi, N.; Escobar, C. Disruption of Circadian Rhythms: A Crucial Factor in the Etiology of Depression. Depression Res. Treat. 2011, 2011, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Foster, R.G.; Peirson, S.N.; Wulff, K.; Winnebeck, E.C.; Vetter, C.; Roenneberg, T. Sleep and Circadian Rhythm Disruption in Social Jetlag and Mental Illness. Prog. Mol. Biol. Transl. Sci. 2013, 119, 325–346. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.W.; Jeong, J.-H.; Hong, S.-C. The Impact of Sleep and Circadian Disturbance on Hormones and Metabolism. Int. J. Endocrinol. 2015, 2015, 1–9. [Google Scholar] [CrossRef]
- Saghir, Z.; Syeda, J.N.; Muhammad, A.S.; Abdalla, T.H.B. The Amygdala, Sleep Debt, Sleep Deprivation, and the Emotion of Anger: A Possible Connection? Cureus 2018, 10, 2912. [Google Scholar] [CrossRef]
- Wichniak, A.; Wierzbicka, A.; Jernajczyk, W. Sleep as a biomarker for depression. Int. Rev. Psychiatry 2013, 25, 632–645. [Google Scholar] [CrossRef]
- Iber, C.; Ancoli-Israel, S.; Chesson, A.L.; Quan, S.F. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology, and Technical Specifications; American Academy of Sleep Medicine: Westchester, IL, USA, 2007. [Google Scholar]
- Karatsoreos, I.N. Links between Circadian Rhythms and Psychiatric Disease. Front. Behav. Neurosci. 2014, 8, 162. [Google Scholar] [CrossRef]
- Bechtel, W. Circadian Rhythms and Mood Disorders: Are the Phenomena and Mechanisms Causally Related? Front. Psychiatry 2015, 6, 118. [Google Scholar] [CrossRef]
- Qian, J.; Scheer, F.A.J.L. Circadian System and Glucose Metabolism: Implications for Physiology and Disease. Trends Endocrinol. Metab. 2016, 27, 282–293. [Google Scholar] [CrossRef]
- Martinez, D.; Lenz, M.D.C.S.; Menna-Barreto, L. Diagnóstico dos transtornos do sono relacionados ao ritmo circadiano. J. Bras. Pneumol. 2008, 34, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Rüger, M.; Scheer, F.A.J.L. Effects of circadian disruption on the cardiometabolic system. Rev. Endocr. Metab. Disord. 2009, 10, 245–260. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Duan, P.; Yao, L.; Hou, H. Shiftwork-Mediated Disruptions of Circadian Rhythms and Sleep Homeostasis Cause Serious Health Problems. Int. J. Genom. 2018, 2018, 1–11. [Google Scholar] [CrossRef]
- Waterhouse, J. Circadian Rhythms and Cognition; Elsevier BV: Amsterdam, The Netherlands, 2010; Volume 185, pp. 131–153. [Google Scholar]
- Kolbe, I.; Dumbell, R.; Oster, H. Circadian Clocks and the Interaction between Stress Axis and Adipose Function. Int. J. Endocrinol. 2015, 2015, 1–13. [Google Scholar] [CrossRef]
- World Medical Association. Recommendations Guiding Physicians in Biomedical Research Involving Human Subjects (Declaration of Helsinki), 18th World Medical Assembly, Helsinki, Finland. June 1964. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 1 November 2018).
