Assessing the Impact of COVID-19 Public Health Stages on Paediatric Emergency Attendance
Abstract
1. Introduction
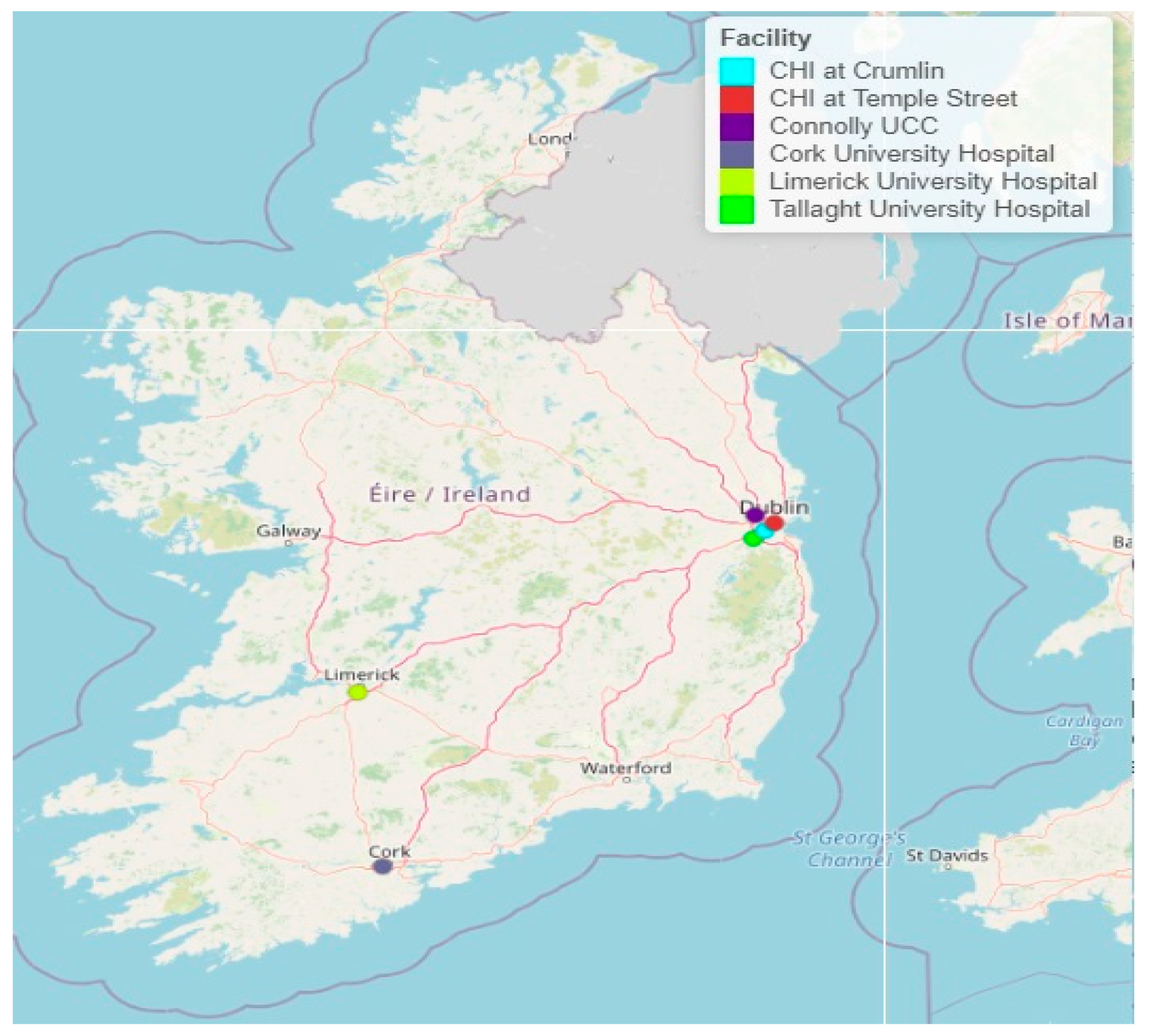
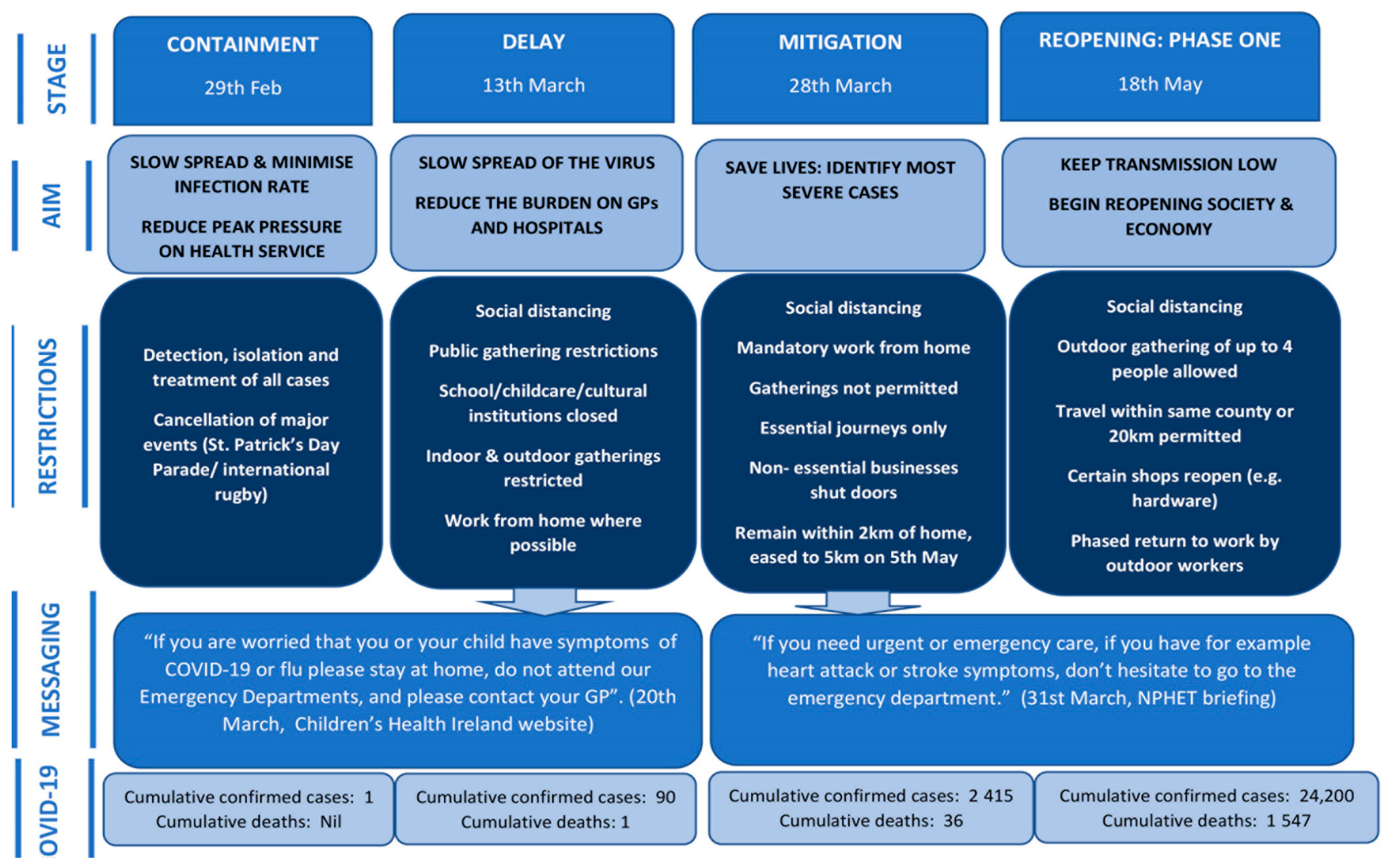
2. Materials and Methods
2.1. Data
2.2. Statistical Approach
2.3. Ethics
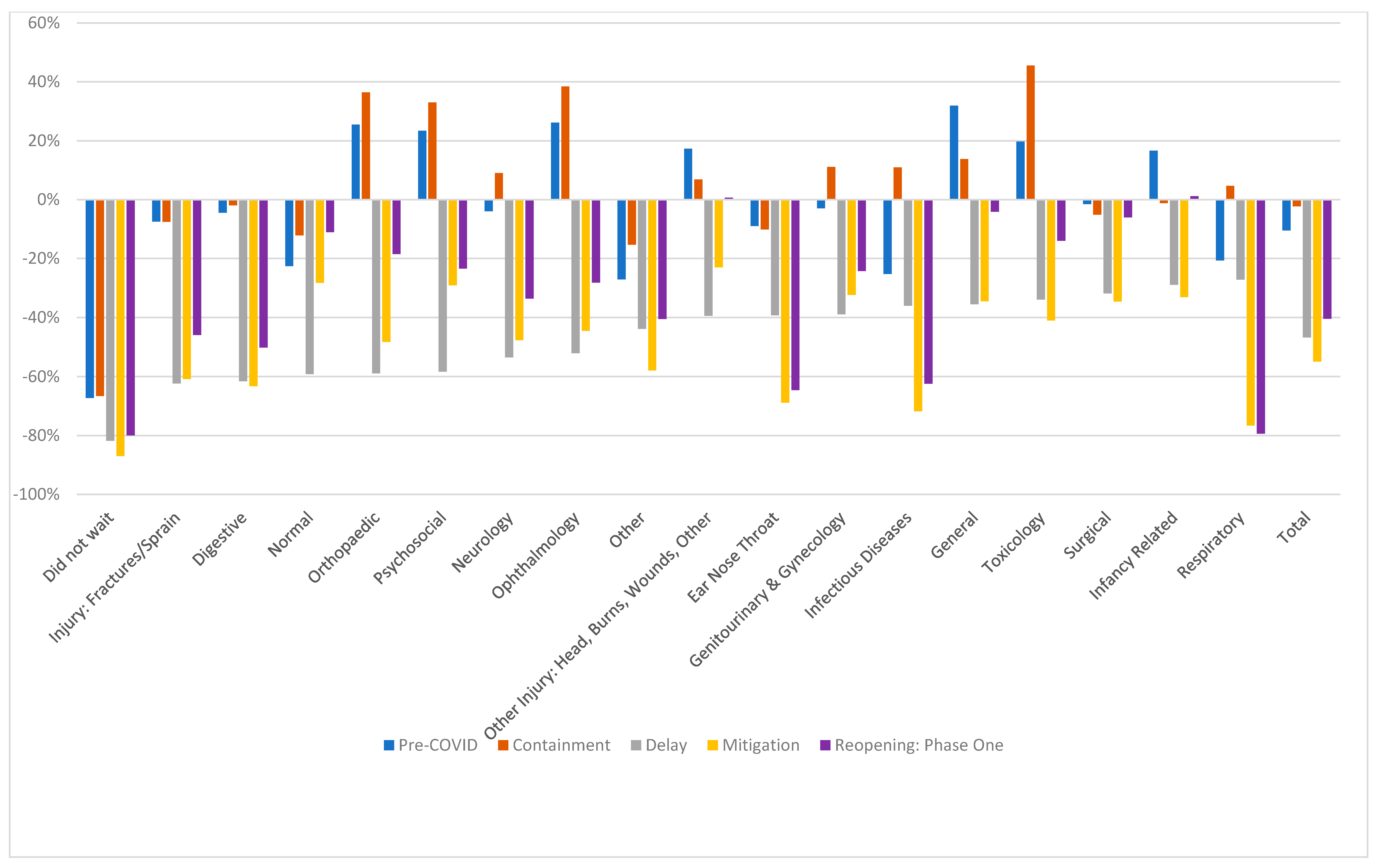
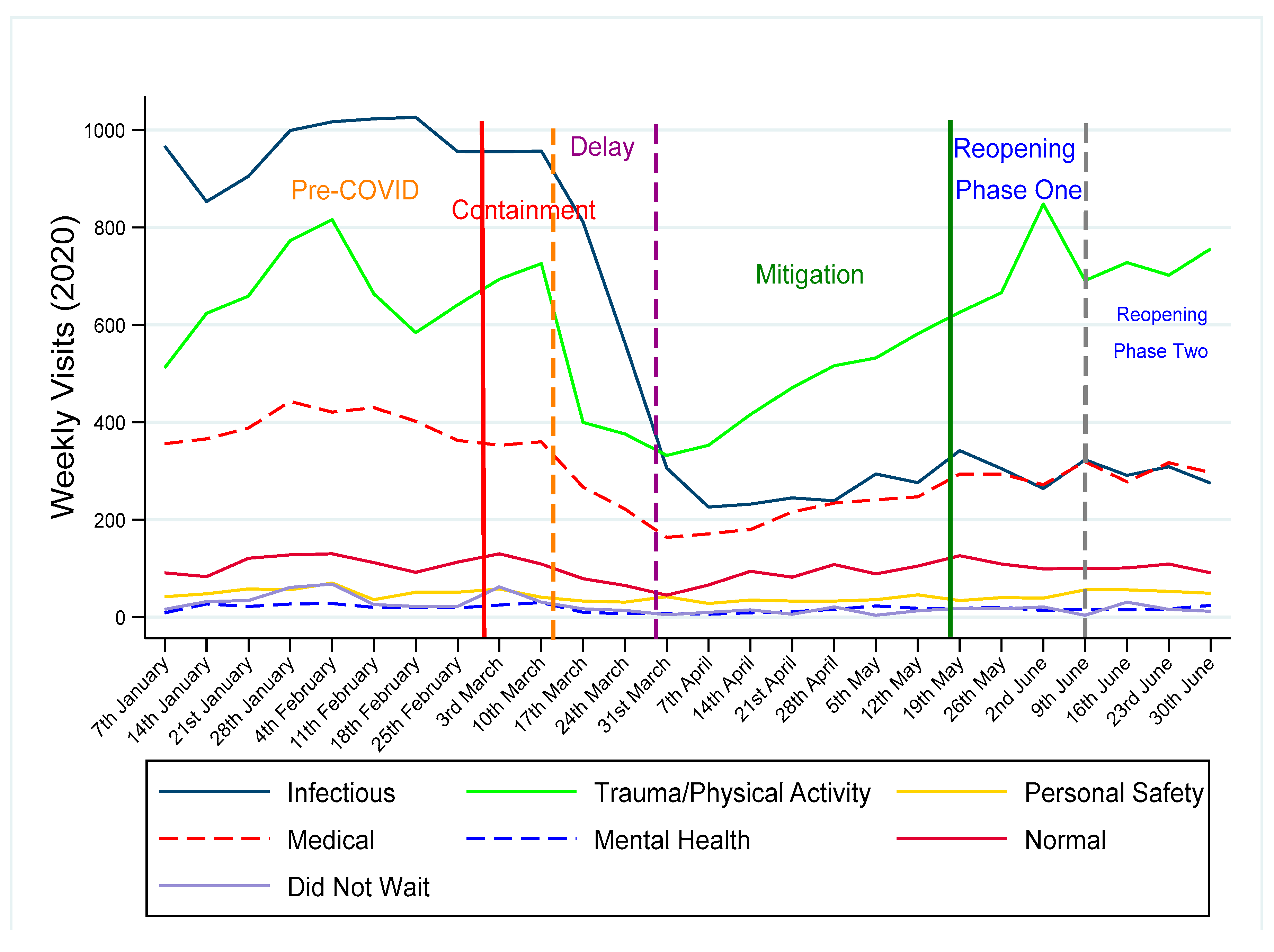
3. Results
4. Discussion
Implications for Policy and Practice
5. Limitations
6. Conclusions
7. Future Research
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
| Pre-COVID | Containment | Delay | Mitigation | Reopening: Phase One | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of days | 59 | 13 | 15 | 51 | 14 | ||||||||||
| 2020 | 2018/19 | % | 2020 | 2018/19 | % | 2020 | 2018/19 | % | 2020 | 2018/19 | % | 2020 | 2018/19 | % | |
| Did not wait | 5.1 | 15.7 | −67% | 5.6 | 16.8 | −67% | 2.1 | 11.7 | −82% | 1.6 | 12.3 | −87% | 2.6 | 13.2 | −80% |
| Injury: Fractures etc. | 47.5 | 51.3 | −7% | 50.5 | 54.7 | −8% | 24.5 | 65.0 | −62% | 31.2 | 79.6 | −61% | 50.1 | 92.6 | −46% |
| Digestive | 31.5 | 33.0 | −4% | 31.6 | 32.3 | −2% | 13.8 | 35.9 | −62% | 13.6 | 37.0 | −63% | 17.1 | 34.3 | −50% |
| Normal | 16.0 | 20.7 | −23% | 15.2 | 17.3 | −12% | 8.7 | 21.2 | −59% | 13.1 | 18.3 | −28% | 15.0 | 16.9 | −11% |
| Orthopaedic | 7.3 | 5.8 | 26% | 6.5 | 4.8 | 36% | 2.5 | 6.2 | −59% | 3.7 | 7.2 | −48% | 5.2 | 6.4 | −18% |
| Psychosocial | 3.1 | 2.5 | 23% | 3.8 | 2.8 | 33% | 1.0 | 2.4 | −58% | 2.0 | 2.8 | −29% | 2.6 | 3.4 | −23% |
| Neurology | 8.3 | 8.6 | −4% | 7.5 | 6.9 | 9% | 4.1 | 8.9 | −54% | 3.7 | 7.1 | −48% | 5.3 | 8.0 | −34% |
| Ophthalmology | 4.6 | 3.6 | 26% | 3.7 | 2.7 | 38% | 1.9 | 3.9 | −52% | 2.2 | 4.0 | −45% | 2.6 | 3.7 | −28% |
| Other | 5.1 | 7.0 | −27% | 4.7 | 5.5 | −15% | 3.2 | 5.7 | −44% | 2.7 | 6.5 | −58% | 3.7 | 6.3 | −41% |
| Other Injury | 42.5 | 36.2 | 17% | 41.3 | 38.7 | 7% | 25.8 | 42.6 | −39% | 35.2 | 45.7 | −23% | 52.0 | 51.7 | 1% |
| Ear Nose Throat | 21.3 | 23.4 | −9% | 20.3 | 22.6 | −10% | 13.9 | 22.8 | −39% | 7.4 | 23.7 | −69% | 8.1 | 22.8 | −65% |
| Genito/Gynaecology | 8.3 | 8.6 | −3% | 9.1 | 8.2 | 11% | 4.8 | 7.9 | −39% | 5.2 | 7.7 | −32% | 6.4 | 8.4 | −24% |
| Infectious Diseases | 37.1 | 49.6 | −25% | 34.8 | 31.4 | 11% | 20.7 | 32.3 | −36% | 7.5 | 26.7 | −72% | 10.7 | 28.5 | −62% |
| General | 10.4 | 7.9 | 32% | 7.5 | 6.6 | 14% | 4.5 | 7.0 | −36% | 4.9 | 7.5 | −35% | 7.5 | 7.8 | −4% |
| Toxicology | 2.8 | 2.4 | 20% | 3.2 | 2.2 | 46% | 2.3 | 3.5 | −34% | 1.5 | 2.6 | −41% | 2.4 | 2.8 | −14% |
| Dermatology | 10.6 | 10.0 | 6% | 8.3 | 9.2 | −9% | 6.5 | 9.8 | −34% | 5.6 | 10.0 | −44% | 7.6 | 10.2 | −26% |
| Surgical | 7.3 | 7.4 | −1% | 7.0 | 7.4 | −5% | 5.1 | 7.5 | −32% | 5.2 | 7.9 | −35% | 6.6 | 7.1 | −6% |
| Infancy Related | 2.8 | 2.4 | 17% | 2.9 | 3.0 | −1% | 2.1 | 3.0 | −29% | 1.9 | 2.9 | −33% | 3.0 | 3.0 | 1% |
| Respiratory | 49.8 | 62.8 | −21% | 46.3 | 44.3 | 5% | 38.8 | 53.3 | −27% | 9.7 | 41.3 | −77% | 7.4 | 35.6 | −79% |
| Total | 321.4 | 358.8 | −10% | 310.0 | 317.2 | −2% | 186.4 | 350.7 | −47% | 158.1 | 351.0 | −55% | 215.9 | 362.3 | −40% |
Appendix C
| Infectious | |
| Respiratory | Bronchitis, Bronchiolitis, Croup, Whooping cough, Asthma, Other Respiratory, Pneumonia, Cystic Fibrosis, Pneumothorax, Haemoptysis, Viral Induced Wheeze, Dyspnoea, Respiratory disorder, Respiratory arrest, Streptococcus pneumoniae, Pleurisy, LRTI, URTI, Pertussis, Wheezing, Stridor, Pleural Effusion, Hay Fever, Aspiration, Chronic Lung Disease |
