Narrative Review on Health-EDRM Primary Prevention Measures for Vector-Borne Diseases
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A. Keywords Used for Literature Search
References
- Vector-Borne Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/vector-borne-diseases (accessed on 31 May 2020).
- Lemon, S.M.; Sparling, P.F.; Hamburg, M.A.; Relman, D.A.; Choffnes, E.R.; Mack, A. Vector-Borne Diseases: Understanding the Environmental, Human Health, and Ecological Connections; The National Academies Press: Washington, DC, USA, 2008; pp. 1–27. ISBN 9780309108973. [Google Scholar]
- WHO. Global Vector Control Response 2017–2030; World Health Organization: Geneva, Switzerland, 2017; ISBN 9789241564090. [Google Scholar]
- Wu, X.; Lu, Y.; Zhou, S.; Chen, L.; Xu, B. Impact of climate change on human infectious diseases: Empirical evidence and human adaptation. Environ. Int. 2016, 86, 14–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoshen, M.B.; Morse, A.P. A weather-driven model of malaria transmission. Malar. J. 2004, 3. [Google Scholar] [CrossRef] [Green Version]
- Caminade, C.; McIntyre, K.M.; Jones, A.E. Impact of recent and future climate change on vector-borne diseases. Ann. N. Y. Acad. Sci. 2019, 1436, 157–173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fouque, F.; Reeder, J.C. Impact of past and on-going changes on climate and weather on vector-borne diseases transmission: A look at the evidence. Infect. Dis. Poverty 2019, 8. [Google Scholar] [CrossRef] [PubMed]
- Mathers, C. Global Burden of Disease. In International Encyclopedia of Public Health; Academic Press: Cambridge, MA, USA, 2016; ISBN 9780128037089. [Google Scholar]
- James, S.L.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 Diseases and Injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1859–1922. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. World Malaria Report 2019; World Health Organization: Geneva, Switzerland, 2019; ISBN 9789241565721. [Google Scholar]
- Mccarthy, D.; Wolf, H.; Wu, Y. Malaria and Growth; The World Bank: Washington, DC, USA, 2000; pp. 2–26. [Google Scholar] [CrossRef] [Green Version]
- United Nations. The Sustainable Development Goals Report 2019; United Nations: New York, NY, USA, 2019. [Google Scholar]
- The Global Fund: Malaria. Available online: https://www.theglobalfund.org/en/malaria/ (accessed on 31 May 2020).
- WHO. Health Emergency and Disaster Risk Management: Overview; World Health Organization: Geneva, Switzerland, 2019; ISBN 9789241516181. [Google Scholar]
- World Health Organisation. Emergency Risk Management for Health—Overview; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- World Health Organization. Sendai Framework for Disaster Risk Reduction 2015–2030; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Wright, N.; Fagan, L.; Lapitan, J.M.; Kayano, R.; Abrahams, J.; Huda, Q.; Murray, V. Health Emergency and Disaster Risk Management: Five Years into Implementation of the Sendai Framework. Int. J. Disaster Risk Sci. 2020, 11, 206–217. [Google Scholar] [CrossRef]
- Chan, E.Y.Y.; Shaw, R. Public Health and Disasters: Health Emergency and Disaster Risk Management in Asia; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar]
- Boslaugh, S. Prevention: Primary, Secondary, and Tertiary. In Encyclopedia of Epidemiology; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2008; pp. 839–840. [Google Scholar]
- Alison, M. Global Health Impacts of Vector-Borne Diseases. In Global Health Impacts of Vector-Borne Diseases; The National Academies Press: Washington, DC, USA, 2016; pp. 1–59. [Google Scholar]
- World Health Organization. A Global Brief on Vector-Borne Diseases; World Health Organization: Geneva, Switzerland, 2014; p. 9. [Google Scholar]
- World Health Organisation. International Clinical Trials Registry Platform; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
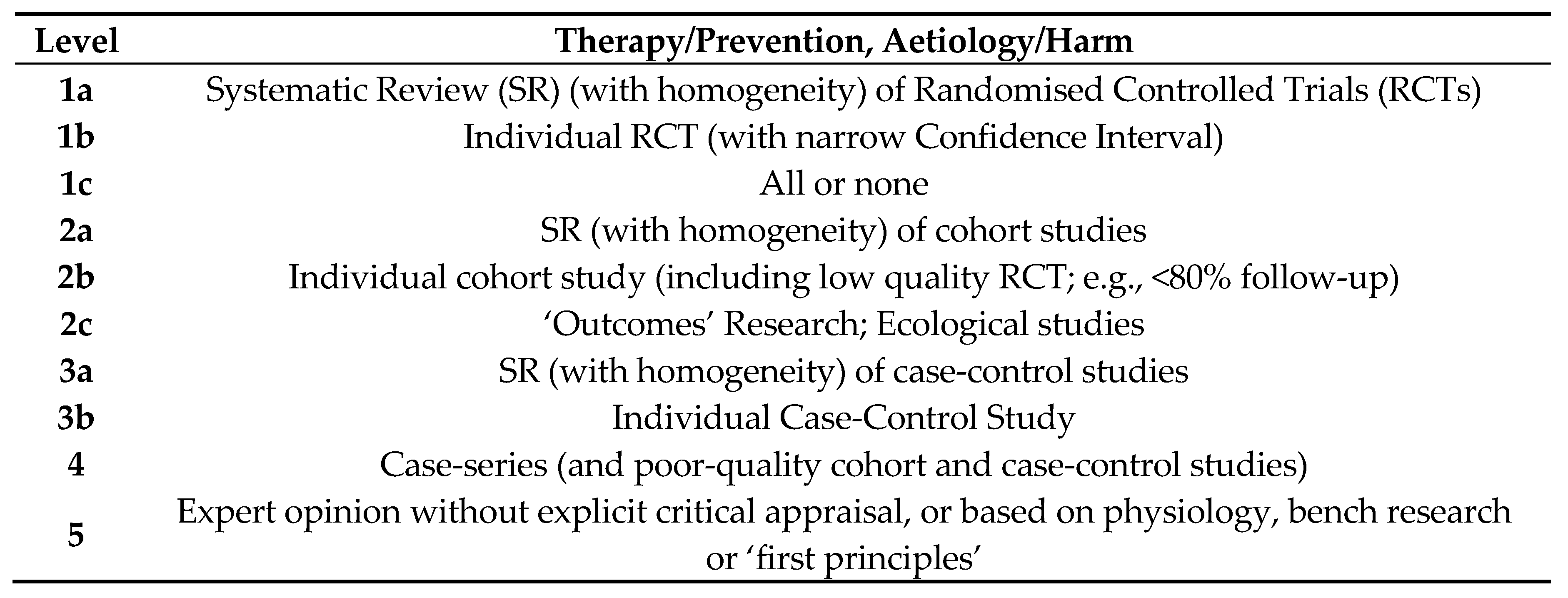
- OCEBM Levels of Evidence Working Group. “The Oxford 2009 Levels of Evidence”. Oxford Center for Evidence-Based Medicine. Available online: https://www.cebm.net/index.aspx?o=5653 (accessed on 10 August 2020).
