“I Get That Spirit in Me”—Mentally Empowering Workplace Health Promotion for Female Workers in Low-Paid Jobs during Menopause and Midlife
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants and Recruitment
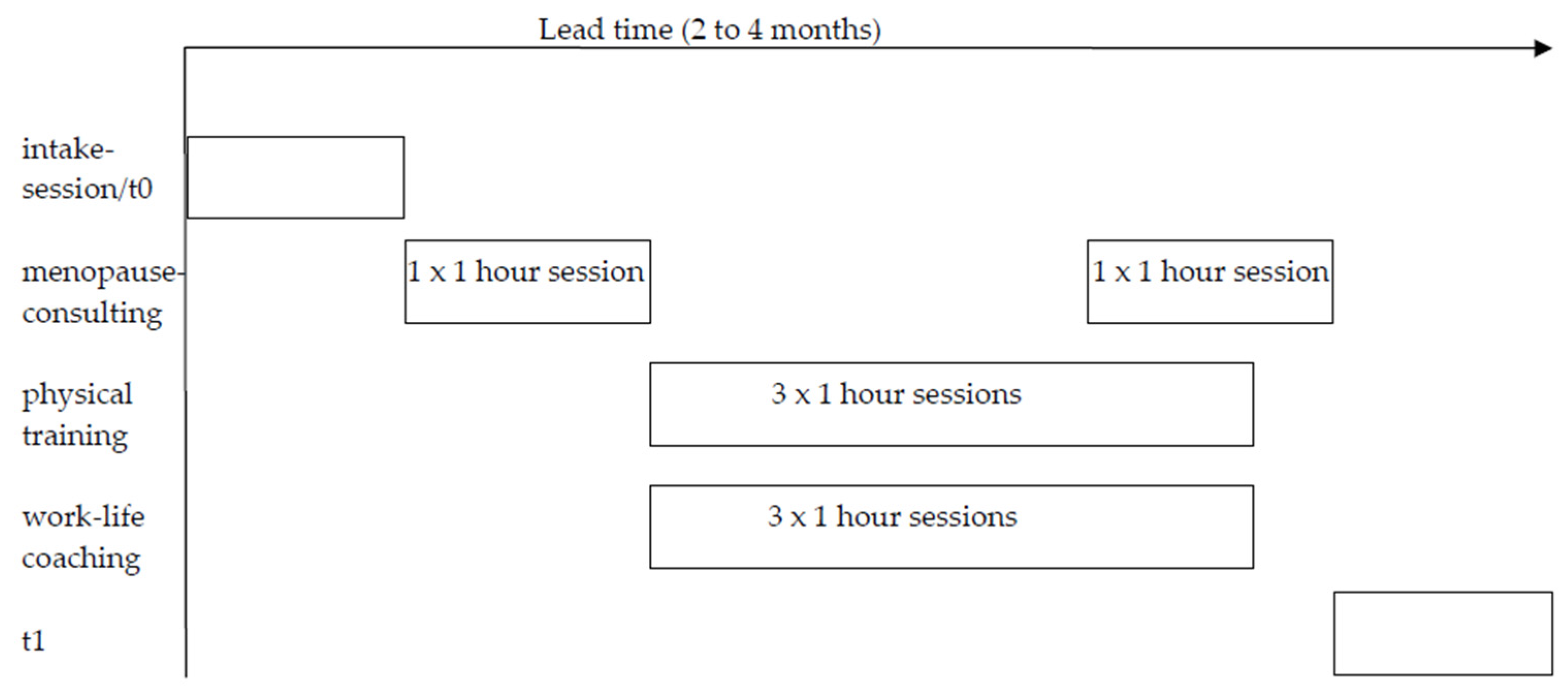
2.3. Intervention
2.4. Data Collection
2.4.1. Quantitative Study
Procedure
Measures
2.4.2. Qualitative Study
Procedure
2.5. Data Analysis
2.5.1. Quantitative
2.5.2. Qualitative
3. Results
3.1. Quantitative
3.1.1. Participant Characteristics
3.1.2. Pre-Test–Post-Test Outcomes
3.2. Qualitative
No, I have become stronger. […] So, about me? I am now really super strong. (20190924)Yes, I have had some really good talks with you. And that has given me a real lift, it has given me the power, the power to keep on going! (20200123)Liberation haha, yes, a sort of weight has been lifted off my shoulders. (20191127)
Yes, you learn, but change...? Nothing has really changed... No, there hasn’t been much change for me. (20191105)
3.2.1. Behavioral Changes
No, but it has had a big effect on me. As I have said before, I often got backache when I’d been walking. Walking is good, so what am I doing wrong? I thought it was just my back. I mean, when you get older your back starts to hurt, but it is probably due to the fact that I was holding myself too straight and stiff, and walking too fast. I don’t know, but now I am much more conscious of how I should walk. (20191111)
Yes, after six hours [of working] I get home at 3:00 p.m. Normally it is 3:00 p.m., go by the supermarket, and get home at 3:30 p.m. Oh, then I go to the attic, iron, fold, tidy up, clean, go to the kitchen, I’m done at 8:00 p.m. […] And then I don’t feel like going outside anymore. (20191105)
Then in my women’s group, in our group of Hindustani women, well they don’t talk about themselves. But, with this thingy [WLP] you can talk freely. And also I can be aware now, for my daughters-in-law for example. So I can explain to them, if you are in your 40s, or around 45 or in your 50s, then you can get these symptoms. […] But no-one said: maybe menopause, that … They don’t talk much. I am happy that you have come up with this program and that such things exist in the Netherlands. That we can get on with it. (20200123)