| Ear Nose Throat | Labrynthitis, Tonsillitis, Rhinitis, Sinus infection, Tinnitus, Eustachian tube disorder, Tonsillar Haemorrhage, Epistaxis, Sinusitis, Quinsy, Cervical lymphadenitis, Stomatitis, Post op tonsillar bleed, Sleep apnoea, Pharyngitis, Disorder of ear, Perforated eardrum, Otitis media, Otitis Externa, Other ENT problem, Discharging ear, Nasal injury, Laryngomalacia, Mastoiditis, Laryngitis |
| Digestive | Abdominal Pain, intestinal infection, Disease of digestive system, Gastroenteritis, Anal Fissure, Bleeding P.R., Oesophagitis, Crohn’s Disease, Coeliac Disease, Constipation, Toddler’s Diarrhoea, Gastritis/enteritis, GORD, Gastro-oesophageal reflux, Threadworm, Haematemesis, Hepatitis, Inflammatory Bowel Disease, Disease of intestine, Ulcerative colitis, Viral intestinal infection, Liver disease, Acute pancreatitis, Haemorrhoids, Non-specific Abdominal Pain, Irritable bowel syndrome, Pancreatitis, Peptic Ulcer Disease, Cramp and spasm, Mesenteric Adenitis, Other G.I.T., Dysphagia |
| Infectious Disease | Tuberculosis, Scarlet fever, Haemophilus influenzae, Bacterial infection unspecified, Varicella, Measles, Influenza, Herpes, Gingivostomatitis, Mumps, Infectious mononucleosis, Other specified viral diseases, Viral infection, Candidiasis/Candida, Unspecified parasitic disease, Chicken Pox, Coxsackie disease, H1N1, Hand, Foot & Mouth Disease, Malaria, Viral Illness, Other, Infectious Disease, Parvovirus, Pertussis, Roseola, Meningococcal infection, Meningitis, Pyrexia of unknown origin (PUO), Fever without source/unspecified, Other Infection (various), Sepsis, Toxic Shock Syndrome |
| Trauma/Physical Activity | |
| Injury: Fracture/Sprain/Dislocation/Bruise | Fracture, Buckle Fracture, Bruise/Contusion/Haematoma, Amputation, Fingertip injury, Dislocation, Pulled Elbow, Query Fracture, Nail bed injury, Subungual Haematoma, Sprain, Toddler’s Fracture, Salter-Harris I/II/III/IV, Sprain/Soft Tissue Injury |
| Other Injury: Head Injury, Burns, Lacerations, Other | Concussion, Head Injury, Unspecified injury of head, Superficial injury of head, Trauma - Head/Brain, Abrasion, Change of Cast, Tooth Avulsion, Bite, Burn, Scald, Stab Wound, Dental Injury, Chest Injury, Crush Injury, Trauma, fracture of tooth, Genital Trauma, Gunshot wound, Wound, Insect bite, RTA, Erythema, Laceration, Multiple injuries, Other Injury, Change of POP, Pneumothorax—Traumatic, Puncture Wound, Superficial injury, Open wound, Needlestick injuries, Scratch wound, Sting, Sunburn, Removal of cast, Partial thickness burn |
| Orthopaedic | Apophysitis, Arthrosis, Back Pain, Baker’s cyst, Haemarthrosis, Discitis, Bursitis, Dysplastic/Dislocation Hip, Cauda Equina Syndrome, Irritable Hip, Joint Pain, Limp, Plantar Fasciitis, Severs Disease, Synovitis, Disc Herniation, Myalgia, Effusion of joint, Unspecified disorder of bone, Osgood Schlatter Disease, Osteomyelitis, Perthe’s Disease, Sacrococcygeal disorders, Other Orthopaedic Problem, Ganglion, Trigger thumb, Tendonitis, Slipped capital femoral epiphysis, Orthopaedic follow-up care, Anterior Knee pain |
| Personal Safety | |
| Toxicology | Accidental Alcohol Poisoning, Accidental Domestic Poisoning, Accidental Drugs Poisoning, Accidental Farming/Gardening Product Poisoning, Accidental Inhalation Poisoning, Accidental Other Poisoning, Accidental Paracetamol Ingestion, Alcohol Intoxication, Alcohol Withdrawal, Alcoholism, Amphetamine Overdose, Anti-convulsant Overdose, Anti-depressant Overdose, Aspirin Overdose, Carbon Monoxide Poisoning, Chemical Exposure, Deliberate Ingestion, Deliberate Inhalation, Food poisoning, Ingestion – Accidental, Inhalation Injury, Other Sedative Overdose, Other Toxicology, Sting Insect Venomous, Aminophenol derivatives, Nonopioid analgesic, Anaesthetic unspecified, Benzodiazepines, Other and unspecified drugs, Ethanol, Alcohol, Tricyclic Overdose, Noxious substance eaten, Cocaine, Tricyclic Overdose, Head Shop Products, Overdose, Other Toxicology, Opioids, Ingestion deliberate, Deliberate Other Poisoning |
