Examining Older Adults’ Perspectives on the Built Environment and Correlates of Healthy Aging in an American Age-Friendly Community
Abstract
1. Introduction
1.1. Ecological Context of Healthy Aging
1.2. Aging, Health and the Built Environment
1.3. Age-Friendly Community Background
2. Materials and Methods
2.1. Study Design and Measures
2.2. Sampling
2.3. Process and Procedures
2.4. Participants and Exclusion Criteria
2.5. Data Analysis
3. Results
3.1. Clusters of Community-Dwelling Older Adults by Health
3.2. Perspectives on the Built Environment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Clarke, P.; Nieuwenhuijsen, E.R. Environments for healthy ageing: A critical review. Maturitas 2009, 64, 14–19. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Age-Friendly Cities: A Guide; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- WHO. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Bronfenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design; Harvard University Press: Cambridge, MA, USA, 1979. [Google Scholar]
- Administration for Community Living. Profile of Older Americans 2019; Administration for Community Living: Washington, DC, USA, 2020.
- WHO. Housing and Health Guidelines; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Harrell, R.; Lynott, J.; Guzman, S.; Lampkin, C. What is Livable? Community Preferences of Older Adults; AARP Public Policy Institute: Washington, DC, USA, 2017. [Google Scholar]
- Golant, S. The quest for residential normalcy by older adults: Relocation but one pathway. J. Aging Stud. 2011, 25, 93–205. [Google Scholar] [CrossRef]
- Walker, R.B.; Hiller, J.E. Places and health: A qualitative study to explore how older women living alone perceive the social and physical dimensions of their neighbourhoods. Soc. Sci. Med. 2007, 65, 1154–1165. [Google Scholar] [CrossRef] [PubMed]
- AARP. Making Room: Housing for A Changing America; AARP Foundation: Washington, DC, USA, 2019. [Google Scholar]
- Musselwhite, C.; Shergold, I. Examining the process of driving cessation in later life. Eur. J. Ageing 2012, 10, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Foley, D.J.; Heimovitz, H.K.; Guralnik, J.M.; Brock, D.B. Driving life expectancy of persons aged 70 years and older in the United States. Am. J. Public Health 2009, 92, 1284–1289. [Google Scholar] [CrossRef]
- Yang, Y.; Xu, Y.; Rodriguez, D.A.; Michael, Y.; Zhang, H. Active travel, public transportation use, and daily transport among older adults: The association of built environment. J. Trans. Health 2018, 9, 288–298. [Google Scholar] [CrossRef]
- MacLeod, K.E.; Ragland, D.R.; Prohaska, T.R.; Smith, M.L.; Irmiter, C.; Satariano, W.A. Missed or delayed medical care appointments by older users of nonemergency medical transportation. Gerontologist 2018, 55, 1026–1037. [Google Scholar] [CrossRef]
- Matsuda, N.; Murata, S.; Torizawa, K.; Isa, T.; Ebina, A.; Kondo, Y.; Tsuboi, J.; Fukuta, A.; Okumura, M.; Shigemoto, C.; et al. Association between public transportation use and loneliness among urban elderly people who stop driving. Geron. Ger. Med. 2019, 5. [Google Scholar] [CrossRef] [PubMed]
- Reinhard, E.; Courtin, E.; Lenthe, F.J.; Avendrano, M. Public transport policy, social engagement and mental health in older age: A quasi-experimental evaluation of free bus passes in England. Epidemiol. Community Health 2018, 72, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Yen, I.H.; Anderson, L.A. Built environment and mobility of older adults: Important policy and practice efforts. J. Am. Ger. Soc. 2011, 60, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Coon, J.T.; Boddy, K.; Stein, K.; Whear, R.; Barton, J.; Depledge, M.H. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ. Sci. Technol. 2011, 45, 1761–1772. [Google Scholar] [CrossRef] [PubMed]
- Etnier, J.L.; Karper, W.B.; Park, S.-Y.; Shih, C.-H.; Aaron, T.; Piepmeier, A.T.; Wideman, L. Motivating mature adults to be physically active. J. Aging Phys. Activity 2018, 25, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Satariano, W.A.; Ivey, S.L.; Kurtovich, E.; Kealey, M.; Hubbard, A.E.; Bayles, C.M.; Bryant, L.L.; Hunter, R.H.; Prohaska, T.R. Lower-body function, neighborhoods, and walking in an older population. Am. J. Prev. Med. 2010, 38, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.A.; Han, B.; Nagel, K.J.; Harnik, P.; McKenzie, T.L.; Evenson, K.R.; Marsh, T.; Williamsol, S.; Vaughan, H.; Katta, S. The first national study of neighborhood parks. Am. J. Prev. Med. 2016, 51, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Florida Department of Health. Profile of Aging Sarasota County; Florida Department of Health: Tallahassee, FL, USA, 2020. Available online: http://www.flhealthcharts.com/ChartsReports/rdPage.aspx?rdReport=ChartsProfiles.AgingInFloridaProfile (accessed on 15 July 2020).