- Grove, R.; Prapavessis, H. Preliminary evidence for the reliability and validity of an abbreviated Profile of Mood States. Int. J. Sport Psychol. 1992, 23, 93–109. [Google Scholar]
- Goldberg, D. Manual of the General Health Questionnaire; NFER Publishing: Windsor, UK, 1978. [Google Scholar]
- Werneke, U.; Goldberg, D.P.; Yalcin, I.; Üstün, B.T. The stability of the factor structure of the General Health Questionnaire. Psychol. Med. 2000, 30, 823–829. [Google Scholar] [CrossRef]
- Jackson, C. The General Health Questionnaire. Occup. Med. 2006, 57, 79. [Google Scholar] [CrossRef]
- Taghavi, M.R. Validity and reliability of the General Health Questionnaire (GHQ-28) in college students of Shiraz University. J. Psychol. Interdiscip. Appl. 2002, 5, 381–398. [Google Scholar]
- Wechsler, D. Wechsler Adult Intelligence Scale, 4th ed.; Pearson: San Antonio, CA, USA, 2008. [Google Scholar]
- Yoo, S.-S.; Gujar, N.; Hu, P.; Jolesz, F.A.; Walker, M.P. The human emotional brain without sleep—a prefrontal amygdala disconnect. Curr. Biol. 2007, 17, R877–R878. [Google Scholar] [CrossRef] [PubMed]
- Kaida, K.; Niki, K. Total sleep deprivation decreases flow experience and mood status. Neuropsychiatr. Dis. Treat. 2013, 10, 19–25. [Google Scholar] [CrossRef]
- Babson, K.A.; Trainor, C.D.; Feldner, M.T.; Blumenthal, H. A test of the effects of acute sleep deprivation on general and specific self-reported anxiety and depressive symptoms: An experimental extension. J. Behav. Ther. Exp. Psychiatry 2010, 41, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Zohar, D.; Tzischinsky, O.; Epstein, R.; Lavie, P. The Effects of Sleep Loss on Medical Residents’ Emotional Reactions to Work Events: A Cognitive-Energy Model. Sleep 2005, 28, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Eastman, C.I.; Suh, C.; Tomaka, V.A.; Crowley, S.J. Circadian rhythm phase shifts and endogenous free-running circadian period differ between African-Americans and European-Americans. Sci. Rep. 2015, 5, 8381. [Google Scholar] [CrossRef]
- Takahashi, M.; Tahara, Y.; Tsubosaka, M.; Fukazawa, M.; Ozaki, M.; Iwakami, T.; Nakaoka, T.; Shibata, S. Chronotype and social jetlag influence human circadian clock gene expression. Sci. Rep. 2018, 8, 10152. [Google Scholar] [CrossRef]
- Watson, S.; Mackin, P. HPA axis function in mood disorders. Psychiatry 2009, 8, 97–101. [Google Scholar] [CrossRef]
- McClung, C.A. How might circadian rhythms control mood? Let me count the ways. Biol. Psychiatry 2013, 74, 242–249. [Google Scholar] [CrossRef]
- Kudielka, B.M.; Buchtal, J.; Uhde, A.; Wüst, S. Circadian cortisol profiles and psychological self-reports in shift workers with and without recent change in the shift rotation system. Biol. Psychol. 2007, 74, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Haus, E.; Smolensky, M. Biological Clocks and Shift Work: Circadian Dysregulation and Potential Long-term Effects. Cancer Causes Control 2006, 17, 489–500. [Google Scholar] [CrossRef]
- Ahasan, R.; Lewko, J.; Campbell, D.; Salmoni, A. Adaptation to Night Shifts and Synchronisation Processes of Night Workers. J. Physiol. Anthropol. Appl. Hum. Sci. 2001, 20, 215–226. [Google Scholar] [CrossRef]