- Achee, N.L.; Youngblood, L.; Bangs, M.J.; Lavery, J.V.; James, S. Considerations for the use of human participants in vector biology research: A tool for investigators and regulators. Vector-Borne Zoonotic Dis. 2015, 15, 89–102. [Google Scholar] [CrossRef] [Green Version]
- Saavedra, M.P.; Conn, J.E.; Alava, F.; Carrasco-Escobar, G.; Prussing, C.; Bickersmith, S.A.; Sangama, J.L.; Fernandez-Miñope, C.; Guzman, M.; Tong, C.; et al. Higher risk of malaria transmission outdoors than indoors by Nyssorhynchus darlingi in riverine communities in the Peruvian Amazon. Parasites Vectors 2019, 12. [Google Scholar] [CrossRef]
- Nakkhara, P.; Chongsuvivatwong, V.; Thammapalo, S. Risk factors for symptomatic and asymptomatic chikungunya infection. Trans. R. Soc. Trop. Med. Hyg. 2013, 107, 789–796. [Google Scholar] [CrossRef]
- Wallace, J.W.; Nicholson, W.L.; Perniciaro, J.L.; Vaughn, M.F.; Funkhouser, S.; Juliano, J.J.; Lee, S.; Kakumanu, M.L.; Ponnusamy, L.; Apperson, C.S.; et al. Incident Tick-Borne Infections in a Cohort of North Carolina Outdoor Workers. Vector-Borne Zoonotic Dis. 2016, 16, 302–308. [Google Scholar] [CrossRef]
- Tangena, J.A.A.; Thammavong, P.; Lindsay, S.W.; Brey, P.T. Risk of exposure to potential vector mosquitoes for rural workers in Northern Lao PDR. PLoS Negl. Trop. Dis. 2017, 11. [Google Scholar] [CrossRef] [PubMed]
- Ndoen, E.; Wild, C.; Dale, P.; Sipe, N.; Dale, M. Dusk to dawn activity patterns of anopheline mosquitoes in West Timor and Java, Indonesia. Southeast Asian J. Trop. Med. Public Health 2011, 42, 550–561. [Google Scholar] [PubMed]
- Van Bortel, W.; Trung, H.D.; Hoi, L.X.; Van Ham, N.; Van Chut, N.; Luu, N.D.; Roelants, P.; Denis, L.; Speybroeck, N.; D’Alessandro, U.; et al. Malaria transmission and vector behaviour in a forested malaria focus in central Vietnam and the implications for vector control. Malar. J. 2010, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loeb, M.; Elliott, S.J.; Gibson, B.; Fearon, M.; Nosal, R.; Drebot, M.; D’Cuhna, C.; Harrington, D.; Smith, S.; George, P.; et al. Protective behavior and West Nile virus risk. Emerg. Infect. Dis. 2005, 11, 1433–1436. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, S.; Gething, P.W.; Brady, O.J.; Messina, J.P.; Farlow, A.W.; Moyes, C.L.; Drake, J.M.; Brownstein, J.S.; Hoen, A.G.; Sankoh, O.; et al. The global distribution and burden of dengue. Nature 2013. [Google Scholar] [CrossRef]
- Tokarevich, N.; Tronin, A.; Gnativ, B.; Revich, B.; Blinova, O.; Evengard, B. Impact of air temperature variation on the ixodid ticks habitat and tick-borne encephalitis incidence in the Russian Arctic: The case of the Komi Republic. Int. J. Circumpolar Health 2017, 76. [Google Scholar] [CrossRef]
- Chowdhury, F.R.; Ibrahim, Q.S.U.; Shafiqul Bari, M.; Jahangir Alam, M.M.; Dunachie, S.J.; Rodriguez-Morales, A.J.; Ismail Patwary, M. The association between temperature, rainfall and humidity with common climate-sensitive infectious diseases in Bangladesh. PLoS ONE 2018, 15, e0199579. [Google Scholar] [CrossRef]
- Vázquez, M.; Muehlenbein, C.; Cartter, M.; Hayes, E.B.; Ertel, S.; Shapiro, E.D. Effectiveness of personal protective measures to prevent lyme disease. Emerg. Infect. Dis. 2008, 14, 210–216. [Google Scholar] [CrossRef]
- Barnard, D.R. Global Collaboration for Development of Pesticides for Public Health (GCDPP) Repellents and Toxicants for Personal Protection; World Health Organization: Geneva, Switzerland, 2000; Volume 46, pp. 408–418. [Google Scholar]
- Donohoe, H.; Pennington-Gray, L.; Omodior, O. Lyme disease: Current issues, implications, and recommendations for tourism management. Tour. Manag. 2015, 46, 408–418. [Google Scholar] [CrossRef]
- Linos, E.; Keiser, E.; Fu, T.; Colditz, G.; Chen, S.; Tang, J.Y. Hat, shade, long sleeves, or sunscreen? Rethinking US sun protection messages based on their relative effectiveness. Cancer Causes Control 2011. [Google Scholar] [CrossRef] [Green Version]
- Szykitka, W. Big Book of Self-Reliant Living: Advice and Information on just about Everything You Need to Know to Live on Planet Earth; The Lyons Press: Guilford, CT, USA, 2010; p. 65. [Google Scholar]
- Harahap, R. Sumatran Tigers Seen on Plantation in Riau. Available online: https://www.thejakartapost.com/news/2019/02/28/sumatran-tigers-seen-on-plantation-in-riau.html (accessed on 31 May 2020).