- Wong, M.; Yu, R. Effects of perceived neigbourhood environments on self-rated health among community-dwelling older Chinese. Int. J. Environ. Res. Public Health 2017, 14, 614. [Google Scholar] [CrossRef] [PubMed]
- Garner, I.W.; Holland, C.A. Age-friendliness of living environments from the older person’s viewpoint: Development of the age-friendly environmental assessment tool. Age Ageing 2019, 49, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Black, K.; Hyer, K. Generational distinctions on the importance of age-friendly community features by older age groups. J. Appl. Gerontol. 2020, 39, 1025–1034. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, D.E.; Huang, D.L.; Simonovich, S.D.; Belza, B. Outdoor built environment barriers and facilitators to activity among midlife and older adults with mobility disabilities. Gerontologist 2012, 53, 268–279. [Google Scholar] [CrossRef] [PubMed]
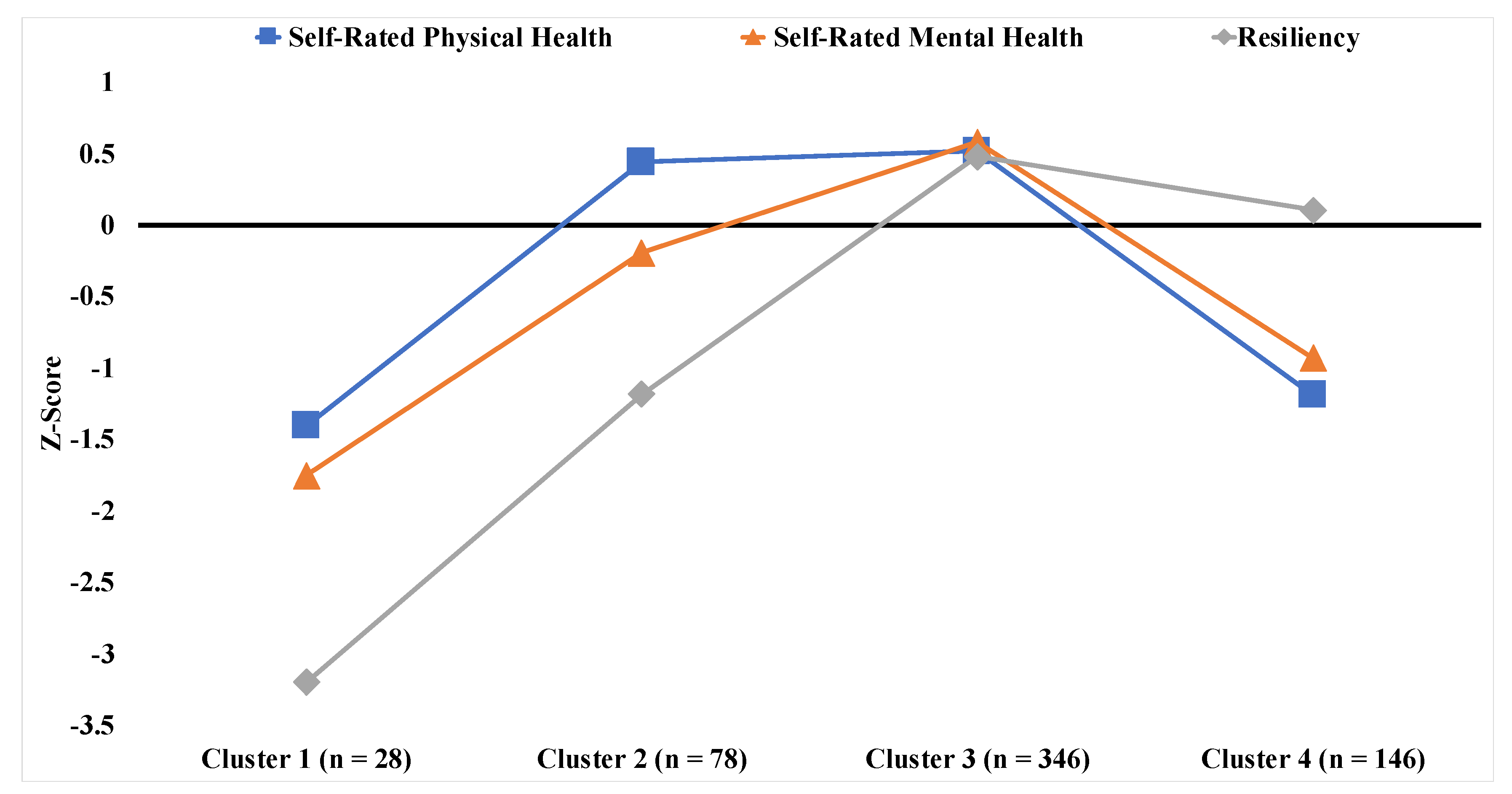
| Cluster 1 N = 28 | Cluster 2 N = 78 | Cluster 3 N = 346 | Cluster 4 N = 146 | p | |
|---|---|---|---|---|---|
| M (SD)% (n) | M (SD)% (n) | M (SD)% (n) | M (SD)% (n) | ||
| Built Environment Domains | |||||
| Outdoor Spaces and Buildings | 5.82 (1.61) | 5.78 (1.60) | 5.87 (1.66) | 5.78 (1.74) | 0.94 |
| Housing | 6.36 (1.68) | 6.21 (2.12) | 5.61 (2.21) | 6.20 (2.09) | 0.008 |
| Transportation | 15.86 (1.92) | 15.14 (3.31) | 13.64 (4.27) | 14.86 (3.43) | <0.001 |
| Health Dimensions | |||||
| Self-Rated Physical Health | 2.71 (0.66) | 4.37 (0.51) | 4.44 (0.54) | 2.90 (0.59) | <0.001 |
| Self-Rated Mental Health | 2.54 (0.79) | 3.92 (0.73) | 4.61 (0.49) | 3.27 (0.69) | <0.001 |
| Social Connectedness (Yes) | 57% (16) | 86% (67) | 97% (336) | 82% (120) | <0.001 |
| Functional Capacities | |||||
| Resiliency | 1.25 (0.84) | 2.76 (0.49) | 4.00 (0.00) | 3.72 (0.45) | <0.001 |
| Physical Needs | 1.21 (1.03) | 0.87 (0.69) | 1.01 (0.65) | 1.21 (0.79) | 0.002 |
| Home Adaptations | 1.46 (1.55) | 0.74 (1.18) | 1.09 (1.40) | 1.40 (1.42) | 0.004 |
| Demographic Covariates | |||||