It all starts with the handover. […] I was someone that was like ‘don’t mess with me’. You know, but now I think what the...? [colleague’s name] is just a colleague, I come to work, she says what is happening on the ward. I need to sort it out and solve it myself. […] Yes, it has changed. Because… I really wasn’t easy. […] No. I was just full of anger. [...] as a flex worker you find yourself in different situations every time. [...] And one person can say never mind let it go, but the other you say today is a collision. I don’t want to be like that anymore. (20190924)
3.2.2. Changes in Physical Health
Before I go to sleep I do the exercise for maybe ten minutes or fifteen minutes. At the start I did five minutes, or maybe not even four minutes, I was really tired. I couldn’t carry on. I really had to get out of bed and have a drink of water. But now, although it has taken some time, I have been doing it now … what…. almost six, seven, eight weeks. […] And thanks to doing her exercises, I don’t need to use my inhaler as much. I used to use it seven times a day and now it is only three. […] I am wondering that if I, continue if maybe I will get down to using it only once, or maybe not at all. My aim is to not use it at all. (20200123)
Maybe it is because of those, those vitamin tablets. And also my food—I have started eating more vegetables. And more nuts. I used not to eat those much. So that kind of thing, that diet wheel that has, that helps too. And I think it has more benefits. Because I was really in pain. I really couldn’t... (20200123)
3.2.3. Changes in Mental Wellbeing
3.2.4. Changes in the Workplace
She also taught me that I should try, also try, must try to hand over work to someone else. I’m, I always want to do everything myself, but she says, she said to me: you have to try to hand things over to someone else. Then you feel lighter in your head too, so I went to my manager and told her. And now she has assigned people, they are fellow students, they don’t actually do much on the ward. And they, they may help me, or they have to help me. It is in their job description. She has hung up a list with their job description, and they help me. And I walk up to them, and then I ask very politely if they can help with this or… you know what I mean? So, it is a success, yes it is. (20191127)
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kopenhager, T.; Guidozzi, F. Working Women and the Menopause. Climacteric 2015, 18, 372–375. [Google Scholar] [CrossRef] [PubMed]
- Sarrel, P.M. Women, work, and menopause. Menopause 2012, 19, 250–252. [Google Scholar] [CrossRef] [PubMed]
- CBS. Arbeidsdeelname; Kerncijfers. Available online: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/82309ned/table?fromstatweb (accessed on 26 May 2020).