| Child Protection/Assault | Abandoned Child, Social Problems, Alleged/Possible CSA, Alleged/Possible NAI, Sexual abuse, Alleged Assault, Physical Assault, Rape/Sexual Assault |
| Foreign Body | Foreign Body, Ingested Foreign Body, Foreign body in genitourinary, Foreign body in cornea, Surgical Foreign Body, ENT Foreign Body |
| Medical | |
| Dermatology | Cellulitis, Eczema, warts, Scabies, Dermatitis, Other dermatology problem, Verruca, Erythema Multiforme, Herpes, Adverse Drug Reaction, Urticaria, Haemangioma, Molluscum contagiosum, Impetigo, Viral exanthem, Paronychia, Psoriasis, Rash, Shingles, Scalded Skin Syndrome, Steven Johnson, Nail disorder, Tinea |
| Cardiac/Vascular | Palpitations, Cardiac Arrest, Cardiac Arrhythmia, Heart Failure, Heart Murmur, Hypertension, Pulmonary Embolism, S.V.T./Supraventricular tachycardia, Bradycardia, Cardiac other, Congenital heart disease, Congestive Heart Disease, Congestive Heart Failure, Tachycardia |
| Endocrine/Metabolic | Known Addison’s Disease, DM 1 DKA, DM 1 with Hyperglycaemia, DM 1 with Hypoglycaemia, DM Known DKA, DM Known Hypoglycaemia, DM New DKA, DM New Hyperglycaemia, DM New Hypoglycaemia, Known Diabetes Insipidus, Diabetes Mellitus, Hypoglycaemia, Hypercalcaemia, Hypernatraemia, Other Endocrine, Thyrotoxicosis, Disorder of adrenal gland, Metabolic disorder, Fatty Acid Oxidation Disorder, Congenital Adrenal Hyperplasia, Galactosaemia, Hyperinsulism, Metabolic disease, Mitochondrial Disorder Other, Metabolic Storage Disorder, Urea Cycle Defect |
| General/Rheumatology | General Collapse, Nut Allergy, Egg Allergy, Fish Allergy, Allergic Reaction, Anaphylaxis, Other General, Costochondritis, Collapse, Apnoea, Dehydration, Dental, Nausea and vomiting, Vaccination, Faint (vasovagal episode), Chest Pain, Faint (vasovagal episode), Enlarged lymph nodes, Temporomandibular joint disorder, Gingivo Stomatitis, Arthritis, Hyperventilation, Hypothermia, Kawasaki Disease, Torticollis, Mouth Ulcers, Myositis, Oedema, Unspecified soft tissue disorder, Other General, Syncope, Osteoarthritis |
| Haematology/Oncology | Anaemia, Bleeding disorder, Henoch Schonlein Purpura, Leukaemia, Sickle-cell disorders, Allergic purpura, Agranulocytosis, Idiopathic thrombocytopenic, Thrombocytopenia, Haemoglobinopathy, Space Occupying Lesion/Tumour, ITP, Other Haematology, Haemophilia, Clotting Disorder, Neutropenia, Acquired haemolytic anaemia, Lymphadenopathy, Neoplasm, Oncology/Malignancy, Tumour |
| Genitourinary & Gynecology | Nephrotic, Haematuria, Renal Colic, Hydrocele, Injury of kidney, Glomerulonephritis, Pyelonephritis, Haemolytic Uraemic Syndrome, Nephrotic syndrome, Calculus of kidney/ureter, Disorder of kidney and ureter, Cystitis, Unspecified renal colic, Urinary tract infection, Dysmenorrhoea, Retention of urine, Dysuria, Other Renal Problem, Pyelonephritis, Epididymo-Orchitis, Renal Failure, Renal Stones, epididymitis, Testicular dysfunction, urethritis, Ovarian dysfunction, Menorrhagia, Disorder of penis unspecified, Disorder of male genital organ, Disorder of breast, Acute vaginitis, Irregular menstruation, Mittelschmerz, Vulvovaginitis, Vaginal Bleed, Other Obstetrics & Gynaecology, Ovarian Cyst |
| Ophthalmology | Conjunctivitis, Hordeolum, Corneal Abrasion, Inflammation of eyelid, Disorder of globe, inflammation of orbit, Diplopia, Disorder of eyelid, Disorder of cornea, Burn of eye and adnexa, Blindness, Hyphaema, Visual disturbance, Disorder of eye and adnexa, Orbital cellulitis, Other Opthalmology, Injury of eye and orbit, Peri-orbital cellulitis, Injury of conjunctiva, Subconjunctival Haemorrhage |
