Psychometric Properties of the Persian Pittsburgh Sleep Quality Index for Adolescents
Abstract
1. Introduction
2. Methods
2.1. Study Procedure
2.2. Sample
2.3. Tools
2.3.1. Sociodemographic Information
2.3.2. Pittsburgh Sleep Quality Index
2.3.3. Adolescent Sleep Hygiene Scale
2.4. Statistical Analysis
3. Results
3.1. Overview of the Dimensions of the Pittsburgh Sleep Quality Index (PSQI)
3.2. Correlations between Dimensions of the PSQI with Dimensions from the Adolescent Sleep Hygiene Scale (ASHS)
3.3. Dimensions of the Adolescent Sleep Hygiene Scale in Participants with Normal (PSQI 5) and with Poor Sleep (PSQI > 6)
3.4. Factor Analysis of Dimensions of PSQI
3.5. Multiple Regression Analysis to Predict Scores of the Adolescent Sleep Hygiene Scale, Based on the Four Factors of the PSQI
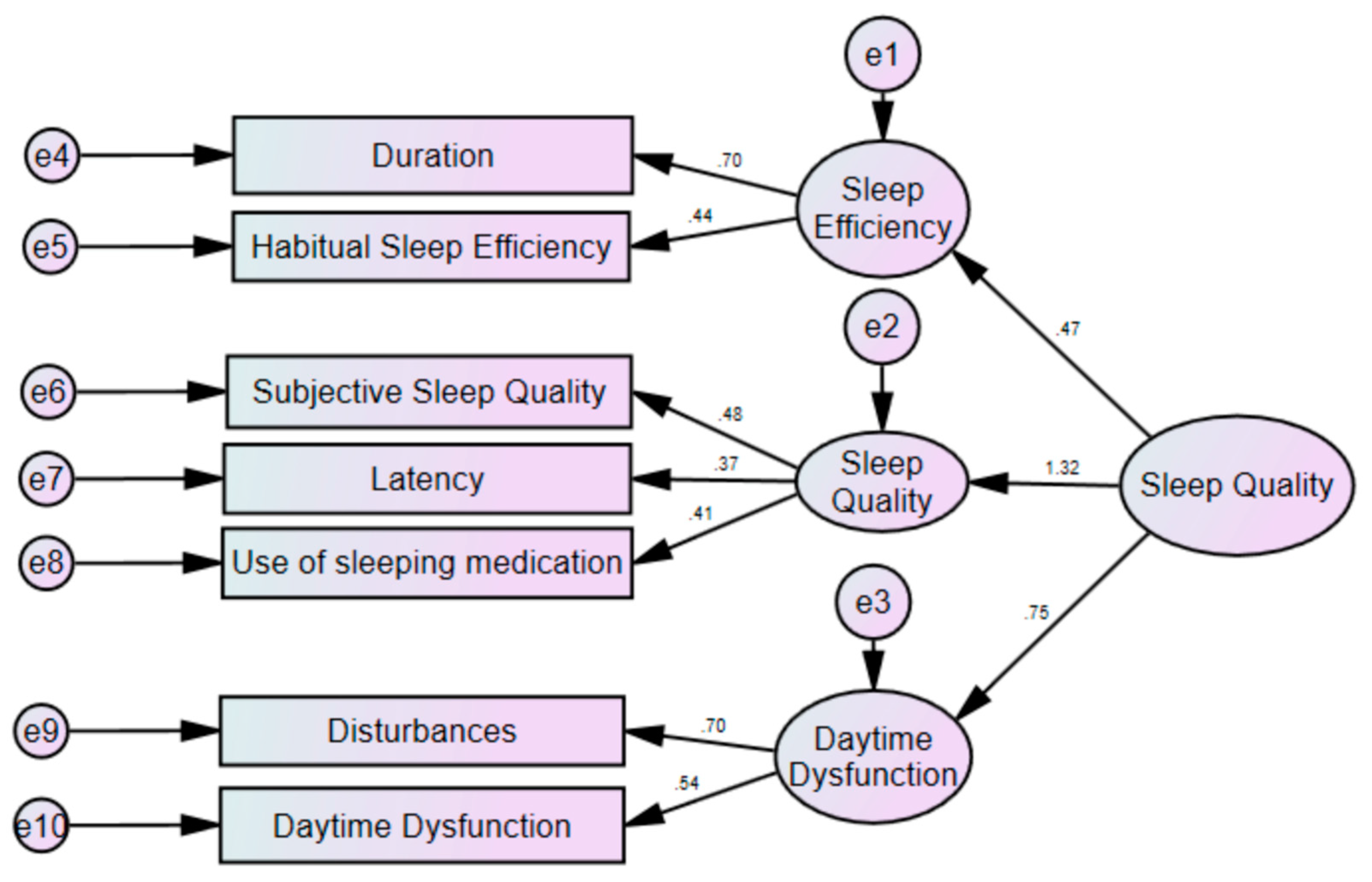
3.6. Model Fit of the PSQI: Results from the Structural Equation Modelling
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Barclay, N.L.; Gregory, A.M. Sleep in childhood and adolescence: Age-specific sleep characteristics, common sleep disturbances and associated difficulties. Curr. Top. Behav. Neurosci. 2014, 16, 337–365. [Google Scholar] [CrossRef] [PubMed]
- Dutil, C.; Walsh, J.J.; Featherstone, R.B.; Gunnell, K.E.; Tremblay, M.S.; Gruber, R.; Weiss, S.K.; Cote, K.A.; Sampson, M.; Chaput, J.-P.; et al. Influence of sleep on developing brain functions and structures in children and adolescents: A systematic review. Sleep Med. Rev. 2018, 42, 184–201. [Google Scholar] [CrossRef] [PubMed]
- Tarokh, L.; Saletin, J.M.; Carskadon, M.A. Sleep in adolescence: Physiology, cognition and mental health. Neurosci. Biobehav. Rev. 2016, 70, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Sivertsen, B.; Skogen, J.C.; Jakobsen, R.; Hysing, M. Sleep and use of alcohol and drug in adolescence. A large population-based study of Norwegian adolescents aged 16 to 19 years. Drug Alcohol Depend. 2015, 149, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Khazaie, H.; Behrouz, B.; Chehri, A.; Gerber, M.; Holsboer-Trachsler, E.; Sadeghi Bahmani, D.; Brand, S. Among adolescents, addiction susceptibility and sleep-related dysfunction have a common cognitive-emotional base and predict poor sleep quantity. J. Subst. Use 2019, 24, 426–431. [Google Scholar] [CrossRef]
- Wong, M.M.; Robertson, G.C.; Dyson, R.B. Prospective relationship between poor sleep and substance-related problems in a national sample of adolescents. Alcohol. Clin. Exp. Res. 2015, 39, 355–362. [Google Scholar] [CrossRef]
- McGlinchey, E.L.; Harvey, A.G. Risk behaviors and negative health outcomes for adolescents with late bedtimes. J. Youth Adolesc. 2015, 44, 478–488. [Google Scholar] [CrossRef]
- Short, M.A.; Weber, N. Sleep duration and risk-taking in adolescents: A systematic review and meta-analysis. Sleep Med. Rev. 2018, 41, 185–196. [Google Scholar] [CrossRef]
- Wong, M.M.; Brower, K.J. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. J. Psychiatr. Res. 2012, 46, 953–959. [Google Scholar] [CrossRef]
