Infantile Colic—The Perspective of German and Polish Pediatricians in 2020
Abstract
:1. Introduction
2. Materials and Methods
2.1. Surveys
2.2. Statistical Analyses
3. Results
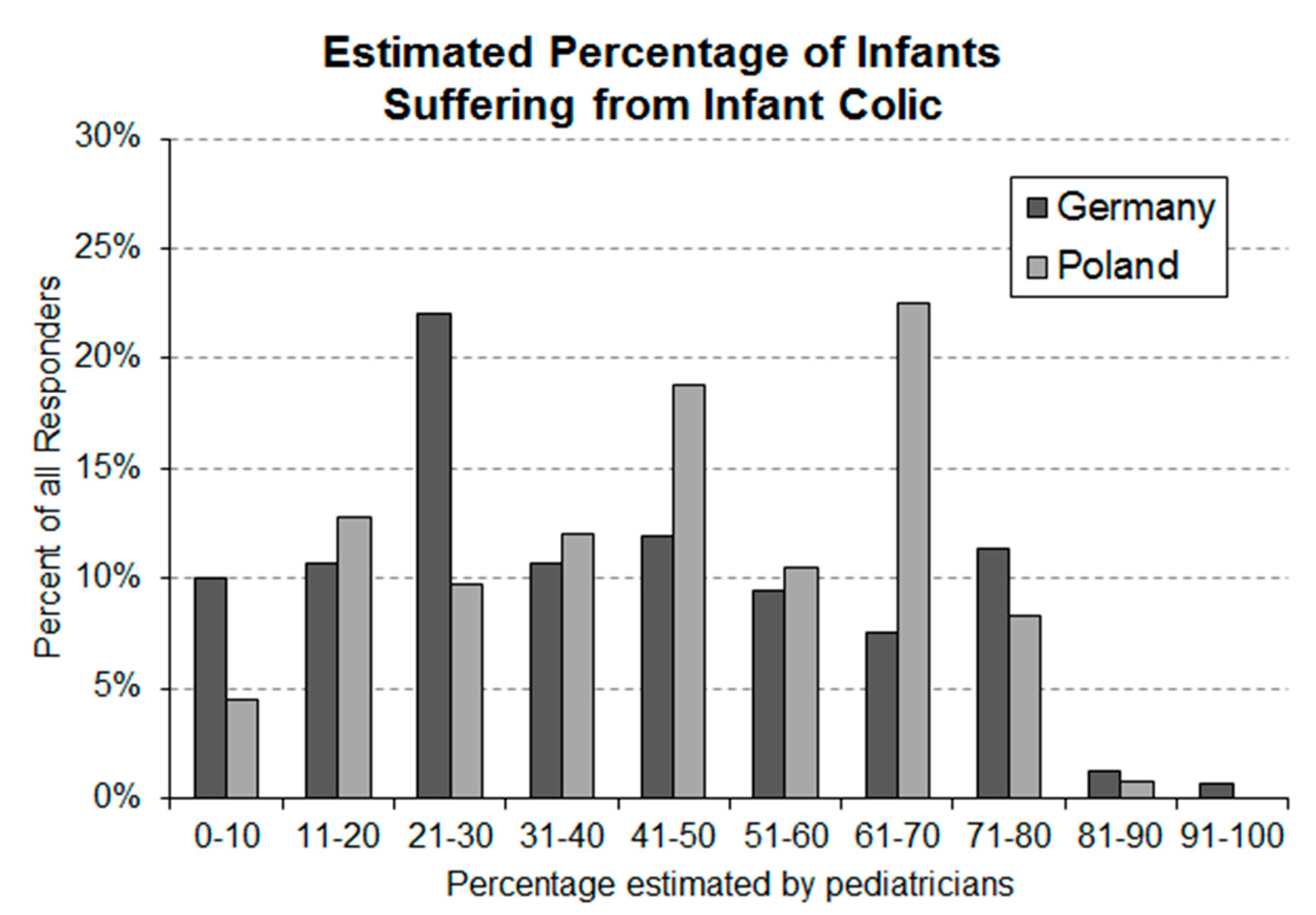
3.1. Question 1: Estimated Occurance Rate of Infantile Colic in Newborns Aged 0–5 Months
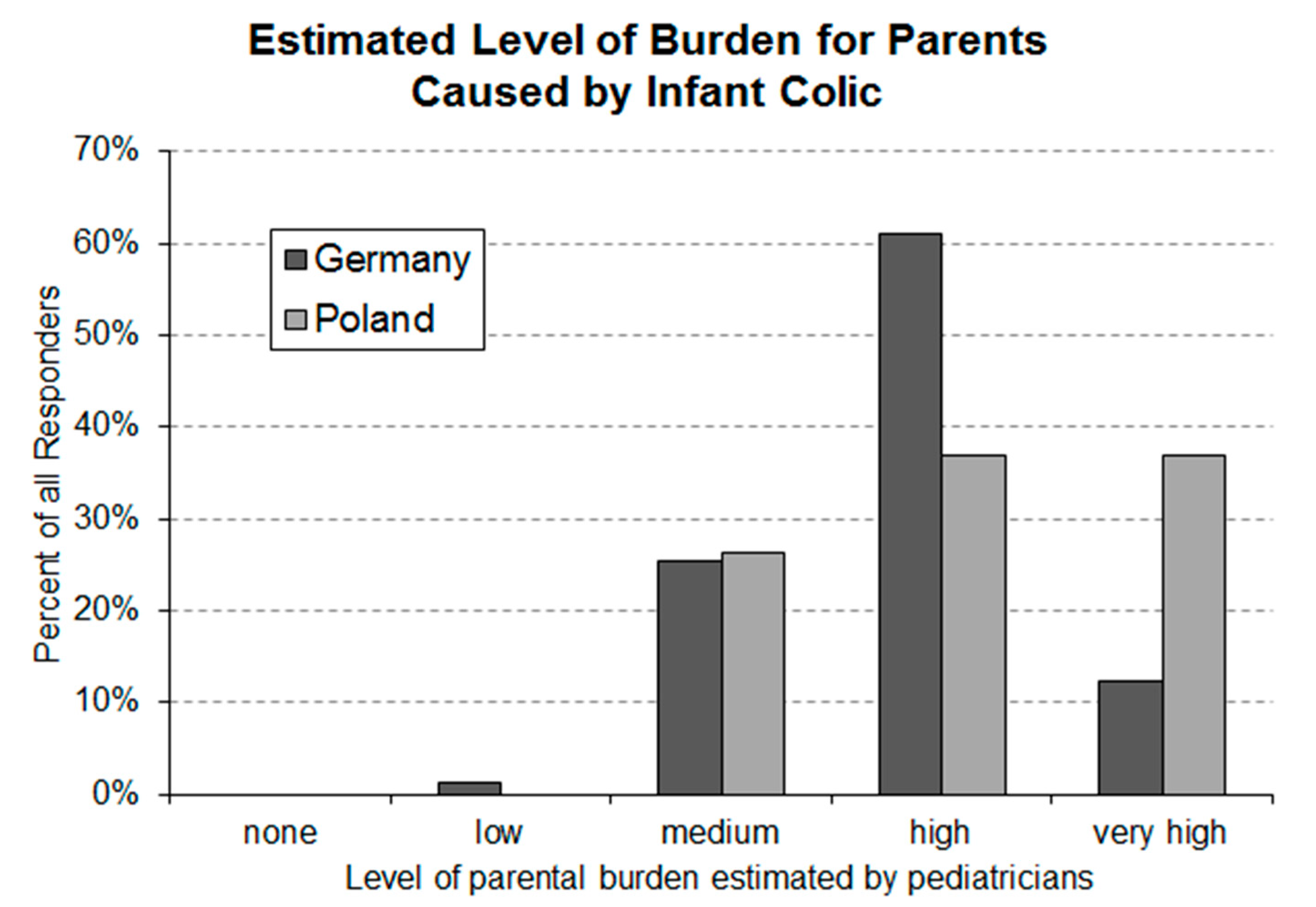
3.2. Question 2: Parental Burden Caused by Infantile Colic as Estimated by Pediatricians
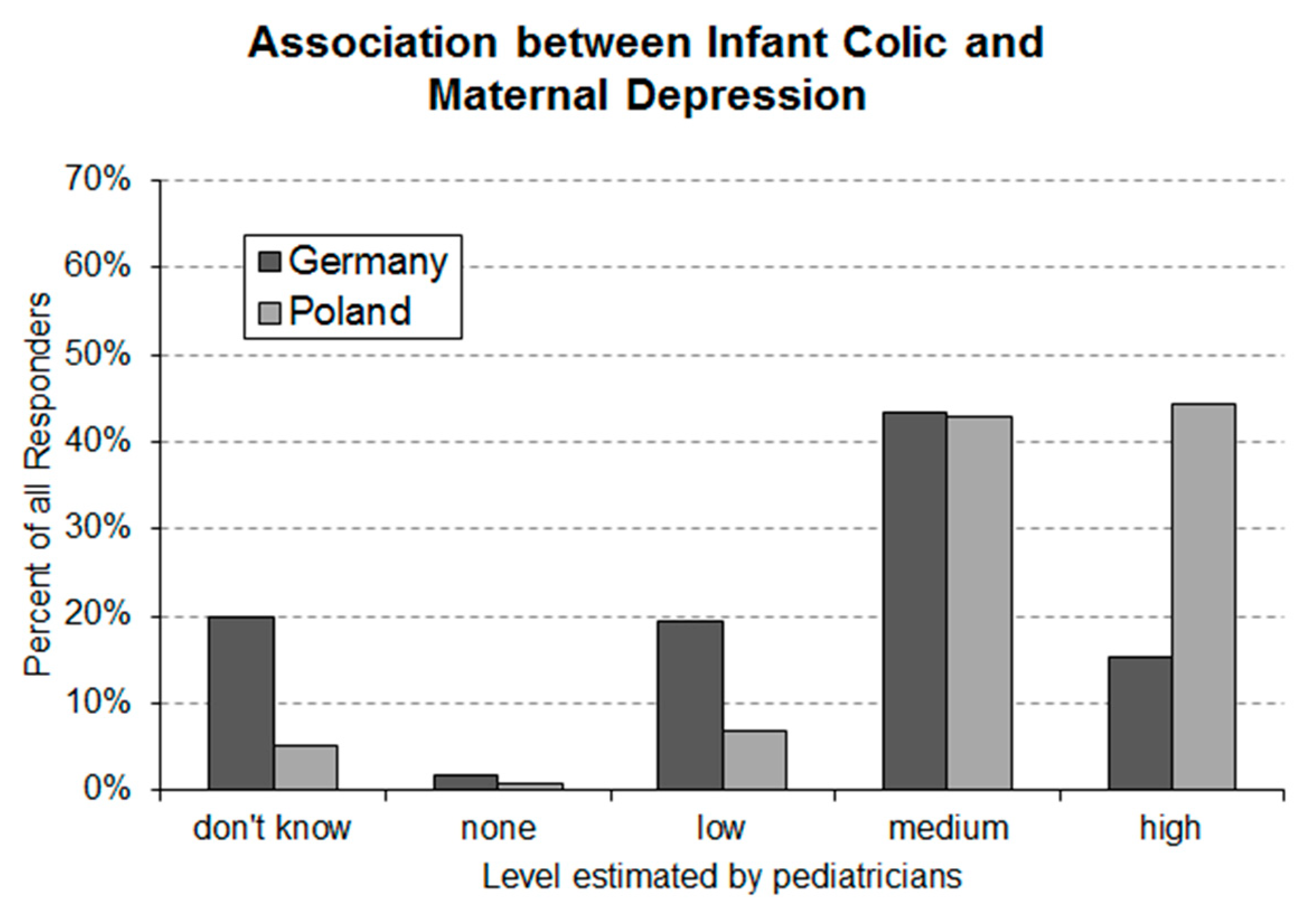
3.3. Question 3: Estimated Assocoation between Maternal Depression and Infantile Colic
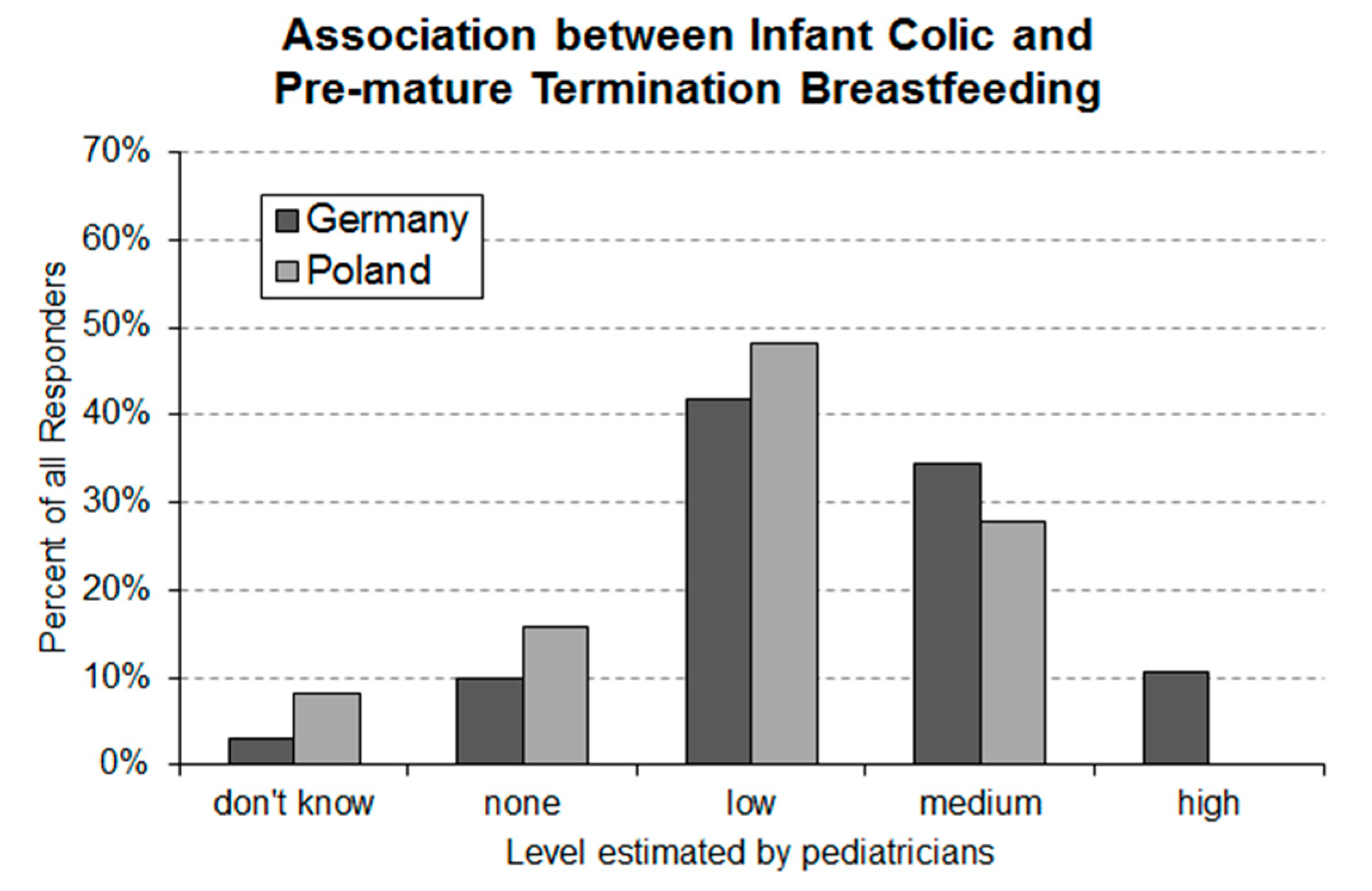
3.4. Question 4: Estimated Association between Premature Termination of Breastfeeding and Infantile Colic
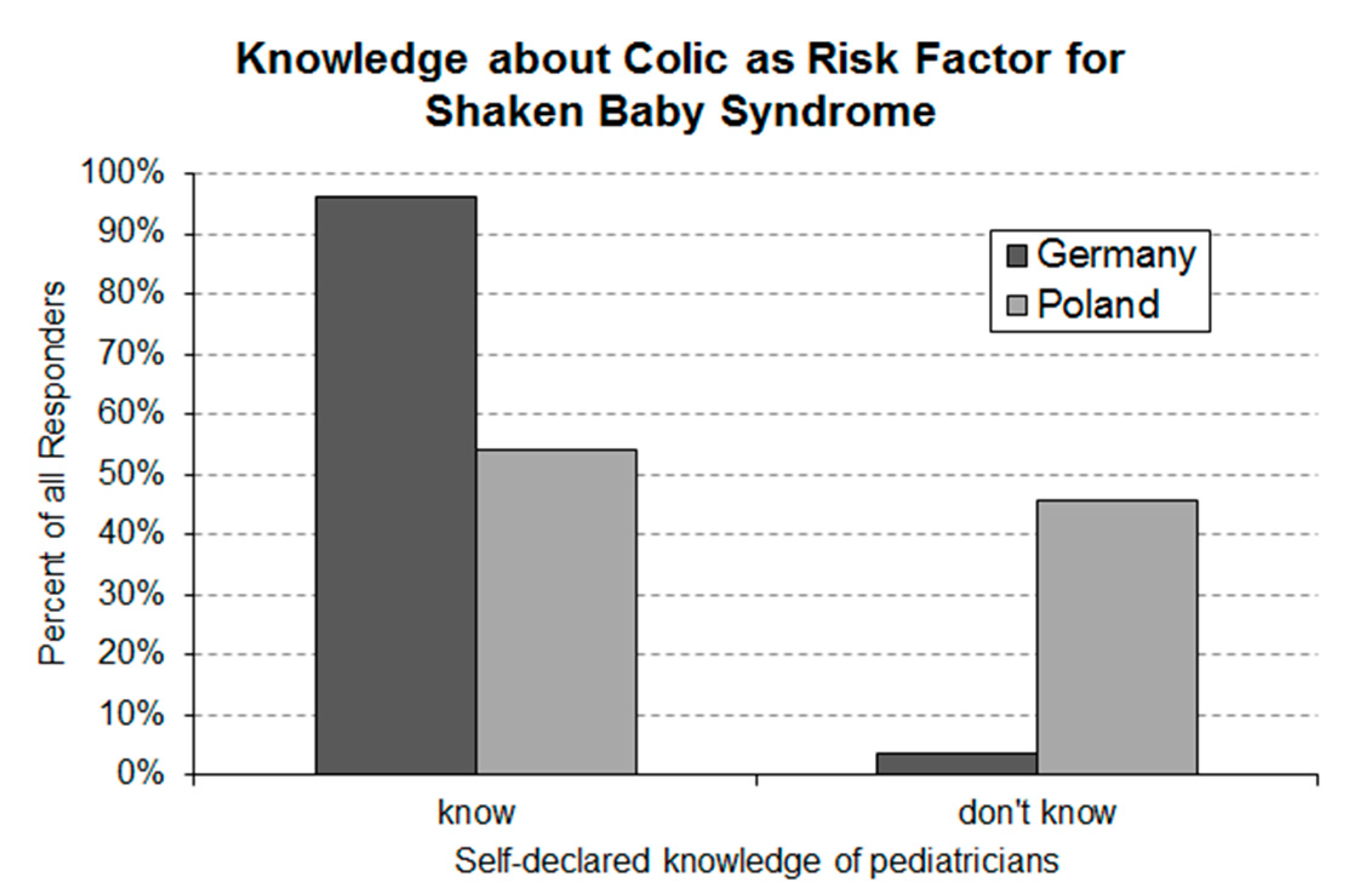
3.5. Question 5: Self-Declared Knowledge of Infantile Colic Being a Risk Factor for Shaken Baby Syndrome