| Neurology | Afebrile Convulsion, Disorder of visual pathways, Bell’s Palsy, Cerebral Palsy, Mononeuropathy, Confusional Episode, Convulsion -febrile, Encephalitis, Facial Palsy, Febrile Seizures, Epilepsy, Migraine, Transient ischaemic attack, headache, Cranial nerve disorder, Intracerebral haemorrhage, Neurodegenerative disease, Intracranial Bleed, Neurology Collapse, Non-Specific Seizure, Other Neurology, Dizziness and giddiness, Injury of unspecified nerve, Febrile Convulsion, Status Epilepticus, Transverse Myelitis, Ataxia, Neuralgia, Weakness/Paralysis, Subarachnoid Haemorrhage, Subdural Haemorrhage, Seizure, Other and unspecified speech, Disorientation, Peripheral neuropathy, Paraesthesia, Intracerebral haemorrhage, Neurodegenerative disease, Coma, Cranial nerve disorder |
| Surgical | Abscess, Appendicitis, Balanitis, Pyloric stenosis, Bartholin’s Abscess, Dental Abscess, Lump, Epididymitis, VP Shunt, Hernia, Ingrown toenail, Cutaneous abscess, Intussusception, Malrotation, Anal abscess, Bowel Obstruction, Lump/swelling, Vascular disorder of intestine, Acute abdomen, Torsion of testis, Volvulus, Redundant prepuce phimosis, Unspecified lump in breast, Other Surgical, Paraphimosis, Peg tube problem, Phimosis, Cholecystitis, Post Op Problem, Post-op complication, Pyloric Stenosis, Localised swelling mass, Open wound of scrotum and testes, Surgical Abscess, Undescended Testes, Surgical Wound Infection, Torsion Hydatid, Torsion Testes |
| Infancy Related | Benign neonatal rash, Breast Feeding Jaundice, Umbilical hernia, Colic, Jaundice, Milia, Neonatal Acne, Other Neonatology, Umbilical Granuloma, Snuffle, Head Circumference/Fontanelle, Erythema toxicum, Cephalhaematoma, Teething syndrome, A.L.T.E. ( BRUE), Breath holding spells, Cow’s Milk Allergy/Protein intolerance, Failure to Thrive, Feeding Difficulty/Feeding Problems |
| Mental Health | |
| Psychosocial | Anorexia Nervosa, Anxiety disorder, Deliberate self- harm, Depression, Mental and behavioural disorder, Unspecified mood, Panic disorder, Acute and transient psychotic disorder, Mixed anxiety and depressive, Adjustment Disorder, Somatoform disorder, Dissociative disorder, Acute reaction to stress, Neurotic disorder, Eating disorder, Conduct disorder, Mental disorder, Personality disorder, Other Psychiatric, Psychosis |
| Chronic Complex Conditions (reported above) | |
| Cystic Fibrosis, Tumour, Space Occupying Lesion/Tumour, Oncology/Malignancy, Diabetes Mellitus, Known Addison’s Disease, DM 1 DKA, DM 1 with Hyperglycaemia, DM 1 with Hypoglycaemia, DM Known DKA, DM Known Hypoglycaemia, DM New DKA, DM New Hyperglycaemia, DM New Hypoglycaemia, Known Diabetes Insipidus, Crohn’s Disease, Coeliac Disease, Ulcerative colitis, Sickle-cell disorders, Haemoglobinopathy, Neoplasm, Leukaemia, Inflammatory Bowel Disease | |
References
- Brick, A.; Walsh, B.; Keegan, C.; Lyons, S. COVID-19 and emergency department attendances in Irish public hospitals. ESRI Special Article 2020. [Google Scholar] [CrossRef]
- Thornton, J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ 2020, 369, m1401. [Google Scholar] [CrossRef] [PubMed]
- Bressan, S.; Buonsenso, D.; Farrugia, R.; Parri, N.; Oostenbrink, R.; Titomanlio, L.; Roland, D.; Nijman, R.G.; Maconochie, I.; Da Dalt, L.; et al. Preparedness and response to Pediatric CoVID-19 in European Emergency Departments: A survey of the REPEM and PERUKI networks. Ann. Emerg. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Scaramuzza, A.; Tagliaferri, F.; Bonetti, L.; Soliani, M.; Morotti, F.; Bellone, S.; Cavalli, C.; Rabbone, I. Changing admission patterns in paediatric emergency departments during the COVID-19 pandemic. Arch. Dis. Child. 2020, 105, 704–706. [Google Scholar] [CrossRef]