- Gangwisch, J.E.; Babiss, L.A.; Malaspina, D.; Turner, J.B.; Zammit, G.K.; Posner, K. Earlier parental set bedtimes as a protective factor against depression and suicidal ideation. Sleep 2010, 33, 97–106. [Google Scholar] [CrossRef]
- Becker, S.P.; Dvorsky, M.R.; Holdaway, A.S.; Luebbe, A.M. Sleep problems and suicidal behaviors in college students. J. Psychiatr. Res. 2018, 99, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Palmer, C.A.; Alfano, C.A. Sleep and emotion regulation: An organizing, integrative review. Sleep Med. Rev. 2017, 31, 6–16. [Google Scholar] [CrossRef] [PubMed]
- De Zambotti, M.; Goldstone, A.; Colrain, I.M.; Baker, F.C. Insomnia disorder in adolescence: Diagnosis, impact, and treatment. Sleep Med. Rev. 2017. [Google Scholar] [CrossRef] [PubMed]
- Chiu, H.Y.; Lee, H.C.; Chen, P.Y.; Lai, Y.F.; Tu, Y.K. Associations between sleep duration and suicidality in adolescents: A systematic review and dose-response meta-analysis. Sleep Med. Rev. 2018, 42, 119–126. [Google Scholar] [CrossRef]
- Mercer, P.W.; Merritt, S.L.; Cowell, J.M. Differences in reported sleep need among adolescents. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 1998, 23, 259–263. [Google Scholar] [CrossRef]
- Kaneita, Y.; Ohida, T.; Osaki, Y.; Tanihata, T.; Minowa, M.; Suzuki, K.; Wada, K.; Kanda, H.; Hayashi, K. Association between mental health status and sleep status among adolescents in Japan: A nationwide cross-sectional survey. J. Clin. Psychiatry 2007, 68, 1426–1435. [Google Scholar] [CrossRef]
- Shimizu, M.; Gillis, B.T.; Buckhalt, J.A.; El-Sheikh, M. Linear and Nonlinear Associations between Sleep and Adjustment in Adolescence. Behav. Sleep Med. 2019, 1–15. [Google Scholar] [CrossRef]
- Kalak, N.; Brand, S.; Beck, J.; Holsboer-Trachsler, E.; Wollmer, M.A. Association between subjective actual sleep duration, subjective sleep need, age, body mass index, and gender in a large sample of young adults. Neuropsychiatr. Dis. Treat. 2015, 11, 107–113. [Google Scholar] [CrossRef]
- Mahlmann, L.; Gerber, M.; Furlano, R.I.; Legeret, C.; Kalak, N.; Holsboer-Trachsler, E.; Brand, S. Impaired objective and subjective sleep in children and adolescents with inflammatory bowel disease compared to healthy controls. Sleep Med. 2017, 39, 25–31. [Google Scholar] [CrossRef]
- Lemola, S.; Ledermann, T.; Friedman, E.M. Variability of sleep duration is related to subjective sleep quality and subjective well-being: An actigraphy study. PLoS ONE 2013, 8, e71292. [Google Scholar] [CrossRef]
- Farhangi, M.A. Night Eating Syndrome and Its Relationship with Emotional Eating, Sleep Quality and Nutritional Status Among Adolescents’ Boys. Community Ment. Health J. 2019, 55, 1411–1418. [Google Scholar] [CrossRef] [PubMed]
- Strong, C.; Lin, C.-Y.; Jalilolghadr, S.; Updegraff, J.A.; Broström, A.; Pakpour, A.H. Sleep hygiene behaviours in Iranian adolescents: An application of the Theory of Planned Behavior. J. Sleep Res. 2018, 27, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behaviour: Reactions and reflections. Psychol. Health 2011, 26, 1113–1127. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallieres, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Bajoghli, H.; Alipouri, A.; Holsboer-Trachsler, E.; Brand, S. Sleep patterns and psychological functioning in families in northeastern Iran; evidence for similarities between adolescent children and their parents. J. Adolesc. 2013, 36, 1103–1113. [Google Scholar] [CrossRef]