- Ghiasvand, M.; Heshmat, R.; Golpira, R.; Haghpanah, V.; Soleimani, A.; Shoushtarizadeh, P.; Tavangar, S.M.; Larijani, B. Shift working and risk of lipid disorders: A cross-sectional study. Lipids Health Dis. 2006, 5, 9. [Google Scholar] [CrossRef] [PubMed]
- Van Amelsvoort, L.; Jansen, N.W.H.; Swaen, G.M.H.; Brandt, P.A.V.D.; Kant, I. Direction of shift rotation among three-shift workers in relation to psychological health and work-family conflict. Scand. J. Work Environ. Health 2004, 30, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Regestein, Q.; Natarajan, V.; Pavlova, M.; Kawasaki, S.; Gleason, R.; Koff, E. Sleep debt and depression in female college students. Psychiatry Res. Neuroimaging 2010, 176, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Fonken, L.K.; Workman, J.L.; Walton, J.C.; Weil, Z.M.; Morris, J.S.; Haim, A.; Nelson, R.J. Light at night increases body mass by shifting the time of food intake. Proc. Natl. Acad. Sci. USA 2010, 107, 18664–18669. [Google Scholar] [CrossRef]

| Demography | General Population (n = 22) | Shift Worker (n = 20) | ||
|---|---|---|---|---|
| Frequency (Percentage) | Mean ± SD | Frequency (Percentage) | Mean ± SD | |
| Sex | ||||
| Male | 5 (22.7%) | 5(25%) | ||
| Female | 17(77.3%) | 15 (75%) | ||
| Marital status | ||||
| Single | 9(41%) | 7(35%) | ||
| Married | 13(59%) | 13(65%) | ||
| Age | ||||
| 20 to 29 | 7(31.8%) | 8(40%) | ||
| 30 to 39 | 11(50%) | 32.82 ± 5.85 | 3(15%) | 34.40 ± 7.10 |
| 40 to 49 | 4(18.2%) | 9(45%) | ||
| Body Mass Index (BMI) | ||||
| 18.0 to 21.9 | 9(41%) | 8(40%) | ||
| 22.0 to 25.9 | 11(50%) | 22.75 ± 2.34 | 9(45%) | 22.99 ± 2.82 |
| 26.0 to 29.9 | 2(9%) | 3(15%) | ||
| Working Experience | ||||
| 1 to 5 years | 8(36.4%) | 8(40%) | ||
| 6 to 10 years | 6(27.3%) | 6(30%) | ||
| 11 to 15 years | 3(13.6%) | 9.45 ± 6.05 | 3(15%) | 8.30 ± 5.43 |
| 16 to 20 years | 4(18.2%) | 3(15%) | ||
| 21 to 25 years | 1(4.5%) | 0 | ||
| Parameter | General Population | Shift Worker | ||
|---|---|---|---|---|
| Mean ± SD (Pre) | Mean ± SD (Post) | Mean ± SD (Pre) | Mean ± SD (Post) | |
| Mood | 88.91 ± 17.87 | 92.59 ± 12.69 | 83.45 ± 21.56 | 93.20 ± 23.30 |
| Psychological wellbeing | 1.05 ± 1.68 | 1.55 ± 2.24 | 2.05 ± 2.54 | 1.60 ± 2.14 |
| Working memory | 94.09 ± 97.50 | 97.50 ± 15.36 | 89.10 ± 11.90 | 91.75 ± 12.75 |
| Processing speed | 101.68 ± 9.46 | 106.85 ± 13.29 | 106.70 ± 11.99 | 111.95 ± 15.98 |
| Parameter | General Population | Shift Worker | ||
|---|---|---|---|---|
| Mean ± SD (Pre) | Mean ± SD (Post) | Mean ± SD (Pre) | Mean ± SD (Post) | |
| Cortisol | 240.85 ± 64.24 | 261.54 ± 81.73 | 311.33 ± 108.66 | 231.25 ± 135.17 |
| Triglycerides | 0.98 ± 0.67 | 1.03 ± 0.60 | 1.11 ± 0.54 | 1.02 ± 0.70 |
| Glucose | 5.02 ± 0.42 | 4.96 ± 0.43 | 4.74 ± 0.68 | 4.71 ± 0.55 |
| Sleep Quality Profile | Pre-Test % (n) | Post-Test % (n) | |
|---|---|---|---|
| Sleep quality | Good sleep | 90.1% (20) | 40.9% (9) |
| Poor sleep | 9.9% (2) | 59.1% (13) | |
| Research Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Circadian rhythm disruption | ||||||||