- Dann, L.; Fitzsimons, J.; Gorman, K.M.; Hourihane, J.; Okafor, I. Disappearing act: COVID-19 and paediatric emergency department attendances. Arch. Dis. Child. 2020, 105, 810–811. [Google Scholar] [CrossRef] [PubMed]
- Santana, R.; Sousa, J.S.; Soares, P.; Lopes, S.; Boto, P.; Rocha, J.V. The Demand for Hospital Emergency Services: Trends during the First Month of COVID-19 Response. Port. J. Public Health 2020, 38, 30–36. [Google Scholar] [CrossRef]
- Mitchell, R.; O’Reilly, G.; Mitra, B.; Smit, D.V.; Miller, J.; Cameron, P.A. Impact of COVID -19 State of Emergency restrictions on presentations to two Victorian emergency departments. Emerg. Med. Australas. 2020. [Google Scholar] [CrossRef]
- Isba, R.; Edge, R.; Jenner, R.; Broughton, E.; Francis, N.; Butler, J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch. Dis. Child. 2020, 105, 704. [Google Scholar] [CrossRef]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Jang, W.M.; Cho, S.; Jang, D.H.; Kim, U.-N.; Jung, H.; Lee, J.Y.; Eun, S.J. Preventive Behavioral Responses to the 2015 Middle East Respiratory Syndrome Coronavirus Outbreak in Korea. Int. J. Environ. Res. Public Health 2019, 16, 2161. [Google Scholar] [CrossRef]
- Jeong, H.; Jeong, S.; Oh, J.; Woo, S.H.; So, B.H.; Wee, J.H.; Kim, J.H.; Im, J.Y.; Choi, S.P.; Park, K.; et al. Impact of Middle East respiratory syndrome outbreak on the use of emergency medical resources in febrile patients. Clin. Exp. Emerg. Med. 2017, 4, 94–101. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, S.Y.; Khang, Y.-H.; Lim, H.-K. Impact of the 2015 Middle East Respiratory Syndrome Outbreak on Emergency Care Utilization and Mortality in South Korea. Yonsei Med. J. 2019, 60, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.-J.; Huang, N.; Lee, C.-H.; Hsu, Y.-J.; Hsieh, C.-J.; Chou, Y.-J. The Impact of the SARS Epidemic on the Utilization of Medical Services: SARS and the Fear of SARS. Am. J. Public Health 2004, 94, 562–564. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.T.; Griffiths, S.; Choi, K.C.; Tsui, H.Y. Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect. Dis. 2010, 10, 139–151. [Google Scholar] [CrossRef]
- Roland, D.; Munro, A. Covid-19 in Children: Develop Solutions Rather than Look for Problems. The BMJ Opinion. 2020. Available online: https://blogs.bmj.com/bmj/2020/06/12/covid-19-in-children-develop-solutions-rather-than-look-for-problems/ (accessed on 15 July 2020).
- Department of Health: Health in Ireland, Key Trends. 2019. Available online: https://www.gov.ie/en/publication/f1bb64-health-in-ireland-key-trends-2019/ (accessed on 15 July 2020).
- Smith, S.; Walsh, B.; Wren, M.-A.; Barron, S.; Morgenroth, E.; Eighan, J.; Lyons, S. Geographic profile of healthcare needs and non-acute healthcare supply in Ireland; Economic and Social Research Institute. 2019. Available online: https://www.esri.ie/pubs/RS90.pdf (accessed on 15 July 2020).
- Smyth, B.; Marsden, P.; Donohue, F.; Kavanagh, P.; Kitching, A.; Feely, E.; Collins, L.; Cullen, L.; Sheridan, A.; Evans, D.; et al. Planning for Health: Trends and Priorities to Inform Health Service Planning 2017. Report from the Health Service Executive. 2017. Available online: https://www.lenus.ie/handle/10147/621262 (accessed on 15 July 2020).
- WHO. International Classifications of Disease. Available online: https://www.who.int/classifications/icd/en/ (accessed on 15 July 2020).