- Takahata, C.; Nielsen, S.E.; Takii, A.; Izumiyama, S. Habitat selection of a large carnivore along human-wildlife boundaries in a highly modified landscape. PLoS ONE 2014, 9, e0086181. [Google Scholar] [CrossRef] [PubMed]
- Gu, S.; Wang, A.; Bian, G.; He, T.; Yi, B.; Lu, B.; Li, X.; Xu, G. Relationship between weather factors and heat stroke in Ningbo city. Chin. J. Endem. 2016, 37, 1131–1136. [Google Scholar] [CrossRef]
- Kenny, G.P.; Wilson, T.E.; Flouris, A.D.; Fujii, N. Heat exhaustion. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2018; pp. 505–529. [Google Scholar]
- Zeng, J.; Zhang, X.; Yang, J.; Bao, J.; Xiang, H.; Dear, K.; Liu, Q.; Lin, S.; Lawrence, W.R.; Lin, A.; et al. Humidity may modify the relationship between temperature and cardiovascular mortality in Zhejiang province, China. Int. J. Environ. Res. Public Health 2017, 14, 1383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, L.W.; Lin, H.Y.; Hsu, C.Y.; Rau, H.H.; Chen, P.L. Effect of weather and time on trauma events determined using emergency medical service registry data. Injury 2015, 46, 1814–1820. [Google Scholar] [CrossRef]
- Crawshaw, A.F.; Maung, T.M.; Shafique, M.; Sint, N.; Nicholas, S.; Li, M.S.; Roca-Feltrer, A.; Hii, J. Acceptability of insecticide-treated clothing for malaria prevention among migrant rubber tappers in Myanmar: A cluster-randomized non-inferiority crossover trial. Malar. J. 2017, 16. [Google Scholar] [CrossRef] [Green Version]
- Ruiu, L.; Floris, I. Susceptibility of environmentally friendly sheep wool insulation panels to the common clothes moth tineola bisselliella in laboratory assays. Insects 2019, 10, 379. [Google Scholar] [CrossRef] [Green Version]
- Gao, C.; Kuklane, K.; Östergren, P.O.; Kjellstrom, T. Occupational heat stress assessment and protective strategies in the context of climate change. Int. J. Biometeorol. 2018, 62, 359–371. [Google Scholar] [CrossRef]
- Unger, A.; Riley, L.W. Slum health: From understanding to action. PLoS Med. 2007, 4, 1561–1566. [Google Scholar] [CrossRef] [Green Version]
- Sobel, A.H. Tropical Weather. Nat. Educ. Knowl. 2012, 3, 2. [Google Scholar]
- Stjernberg, L.; Berglund, J. Detecting ticks on light versus dark clothing. Scand. J. Infect. Dis. 2009, 37, 361–364. [Google Scholar] [CrossRef]
- Dejenie, T.; Yohannes, M.; Assmelash, T. Characterization of Mosquito Breeding Sites in and in the Vicinity of Tigray Microdams. Ethiop. J. Health Sci. 2011, 21, 57–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sumodan, P.K. Species diversity of mosquito breeding in rubber plantations of Kerala, India. J. Am. Mosq. Control Assoc. 2012, 28, 114–115. [Google Scholar] [CrossRef] [PubMed]
- Mackensie, J.S.; Lindsay, M.D.; Broom, A.K. Effect of climate and weather on the transmission of Ross River and Murray Valley encephalitis viruses. Microbiol. Aust. 2000, 21, 40. [Google Scholar]
- Reinhold, J.M.; Lazzari, C.R.; Lahondère, C. Effects of the environmental temperature on Aedes aegypti and Aedes albopictus mosquitoes: A review. Insects 2018, 9, 158. [Google Scholar] [CrossRef] [Green Version]
- Eldridge, B.F.; Edman, J.D.; Moncayo, A.C. Medical Entomology: A Textbook on Public Health and Veterinary Problems Caused by Arthropods. J. Med. Entomol. 2000, 116, 15086–15095. [Google Scholar] [CrossRef]
- Sherrard-Smith, E.; Skarp, J.E.; Beale, A.D.; Fornadel, C.; Norris, L.C.; Moore, S.J.; Mihreteab, S.; Charlwood, J.D.; Bhatt, S.; Winskill, P.; et al. Mosquito feeding behavior and how it influences residual malaria transmission across Africa. Proc. Natl. Acad. Sci. USA 2019. [Google Scholar] [CrossRef] [Green Version]
- Sutherst, R.W. Global Change and Human Vulnerability to Vector-Borne Diseases. Clin. Microbiol. Rev. 2004, 17, 136–167. [Google Scholar] [CrossRef] [Green Version]
- Leal, W.S. The enigmatic reception of DEET—The gold standard of insect repellents. Curr. Opin. Insect Sci. 2014, 6, 93–98. [Google Scholar] [CrossRef] [Green Version]
- CDC, Centers for Disease Control and Prevention. Fight the Bite for Protection from Malaria Guidelines for DEET Insect Repellent Use; CDC: Atlanta, GA, USA, 2005; p. 1.
- Staub, D.; Debrunner, M.; Amsler, L.; Steffen, R. Effectiveness of a repellent containing DEET and EBAAP for preventing tick bites. Wilderness Environ. Med. 2002, 13, 12–20. [Google Scholar] [CrossRef] [Green Version]
- Onyett, H.; Bortolussi, R.; Bridger, N.A.; Finlay, J.C.; Martin, S.; McDonald, J.C.; Robinson, J.L.; Salvadori, M.I.; Vanderkooi, O.G.; Allen, U.D.; et al. Preventing mosquito and tick bites: A Canadian update. Paediatr. Child Health 2014, 19, 326–328. [Google Scholar] [CrossRef] [Green Version]
- Tips for Using Insect Repellents. Available online: https://www.chp.gov.hk/en/features/38927.html (accessed on 31 May 2020).
- Msellemu, D.; Shemdoe, A.; Makungu, C.; Mlacha, Y.; Kannady, K.; Dongus, S.; Killeen, G.F.; Dillip, A. The underlying reasons for very high levels of bed net use, and higher malaria infection prevalence among bed net users than non-users in the Tanzanian city of Dar es Salaam: A qualitative study. Malar. J. 2017, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ochomo, E.O.; Bayoh, N.M.; Walker, E.D.; Abongo, B.O.; Ombok, M.O.; Ouma, C.; Githeko, A.K.; Vulule, J.; Yan, G.; Gimnig, J.E. The efficacy of long-lasting nets with declining physical integrity may be compromised in areas with high levels of pyrethroid resistance. Malar. J. 2013, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, M.P.; Steinhardt, L.C.; Mwandama, D.; Mzilahowa, T.; Gimnig, J.E.; Bauleni, A.; Wong, J.; Wiegand, R.; Mathanga, D.P.; Lindblade, K.A. The effectiveness of older insecticide-treated bed nets (ITNs) to prevent malaria infection in an area of moderate pyrethroid resistance: Results from a cohort study in Malawi. Malar. J. 2020, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Insecticide-Treated Bed Nets. Available online: https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html (accessed on 31 May 2020).