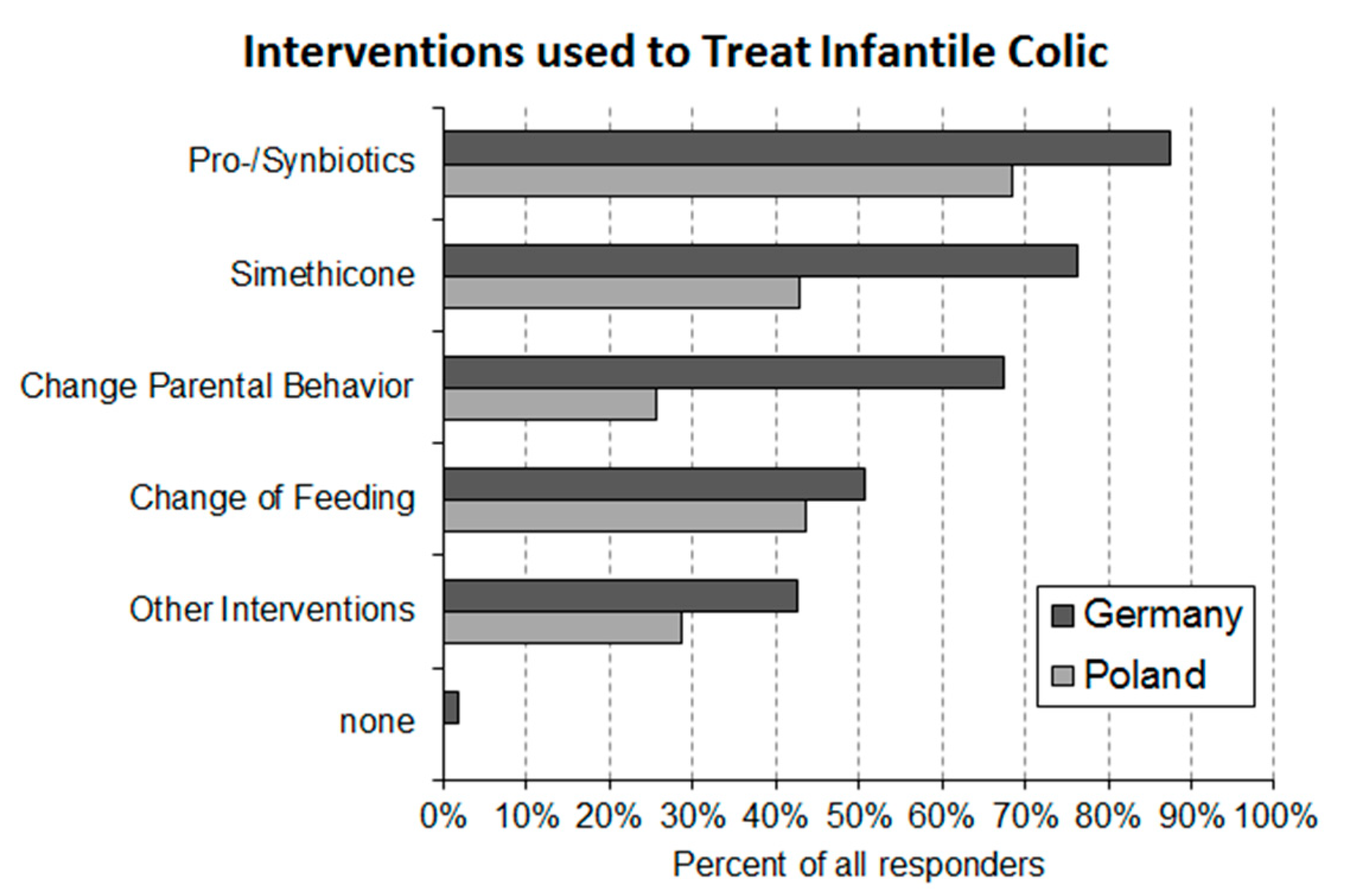
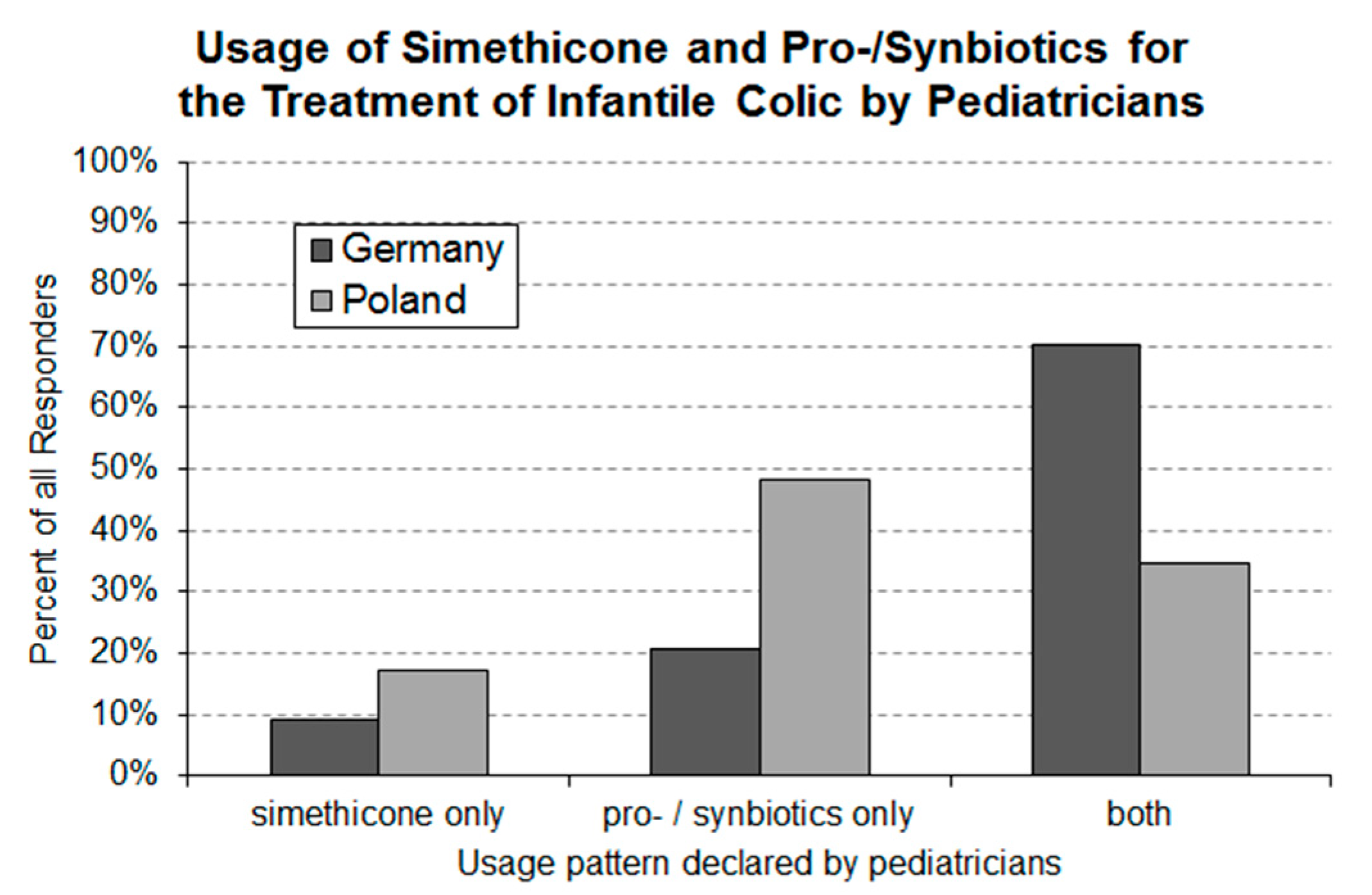
3.6. Question 6: Interventional Approaches Used by Pediatricians for the Treatment of Infantile Colic
3.7. Question 7: Interest in the Topic of Infantile Colic
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wessel, M.A.; Jackson, E.B.; Harris, G.S.; Detwiler, A.C. Paroxysmal fussing in infancy, sometimes called colic. Pediatrics 1954, 14, 421–435. [Google Scholar] [PubMed]
- Lucassen, P.; Assendelft, W.; van Eijk, J.T.M.; Gubbels, J.; Douwes, A.; van Geldrop, W.J. Systematic review of the occurrence of infantile colic in the community. Arch. Dis. Child. 2001, 84, 398–403. [Google Scholar] [CrossRef] [PubMed]