| 2 | Mood | 0.305 * | |||||||
| 3 | Psychological wellbeing | 0.028 | −0.042 | ||||||
| 4 | Working Memory | −0.114 | −0.178 | 0.026 | |||||
| 5 | Processing Speed | −0.167 | −0.005 | 0.026 | 0.034 | ||||
| 6 | Glucose | 0.091 | −0.183 | −0.238 | 0.049 | −0.219 * | |||
| 7 | Triglycerides | −0.046 | −0.098 | −0.162 | 0.118 | −0.088 | 0.212 | ||
| 8 | Cortisol | 0.074 | 0.263 * | −0.183 | −0.078 | 0.097 | 0.089 | −0.116 | |
| Parameter | General Population | Shift Worker | p Value | p Value | ||
|---|---|---|---|---|---|---|
| Mean ± SD (Pre) | Mean ± SD (Post) | Mean ± SD (Pre) | Mean ± SD (Post) | (Within) | (Between) | |
| Mood | 88.91 ± 17.87 | 92.59 ± 12.69 | 83.45 ± 21.56 | 93.20 ± 23.30 | 0.005 ** | 0.659 |
| Psychological wellbeing | 1.05 ± 1.68 | 1.55 ± 2.24 | 2.05 ± 2.54 | 1.60 ± 2.14 | 0.942 | 0.363 |
| Working memory | 94.09 ± 11.01 | 97.50 ± 15.36 | 89.10 ± 11.90 | 91.75 ± 12.75 | 0.032 * | 0.159 |
| Processing speed | 101.68 ± 9.46 | 106.85 ± 13.29 | 106.70 ± 11.99 | 111.95 ± 15.98 | 0.004 ** | 0.165 |
| Cortisol | 240.85 ± 64.24 | 261.54 ± 81.73 | 311.33 ± 108.66 | 231.25 ± 135.17 | 0.182 | 0.557 |
| Triglycerides | 0.98 ± 0.67 | 1.03 ± 0.60 | 1.11 ± 0.54 | 1.02 ± 0.70 | 0.852 | 0.729 |
| Glucose | 5.02 ± 0.42 | 4.96 ± 0.43 | 4.74 ± 0.68 | 4.71 ± 0.55 | 0.592 | 0.069 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmad, M.; Md. Din, N.S.B.; Tharumalay, R.D.; Che Din, N.; Ibrahim, N.; Amit, N.; Farah, N.M.; Osman, R.A.; Abdul Hamid, M.F.; Ibrahim, I.A.; et al. The Effects of Circadian Rhythm Disruption on Mental Health and Physiological Responses among Shift Workers and General Population. Int. J. Environ. Res. Public Health 2020, 17, 7156. https://doi.org/10.3390/ijerph17197156
Ahmad M, Md. Din NSB, Tharumalay RD, Che Din N, Ibrahim N, Amit N, Farah NM, Osman RA, Abdul Hamid MF, Ibrahim IA, et al. The Effects of Circadian Rhythm Disruption on Mental Health and Physiological Responses among Shift Workers and General Population. International Journal of Environmental Research and Public Health. 2020; 17(19):7156. https://doi.org/10.3390/ijerph17197156
Chicago/Turabian StyleAhmad, Mahadir, Nur Syafiqa Balqis Md. Din, Ruthra Devi Tharumalay, Normah Che Din, Norhayati Ibrahim, Noh Amit, Nor MF Farah, Rose Azzlinda Osman, Mohamed Faisal Abdul Hamid, Ibnor Azli Ibrahim, and et al. 2020. "The Effects of Circadian Rhythm Disruption on Mental Health and Physiological Responses among Shift Workers and General Population" International Journal of Environmental Research and Public Health 17, no. 19: 7156. https://doi.org/10.3390/ijerph17197156
APA StyleAhmad, M., Md. Din, N. S. B., Tharumalay, R. D., Che Din, N., Ibrahim, N., Amit, N., Farah, N. M., Osman, R. A., Abdul Hamid, M. F., Ibrahim, I. A., Jamsari, E. A., Palil, M. R., & Ahmad, S. (2020). The Effects of Circadian Rhythm Disruption on Mental Health and Physiological Responses among Shift Workers and General Population. International Journal of Environmental Research and Public Health, 17(19), 7156. https://doi.org/10.3390/ijerph17197156