- Bajoghli, H.; Farnia, V.; Joshaghani, N.; Haghighi, M.; Jahangard, L.; Ahmadpanah, M.; Sadeghi Bahmani, D.; Holsboer-Trachsler, E.; Brand, S. "I love you forever (more or less)"-stability and change in adolescents’ romantic love status and associations with mood states. Rev. Bras. Psiquiatr. 2017, 39, 323–329. [Google Scholar] [CrossRef][Green Version]
- Bajoghli, H.; Joshaghani, N.; Gerber, M.; Mohammadi, M.R.; Holsboer-Trachsler, E.; Brand, S. In Iranian female and male adolescents, romantic love is related to hypomania and low depressive symptoms, but also to higher state anxiety. Int. J. Psychiatry Clin. Pract. 2013, 17, 98–109. [Google Scholar] [CrossRef]
- Bajoghli, H.; Joshaghani, N.; Mohammadi, M.R.; Holsboer-Trachsler, E.; Brand, S. In female adolescents, romantic love is related to hypomanic-like stages and increased physical activity, but not to sleep or depressive symptoms. Int. J. Psychiatry Clin. Pract. 2011, 15, 164–170. [Google Scholar] [CrossRef]
- Bajoghli, H.; Keshavarzi, Z.; Mohammadi, M.R.; Schmidt, N.B.; Norton, P.J.; Holsboer-Trachsler, E.; Brand, S. "I love you more than I can stand!"-romantic love, symptoms of depression and anxiety, and sleep complaints are related among young adults. Int. J. Psychiatry Clin. Pract. 2014, 18, 169–174. [Google Scholar] [CrossRef]
- Chehri, A.; Khazaie, H.; Eskandari, S.; Khazaie, S.; Holsboer-Trachsler, E.; Brand, S.; Gerber, M. Validation of the Farsi version of the revised Adolescent Sleep Hygiene Scale (ASHSr): A cross-sectional study. BMC Psychiatry 2017, 17, 408. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-Y.; Strong, C.; Siu, A.M.H.; Jalilolghadr, S.; Nilsen, P.; Broström, A.; Pakpour, A.H. Validating the Persian Adolescent Sleep Hygiene Scale-Revised (ASHSr) using comprehensive psychometric testing methods. Sleep Med. 2018, 50, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Amra, B.; Shahsavari, A.; Shayan-Moghadam, R.; Mirheli, O.; Moradi-Khaniabadi, B.; Bazukar, M.; Yadollahi-Farsani, A.; Kelishadi, R. The association of sleep and late-night cell phone use among adolescents. J. Pediatr. 2017, 93, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Sadeghniiat-Haghighi, K.; Montazeri, A.; Khajeh-Mehrizi, A.; Nedjat, S.; Aminian, O. The Insomnia Severity Index: Cross-cultural adaptation and psychometric evaluation of a Persian version. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2014, 23, 533–537. [Google Scholar] [CrossRef]
- Farrahi Moghaddam, J.; Nakhaee, N.; Sheibani, V.; Garrusi, B.; Amirkafi, A. Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P). Sleep Breath. Schlaf Atm. 2012, 16, 79–82. [Google Scholar] [CrossRef]