- Bennett, M.; Vecchia, C.D.; Blackburn, C.; Walsh, S.; Barrett, M. Too old for a paediatric emergency department? It’s complex. Ir. J. Med Sci. 2020, 1–5. [Google Scholar] [CrossRef]
- Nicholson, E.; McDonnell, T.; De Brún, A.; Barrett, M.; Bury, G.; Collins, C.; Hensey, C.; McAuliffe, E. Factors that influence family and parental preferences and decision making for unscheduled paediatric healthcare–systematic review. BMC Health Serv. Res. 2020, 20, 1–23. [Google Scholar] [CrossRef]
- Coster, J.E.; Turner, J.K.; Bradbury, D.; Cantrell, A. Why Do People Choose Emergency and Urgent Care Services? A Rapid Review Utilizing a Systematic Literature Search and Narrative Synthesis. Acad. Emerg. Med. 2017, 24, 1137–1149. [Google Scholar] [CrossRef]
- Nicholson, E.; McDonnell, T.; Conlon, C.; Barrett, M.; Cummins, F.; Hensey, C.; McAuliffe, E. Understanding the Impact of Public Health Advice on Paediatric Healthcare Use During COVID-19: A Cross-sectional Survey of Parents. 2020. In Press. Available online: https://www.researchsquare.com/article/rs-56016/v1 (accessed on 1 September 2020). [CrossRef]
- Influenza Surveillance in Ireland—Weekly Report. Influenza Week 22 2020. Health Protection Surveillance Centre, HSE, 2020. Available online: https://www.hpsc.ie/az/respiratory/influenza/seasonalinfluenza/surveillance/influenzasurveillancereports/20192020season/ (accessed on 15 July 2020).
- Government of Ireland. COVID-19 Health Surveillance Monitor (Ireland). 2020. Available online: https://covid19ireland-geohive.hub.arcgis.com/ (accessed on 15 July 2020).
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health 2020, 14, 1–11. [Google Scholar] [CrossRef]
- Benahmed, N.; Laokri, S.; Zhang, W.-H.; Verhaeghe, N.; Trybou, J.; Cohen, L.; De Wever, A.; Alexander, S. Determinants of nonurgent use of the emergency department for pediatric patients in 12 hospitals in Belgium. Eur. J. Nucl. Med. Mol. Imaging 2012, 171, 1829–1837. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Health, United States, 2015. Available online: http://www.cdc.gov/nchs/data/hus/hus15.pdf (accessed on 15 July 2020).
- McDonnell, T.; McAuliffe, E.; Barrett, M.; Conlon, C.; Cummins, F.; Deasy, C.; Hensey, C.; Martin, C.; Nicholson, E. CUPID COVID-19: Emergency department attendance by paediatric patients during COVID-19—Project protocol. HRB Open Res. 2020, 3, 37. [Google Scholar] [CrossRef]
- McAuliffe, E.; Hamza, M.; McDonnell, T.; Nicholson, E.; De Brún, A.; Barrett, M.; Brunsdon, C.; Bury, G.; Collins, C.; Deasy, C.; et al. Children’s unscheduled primary and emergency care in Ireland: A multimethod approach to understanding decision making, trends, outcomes and parental perspectives (CUPID): Project protocol. BMJ Open 2020, 10, e036729. [Google Scholar] [CrossRef] [PubMed]
- Chanchlani, N.; Buchanan, F.; Gill, P.J. Addressing the indirect effects of COVID-19 on the health of children and young people. Can. Med. Assoc. J. 2020, 192, E921–E927. [Google Scholar] [CrossRef] [PubMed]
| Pre-COVID | Containment | Delay | Mitigation | Reopening: Phase One | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Date from | 01/01/2020 | 29/02/2020 | 13/03/2020 | 28/03/2020 | 18/05/2020 | ||||||||||
| Date to | 28/02/2020 | 12/03/2020 | 27/03/2020 | 17/05/2020 | 31/05/2020 | ||||||||||
| Number of Days | 59 | 13 | 15 | 51 | 14 | ||||||||||
| Daily Visits | % | % | % | % | % | ||||||||||
| Observed Mean | 396 | 100% | 370 | 100% | 232 | 100% | 195 | 100% | 257 | 100% | |||||
| Prior Years Mean | 444 | 100% | 396 | 100% | 435 | 100% | 435 | 100% | 450 | 100% | |||||
| IRR | 0.93 | 0.93 | 0.58 | 0.46 | 0.58 | ||||||||||
| Confidence Interval | 0.89 | 0.98 | 0.85 | 1.01 | 0.54 | 0.64 | 0.44 | 0.49 | 0.53 | 0.63 | |||||
| p-value | 0.004 | 0.086 | 0.000 | 0.000 | 0.000 | ||||||||||
| GP Referrals | |||||||||||||||
| Observed Mean | 133 | 34% | 115 | 31% | 49 | 21% | 42 | 21% | 54 | 21% | |||||
| Prior Years Mean | 157 | 35% | 131 | 31% | 149 | 34% | 140 | 32% | 143 | 32% | |||||
| IRR | 0.88 | 0.85 | 0.37 | 0.30 | 0.38 | ||||||||||
| Confidence Interval | 0.78 | 0.99 | 0.69 | 1.07 | 0.30 | 0.46 | 0.26 | 0.34 | 0.31 | 0.47 | |||||
| p-value | 0.033 | 0.163 | 0.000 | 0.000 | 0.000 | ||||||||||
| Admitted | |||||||||||||||
| Observed Mean | 57 | 14% | 54 | 15% | 34 | 15% | 29 | 15% | 36 | 14% | |||||
| Prior Years Mean | 63 | 14% | 60 | 14% | 64 | 15% | 62 | 14% | 64 | 14% | |||||
| IRR | 0.92 | 0.89 | 0.55 | 0.46 | 0.57 | ||||||||||
| Confidence Interval | 0.86 | 0.97 | 0.79 | 0.99 | 0.49 | 0.62 | 0.43 | 0.49 | 0.51 | 0.64 | |||||
| p-value | 0.004 | 0.030 | 0.000 | 0.000 | 0.000 | ||||||||||
| Triage urgent (score 1 or 2) | |||||||||||||||
| Observed Mean | 85 | 21% | 78 | 21% | 47 | 20% | 38 | 19% | 53 | 20% | |||||
| Prior Years Mean | 91 | 20% | 80 | 19% | 88 | 20% | 87 | 20% | 88 | 19% | |||||
| IRR | 0.97 | 0.95 | 0.58 | 0.44 | 0.60 | ||||||||||
| Confidence Interval | 0.91 | 1.03 | 0.85 | 1.06 | 0.52 | 0.65 | 0.41 | 0.48 | 0.54 | 0.68 | |||||
| p-value | 0.255 | 0.340 | 0.000 | 0.000 | 0.000 | ||||||||||
| Triage low urgency (score 4 or 5) | |||||||||||||||