- Jayanti, P.; Acharya, I.A. A Study on Efficacy of LLINS As Compared To In-Use ITNs Amongst Troops in a Malaria Endemic Area. J. Trop. Dis. 2015, 3. [Google Scholar] [CrossRef] [Green Version]
- Clem, A.S. Fundamentals of vaccine immunology. J. Glob. Infect. Dis. 2011, 3, 73–78. [Google Scholar] [CrossRef]
- McBride, W.J.H. Chemoprophylaxis of tropical infectious diseases. Pharmaceuticals 2010, 3, 1561–1575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, A.L.; Dhiman, R.C.; Kitron, U.; Scott, T.W.; van den Berg, H.; Lindsay, S.W. Benefit of Insecticide-Treated Nets, Curtains and Screening on Vector Borne Diseases, Excluding Malaria: A Systematic Review and Meta-analysis. PLoS Negl. Trop. Dis. 2014, 8. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.W.; Liao, Y.M.; Liu, H.; Nie, R.H.; Havumaki, J. Use of bed nets and factors that influence bed net use among jinuo ethnic minority in southern China. PLoS ONE 2014, 9, e0103780. [Google Scholar] [CrossRef]
- Das, M.L.; Singh, S.P.; Vanlerberghe, V.; Rijai, S.; Rai, M.; Karki, P.; Sundar, S.; Boelaert, M. Population preference of net texture prior to bed net trial in Kala-Azar-endemic areas. PLoS Negl. Trop. Dis. 2007, 1. [Google Scholar] [CrossRef] [Green Version]
- Maia, M.F.; Moore, S.J. Plant-based insect repellents: A review of their efficacy, development and testing. Malar. J. 2011, 10. [Google Scholar] [CrossRef] [Green Version]
- Batish, D.R.; Singh, H.P.; Kohli, R.K.; Kaur, S. Eucalyptus essential oil as a natural pesticide. For. Ecol. Manag. 2008, 256, 2166–2174. [Google Scholar] [CrossRef]
- McHenry, M.; Lacuesta, G. Severe allergic reaction to diethyltoluamide (DEET) containing insect repellent. Allergy, Asthma Clin. Immunol. 2014, 10. [Google Scholar] [CrossRef]
- Nelson, K.E.; Williams, C.M. Infectious Disease Epidemiology: Theory and Practice; Jones & Bartlett Publishers: Burlington, MA, USA, 2008; pp. 1014–1015. [Google Scholar]
- Von Seidlein, L.; Ikonomidis, K.; Bruun, R.; Jawara, M.; Pinder, M.; Knols, B.G.J.; Knudsen, J.B. Airflow attenuation and bed net utilization: Observations from Africa and Asia. Malar. J. 2012, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ntonifor, N.H.; Veyufambom, S. Assessing the effective use of mosquito nets in the prevention of malaria in some parts of Mezam division, Northwest Region Cameroon. Malar. J. 2016, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pulford, J.; Hetzel, M.W.; Bryant, M.; Siba, P.M.; Mueller, I. Reported reasons for not using a mosquito net when one is available: A review of the published literature. Malar. J. 2011, 10. [Google Scholar] [CrossRef] [Green Version]
- Pugliese-Garcia, M.; Heyerdahl, L.W.; Mwamba, C.; Nkwemu, S.; Chilengi, R.; Demolis, R.; Guillermet, E.; Sharma, A. Factors influencing vaccine acceptance and hesitancy in three informal settlements in Lusaka, Zambia. Vaccine 2018, 36, 5617–5624. [Google Scholar] [CrossRef]
- Muhsen, K.; Abed El-Hai, R.; Amit-Aharon, A.; Nehama, H.; Gondia, M.; Davidovitch, N.; Goren, S.; Cohen, D. Risk factors of underutilization of childhood immunizations in ultraorthodox Jewish communities in Israel despite high access to health care services. Vaccine 2012, 30, 2109–2115. [Google Scholar] [CrossRef]
- The Lancet Infectious Diseases Malaria vaccination: A major milestone. Lancet Infect. Dis. 2019, 19, 559. [CrossRef] [Green Version]
- Malande, O.O.; Munube, D.; Afaayo, R.N.; Annet, K.; Bodo, B.; Bakainaga, A.; Ayebare, E.; Njunwamukama, S.; Mworozi, E.A.; Musyoki, A.M. Barriers to effective uptake and provision of immunization in a rural district in Uganda. PLoS ONE 2019, 14, e0212270. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez, S.D.; Drake, L.L.; Price, D.P.; Hammond, J.I.; Hansen, I.A.; Liu, N. The efficacy of some commercially available insect repellents for Aedes aegypti (Diptera: Culicidae) and Aedes albopictus (Diptera: Culicidae). J. Insect Sci. 2015, 15. [Google Scholar] [CrossRef]
- Legeay, S.; Clere, N.; Hilairet, G.; Do, Q.T.; Bernard, P.; Quignard, J.F.; Apaire-Marchais, V.; Lapied, B.; Faure, S. The insect repellent N,N-diethyl-m-Toluamide (DEET) induces angiogenesis via allosteric modulation of the M3 muscarinic receptor in endothelial cells. Sci. Rep. 2016, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swale, D.R.; Bloomquist, J.R. Is DEET a dangerous neurotoxicant? Pest Manag. Sci. 2019, 75. [Google Scholar] [CrossRef] [PubMed]
- Koren, G.; Matsui, D.; Bailey, B. DEET-based insect repellents: Safety implications for children and pregnant and lactating women. Can. Med. Assoc. J. 2003, 169, 209–212. [Google Scholar]
- Lenhart, A.; Orelus, N.; Maskill, R.; Alexander, N.; Streit, T.; McCall, P.J. Insecticide-treated bednets to control dengue vectors: Preliminary evidence from a controlled trial in Haiti. Trop. Med. Int. Heal. 2008, 13, 56–57. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, S.; Weiss, D.J.; Cameron, E.; Bisanzio, D.; Mappin, B.; Dalrymple, U.; Battle, K.E.; Moyes, C.L.; Henry, A.; Eckhoff, P.A.; et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature 2015, 526, 207–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawley, W.A.; Phillips-Howard, P.A.; Ter Kuile, F.O.; Terlouw, D.J.; Vulule, J.M.; Ombok, M.; Nahlen, B.L.; Gimnig, J.E.; Kariuki, S.K.; Kolczak, M.S.; et al. Community-wide effects of permethrin-treated bed nets on child mortality and malaria morbidity in western Kenya. Am. J. Trop. Med. Hyg. 2003, 68, 121–127. [Google Scholar] [CrossRef]
- Killeen, G.F.; Smith, T.A.; Ferguson, H.M.; Mshinda, H.; Abdulla, S.; Lengeler, C.; Kachur, S.P. Preventing childhood malaria in Africa by protecting adults from mosquitoes with insecticide-treated nets. PLoS Med. 2007, 4, 1246–1258. [Google Scholar] [CrossRef] [Green Version]
- Hauser, G.; Thiévent, K.; Koella, J.C. The ability of Anopheles gambiae mosquitoes to bite through a permethrin-treated net and the consequences for their fitness. Sci. Rep. 2019, 9. [Google Scholar] [CrossRef]
- World Health Organization. Vaccines and vaccination against yellow fever WHO Position Paper—June Note de synthèse: Position de l’ OMS sur les vaccins et la vaccination contre la fièvre jaune, juin 2013. Relevé Épidémiologique Hebdomadaire 2013, 88, 269–284. [Google Scholar]
- Gotuzzo, E.; Yactayo, S.; Córdova, E. Review article: Efficacy and duration of immunity after yellow fever vaccination: Systematic review on the need for a booster every 10 years. Am. J. Trop. Med. Hyg. 2013, 89, 434–444. [Google Scholar] [CrossRef] [Green Version]
- WHO Publication. Vaccines against tick-borne encephalitis: WHO position paper—Recommendations. Vaccine 2011, 86, 241–256. [Google Scholar] [CrossRef]
- Bogovic, P. Tick-borne encephalitis: A review of epidemiology, clinical characteristics, and management. World J. Clin. Cases 2015. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Japanese Encephalitis Vaccines: WHO position paper, February 2015—Recommendations. Vaccine 2016, 90, 69–88. [Google Scholar] [CrossRef]
- Hegde, N.R.; Gore, M.M. Japanese encephalitis vaccines: Immunogenicity, protective efficacy, effectiveness, and impact on the burden of disease. Hum. Vaccines Immunother. 2017, 13, 1320–1337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malaria Vaccine Pilot Launched in Malawi. Available online: https://www.who.int/news-room/detail/23-04-2019-malaria-vaccine-pilot-launched-in-malawi (accessed on 31 May 2020).