- Khosravifar, S.; Bandi, M.G.; Alavi, K.; Javadi, P.H.S. Evaluation of the psychometric properties of the Persian version of the Pittsburgh Sleep Quality Index in depressed patients. Electron. Phys. 2015, 7, 1644–1652. [Google Scholar] [CrossRef]
- Raniti, M.B.; Waloszek, J.M.; Schwartz, O.; Allen, N.B.; Trinder, J. Factor structure and psychometric properties of the Pittsburgh Sleep Quality Index in community-based adolescents. Sleep 2018, 41. [Google Scholar] [CrossRef]
- Passos, M.H.P.; Silva, H.A.; Pitangui, A.C.R.; Oliveira, V.M.A.; Lima, A.S.; Araújo, R.C. Reliability and validity of the Brazilian version of the Pittsburgh Sleep Quality Index in adolescents. J. Pediatr. 2017, 93, 200–206. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Brislin, R.W. The wording and translation of research instrument. In Field Methods in Cross-Cultural Research; Lonner, W.J., Berry, J.W., Eds.; SAGE: Beverly Hills, Los Angeles, CA, USA, 1986; pp. 137–164. [Google Scholar]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef] [PubMed]
- Storfer-Isser, A.; Lebourgeois, M.K.; Harsh, J.; Tompsett, C.J.; Redline, S. Psychometric properties of the Adolescent Sleep Hygiene Scale. J. Sleep Res. 2013, 22, 707–716. [Google Scholar] [CrossRef] [PubMed]
- LeBourgeois, M.K.; Giannotti, F.; Cortesi, F.; Wolfson, A.; Harsh, J. Sleep hygiene and sleep quality in Italian and American adolescents. Ann. N. Y. Acad. Sci. 2004, 1021, 352–354. [Google Scholar] [CrossRef] [PubMed]
- McDonald, R.P.; Ho, M.-H.R. Principles and practice in reporting structural equation analyses. Psychol. Methods 2002, 7, 64–82. [Google Scholar] [CrossRef]
- Byrne, B. Structural Equation Modeling with AMOS. Basic Concepts, Applications, and Programming; Taylor & Francis: New York, NY, USA, 2010. [Google Scholar]
- Comrey, A.L.; Lee, H.B. A First Course in Factor Analysis; Erlbaum: Hillsdale, NJ, USA, 1992. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Adib-Hajbaghery, M.; Izadi-Avanji, F.; Akbari, H. Quality of sleep and its related risk factors in hospitalized older patients in Kashan’s Hospitals, Iran 2009. Iran. J. Nurs. Midwifery Res. 2012, 17, 414–420. [Google Scholar]
- Yazdi, Z.; Sadeghniiat-Haghighi, K.; Zohal, M.A.; Elmizadeh, K. Validity and reliability of the Iranian version of the insomnia severity index. Malays. J. Med. Sci. 2012, 19, 31–36. [Google Scholar]
- Baglioni, C.; Nanovska, S.; Regen, W.; Spiegelhalder, K.; Feige, B.; Nissen, C.; Reynolds, C.F.; Riemann, D. Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychol. Bull. 2016, 142, 969–990. [Google Scholar] [CrossRef]
- Baglioni, C.; Spiegelhalder, K.; Lombardo, C.; Riemann, D. Sleep and emotions: A focus on insomnia. Sleep Med. Rev. 2010, 14, 227–238. [Google Scholar] [CrossRef]
- Hertenstein, E.; Feige, B.; Gmeiner, T.; Kienzler, C.; Spiegelhalder, K.; Johann, A.; Jansson-Frojmark, M.; Palagini, L.; Rucker, G.; Riemann, D.; et al. Insomnia as a predictor of mental disorders: A systematic review and meta-analysis. Sleep Med. Rev. 2018, 43, 96–105. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Knutson, K.L.; Rathouz, P.J.; Yan, L.L.; Liu, K.; Lauderdale, D.S. Stability of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Questionnaires over 1 year in early middle-aged adults: The CARDIA study. Sleep 2006, 29, 1503–1506. [Google Scholar] [CrossRef] [PubMed]