- St James-Roberts, I.; Halil, T. Infant crying patterns in the first year: Normal community and clinical findings. J. Child. Psychol. Psychiatry 1991, 32, 951–968. [Google Scholar] [CrossRef] [PubMed]
- Lucassen, P. Colic in infants. BMJ Clin. Evid. 2010, 2010, 0309. [Google Scholar]
- Sung, V. Infantile colic. Aust. Prescr. 2018, 41, 105–110. [Google Scholar] [CrossRef]
- Vik, T.; Grote, V.; Escribano, J.; Socha, J.; Verduci, E.; Fritsch, M.; Carlier, C.; von Kries, R.; Koletzko, B. For the European Childhood Obesity Trial Study Group. Infantile colic, prolonged crying and maternal postnatal depression. Acta Paediatr. 2009, 98, 1344–1348. [Google Scholar] [CrossRef]
- Howard, C.R.; Lanphear, N.; Lanphear, B.P.; Eberly, S.; Lawrence, R.A. Parental Responses to Infant Crying and Colic: The Effect on Breastfeeding Duration. Breastfeed. Med. 2006, 1, 146–155. [Google Scholar] [CrossRef] [Green Version]
- Barr, R.G. Preventing abusive head trauma resulting from a failure of normal interaction between infants and their caregivers. Proc. Natl. Acad. Sci. USA 2012, 109, 17294–17301. [Google Scholar] [CrossRef] [Green Version]
- Sung, V.; Cabana, M.D. Probiotics for Colic-Is the Gut Responsible for Infant Crying After All? J. Pediatr. 2017, 191, 6–8. [Google Scholar] [CrossRef]
- Savino, F.; Cordisco, L.; Tarasco, V.; Calabrese, R.; Palumeri, E.; Matteuzzi, D. Molecular identification of coliform bacteria from colicky breastfed infants. Acta Paediatr. 2009, 98, 1582–1588. [Google Scholar] [CrossRef]
- Savino, F.; Cresi, F.; Pautasso, S.; Palumeri, E.; Tullio, V.; Roana, J.; Silvestro, L.; Oggero, R. Intestinal microflora in breastfed colicky and non-colicky infants. Acta Paediatr. 2004, 93, 825–829. [Google Scholar] [CrossRef] [PubMed]