- Jover, J.A.; Leon, L.; Pato, E.; Loza, E.; Rosales, Z.; Matias, M.A.; Mendez-Fernandez, R.; Díaz-Valle, D.; Benitez-del-Castillo, J.M.; Abasolo, L. Long-term use of antimalarial drugs in rheumatic diseases. Clin. Exp. Rheumatol. 2012, 30, 380–387. [Google Scholar]
- Schwartz, E. Prophylaxis of Malaria. Mediterr. J. Hematol. Infect. Dis. 2012, 4. [Google Scholar] [CrossRef]
- Chen, L.H.; Wilson, M.E.; Schlagenhauf, P. Prevention of malaria in long-term travelers. J. Am. Med. Assoc. 2006, 296, 2234–2244. [Google Scholar] [CrossRef] [Green Version]
- First FDA-Approved Vaccine for the Prevention of Dengue Diseases in Endemic Regions. Available online: https://www.fda.gov/news-events/press-announcements/first-fda-approved-vaccine-prevention-dengue-disease-endemic-regions#:~:text=The_U.S._Food_and_Drug,who_live_in_endemic_areas (accessed on 31 May 2020).
- Da Silveira, L.T.C.; Tura, B.; Santos, M. Systematic review of dengue vaccine efficacy. BMC Infect. Dis. 2019, 19. [Google Scholar] [CrossRef]
- Du, S.; Liu, Y.; Liu, J.; Zhao, J.; Champagne, C.; Tong, L.; Zhang, R.; Zhang, F.; Qin, C.F.; Ma, P.; et al. Aedes mosquitoes acquire and transmit Zika virus by breeding in contaminated aquatic environments. Nat. Commun. 2019, 10. [Google Scholar] [CrossRef]
- Monteiro, V.V.S.; Navegantes-Lima, K.C.; De Lemos, A.B.; Da Silva, G.L.; De Souza Gomes, R.; Reis, J.F.; Junior, L.C.R.; Da Silva, O.S.; Romão, P.R.T.; Monteiro, M.C. Aedes-chikungunya virus interaction: Key role of vector midguts microbiota and its saliva in the host infection. Front. Microbiol. 2019, 10. [Google Scholar] [CrossRef] [Green Version]
- Soleimani-Ahmadi, M.; Vatandoost, H.; Zare, M. Characterization of larval habitats for anopheline mosquitoes in a malarious area under elimination program in the southeast of Iran. Asian Pac. J. Trop. Biomed. 2014, 4, 73–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ziraba, A.K.; Haregu, T.N.; Mberu, B. A review and framework for understanding the potential impact of poor solid waste management on health in developing countries. Arch. Public Health 2016, 74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hori, M.; Shibuya, K.; Sato, M.; Saito, Y. Lethal effects of short-wavelength visible light on insects. Sci. Rep. 2014, 4. [Google Scholar] [CrossRef] [PubMed]
- Puri, A.; Kumar, M.; Johal, E. Solid-waste management in Jalandhar city and its impact on community health. Indian J. Occup. Environ. Med. 2008, 12, 76–81. [Google Scholar] [CrossRef]
- Achudume, A.C.; Olawale, J.T. Microbial pathogens of public health significance in waste dumps and common sites. J. Environ. Biol. 2007, 28, 151–154. [Google Scholar]
- Bell, J.L.; Collins, J.W.; Wolf, L.; Gronqvist, R.; Chiou, S.; Chang, W.R.; Sorock, G.; Courtney, T.; Lombardi, D.; Evanoff, B. Evaluation of a comprehensive slip, trip and fall prevention programme for hospital employees. Ergonomics 2009, 51, 1905–1925. [Google Scholar] [CrossRef]
- Weinhold, B. A spreading concern: Inhalational health effects of mold. Environ. Health Perspect. 2007, 115, 300–305. [Google Scholar] [CrossRef] [Green Version]
- Mattiello, A.; Chiodini, P.; Bianco, E.; Forgione, N.; Flammia, I.; Gallo, C.; Pizzuti, R.; Panico, S. Health effects associated with the disposal of solid waste in landfills and incinerators in populations living in surrounding areas: A systematic review. Int. J. Public Health 2013, 58, 725–735. [Google Scholar] [CrossRef]
- Ferronato, N.; Torretta, V. Waste mismanagement in developing countries: A review of global issues. Int. J. Environ. Res. Public Health 2019, 16, 1060. [Google Scholar] [CrossRef] [Green Version]
- Abeyewickreme, W.; Wickremasinghe, A.R.; Karunatilake, K.; Sommerfeld, J.; Axel, K. Community mobilization and household level waste management for dengue vector control in Gampaha district of Sri Lanka; an intervention study. Pathog. Glob. Health 2012, 106, 479–487. [Google Scholar] [CrossRef] [Green Version]
- SDG7: Data and Projections. Available online: https://www.iea.org/reports/sdg7-data-and-projections/access-to-electricity (accessed on 31 May 2020).
- Ritchie, S.A.; Cortis, G.; Paton, C.; Townsend, M.; Shroyer, D.; Zborowski, P.; Hall-Mendelin, S.; Van Den Hurk, A.F. A Simple Non-Powered Passive Trap for the Collection of Mosquitoes for Arbovirus Surveillance. J. Med. Entomol. 2013, 50, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Bei, Y.; Zhang, J. Are Yellow Sticky Traps an Effective Method for Control of Sweetpotato Whitefly, Bemisia tabaci, in the Greenhouse or Field? J. Insect Sci. 2012, 12. [Google Scholar] [CrossRef]
- García-Betancourt, T.; Higuera-Mendieta, D.R.; González-Uribe, C.; Cortés, S.; Quintero, J. Understanding water storage practices of urban residents of an endemic dengue area in Colombia: Perceptions, rationale and socio-demographic characteristics. PLoS ONE 2015, 10, e0129054. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dambach, P.; Jorge, M.M.; Traoré, I.; Phalkey, R.; Sawadogo, H.; Zabré, P.; Kagoné, M.; Sié, A.; Sauerborn, R.; Becker, N.; et al. A qualitative study of community perception and acceptance of biological larviciding for malaria mosquito control in rural Burkina Faso. BMC Public Health 2018, 18. [Google Scholar] [CrossRef] [PubMed]
- Yukalang, N.; Clarke, B.; Ross, K. Barriers to effective municipal solid waste management in a rapidly urbanizing area in Thailand. Int. J. Environ. Res. Public Health 2017, 14, 1013. [Google Scholar] [CrossRef] [Green Version]
- Shockley Cruz, M.; Lindner, R.; Cruz, M.S.; Lindner, R. Insect Vision: Ultraviolet, Color, and LED Light. Ph.D. Thesis, University of Georgia Department of Entomology, Athens, GA, USA, 2011. [Google Scholar]
- Van Loon, J.J.A.; Smallegange, R.C.; Bukovinszkiné-Kiss, G.; Jacobs, F.; De Rijk, M.; Mukabana, W.R.; Verhulst, N.O.; Menger, D.J.; Takken, W. Mosquito Attraction: Crucial Role of Carbon Dioxide in Formulation of a Five-Component Blend of Human-Derived Volatiles. J. Chem. Ecol. 2015, 41, 567–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Hara, J.E.; UsUpensky, I.; Bostanian, N.J.; Capinera, J.L.; Chapman, R.; Barfield, C.S.; Swisher, M.E.; Barfield, C.S.; Heppner, J.; Fitzgerald, T.D.; et al. Traps for Capturing Insects. In Encyclopedia of Entomology; Springer Science & Business Media: Berlin, Germany, 2008; pp. 3675–4007. [Google Scholar]