| Age | 62.86 (9.01) | 65.73 (9.20) | 68.76 (8.70) | 67.58 (9.08) | <0.001 |
| Gender (% Male) | 29% (8) | 23% (18) | 41% (142) | 27% (39) | 0.002 |
| Race (% Non-White Race) | 0% (0) | 5% (4) | 5% (17) | 4% (6) | 0.67 |
| Marital Status | 0.07 | ||||
| Married | 61% (17) | 63% (49) | 64% (220) | 63% (92) | |
| Divorced | 14% (4) | 22% (17) | 14% (49) | 12% (18) | |
| Widowed | 7% (2) | 6% (5) | 13% (44) | 13% (19) | |
| Never Married | 14% (4) | 9% (7) | 3% (12) | 5% (8) | |
| Unmarried and Cohabiting | 4% (1) | 0% (0) | 6% (21) | 6% (9) | |
| Education | 0.002 | ||||
| K-12th Grade | 7% (2) | 4% (3) | 0% (0) | 0% (0) | |
| High School Graduate | 4% (1) | 1% (1) | 2% (6) | 3% (4) | |
| Post-High School Education | 11% (3) | 9% (7) | 7% (25) | 15% (22) | |
| 2 year College Degree | 14% (4) | 13% (10) | 9% (30) | 11% (16) | |
| 4 year College Degree | 36% (10) | 27% (21) | 35% (120) | 32% (47) | |
| Graduate/Profess Degree | 29% (8) | 46% (36) | 48% (165) | 39% (57) | |
| Income | <0.001 | ||||
| <$10,000 | 14% (4) | 3% (2) | 1% (5) | 2% (3) | |
| $10,000–$19,999 | 4% (1) | 4% (3) | 1% (4) | 5% (8) | |
| $20,000–$29,999 | 11% (3) | 14% (11) | 4% (15) | 5% (7) | |
| $30,000–$49,999 | 21% (6) | 10% (8) | 11% (39) | 23% (33) | |
| $50,000–$74,999 | 11% (3) | 22% (17) | 20% (68) | 21% (30) | |
| $75,000–$99,999 | 7% (2) | 15% (12) | 16% (57) | 21% (31) | |
| $100,000–$149,000 | 7% (2) | 26% (20) | 16% (54) | 12% (17) | |
| >$150,000 | 25% (7) | 6% (5) | 30% (104) | 12% (17) |
| Outdoor Spaces and Buildings | Housing | Transportation | ||||
|---|---|---|---|---|---|---|
| Beta [95% CI] | p | Beta [95% CI] | p | Beta [95% CI] | p | |
| Cluster 1 (ref = 3) | −0.14 [−0.80, 0.53] | 0.68 | 0.38 [−0.46, 1.22] | 0.37 | 1.71 [0.17, 3.25] | 0.03 * |
| Cluster 2 (ref = 3) | −0.18 [−0.60, 0.24] | 0.40 | 0.42 [−0.11, 0.95] | 0.12 | 1.29 [0.31, 2.26] | 0.01 * |
| Cluster 4 (ref = 3) | −0.13 [−0.47, 0.21] | 0.46 | 0.44 [0.02, 0.87] | 0.04 * | 0.87 [0.09, 1.66] | 0.03 * |