- Geukes, M.; Van Aalst, M.P.; Robroek, S.J.; Laven, J.S.; Oosterhof, H. The impact of menopause on work ability in women with severe menopausal symptoms. Maturitas 2016, 90, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Payne, S.; Doyal, L. Older women, work and health. Occup. Med. 2010, 60, 172–177. [Google Scholar] [CrossRef]
- Verdonk, P.; Hooftman, W.E.; Van Veldhoven, M.J.; Boelens, L.R.; Koppes, L.L. Work-related fatigue: The specific case of highly educated women in the Netherlands. Int. Arch. Occup. Environ. Health 2010, 83, 309–321. [Google Scholar] [CrossRef]
- Karnaki, P.; Polychronakis, I.; Linos, A.; Kotsioni, I. Introduction to health promotion for working women: A methodology. In Promoting Health for Working Women; Linos, A., Kirch, W., Eds.; Springer: New York, NY, USA, 2008; pp. 3–29. [Google Scholar]
- Viotti, S.; Guidetti, G.; Converso, D.; Sottimano, I. Fostering Work Ability Among Menopausal Women. Does Any Work-Related Psychosocial Factor Help? Int. J. Women’s Health 2020, 12, 399. [Google Scholar] [CrossRef]
- CBS. Meer Ziekteverzuim Bij Vrouwen Dan Bij Mannen. Available online: https://www.cbs.nl/nl-nl/nieuws/2017/42/meer-ziekteverzuim-bij-vrouwen-dan-bij-mannen (accessed on 26 May 2020).
- Bekker, M.H.; Rutte, C.G.; Van Rijswijk, K. Sickness absence: A gender-focused review. Psychol. Health Med. 2009, 14, 405–418. [Google Scholar] [CrossRef]
- Jack, G.; Riach, K.; Bariola, E.; Pitts, M.; Schapper, J.; Sarrel, P. Menopause in the workplace: What employers should be doing. Maturitas 2016, 85, 88–95. [Google Scholar] [CrossRef]
- Stringhini, S.; Sabia, S.; Shipley, M.; Brunner, E.; Nabi, H.; Kivimaki, M.; Singh-Manoux, A. Association of socioeconomic position with health behaviors and mortality. JAMA 2010, 303, 1159–1166. [Google Scholar] [CrossRef]
- Dillaway, H.E. When does menopause occur, and how long does it last? Wrestling with age-and time-based conceptualizations of reproductive aging. NWSA J. 2006, 31–60. [Google Scholar] [CrossRef]
- Griffiths, A.; MacLennan, S.J.; Hassard, J. Menopause and work: An electronic survey of employees’ attitudes in the UK. Maturitas 2013, 76, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Samsioe, G.; Borgfeldt, C.; Lidfeldt, J.; Agardh, C.D.; Nerbrand, C. Menopause-related symptoms: What are the background factors? A prospective population-based cohort study of Swedish women (The Women’s Health in Lund Area study). Am. J. Obstet. Gynecol. 2003, 189, 1646–1653. [Google Scholar] [CrossRef]
- Brzyski, R.G.; Medrano, M.A.; Hyatt-Santos, J.M.; Ross, J.S. Quality of life in low-income menopausal women attending primary care clinics. Fertil. Steril. 2001, 76, 44–50. [Google Scholar] [CrossRef]
- Avis, N.E.; Crawford, S.L.; McKinlay, S.M. Psychosocial, behavioral, and health factors related to menopause symptomatology. Womens Health 1997, 3, 103–120. [Google Scholar] [PubMed]
- Hunter, M.; Battersby, R.; Whitehead, M. Relationships between psychological symptoms, somatic complaints and menopausal status. Maturitas 1986, 8, 217–228. [Google Scholar] [CrossRef]
- Dennerstein, L.; Dudley, E.C.; Hopper, J.L.; Guthrie, J.R.; Burger, H.G. A prospective population-based study of menopausal symptoms. Obstet. Gynecol. 2000, 96, 351–358. [Google Scholar] [CrossRef]
- Polit, D.F.; LaRocco, S.A. Social and psychological correlates of menopausal symptoms. Psychosom. Med. 1980. [Google Scholar] [CrossRef]
- Sarrel, P.; Rousseau, M.; Mazure, C.; Glazer, W. Ovarian steroids and the capacity to function at home and in the workplace. Ann. N. Y. Acad. Sci. 1990, 592, 156–161. [Google Scholar] [CrossRef]
- High, R.V.; Marcellino, P.A. Menopausal women and the work environment. Soc. Behav. Pers. 1994, 22, 347–354. [Google Scholar] [CrossRef]
- Geukes, M.; Van Aalst, M.P.; Nauta, M.C.; Oosterhof, H. The impact of menopausal symptoms on work ability. Menopause 2012, 19, 278–282. [Google Scholar] [CrossRef]