- Zhou, Y.H.; Zhang, Z.W.; Fu, Y.F.; Zhang, G.C.; Yuan, S. Carbon dioxide, odorants, heat and visible cues affect wild mosquito landing in open spaces. Front. Behav. Neurosci. 2018, 12. [Google Scholar] [CrossRef] [PubMed]
- Lorenzi, O.D.; Major, C.; Acevedo, V.; Perez-Padilla, J.; Rivera, A.; Biggerstaff, B.J.; Munoz-Jordan, J.; Waterman, S.; Barrera, R.; Sharp, T.M. Reduced incidence of Chikungunya virus infection in communities with ongoing aedes aegypti mosquito trap intervention studies—Salinas and Guayama, Puerto Rico, November 2015–february 2016. Morb. Mortal. Wkly. Rep. 2016, 65, 479–480. [Google Scholar] [CrossRef] [Green Version]
- Junnila, A.; Kline, D.L.; Müller, G.C. Comparative efficacy of small commercial traps for the capture of adult Phlebotomus papatasi. J. Vector Ecol. 2011, 36, 172–178. [Google Scholar] [CrossRef]
- Sliney, D.H.; Gilbert, D.W.; Lyon, T. Ultraviolet safety assessments of insect light traps. J. Occup. Environ. Hyg. 2016, 13, 413–424. [Google Scholar] [CrossRef]
- Urban, J.E.; Broce, A. Killing of flies in electrocuting insect traps releases bacteria and viruses. Curr. Microbiol. 2000, 41, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Getachew, D.; Tekie, H.; Gebre-Michael, T.; Balkew, M.; Mesfin, A. Breeding sites of aedes aegypti: Potential dengue vectors in dire Dawa, east Ethiopia. Interdiscip. Perspect. Infect. Dis. 2015, 2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- UNICEF. Djibouti Humanitarian Situation Report No. 2 Flood Response; UNICEF: New York, NY, USA, 2019; pp. 1–5. [Google Scholar]
- Krystosik, A.; Njoroge, G.; Odhiambo, L.; Forsyth, J.E.; Mutuku, F.; LaBeaud, A.D. Solid Wastes Provide Breeding Sites, Burrows, and Food for Biological Disease Vectors, and Urban Zoonotic Reservoirs: A Call to Action for Solutions-Based Research. Front. Public Health 2020, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banerjee, S.; Aditya, G.; Saha, G.K. Household wastes as larval habitats of dengue vectors: Comparison between urban and rural areas of Kolkata, India. PLoS ONE 2015, 10, e0138082. [Google Scholar] [CrossRef] [Green Version]
- Becher, P.G.; Hagman, A.; Verschut, V.; Chakraborty, A.; Rozpędowska, E.; Lebreton, S.; Bengtsson, M.; Flick, G.; Witzgall, P.; Piškur, J. Chemical signaling and insect attraction is a conserved trait in yeasts. Ecol. Evol. 2018, 8, 2962–2974. [Google Scholar] [CrossRef] [Green Version]
- Billeter, J.C.; Wolfner, M.F. Chemical Cues that Guide Female Reproduction in Drosophila melanogaster. J. Chem. Ecol. 2018, 44, 750–769. [Google Scholar] [CrossRef] [Green Version]
- Boadi, K.O.; Kuitunen, M. Environmental and health impacts of household solid waste handling and disposal practices in Third World cities: The case of the Accra Metropolitan Area, Ghana. J. Environ. Health 2005, 68, 32–36. [Google Scholar]
- Barreiro, C.; Albano, H.; Silva, J.; Teixeira, P. Role of Flies as Vectors of Foodborne Pathogens in Rural Areas. ISRN Microbiol. 2013, 2013. [Google Scholar] [CrossRef] [Green Version]
- Zamora, D.M.B.; Hernández, M.M.; Torres, N.; Zúniga, C.; Sosa, W.; De Abrego, V.; Escobar, M.C.M. Information to act: Household characteristics are predictors of domestic infestation with the Chagas vector Triatoma dimidiata in central America. Am. J. Trop. Med. Hyg. 2015, 93. [Google Scholar] [CrossRef]
- Jawara, M.; Jatta, E.; Bell, D.; Burkot, T.R.; Bradley, J.; Hunt, V.; Kandeh, B.; Jones, C.; Manjang, A.M.; Pinder, M.; et al. New prototype screened doors and windows for excluding mosquitoes from houses: A pilot study in rural Gambia. Am. J. Trop. Med. Hyg. 2018, 99, 1475–1484. [Google Scholar] [CrossRef]
- Che-Mendoza, A.; Medina-Barreiro, A.; Koyoc-Cardeña, E.; Uc-Puc, V.; Contreras-Perera, Y.; Herrera-Bojórquez, J.; Dzul-Manzanilla, F.; Correa-Morales, F.; Ranson, H.; Lenhart, A.; et al. House screening with insecticide-treated netting provides sustained reductions in domestic populations of Aedes aegypti in Merida, Mexico. PLoS Negl. Trop. Dis. 2018, 12. [Google Scholar] [CrossRef] [PubMed]
- Tusting, L.S.; Ippolito, M.M.; Willey, B.A.; Kleinschmidt, I.; Dorsey, G.; Gosling, R.D.; Lindsay, S.W. The evidence for improving housing to reduce malaria: A systematic review and meta-analysis. Malar. J. 2015, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Massebo, F.; Lindtjørn, B. The effect of screening doors and windows on indoor density of Anopheles arabiensis in south-west Ethiopia: A randomized trial. Malar. J. 2013, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Musoke, D.; Karani, G.; Ssempebwa, J.C.; Musoke, M.B. Integrated approach to malaria prevention at household level in rural communities in Uganda: Experiences from a pilot project. Malar. J. 2018, 18, 1144–1156. [Google Scholar] [CrossRef] [Green Version]
- Matsui, E.C. Management of rodent exposure and allergy in the pediatric population. Curr. Allergy Asthma Rep. 2013, 13. [Google Scholar] [CrossRef] [Green Version]
- Hopkins, A.S.; Whitetail-Eagle, J.; Corneli, A.L.; Person, B.; Ettestad, P.J.; DiMenna, M.; Norstog, J.; Creswell, J.; Khan, A.S.; Olson, J.G.; et al. Experimental evaluation of rodent exclusion methods to reduce hantavirus transmission to residents in a Native American community in New Mexico. Vector Borne Zoonotic Dis. 2002, 2, 61–68. [Google Scholar] [CrossRef]
- Jones, C.H.; Benítez-Valladares, D.; Guillermo-May, G.; Dzul-Manzanilla, F.; Che-Mendoza, A.; Barrera-Pérez, M.; Selem-Salas, C.; Chablé-Santos, J.; Sommerfeld, J.; Kroeger, A.; et al. Use and acceptance of long lasting insecticidal net screens for dengue prevention in Acapulco, Guerrero, Mexico. BMC Public Health 2014, 14. [Google Scholar] [CrossRef] [Green Version]
- Bonner, P.C.; Schmidt, W.P.; Belmain, S.R.; Oshin, B.; Baglole, D.; Borchert, M. Poor housing quality increases risk of rodent infestation and lassa fever in refugee camps of sierra leone. Am. J. Trop. Med. Hyg. 2007, 77, 169–175. [Google Scholar] [CrossRef] [Green Version]
- Safan, M.A.; Etman, Z.A.; Konswa, A. Evaluation of polyurethane resin injection for concrete leak repair. Case Stud. Constr. Mater. 2019, 11. [Google Scholar] [CrossRef]