| Age | −0.02 [−0.04, 0.00] | 0.01 * | −0.05 [−0.07, −0.03] | <0.001 *** | −0.03 [−0.07, 0.01] | 0.11 |
| Gender (Male) | −0.12 [−0.42, 0.18] | 0.44 | −0.05 [−0.43, 0.33] | 0.80 | −0.41 [−1.11, 0.28] | 0.24 |
| Race (White) | −0.66 [−1.31, −0.01] | 0.05 | −0.42 [−1.23, 0.39] | 0.31 | 0.17 [−1.33, 1.66] | 0.83 |
| Marital Status (Married) | 0.17 [−0.16, 0.50] | 0.31 | 0.34 [−0.07, 0.75] | 0.11 | 0.20 [−0.55, 0.96] | 0.60 |
| Education | 0.07 [−0.06, 0.20] | 0.28 | 0.11 [−0.06, 0.27] | 0.21 | 0.25 [−0.05, 0.55] | 0.10 |
| Income | −0.03 [−0.13, 0.06] | 0.48 | −0.10 [−0.21, 0.02] | 0.10 | −0.27 [−0.48, −0.05] | 0.02 * |
| Physical Needs | −0.09 [−0.29, 0.12] | 0.40 | −0.12 [−0.38, 0.13] | 0.34 | −0.12 [−0.59, 0.35] | 0.62 |
| Home Adaptations | 0.04 [−0.06, 0.14] | 0.42 | 0.17 [0.05, 0.30] | 0.007 ** | 0.38 [0.14, 0.61] | 0.001 ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Black, K.; Jester, D.J. Examining Older Adults’ Perspectives on the Built Environment and Correlates of Healthy Aging in an American Age-Friendly Community. Int. J. Environ. Res. Public Health 2020, 17, 7056. https://doi.org/10.3390/ijerph17197056
Black K, Jester DJ. Examining Older Adults’ Perspectives on the Built Environment and Correlates of Healthy Aging in an American Age-Friendly Community. International Journal of Environmental Research and Public Health. 2020; 17(19):7056. https://doi.org/10.3390/ijerph17197056
Chicago/Turabian StyleBlack, Kathy, and Dylan J. Jester. 2020. "Examining Older Adults’ Perspectives on the Built Environment and Correlates of Healthy Aging in an American Age-Friendly Community" International Journal of Environmental Research and Public Health 17, no. 19: 7056. https://doi.org/10.3390/ijerph17197056
APA StyleBlack, K., & Jester, D. J. (2020). Examining Older Adults’ Perspectives on the Built Environment and Correlates of Healthy Aging in an American Age-Friendly Community. International Journal of Environmental Research and Public Health, 17(19), 7056. https://doi.org/10.3390/ijerph17197056