- Gartoulla, P.; Bell, R.J.; Worsley, R.; Davis, S.R. Menopausal vasomotor symptoms are associated with poor self-assessed work ability. Maturitas 2016, 87, 33–39. [Google Scholar] [CrossRef]
- Olajubu, A.O.; Olowokere, A.E.; Amujo, D.O.; Olajubu, T.O. Influence of menopausal symptoms on perceived work ability among women in a Nigerian University. Climacteric 2017, 20, 558–563. [Google Scholar] [CrossRef]
- Appelman, Y.; Van Rijn, B.B.; Ten Haaf, M.E.; Boersma, E.; Peters, S.A. Sex differences in cardiovascular risk factors and disease prevention. Atherosclerosis 2015, 241, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Hardy, C.; Griffiths, A.; Hunter, M.S. What do working menopausal women want? A qualitative investigation into women’s perspectives on employer and line manager support. Maturitas 2017, 101, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Bendien, E.; Van Gemert, I.; Appelman, Y.; Verdonk, P. Werken Aan De Overgang. Een Uitgebreide Literatuurstudie Naar Overgang, Menopauze, Gezondheid, En Werk; Amsterdam UMC-VUmc: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Ariyoshi, H. Evaluation of menopausal interventions at a Japanese company. AAOHN J. 2009, 57, 106–111. [Google Scholar] [CrossRef]
- Hardy, C.; Griffiths, A.; Norton, S.; Hunter, M.S. Self-help cognitive behavior therapy for working women with problematic hot flushes and night sweats (MENOS@Work): A multicenter randomized controlled trial. Menopause 2018, 25, 508–519. [Google Scholar] [CrossRef] [PubMed]
- Geukes, M.; Anema, J.R.; Van Aalst, M.P.; De Menezes, R.X.; Oosterhof, H. Improvement of menopausal symptoms and the impact on work ability: A retrospective cohort pilot study. Maturitas 2019, 120, 23–28. [Google Scholar] [CrossRef]
- Rutanen, R.; Nygård, C.-H.; Moilanen, J.; Mikkola, T.; Raitanen, J.; Tomas, E.; Luoto, R. Effect of physical exercise on work ability and daily strain in symptomatic menopausal women: A randomized controlled trial. Work 2014, 47, 281–286. [Google Scholar] [CrossRef]
- Creswell, J.W. A Concise Introduction to Mixed Methods Research; SAGE Publications: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Audrey, S.; Holliday, J.; Parry-Langdon, N.; Campbell, R. Meeting the challenges of implementing process evaluation within randomized controlled trials: The example of ASSIST (A Stop Smoking in Schools Trial). Health Educ. Res. 2006, 21, 366–377. [Google Scholar] [CrossRef]
- Robinson, O.C. Sampling in interview-based qualitative research: A theoretical and practical guide. Qual. Res. Psychol. 2014, 11, 25–41. [Google Scholar] [CrossRef]
- An, C.; Yu, Y.Y.; Chou, B.C.; Szu, L.Y.; Tsao, L.I. Empowering self-care ability—A follow-up study of clinical-based perimenopausal women personal health counselling. J. Clin. Nurs. 2016, 25, 2979–2988. [Google Scholar] [CrossRef] [PubMed]
- Hunter, M.S.; Griffiths, A.; Mann, E.; Moss-Morris, R.; Smith, M.; Slade, P. NICE guidance on menopause: Cognitive behavioural therapy is an effective non-hormonal intervention for managing vasomotor symptoms. BMJ 2015, 351, h6434. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mishra, G.; Kuh, D. Perceived change in quality of life during the menopause. Soc. Sci. Med. 2006, 62, 93–102. [Google Scholar] [CrossRef]
- CBS. Standaarddefinitie van Allochtonen. Available online: https://www.cbs.nl/nl-nl/achtergrond/2000/48/standaarddefinitie-allochtonen (accessed on 15 June 2020).
- Stronks, K.; Kulu-Glasgow, I.; Agyemang, C. The utility of ‘country of birth’for the classification of ethnic groups in health research: The Dutch experience. Ethn. Health 2009, 14, 255–269. [Google Scholar] [CrossRef]
- CBS. Standaard Onderwijsindeling (SOI). Available online: https://www.cbs.nl/nl-nl/onze-diensten/methoden/classificaties/onderwijs-en-beroepen/standaard-onderwijsindeling--soi-- (accessed on 17 August 2020).