- Tseloni, A.; Farrell, G.; Thompson, R.; Evans, E.; Tilley, N. Domestic burglary drop and the security hypothesis. Crime Sci. 2017, 6. [Google Scholar] [CrossRef] [Green Version]
- Carter, A.D. Are Housing Improvements an Effective Supplemental Vector Control Strategy to Reduce Malaria Transmission? A Systematic Review. Ph.D. Thesis, Georgia State University, Atlanta, GA, USA, 2014. [Google Scholar]
- Bublitz, D.A.C.; Poché, R.M.; Garlapati, R. Measures to control Phlebotomus argentipes and visceral leishmaniasis in India. J. Arthropod. Borne. Dis. 2016, 10, 113–126. [Google Scholar] [PubMed]
- Kaindoa, E.W.; Finda, M.; Kiplagat, J.; Mkandawile, G.; Nyoni, A.; Coetzee, M.; Okumu, F.O. Housing gaps, mosquitoes and public viewpoints: A mixed methods assessment of relationships between house characteristics, malaria vector biting risk and community perspectives in rural Tanzania. Malar. J. 2018, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogoma, S.B.; Kannady, K.; Sikulu, M.; Chaki, P.P.; Govella, N.J.; Mukabana, W.R.; Killeen, G.F. Window screening, ceilings and closed eaves as sustainable ways to control malaria in Dar es Salaam, Tanzania. Malar. J. 2009, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ranjan, A.; Sur, D.; Singh, V.P.; Siddique, N.A.; Manna, B.; Lal, C.S.; Sinha, P.K.; Kishore, K.; Bhattacharya, S.K. Risk factors for Indian kala-azar. Am. J. Trop. Med. Hyg. 2005, 73, 74–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, E.Y.Y.; Shaw, R. Public Health Humanitarian Responses to Natural Disasters; Springer: Berlin/Heidelberg, Germany, 2017; ISBN 9781317357445. [Google Scholar]
- Ryan, J. Environmental Health in Emergencies and Disasters: A Practical Guide. Emerg. Med. J. 2002, 22, 610. [Google Scholar] [CrossRef] [Green Version]
- Laaser, U.; Dorey, S.; Nurse, J. A plea for global health action bottom-up. Front. Public Health 2016, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hou, S.I. Health Education: Theoretical Concepts, Effective Strategies and Core Competencies; World Health Organization: Geneva, Switzerland, 2012; Volume 15, ISBN 9789290218289. [Google Scholar]
- Naranjo, D.P.; Qualls, W.A.; Jurado, H.; Perez, J.C.; De Xue, R.; Gomez, E.; Beier, J.C. Vector control programs in Saint Johns County, Florida and Guayas, Ecuador: Successes and barriers to integrated vector management. BMC Public Health 2014, 14. [Google Scholar] [CrossRef]
- Demanou, M.; Pouillot, R.; Grandadam, M.; Boisier, P.; Kamgang, B.; Hervé, J.P.; Rogier, C.; Rousset, D.; Paupy, C. Evidence of Dengue Virus Transmission and Factors Associated with the Presence of Anti-Dengue Virus Antibodies in Humans in Three Major Towns in Cameroon. PLoS Negl. Trop. Dis. 2014, 8. [Google Scholar] [CrossRef]
- Poinsignon, A.; Boulanger, D.; Binetruy, F.; Elguero, E.; Darriet, F.; Gallian, P.; De Lamballerie, X.; Charrel, R.N.; Remoue, F. Risk factors of exposure to Aedes albopictus bites in mainland France using an immunological biomarker. Epidemiol. Infect. 2019, 147. [Google Scholar] [CrossRef]
- Reiter, P.; Lathrop, S.; Bunning, M.; Biggerstaff, B.; Singer, D.; Tiwari, T.; Baber, L.; Amador, M.; Thirion, J.; Hayes, J.; et al. Texas lifestyle limits transmission of dengue virus. Emerg. Infect. Dis. 2003, 9, 86–89. [Google Scholar] [CrossRef]
- Bloch, D.; Roth, N.M.; Caraballo, E.V.; Muñoz-Jordan, J.; Hunsperger, E.; Rivera, A.; Pérez-Padilla, J.; Rivera Garcia, B.; Sharp, T.M. Use of Household Cluster Investigations to Identify Factors Associated with Chikungunya Virus Infection and Frequency of Case Reporting in Puerto Rico. PLoS Negl. Trop. Dis. 2016, 10. [Google Scholar] [CrossRef]
- Mathanga, D.P.; Mwandama, D.A.; Bauleni, A.; Chisaka, J.; Shah, M.P.; Landman, K.Z.; Lindblade, K.A.; Steinhardt, L.C. The effectiveness of long-lasting, insecticide-treated nets in a setting of pyrethroid resistance: A case-control study among febrile children 6 to 59 months of age in Machinga District, Malawi. Malar. J. 2015, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pryce, J.; Richardson, M.; Lengeler, C. Insecticide-treated nets for preventing malaria. Cochrane Database Syst. Rev. 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Deletre, E.; Martin, T.; Duménil, C.; Chandre, F. Insecticide resistance modifies mosquito response to DEET and natural repellents. Parasites Vectors 2019, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Handbook for Integrated Vector Management; World Health Organization: Geneva, Switzerland, 2013; ISBN 9789241502801. [Google Scholar]
- Wilson, A.L.; Boelaert, M.; Kleinschmidt, I.; Pinder, M.; Scott, T.W.; Tusting, L.S.; Lindsay, S.W. Evidence-based vector control? Improving the quality of vector control trials. Trends Parasitol. 2015, 31, 380–390. [Google Scholar] [CrossRef] [Green Version]
- Corrin, T.; Waddell, L.; Greig, J.; Young, I.; Hierlihy, C.; Mascarenhas, M. Risk perceptions, attitudes, and knowledge of chikungunya among the public and health professionals: A systematic review. Trop. Med. Health 2017, 45. [Google Scholar] [CrossRef] [Green Version]
- Degroote, S.; Zinszer, K.; Ridde, V. Interventions for vector-borne diseases focused on housing and hygiene in urban areas: A scoping review. Infect. Dis. Poverty 2018, 7. [Google Scholar] [CrossRef]
- Giantsis, I.A.; Chaskopoulou, A. Broadening the tools for studying sand fly breeding habitats: A novel molecular approach for the detection of phlebotomine larval DNA in soil substrates. Acta Trop. 2019, 190, 123–128. [Google Scholar] [CrossRef]
- Moncaz, A.; Faiman, R.; Kirstein, O.; Warburg, A. Breeding sites of Phlebotomus sergenti, the sand fly vector of cutaneous leishmaniasis in the Judean desert. PLoS Negl. Trop. Dis. 2012, 6. [Google Scholar] [CrossRef] [Green Version]
- Vivero, R.J.; Torres-Gutierrez, C.; Bejarano, E.E.; Peña, H.C.; Estrada, L.G.; Florez, F.; Ortega, E.; Aparicio, Y.; Muskus, C.E. Study on natural breeding sites of sand flies (Diptera: Phlebotominae) in areas of Leishmania transmission in Colombia. Parasites Vectors 2015, 8. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Dengue Guidelines for Diagnosis, Treatment, Prevention and Control; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Iwamura, T.; Guzman-Holst, A.; Murray, K.A. Accelerating invasion potential of disease vector Aedes aegypti under climate change. Nat. Commun. 2020, 1. [Google Scholar] [CrossRef] [PubMed]