| Observed Mean | 150 | 38% | 146 | 40% | 90 | 39% | 77 | 39% | 105 | 41% | |||||
| Prior Years Mean | 164 | 37% | 150 | 35% | 164 | 38% | 173 | 40% | 184 | 41% | |||||
| IRR | 0.97 | 0.98 | 0.61 | 0.46 | 0.58 | ||||||||||
| Confidence Interval | 0.91 | 1.03 | 0.88 | 1.10 | 0.54 | 0.68 | 0.43 | 0.50 | 0.52 | 0.65 | |||||
| p-value | 0.328 | 0.781 | 0.000 | 0.000 | 0.000 | ||||||||||
| Arrival by ambulance | |||||||||||||||
| Observed Mean | 24 | 6% | 26 | 7% | 18 | 8% | 12 | 6% | 14 | 5% | |||||
| Prior Years Mean | 25 | 6% | 24 | 5% | 25 | 6% | 23 | 5% | 26 | 6% | |||||
| IRR | 1.13 | 1.25 | 0.87 | 0.58 | 0.63 | ||||||||||
| Confidence Interval | 1.05 | 1.22 | 1.10 | 1.42 | 0.76 | 1.00 | 0.53 | 0.64 | 0.53 | 0.73 | |||||
| p-value | 0.002 | 0.001 | 0.057 | 0.000 | 0.000 | ||||||||||
| Other statistics | n | Std Dev | n | Std Dev | n | Std Dev | n | Std Dev | n | Std Dev | |||||
| ICU admissions in period (actual) | 34 | 11 | 10 | 20 | 4 | ||||||||||
| ICU admissions per day (mean) | 0.6 | 0.6 | 0.8 | 0.8 | 0.7 | 0.6 | 0.4 | 0.6 | 0.3 | 0.5 | |||||
| Age category (% proportion) | |||||||||||||||
| Under 2 | 107 | 16 | 27% | 93 | 13 | 25% | 76 | 13 | 33% | 55 | 9 | 28% | 63 | 11 | 25% |
| Age 2 to 5 | 86 | 12 | 22% | 81 | 9 | 22% | 59 | 13 | 25% | 45 | 9 | 23% | 50 | 6 | 19% |
| Age 5 to 12 | 130 | 29 | 33% | 122 | 24 | 33% | 71 | 14 | 31% | 66 | 15 | 34% | 95 | 17 | 37% |
| Age 13 to 15 | 74 | 21 | 19% | 74 | 22 | 20% | 27 | 8 | 12% | 29 | 9 | 15% | 49 | 8 | 19% |
| Pre-COVID | Containment | Delay | Mitigation | Reopening: Phase One | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Date from | 01/01/2020 | 29/02/2020 | 13/03/2020 | 28/03/2020 | 18/05/2020 | ||||||||||
| Date to | 28/02/2020 | 12/03/2020 | 27/03/2020 | 17/05/2020 | 31/05/2020 | ||||||||||
| Number of Days | 59 | 13 | 15 | 51 | 14 | ||||||||||
| Daily Visits | % | % | % | % | % | ||||||||||
| Observed Mean | 321 | 100% | 310 | 100% | 186 | 100% | 158 | 100% | 216 | 100% | |||||
| Prior Years Mean | 359 | 100% | 317 | 100% | 351 | 100% | 351 | 100% | 362 | 100% | |||||
| IRR | 0.94 | 0.97 | 0.59 | 0.47 | 0.60 | ||||||||||
| Confidence Interval | 0.89 | 0.99 | 0.88 | 1.06 | 0.54 | 0.64 | 0.44 | 0.49 | 0.55 | 0.66 | |||||
| p-value | 0.013 | 0.522 | 0.000 | 0.000 | 0.000 | ||||||||||
| GP referral | |||||||||||||||
| Observed Mean | 89 | 28% | 80 | 26% | 32 | 17% | 25 | 16% | 36 | 17% | |||||
| Prior Years Mean | 105 | 29% | 88 | 25% | 100 | 28% | 95 | 27% | 95 | 26% | |||||
| IRR | 0.88 | 0.89 | 0.36 | 0.28 | 0.37 | ||||||||||
| Confidence Interval | 0.76 | 1.02 | 0.68 | 1.17 | 0.27 | 0.47 | 0.23 | 0.32 | 0.28 | 0.49 | |||||
| p-value | 0.097 | 0.417 | 0.000 | 0.000 | 0.000 | ||||||||||
| Admitted | |||||||||||||||
| Observed Mean | 37 | 12% | 37 | 12% | 21 | 11% | 18 | 11% | 23 | 11% | |||||
| Prior Years Mean | 43 | 12% | 42 | 12% | 43 | 12% | 42 | 12% | 43 | 12% | |||||
| IRR | 0.86 | 0.88 | 0.50 | 0.42 | 0.52 | ||||||||||
| Confidence Interval | 0.80 | 0.92 | 0.78 | 1.00 | 0.43 | 0.57 | 0.38 | 0.45 | 0.45 | 0.59 | |||||
| p-value | 0.000 | 0.045 | 0.000 | 0.000 | 0.000 | ||||||||||
| Triage urgent (score 1 or 2) | |||||||||||||||
| Observed Mean | 64 | 20% | 60 | 19% | 37 | 20% | 30 | 19% | 43 | 20% | |||||
| Prior Years Mean | 70 | 19% | 61 | 18% | 68 | 19% | 66 | 19% | 67 | 18% | |||||
| IRR | 0.95 | 0.95 | 0.59 | 0.46 | 0.64 | ||||||||||
| Confidence Interval | 0.89 | 1.02 | 0.84 | 1.07 | 0.52 | 0.67 | 0.43 | 0.50 | 0.56 | 0.50 | |||||
| p-value | 0.142 | 0.413 | 0.000 | 0.000 | 0.000 | ||||||||||
| Triage low urgency (score 4 or 5) | |||||||||||||||
| Observed Mean | 141 | 44% | 140 | 45% | 83 | 44% | 71 | 45% | 99 | 46% | |||||
| Prior Years Mean | 153 | 43% | 139 | 41% | 155 | 44% | 162 | 46% | 171 | 47% | |||||
| IRR | 0.97 | 1.00 | 0.59 | 0.45 | 0.59 | ||||||||||
| Confidence Interval | 0.91 | 1.03 | 0.89 | 1.13 | 0.53 | 0.67 | 0.42 | 0.49 | 0.52 | 0.66 | |||||
| p-value | 0.320 | 0.939 | 0.000 | 0.000 | 0.000 | ||||||||||
| Arrival by ambulance | |||||||||||||||
| Observed Mean | 18 | 6% | 19 | 6% | 13 | 7% | 9 | 6% | 12 | 5% | |||||
| Prior Years Mean | 18 | 5% | 16 | 5% | 17 | 5% | 17 | 5% | 18 | 5% | |||||
| IRR | 1.20 | 1.37 | 0.94 | 0.66 | 0.74 | ||||||||||
| Confidence Interval | 1.10 | 1.30 | 1.18 | 1.59 | 0.80 | 1.11 | 0.60 | 0.74 | 0.62 | 0.88 | |||||
| p-value | 0.000 | 0.000 | 0.478 | 0.000 | 0.001 | ||||||||||
| Age category (% proportion) | Std Dev | Std Dev | Std Dev | Std Dev | Std Dev | ||||||||||
| Under 2 | 86 | 13 | 27% | 78 | 12 | 25% | 61 | 12 | 33% | 44 | 9 | 28% | 52 | 10 | 24% |
| Age 2 to 5 | 69 | 10 | 22% | 67 | 7 | 22% | 47 | 11 | 25% | 36 | 8 | 23% | 42 | 5 | 19% |
| Age 5 to 12 | 107 | 25 | 33% | 102 | 21 | 33% | 58 | 14 | 31% | 54 | 14 | 34% | 83 | 16 | 38% |
| Age 13 to 15 | 60 | 18 | 19% | 63 | 17 | 20% | 22 | 7 | 12% | 22 | 9 | 15% | 40 | 7 | 18% |
| Pre-COVID | Containment | Delay | Mitigation | Reopening: Phase One | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Date from | 01/01/2020 | 29/02/2020 | 13/03/2020 | 28/03/2020 | 18/05/2020 | ||||||||||
| Date to | 28/02/2020 | 12/03/2020 | 27/03/2020 | 17/05/2020 | 31/05/2020 | ||||||||||
| Number of Days | 59 | 13 | 15 | 51 | 14 | ||||||||||