- Tang, K.L.; Rashid, R.; Godley, J.; Ghali, W.A. Association between subjective social status and cardiovascular disease and cardiovascular risk factors: A systematic review and meta-analysis. BMJ Open 2016, 6, e010137. [Google Scholar] [CrossRef]
- Adler, N.E.; Epel, E.S.; Castellazzo, G.; Ickovics, J.R. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychol. 2000, 19, 586–592. [Google Scholar] [CrossRef]
- Harlow, S.D.; Gass, M.; Hall, J.E.; Lobo, R.; Maki, P.; Rebar, R.W.; Sherman, S.; Sluss, P.M.; de Villiers, T.J.; Group, S.C. Executive summary of the Stages of Reproductive Aging Workshop+ 10: Addressing the unfinished agenda of staging reproductive aging. J. Clin. Endocrinol. Metab. 2012, 97, 1159–1168. [Google Scholar] [CrossRef]
- Van Veldhoven, M.; Broersen, S. Measurement quality and validity of the “need for recovery scale”. Occup. Environ. Med. 2003, 60, i3–i9. [Google Scholar] [CrossRef]
- Boezeman, E.J.; Sluiter, J.K.; Nieuwenhuijsen, K. Measuring Work Functioning: Validity of a Weighted Composite Work Functioning Approach. J. Occup. Rehabil. 2015, 25, 537–542. [Google Scholar] [CrossRef]
- Boezeman, E.J.; Nieuwenhuijsen, K.; De Bekker-Grob, E.W.; Van den Akker-Van, M.E.; Sluiter, J.K. The relative importance of the domains of work functioning: Evaluations of health-impaired employees, healthy employees, and employers. J. Occup. Environ. Med. 2015, 57, 361–366. [Google Scholar] [CrossRef]
- Greene, J.G. Constructing a standard climacteric scale. Maturitas 1998, 61, 78–84. [Google Scholar] [CrossRef] [PubMed]
- El Fassi, M.; Bocquet, V.; Majery, N.; Lair, M.L.; Couffignal, S.; Mairiaux, P. Work ability assessment in a worker population: Comparison and determinants of Work Ability Index and Work Ability score. BMC Public Health 2013, 13, 305. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.W. Statistical Power Analysis for the Behavioral Sciences; Taylor & Francis Inc.: Abingdon, Oxfordshire, UK, 1988. [Google Scholar]
- Morris, S.B. Estimating effect sizes from pretest-posttest-control group designs. Organ. Res. Methods 2008, 11, 364–386. [Google Scholar] [CrossRef]
- Boeije, H. Analyseren in Kwalitatief Onderzoek: Denken en Doen; Boom: Amsterdam, The Netherlands, 2005. [Google Scholar]
- Bandura, A. Self-Efficacy: The exErcise of Control; W H Freeman/Times Books/ Henry Holt & Co.: New York, NY, USA, 1997. [Google Scholar]
- Teuscher, D.; Bukman, A.J.; Van Baak, M.A.; Feskens, E.J.; Renes, R.J.; Meershoek, A. Challenges of a healthy lifestyle for socially disadvantaged people of Dutch, Moroccan and Turkish origin in the Netherlands: A focus group study. Crit. Public Health 2015, 25, 615–626. [Google Scholar] [CrossRef]
- Qi, X.; Liu, Y.; Zhang, J.; Ji, S.; Sluiter, J.K.; Zhou, R.; Deng, H. Relationship between work strain, need for recovery after work and cumulative cortisol among kindergarten teachers. Int. J. Occup. Environ. Health 2015, 88, 1053–1059. [Google Scholar] [CrossRef]
- De Croon, E.M.; Sluiter, J.K.; Frings-Dresen, M.H. Psychometric properties of the Need for Recovery after work scale: Test-retest reliability and sensitivity to detect change. J. Occup. Environ. Med. 2006, 63, 202–206. [Google Scholar] [CrossRef]