- Millman, R.P. Excessive sleepiness in adolescents and young adults: Causes, consequences, and treatment strategies. Pediatrics 2005, 115, 1774–1786. [Google Scholar] [CrossRef] [PubMed]
- Polanczyk, C.A.; de Lima, M.S.; Horta, B.L.; Biederman, J.; Rohde, L.A. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am. J. Psychiatry 2007, 164, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Polanczyk, C.A.; Willcutt, E.G.; Salum, G.A.; Kieling, C.; Rohde, L.A. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int. J. Epidemiol. 2014, 43, 434–442. [Google Scholar] [CrossRef] [PubMed]
| Dimensions | ||||||||
|---|---|---|---|---|---|---|---|---|
| Subjective Sleep Quality | Sleep Onset Latency | Sleep Duration | Habitual Sleep Efficiency | Sleep Disturbances | Medication Use | Daytime Dysfunction | Overall Sleep Quality | |
| Subjective sleep quality | - | 0.24 *** | 0.26 *** | 0.11 ** | 0.31 *** | 0.19 *** | 0.23 *** | 0.59 *** |
| Sleep onset latency | - | 0.16 *** | 0.07 * | 0.25 *** | 0.09 * | 0.24 *** | 0.52 *** | |
| Sleep duration | - | 0.31 *** | 0.20 ** | 0.11 * | 0.11 * | 0.55 *** | ||
| Habitual sleep efficiency | - | 0.09 * | 0.17 ** | 0.10 * | 0.52 *** | |||
| Sleep disturbances | - | 0.32 *** | 0.38 *** | 0.60 *** | ||||
| Medication use | - | 0.23 ** | 0.54 *** | |||||
| Daytime dysfunction | - | 0.58 *** | ||||||
| Overall sleep quality | - | |||||||
| Component | Cronbach’s Alpha When Item Deleted | |
|---|---|---|
| 1 | Subjective sleep quality | 0.77 |
| 2 | Sleep latency | 0.71 |
| 3 | Sleep duration | 0.69 |
| 4 | Sleep efficiency | 0.79 |
| 5 | Sleep disturbance | 0.79 |
| 6 | Use of sleep medication | 0.77 |
| 7 | Daytime dysfunction | 0.070 |
| Cronbach’s alpha | 0.73 |
| Adolescent Sleep Hygiene Scale Factors | ||||||
|---|---|---|---|---|---|---|
| Physiological | Behavioral–Arousing | Cognitive–Emotional | Daytime Sleepiness | Sleep Environment | Sleep Stability | |
| Pittsburgh Sleep Quality Index | ||||||
| Subjective sleep quality | 0.15 ** | 0.25 *** | 0.26 *** | 0.27 *** | 0.16 *** | 0.21 *** |
| Sleep onset latency | 0.00 | 0.07 * | 0.21 *** | 0.13 ** | 0.01 | 0.15 *** |
| Sleep duration | 0.11 ** | 0.15 *** | 0.19 *** | 0.15 ** | 0.05 | 0.10 * |
| Habitual sleep efficiency | 0.02 | 0.06 | 0.06 | 0.06 | 0.06 | 0.09 * |
| Sleep disturbances | 0.24 *** | 0.30 *** | 0.33 *** | 0.35 *** | 0.29 *** | 0.23 *** |
| Medication use | 0.30 *** | 0.31 *** | 0.23 *** | 0.25 *** | 0.30 *** | 0.17 *** |
| Daytime dysfunction | 0.15 * | 0.17 ** | 0.24 *** | 0.21 *** | 0.19 *** | 0.18 *** |
| Overall sleep quality | 0.24 *** | 0.33 *** | 0.38 *** | 0.35 *** | 0.26 ** | 0.28 *** |
| Pittsburgh Sleep Quality Index; Categories | ||||
|---|---|---|---|---|
| Good Sleepers | Poor Sleepers | |||
| N | 729 | 748 | ||
| M (SD) | M (SD) | t-tests | Cohen’s d | |
| Dimensions of Adolescent Sleep Hygiene Scale | ||||