- Savino, F.; Bailo, E.; Oggero, R.; Tullio, V.; Roana, J.; Carlone, N.; Cuffini, A.M.; Silvestro, L. Bacterial counts of intestinal Lactobacillus species in infants with colic. Pediatr. Allergy Immunol. 2005, 16, 72–75. [Google Scholar] [CrossRef] [PubMed]
- Savino, F.; Cordisco, L.; Tarasco, V.; Locatelli, E.; Di Gioia, D.; Oggero, R.; Matteuzzi, D. Antagonistic effect of Lactobacillus strains against gas-producing coliforms isolated from colicky infants. BMC Microbiol. 2011, 11, 157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Weerth, C.; Fuentes, S.; de Vos, W.M. Crying in infants. On the possible role of intestinal microbiota in the development of colic. Gut Microbes 2013, 4, 416–421. [Google Scholar] [CrossRef] [Green Version]
- Anabrees, J.; Indrio, F.; Paes, B.; AlFaleh, K. Probiotics for infantile colic: A systematic review. BMC Pediatr. 2013, 13, 186. [Google Scholar] [CrossRef] [Green Version]
- Dryl, R.; Szajewska, H. Probiotics for management of infantile colic: A systematic review of randomized controlled trials. Arch. Med. Sci. 2018, 14, 1137–1143. [Google Scholar] [CrossRef] [Green Version]
- Tintore, M.; Colome, G.; Santas, J.; Espadaler, J. Gut Microbiota Dysbiosis and Role of Probiotics in Infant Colic. Arch. Clin. Microbiol. 2017, 8, 56. [Google Scholar]
- Schreck Bird, A.; Gregory, P.J.; Jalloh, M.A.; Risoldi Cochrane, Z.; Hein, D.J. Probiotics for the Treatment of Infantile Colic: A Systematic Review. J. Pharm. Pract. 2017, 30, 366–374. [Google Scholar] [CrossRef]
- Ong, T.; Gordon, M.; Banks, S.S.C.; Thomas, M.R.; Akobeng, A.K. Probiotics to prevent infantile colic. Cochrane Database Syst. Rev. 2019, 3, CD012473. [Google Scholar] [CrossRef]
- Pärtty, A.; Kalliomäki, M.; Salminen, S.; Isolauri, E. Infantile Colic Is Associated With Low-grade Systemic Inflammation. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 691–695. [Google Scholar] [CrossRef]
- Simethicone. Available online: https://www.drugs.com/mtm/simethicone.html (accessed on 7 September 2020).
- Landgren, K.; Hallström, I. Parents’ experience of living with a baby with infantile colic—A phenomenological hermeneutic study. Scand. J. Caring Sci. 2011, 25, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Von Gontard, A.; Möhler, E.; Bindt, C. S2k Guideline 028/041 “Mental Disorders in the Infant, Toddler and Preschooler” 2015. Available online: https://www.awmf.org/leitlinien/detail/ll/028-041.html (accessed on 1 September 2020).