- Sluiter, J.; De Croon, E.; Meijman, T.; Frings-Dresen, M. Need for recovery from work related fatigue and its role in the development and prediction of subjective health complaints. J. Occup. Environ. Med. 2003, 60, i62–i70. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, K.; Sluiter, J.K.; Dewa, C.S. Need for recovery as an early sign of depression risk in a working population. J. Occup. Environ. Med. 2016, 58, e350–e354. [Google Scholar] [CrossRef]
- Griffiths, A.; Ceausu, I.; Depypere, H.; Lambrinoudaki, I.; Mueck, A.; Perez-Lopez, F.R.; Van der Schouw, Y.T.; Senturk, L.M.; Simoncini, T.; Stevenson, J.C.; et al. EMAS recommendations for conditions in the workplace for menopausal women. Maturitas 2016, 85, 79–81. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
| Lifestyle |
| Perceived changes |
| Tell me whether you experienced any changes in your body, exercise habits, or nutrition after following the work-life program (WLP). |
| Tell me what has changed. Tell me how this has changed. Tell me why nothing has changed. |
| Contribution WLP |
| Tell me how and if the WLP contributed to these changes. |
| Health |
| Perceived changes |
| Tell me whether you experienced any changes in your health – menopausal symptoms, physical- and mental health—after following the WLP. |
| Tell me what has changed. Tell me how this has changed. Tell me why nothing has changed. |
| Contribution WLP |
| Tell me how and if the WLP contributed to these changes. |
| Work functioning |
| Perceived changes |
| Tell me whether you experienced any changes in your work after following the WLP. |
| Tell me whether you experienced any changes in your work-life balance after following the WLP. |
| Tell me what has changed. Tell me how this has changed. Tell me why nothing has changed. |
| Contribution WLP |
| Tell me how and if the WLP contributed to these changes. |
| Descriptive | n | (%) | Mean | SD |
|---|---|---|---|---|
| Age | 52.6 | 4.5 | ||
| Ethnicity | ||||
| Ethnic minority | 36 | (51.4%) | ||
| Ethnic majority (Dutch) | 34 | (48.6%) | ||
| Educational level | ||||
| Low | 29 | (41.4%) | ||
| Intermediate | 36 | (51.4%) | ||
| High | 5 | (7.1%) | ||
| Subjective social status (SSS) 1 | 4.7 | 1.5 | ||
| Living situation | ||||
| Alone | 11 | (15.7%) | ||
| With partner | 11 | (15.7%) | ||
| With partner and children | 32 | (45.7%) | ||
| No partner but with children | 15 | (21.4%) | ||
| Other | 1 | (1.4%) | ||
| Main wage earner | ||||
| Yes | 38 | (54.3%) | ||
| No, my partner | 24 | (34.3%) | ||
| Equal with partner | 8 | (11.4%) | ||
| Type of contract | ||||
| Full time | 22 | (31.4%) | ||
| Part time | 48 | (68.6%) | ||
| Informal care responsibilities | ||||
| Yes | 15 | (21.4%) | ||
| No | 55 | (78.6%) | ||
| Menopausal status 2 | ||||
| Pre-menopause | 4 | (7.1%) | ||
| Early peri-menopause | 3 | (5.4%) | ||
| Late peri-menopause | 3 | (5.4%) | ||
| Post-menopause | 38 | (67.9%) | ||
| Unknown | 8 | (14.3%) |
| n2 | T0 (Pre-Test) 3 | n2 | T1 (Post-Test) | Pre- and Post-Test | Effect Size | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | Mean Diff 4 | t or z 5 | p | ||||
| Work functioning problems (0–100) (lower is better) | 65 | 21.1 (20.0) | 54 | 18.6 (16.0) | z = −0.27 | 0.791 | ||||
| Work performance | 70 | 00.0 (6.0) | 55 | 00.0 (6.0) | z = 0.59 | 0.556 | ||||
| Need for recovery after work 1 | 70 | 40.9 (55.0) | 55 | 36.4 (64.0) | z = −0.66 | 0.508 | ||||
| Quantity of work | 66 | 21.4 (19.88) | 54 | 20.8 (16.68) | 2.4 | t = 0.94 | 0.350 | |||