| Physiological | 12.93 (4.27) | 14.66 (4.96) | t(1475) = 7.15 *** | 0.37 (S) |
| Behavioral–arousing | 6.22 (2.78) | 7.80 (3.35) | t(1475) = 9.83 *** | 0.51 (M) |
| Cognitive–emotional | 18.74 (5.81) | 22.12 (5.79 | t(1475) = 11.21 *** | 0.58 (M) |
| Daytime sleepiness | 5.29 (2.43) | 6.92 (2.83) | t(1475) = 11.86 *** | 0.61 (M) |
| Sleep environment | 11.18 (4.69) | 13.58 (5.43) | t(1475) = 9.09 *** | 0.47 (S) |
| Sleep stability | 9.09 (3.38) | 10.68 (3.49) | t(1475) = 8.91 *** | 0.46 (S) |
| New Factors | |||||
|---|---|---|---|---|---|
| Original Dimensions | High Sleep Disturbances, Medication Use and Low Daytime Function | Short Sleep Duration and Low Sleep Efficiency | Short Sleep Duration and Poor Sleep Quality | Long Sleep Onset Latency and Low Daytime Function | |
| Overall variance | 72.72% | 31.8% | 16.1% | 13.5% | 11.2% |
| Subjective sleep quality | 0.833 | ||||
| Sleep onset latency | 0.867 | ||||
| Sleep Duration | 0.581 | 0.603 | |||
| Habitual sleep efficiency | 0.906 | ||||
| Sleep disturbances | 0.673 | ||||
| Use of sleep medications | 0.807 | ||||
| Daytime dysfunction | 0.613 | 0.505 | |||
| Dimension | Variables | Coefficient | Standard Error | Coefficient β | t | p | R | R2 | Durbin–Watson Coefficient |
|---|---|---|---|---|---|---|---|---|---|
| ASHS total score | Intercept | 11.61 | 0.072 | - | 160.851 | 0.000 | 0.485 | 0.235 | 1.572 |
| High sleep disturbances, medication use and low daytime function | 1.345 | 0.072 | 0.424 | 18.623 | 0.000 | ||||
| Short sleep duration and low sleep efficiency | 0.720 | 0.072 | 0.227 | 9.967 | 0.000 | ||||
| Long sleep onset latency and low daytime function | 0.189 | 0.072 | 0.060 | 2.616 | 0.006 | ||||
| Excluded variable: | Short sleep duration and poor sleep quality: p > 0.05 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chehri, A.; Brand, S.; Goldaste, N.; Eskandari, S.; Brühl, A.; Sadeghi Bahmani, D.; Khazaie, H. Psychometric Properties of the Persian Pittsburgh Sleep Quality Index for Adolescents. Int. J. Environ. Res. Public Health 2020, 17, 7095. https://doi.org/10.3390/ijerph17197095
Chehri A, Brand S, Goldaste N, Eskandari S, Brühl A, Sadeghi Bahmani D, Khazaie H. Psychometric Properties of the Persian Pittsburgh Sleep Quality Index for Adolescents. International Journal of Environmental Research and Public Health. 2020; 17(19):7095. https://doi.org/10.3390/ijerph17197095
Chicago/Turabian StyleChehri, Azita, Serge Brand, Nastaran Goldaste, Sodabeh Eskandari, Annette Brühl, Dena Sadeghi Bahmani, and Habibolah Khazaie. 2020. "Psychometric Properties of the Persian Pittsburgh Sleep Quality Index for Adolescents" International Journal of Environmental Research and Public Health 17, no. 19: 7095. https://doi.org/10.3390/ijerph17197095
APA StyleChehri, A., Brand, S., Goldaste, N., Eskandari, S., Brühl, A., Sadeghi Bahmani, D., & Khazaie, H. (2020). Psychometric Properties of the Persian Pittsburgh Sleep Quality Index for Adolescents. International Journal of Environmental Research and Public Health, 17(19), 7095. https://doi.org/10.3390/ijerph17197095