- Jastrzębska, I. Kolka niemowlęca (Baby colic). Pediatr. Dypl. 2013, 17, 40–45. [Google Scholar]
- Johnson, J.D.; Cocker, K.; Chang, E. Infantile colic: Recognition and treatment. Am. Fam. Physician 2015, 92, 577–582. [Google Scholar] [PubMed]
- Agresti, A. An Introduction to Categorical Data Analysis, 2nd ed.; Wiley-Interscience, John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2007; pp. 297–324. [Google Scholar]
- Hothorn, T.; Hornik, K.; Van de Wiel, M.; Zeileis, A. A Lego System for Conditional Inference. Am. Stat. 2006, 60, 257–263. [Google Scholar] [CrossRef] [Green Version]
- EU Project on Promotion of Breastfeeding in Europe. Protection, Promotion and Support of Breastfeeding in Europe: A Blueprint for Action. European Commission, Directorate Public Health and Risk Assessment, Luxembourg, 2004. Available online: https://ec.europa.eu/health/ph_projects/2002/promotion/fp_promotion_2002_frep_18_en.pdf (accessed on 7 September 2020).
- Przyrembel, H. Stillen und Muttermilchernährung: Grundlagen, Erfahrungen und Empfehlungen/Bundeszentrale für Gesundheitliche Aufklärung, BzgA, Neue, erw. und Überarb. Aufl., Stand: Juli 2001; BzgA: Cologne, Germany, 2001; pp. 13–24. [Google Scholar]
- Szajewska, H.; Horvath, A.; Rybak, A.; Socha, P. Breastfeeding. A Position Paper by the Polish Society for Paediatric Gastroenterology, Hepatology and Nutrition. Stand. Medyczne Pediatr. 2016, 13, 9–24. [Google Scholar]
- Matschke, J.; Herrmann, B.; Sperhake, J.; Körber, F.; Bajanowski, T.; Glatzel, M. Shaken Baby Syndrome—A Common Variant of Non-Accidental Head Injury in Infants. Dtsch. Arztebl. Int. 2009, 106, 211–217. [Google Scholar]
| No | Question | Type of Answer |
|---|---|---|
| 1 | What is the average occurrence rate of infantile colic in infants between the age of 0 and 5 months? | Numerical percentage |
| 2 | How would you estimate the burden for parents caused by infantile colic? | Selection of one of the pre-defined answers |
| 3 | How do you assess the association between maternal depression and infantile colic? | Selection of one of the pre-defined answers * |
| 4 | How do you assess the association between premature termination of breastfeeding and infantile colic? | Selection of one of the pre-defined answers * |
| 5 | Are you aware that infantile colic is a risk factor for the “shaken baby syndrome” in babies? | Selection of one of the pre-defined answers |
| 6 | What kind of treatments do you employ for the management of infantile colic? | Multiple selection of predefined answers and field for free-text answer |
| 7 | Are you interested in the topic of infantile colic? | Selection of one of the pre-defined answers |
| Type of Other Intervention | Number of Responders (% of Responders Who Declared the Use of Other Interventions) | |
|---|---|---|
| Germany (n = 60) | Poland (n = 37) | |
| Change of mother’s diet | None | 18 (48.6%) |
| Abdominal massage | 21 (35.0%) | 11 (29.7%) |
| Osteopathy | 14 (23.3%) | None |
| Warm compresses | None | 8 (21.6%) |
| Cumin preparations (incl. Carum carvi *) | 12 (20.0%) | none |
| Homeopathy | 7 (11.7%) | none |
| Tea (fennel, aniseed) | 7 (11.7%) | none |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sommermeyer, H.; Krauss, H.; Chęcińska-Maciejewska, Z.; Pszczola, M.; Piątek, J. Infantile Colic—The Perspective of German and Polish Pediatricians in 2020. Int. J. Environ. Res. Public Health 2020, 17, 7011. https://doi.org/10.3390/ijerph17197011
Sommermeyer H, Krauss H, Chęcińska-Maciejewska Z, Pszczola M, Piątek J. Infantile Colic—The Perspective of German and Polish Pediatricians in 2020. International Journal of Environmental Research and Public Health. 2020; 17(19):7011. https://doi.org/10.3390/ijerph17197011
Chicago/Turabian StyleSommermeyer, Henning, Hanna Krauss, Zuzanna Chęcińska-Maciejewska, Marcin Pszczola, and Jacek Piątek. 2020. "Infantile Colic—The Perspective of German and Polish Pediatricians in 2020" International Journal of Environmental Research and Public Health 17, no. 19: 7011. https://doi.org/10.3390/ijerph17197011