| Daily Visits | % | % | % | % | % | ||||||||||
| Observed Mean | 75 | 100% | 60 | 100% | 46 | 100% | 37 | 100% | 41 | 100% | |||||
| Prior Years Mean | 85 | 100% | 79 | 100% | 85 | 100% | 84 | 100% | 88 | 100% | |||||
| IRR | 0.91 | 0.75 | 0.57 | 0.45 | 0.50 | ||||||||||
| Confidence Interval | 0.86 | 0.96 | 0.67 | 0.83 | 0.52 | 0.64 | 0.42 | 0.48 | 0.44 | 0.56 | |||||
| p-value | 0.001 | 0.000 | 0.000 | 0.000 | 0.000 | ||||||||||
| GP Referrals | |||||||||||||||
| Observed Mean | 44 | 59% | 35 | 59% | 17 | 38% | 16 | 44% | 18 | 44% | |||||
| Prior Years Mean | 52 | 61% | 44 | 51% | 49 | 58% | 46 | 55% | 48 | 55% | |||||
| IRR | 0.87 | 0.77 | 0.39 | 0.35 | 0.40 | ||||||||||
| Confidence Interval | 0.79 | 0.94 | 0.66 | 0.91 | 0.32 | 0.46 | 0.31 | 0.39 | 0.33 | 0.48 | |||||
| p-value | 0.001 | 0.002 | 0.000 | 0.000 | 0.000 | ||||||||||
| Admitted | |||||||||||||||
| Observed Mean | 20 | 27% | 17 | 29% | 13 | 28% | 11 | 29% | 13 | 32% | |||||
| Prior Years Mean | 20 | 24% | 19 | 22% | 21 | 25% | 19 | 23% | 21 | 24% | |||||
| IRR | 1.04 | 0.90 | 0.68 | 0.56 | 0.69 | ||||||||||
| Confidence Interval | 0.96 | 1.14 | 0.77 | 1.05 | 0.57 | 0.80 | 0.51 | 0.62 | 0.58 | 0.62 | |||||
| p-value | 0.318 | 0.189 | 0.000 | 0.000 | 0.000 | ||||||||||
| Triage urgent (score 1 or 2) | |||||||||||||||
| Observed Mean | 20 | 27% | 18 | 30% | 10 | 23% | 8 | 22% | 10 | 24% | |||||
| Prior Years Mean | 21 | 25% | 19 | 22% | 20 | 23% | 21 | 25% | 21 | 24% | |||||
| IRR | 1.01 | 0.93 | 0.56 | 0.39 | 0.50 | ||||||||||
| Confidence Interval | 0.93 | 1.10 | 0.79 | 1.10 | 0.46 | 0.67 | 0.35 | 0.44 | 0.41 | 0.61 | |||||
| p-value | 0.784 | 0.420 | 0.000 | 0.000 | 0.000 | ||||||||||
| Triage low urgency (score 4 or 5) | |||||||||||||||
| Observed Mean | 10 | 13% | 6 | 11% | 7 | 16% | 6 | 16% | 6 | 14% | |||||
| Prior Years Mean | 11 | 13% | 11 | 12% | 10 | 11% | 11 | 13% | 13 | 15% | |||||
| IRR | 0.98 | 0.68 | 0.76 | 0.57 | 0.53 | ||||||||||
| Confidence Interval | 0.85 | 1.13 | 0.51 | 0.90 | 0.59 | 1.00 | 0.49 | 0.67 | 0.39 | 0.70 | |||||
| p-value | 0.769 | 0.008 | 0.046 | 0.000 | 0.000 | ||||||||||
| Arrival by ambulance | |||||||||||||||
| Observed Mean | 7 | 9% | 7 | 12% | 6 | 12% | 3 | 8% | 3 | 6% | |||||
| Prior Years Mean | 7 | 8% | 7 | 8% | 8 | 9% | 7 | 8% | 8 | 9% | |||||
| IRR | 0.98 | 1.00 | 0.78 | 0.45 | 0.37 | ||||||||||
| Confidence Interval | 0.85 | 1.12 | 0.79 | 1.28 | 0.60 | 1.01 | 0.37 | 0.55 | 0.26 | 0.52 | |||||
| p-value | 0.77 | 0.98 | 0.06 | 0.00 | 0.00 | ||||||||||
| Age category (% proportion) | n | Std Dev | n | Std Dev | n | Std Dev | n | Std Dev | n | Std Dev | |||||
| Under 2 | 21 | 6 | 27% | 15 | 5 | 24% | 15 | 4 | 33% | 11 | 3 | 29% | 11 | 4 | 27% |
| Age 2 to 5 | 17 | 4 | 22% | 14 | 3 | 24% | 12 | 4 | 27% | 9 | 3 | 25% | 8 | 3 | 21% |
| Age 5 to 12 | 24 | 6 | 33% | 21 | 5 | 35% | 13 | 4 | 29% | 12 | 4 | 33% | 12 | 3 | 29% |
| Age 13 to 15 | 14 | 5 | 19% | 10 | 6 | 17% | 6 | 2 | 11% | 5 | 2 | 13% | 9 | 3 | 23% |
| Pre-COVID | Containment | Delay | Mitigation | Reopening: Phase One | Total | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2020 | 2018/ 2019 | Change (n) | 2020 | 2018/ 2019 | Change (n) | 2020 | 2018/ 2019 | Change (n) | 2020 | 2018/ 2019 | Change (n) | 2020 | 2018/ 2019 | Change (n) | 2020 | 2018/ 2019 | Change (n) | |
| Respiratory | 2 | 0 | 2 | 0 | 1 | −1 | 0 | 0 | 0 | 1 | 2 | −1 | 3 | 0 | 3 | 6 | 3 | 4 |
| Endocrine/ Metabolic | 33 | 38 | −5 | 9 | 7 | 2 | 3 | 6 | −3 | 15 | 24 | −9 | 4 | 13 | −9 | 64 | 87 | −23 |
| Digestive | 2 | 3 | −1 | 0 | 2 | −2 | 0 | 1 | −1 | 1 | 4 | −3 | 0 | 1 | −1 | 3 | 10 | −7 |
| Haematology/ Oncology | 11 | 23 | −12 | 3 | 4 | −1 | 1 | 8 | −7 | 6 | 16 | −10 | 3 | 5 | −2 | 24 | 54 | −30 |
| Total | 48 | 64 | −16 | 12 | 13 | −1 | 4 | 14 | −10 | 23 | 45 | −22 | 10 | 18 | −8 | 97 | 153 | −56 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
McDonnell, T.; Nicholson, E.; Conlon, C.; Barrett, M.; Cummins, F.; Hensey, C.; McAuliffe, E. Assessing the Impact of COVID-19 Public Health Stages on Paediatric Emergency Attendance. Int. J. Environ. Res. Public Health 2020, 17, 6719. https://doi.org/10.3390/ijerph17186719
McDonnell T, Nicholson E, Conlon C, Barrett M, Cummins F, Hensey C, McAuliffe E. Assessing the Impact of COVID-19 Public Health Stages on Paediatric Emergency Attendance. International Journal of Environmental Research and Public Health. 2020; 17(18):6719. https://doi.org/10.3390/ijerph17186719
Chicago/Turabian StyleMcDonnell, Thérèse, Emma Nicholson, Ciara Conlon, Michael Barrett, Fergal Cummins, Conor Hensey, and Eilish McAuliffe. 2020. "Assessing the Impact of COVID-19 Public Health Stages on Paediatric Emergency Attendance" International Journal of Environmental Research and Public Health 17, no. 18: 6719. https://doi.org/10.3390/ijerph17186719
APA StyleMcDonnell, T., Nicholson, E., Conlon, C., Barrett, M., Cummins, F., Hensey, C., & McAuliffe, E. (2020). Assessing the Impact of COVID-19 Public Health Stages on Paediatric Emergency Attendance. International Journal of Environmental Research and Public Health, 17(18), 6719. https://doi.org/10.3390/ijerph17186719