- Campbell-Lendrum, D.; Manga, L.; Bagayoko, M.; Sommerfeld, J. Climate change and vector-borne diseases: What are the implications for public health research and policy? Philos. Trans. R. Soc. B Biol. Sci. 2015, 370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Parametres | Wear Protective Clothing When Outdoors | Avoid Heading Outdoors to Vector-Prone Areas and During Peak Biting Conditions | |
|---|---|---|---|
| Vector-Prone Areas | Peak Biting Conditions | ||
| Risk |
|
| |
| Behavioural Change |
|
| |
| Co-benefit(s) |
| ||
| Enabling Factor(s) |
|
| |
| Limiting Factor(s) and/or Alternative(s) |
| ||
|
| ||
| |||
| Strength of Evidence |
|
| |
| Parametre | Apply Insect Repellent | Sleep Under Bed Nets | Receive Prophylactic Vaccinations and Chemoprophylaxis |
|---|---|---|---|
| Risk |
| ||
| Behavioural Change |
|
| |
| Co-benefit(s) |
|
|
|
| Enabling Factor(s) |
|
|
|
| Limiting Factor(s) and/or Alternative(s) |
|
|
|
| Strength of Evidence |
|
|
|
| Parametre | Use Insect-Killing Traps | Manage Stagnant Water Appropriately | Manage Waste Appropriately |
|---|---|---|---|
| Risk |
|
|
|
| Behavioural Change |
|
|
|
| Co-benefit(s) |
|
| |
| Enabling Factor(s) |
|
|
|
| Limiting Factor(s) and/or Alternative(s) |
|
| |
| Strength of Evidence |
|
|
|
| Parametre | Minimise Household Entry Points | Cover Exposed Foodstuffs | |
|---|---|---|---|
| Wall Cracks | Door and Window Openings | ||
| Risk |
|
| |
|
| ||
| Behavioural Change |
| ||
| |||
| Co-benefit(s) |
| ||
|
| ||
| Enabling Factor(s) |
|
|
|
| Limiting Factor(s) and/or Alternative(s) |
|
| |
|
| ||
| Strength of Evidence |
|
|
|
| Category | Intervention | Number of Reviewed Articles under Each Category in the OCEBM Levels of Evidence | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1a | 1b | 1c | 2a | 2b | 2c | 3a | 3b | 4 | 5 | Others * | Total | ||
| Personal Protection Practices | Wear Protective Clothing When Outdoors | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 4 | 4 | 3 | 14 |
| Avoid Heading Outdoors to Vector-Prone Areas and During Peak Biting Conditions | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 16 | 4 | 23 | |
| Apply Insect Repellent | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 9 | 5 | 17 | |
| Sleep Under Bed Nets | 2 | 2 | 0 | 0 | 2 | 0 | 1 | 0 | 5 | 7 | 3 | 22 | |
| Receive Prophylactic Vaccinations and Chemoprophylaxis | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 3 | 8 | 6 | 20 | |
| Environmental Management Practices | Use Insect-Killing Traps | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 5 | 14 |
| Manage Stagnant Water Appropriately | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 1 | 11 | 1 | 15 | |
| Manage Waste Appropriately | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 4 | 2 | 9 | |
| Customary Household Practices | Minimise Household Entry Points | 1 | 3 | 0 | 1 | 1 | 0 | 0 | 1 | 6 | 3 | 2 | 18 |
| Cover Exposed Foodstuffs | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 2 | 2 | 1 | 7 | |
| Total | 4 | 9 | 0 | 3 | 7 | 0 | 2 | 3 | 27 | 72 | 32 | 159 ** | |
| Research Gaps | |
|---|---|
| 1 | Current studies on health-EDRM primary prevention measures for VBDs mostly focus on health risk reduction practices, yet efficacy evaluation on actual disease reduction is lacking. |
| 2 | Available literature is mostly classified as cross-sectional studies. Evidence on efficacy of the prevention measure based on randomised controlled studies or extensive cohort studies is limited. |
| 3 | Comparative evaluations for variations of certain primary prevention measures, such as efficacy of different insect-killing mechanisms or household modification materials, are limited. |
| 4 | Research outcomes are skewed towards certain vectors (e.g., mosquitoes). Research evidence on other vectors such as sand flies or ticks is limited. |
| 5 | Research outcomes are skewed towards certain VBDs (e.g., malaria). Research evidence on other VBDs such as Zika, chikungunya, or tick-borne encephalitis is limited. |
| 6 | Research and evidence on available alternatives to the proposed practices (e.g., using natural substitutes as opposed to chemical-based insect repellents) is limited. |
| 7 | Updated research on evidence relating technological advancements and the rapid change of ecological and human living environments to behavioural practices against VBDs is limited. |
| 8 | Consistency in recommendations from research papers, policies, and frontline international agencies (e.g., as in DEET concentration recommendations) is lacking. |
| 9 | Literature highlighting the effectiveness of multi-faceted, multi-sectoral and coordinated responses in enabling effective risk mitigation for population-level protection is lacking. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, E.Y.Y.; Sham, T.S.T.; Shahzada, T.S.; Dubois, C.; Huang, Z.; Liu, S.; Hung, K.K.C.; Tse, S.L.A.; Kwok, K.O.; Chung, P.-H.; et al. Narrative Review on Health-EDRM Primary Prevention Measures for Vector-Borne Diseases. Int. J. Environ. Res. Public Health 2020, 17, 5981. https://doi.org/10.3390/ijerph17165981
Chan EYY, Sham TST, Shahzada TS, Dubois C, Huang Z, Liu S, Hung KKC, Tse SLA, Kwok KO, Chung P-H, et al. Narrative Review on Health-EDRM Primary Prevention Measures for Vector-Borne Diseases. International Journal of Environmental Research and Public Health. 2020; 17(16):5981. https://doi.org/10.3390/ijerph17165981
Chicago/Turabian StyleChan, Emily Ying Yang, Tiffany Sze Tung Sham, Tayyab Salim Shahzada, Caroline Dubois, Zhe Huang, Sida Liu, Kevin K.C. Hung, Shelly L.A. Tse, Kin On Kwok, Pui-Hong Chung, and et al. 2020. "Narrative Review on Health-EDRM Primary Prevention Measures for Vector-Borne Diseases" International Journal of Environmental Research and Public Health 17, no. 16: 5981. https://doi.org/10.3390/ijerph17165981
APA StyleChan, E. Y. Y., Sham, T. S. T., Shahzada, T. S., Dubois, C., Huang, Z., Liu, S., Hung, K. K. C., Tse, S. L. A., Kwok, K. O., Chung, P.-H., Kayano, R., & Shaw, R. (2020). Narrative Review on Health-EDRM Primary Prevention Measures for Vector-Borne Diseases. International Journal of Environmental Research and Public Health, 17(16), 5981. https://doi.org/10.3390/ijerph17165981