| Capacity to work | 69 | 18.8 (27.0) | 55 | 19.6 (25.0) | z = 0.99 | 0.320 | ||||
| Menopausal symptoms (GCS) (0–63) (lower is better) | 70 | 18.0 (12.0) | 56 | 13.0 (11.0) | z = −3.91 | 0.000 | 0.39 (0.03, 0.74) | |||
| Psychological | 70 | 8.5 (8.0) | 56 | 7.0 (7.0) | z = −2.59 | 0.010 | 0.30 (−0.05, 0.66) | |||
| Anxiety | 70 | 4.8 (3.10) | 56 | 4.4 (2.73) | 0.5 | t = 1.68 | 0.099 | |||
| Depression | 70 | 4.0 (4.0) | 56 | 3.0 (4.0) | z = −3.08 | 0.002 | 0.41 (0.05, 0.76) | |||
| Somatic | 70 | 5.4 (3.04) | 56 | 4.3 (2.81) | 1.1 | t = 3.47 | 0.001 | 0.35 (−0.00, 0.71) | ||
| Vasomotor | 70 | 2.0 (3.0) | 56 | 2.0 (3.0) | z = −3.24 | 0.001 | 0.33 (−0.02, 0.68) | |||
| Sexual dysfunction | 70 | 1.0 (1.0) | 56 | 0.0 (1.0) | z = −0.78 | 0.438 | ||||
| Quality of life (0–100) (higher is better) | ||||||||||
| Physically | 70 | 48.8 (15.0) | 56 | 50.1 (10.0) | z = −1.15 | 0.250 | ||||
| Mentally | 70 | 48.2 (10.37) | 56 | 48.7 (9.40) | −0.2 | t = −0.12 | 0.908 | |||
| Work ability (0–10) (higher is better) | 70 | 7.0 (1.0) | 56 | 8.0 (1.0) | z = −1.80 | 0.072 | ||||
| Descriptive | n | (%) | Mean | SD |
|---|---|---|---|---|
| Age | 53.4 | 4.2 | ||
| Ethnicity | ||||
| Ethnic minority 1 | 7 | (58.3%) | ||
| Ethnic majority (Dutch) | 5 | (41.7%) | ||
| Educational level | ||||
| Low | 4 | (33.3%) | ||
| Intermediate | 8 | (66.7%) | ||
| High | 0 | (0.0%) | ||
| Type of contract | ||||
| Full time | 6 | (50.0%) | ||
| Part time | 6 | (50.0%) | ||
| Living situation | ||||
| Alone | 2 | (16.7%) | ||
| With partner | 3 | (25.0%) | ||
| With partner and children | 6 | (50.0%) | ||
| No partner but with children | 1 | (8.3%) | ||
| Menopausal status | ||||
| Pre-menopause | 1 | (8.3%) | ||
| Early peri-menopause | 1 | (8.3%) | ||
| Late peri-menopause | 0 | (0.0%) | ||
| Post-menopause | 9 | (75.0%) | ||
| Unknown | 1 | (8.3%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Verburgh, M.; Verdonk, P.; Appelman, Y.; Brood-van Zanten, M.; Nieuwenhuijsen, K. “I Get That Spirit in Me”—Mentally Empowering Workplace Health Promotion for Female Workers in Low-Paid Jobs during Menopause and Midlife. Int. J. Environ. Res. Public Health 2020, 17, 6462. https://doi.org/10.3390/ijerph17186462
Verburgh M, Verdonk P, Appelman Y, Brood-van Zanten M, Nieuwenhuijsen K. “I Get That Spirit in Me”—Mentally Empowering Workplace Health Promotion for Female Workers in Low-Paid Jobs during Menopause and Midlife. International Journal of Environmental Research and Public Health. 2020; 17(18):6462. https://doi.org/10.3390/ijerph17186462
Chicago/Turabian StyleVerburgh, Marjolein, Petra Verdonk, Yolande Appelman, Monique Brood-van Zanten, and Karen Nieuwenhuijsen. 2020. "“I Get That Spirit in Me”—Mentally Empowering Workplace Health Promotion for Female Workers in Low-Paid Jobs during Menopause and Midlife" International Journal of Environmental Research and Public Health 17, no. 18: 6462. https://doi.org/10.3390/ijerph17186462
APA StyleVerburgh, M., Verdonk, P., Appelman, Y., Brood-van Zanten, M., & Nieuwenhuijsen, K. (2020). “I Get That Spirit in Me”—Mentally Empowering Workplace Health Promotion for Female Workers in Low-Paid Jobs during Menopause and Midlife. International Journal of Environmental Research and Public Health, 17(18), 6462. https://doi.org/10.3390/ijerph17186462






